Global Hypertension Guidelines: Are Central Haemodynamics Critical and Neglected
Article Information
Robert A PHILLIPSa, Stéphane G CARLIERb, Alessandro SCALIAb, Philippe DELMOTTEb, Giles N CATTERMOLEc, Joe BRIERLEYd
aThe Faculty of Medicine, The University of Queensland, Brisbane, Australia.
bDepartment of Cardiology, Hôpital Ambroise Par’e and University of Mons, Mons, Belgium.
cEmergency Medicine Department, Kings College Hospital NHS Foundation Trust, London, United Kingdom
dPaediatric Intensive Care Unit, Great Ormond St Hospital for Children and University College, London, United Kingdom.
*Corresponding Author: Rob Phillips, Faculty of Medicine, Herston Campus, University of Queensland, Brisbane, 4006, Australia.
Received: 07 September 2023; Accepted: 16 September 2023; Published: 15 December 2023
Citation: Robert A PHILLIPS, Stéphane G CARLIER, Alessandro SCALIA, Philippe DELMOTTE, Giles N CATTERMOLE, Joe BRIERLEY. Global Hypertension Guidelines: Are Central Haemodynamics Critical and Neglected. Anesthesia and Critical care 5(2023): 87-97
View / Download Pdf Share at FacebookAbstract
Hypertension (HTN) is an elevated blood pressure (BP) compared to normative data and occurs in 30-50% of adults and is the number one risk of human death. While non-invasive brachial BP defines hypertension, physiologically BP is the product of the central haemodynamic (CH) variables of stroke volume (SV), heart rate (HR), cardiac output (CO) and systemic vascular resistance (SVR) or BP = (SV x HR) x SVR. Pathophysiologically HTN is the result of one or more elevated CH parameters and while global clinical guidelines recommend anti-hypertensive therapy to reduce CH BP monitoring is recommended to monitor therapeutic effectiveness. Significantly control of people diagnosed with HTN remains persistently dismal at <23% while CH are ignored. We reviewed Australian, Canadian, Chinese, European, Japanese, Singaporean, UK, US and International HTN guidelines. The focus of the guidelines on cardiovascular physiology, allied science and novel concepts of HTN management were assessed using proprietary word-count functions targeting BP and CH, and the results tabulated. A total of 695 pages and 478,537 words were published in the nine representative global HTN guidelines, with BP parameters mentioned 7,535 times (99.4%), and CH parameters mentioned 47 times (0.6%), while 4 of 9 (44%) guidelines omitted any mention of CH. All guidelines recommended BP definitions and BP-centric therapies, without mention of CH. The adoption of CH in HTN practice may improve our understanding of the aetiology of HTN and advance precision therapy in adults and children with this pandemic condition
Keywords
Hypertension; Central Haemodynamics; physiology; Blood pressure; Hypertension Guidelines; Therapy; Outcomes.
Hypertension articles; Central Haemodynamics articles; physiology articles; Blood pressure articles; Hypertension Guidelines articles; Therapy articles; Outcomes articles.
Hypertension articles Hypertension Research articles Hypertension review articles Hypertension PubMed articles Hypertension PubMed Central articles Hypertension 2023 articles Hypertension 2024 articles Hypertension Scopus articles Hypertension impact factor journals Hypertension Scopus journals Hypertension PubMed journals Hypertension medical journals Hypertension free journals Hypertension best journals Hypertension top journals Hypertension free medical journals Hypertension famous journals Hypertension Google Scholar indexed journals Central Haemodynamics articles Central Haemodynamics Research articles Central Haemodynamics review articles Central Haemodynamics PubMed articles Central Haemodynamics PubMed Central articles Central Haemodynamics 2023 articles Central Haemodynamics 2024 articles Central Haemodynamics Scopus articles Central Haemodynamics impact factor journals Central Haemodynamics Scopus journals Central Haemodynamics PubMed journals Central Haemodynamics medical journals Central Haemodynamics free journals Central Haemodynamics best journals Central Haemodynamics top journals Central Haemodynamics free medical journals Central Haemodynamics famous journals Central Haemodynamics Google Scholar indexed journals physiology articles physiology Research articles physiology review articles physiology PubMed articles physiology PubMed Central articles physiology 2023 articles physiology 2024 articles physiology Scopus articles physiology impact factor journals physiology Scopus journals physiology PubMed journals physiology medical journals physiology free journals physiology best journals physiology top journals physiology free medical journals physiology famous journals physiology Google Scholar indexed journals Blood pressure articles Blood pressure Research articles Blood pressure review articles Blood pressure PubMed articles Blood pressure PubMed Central articles Blood pressure 2023 articles Blood pressure 2024 articles Blood pressure Scopus articles Blood pressure impact factor journals Blood pressure Scopus journals Blood pressure PubMed journals Blood pressure medical journals Blood pressure free journals Blood pressure best journals Blood pressure top journals Blood pressure free medical journals Blood pressure famous journals Blood pressure Google Scholar indexed journals Hypertension Guidelines articles Hypertension Guidelines Research articles Hypertension Guidelines review articles Hypertension Guidelines PubMed articles Hypertension Guidelines PubMed Central articles Hypertension Guidelines 2023 articles Hypertension Guidelines 2024 articles Hypertension Guidelines Scopus articles Hypertension Guidelines impact factor journals Hypertension Guidelines Scopus journals Hypertension Guidelines PubMed journals Hypertension Guidelines medical journals Hypertension Guidelines free journals Hypertension Guidelines best journals Hypertension Guidelines top journals Hypertension Guidelines free medical journals Hypertension Guidelines famous journals Hypertension Guidelines Google Scholar indexed journals Therapy articles Therapy Research articles Therapy review articles Therapy PubMed articles Therapy PubMed Central articles Therapy 2023 articles Therapy 2024 articles Therapy Scopus articles Therapy impact factor journals Therapy Scopus journals Therapy PubMed journals Therapy medical journals Therapy free journals Therapy best journals Therapy top journals Therapy free medical journals Therapy famous journals Therapy Google Scholar indexed journals Outcomes articles Outcomes Research articles Outcomes review articles Outcomes PubMed articles Outcomes PubMed Central articles Outcomes 2023 articles Outcomes 2024 articles Outcomes Scopus articles Outcomes impact factor journals Outcomes Scopus journals Outcomes PubMed journals Outcomes medical journals Outcomes free journals Outcomes best journals Outcomes top journals Outcomes free medical journals Outcomes famous journals Outcomes Google Scholar indexed journals chronic kidney disease articles chronic kidney disease Research articles chronic kidney disease review articles chronic kidney disease PubMed articles chronic kidney disease PubMed Central articles chronic kidney disease 2023 articles chronic kidney disease 2024 articles chronic kidney disease Scopus articles chronic kidney disease impact factor journals chronic kidney disease Scopus journals chronic kidney disease PubMed journals chronic kidney disease medical journals chronic kidney disease free journals chronic kidney disease best journals chronic kidney disease top journals chronic kidney disease free medical journals chronic kidney disease famous journals chronic kidney disease Google Scholar indexed journals White coat HTN articles White coat HTN Research articles White coat HTN review articles White coat HTN PubMed articles White coat HTN PubMed Central articles White coat HTN 2023 articles White coat HTN 2024 articles White coat HTN Scopus articles White coat HTN impact factor journals White coat HTN Scopus journals White coat HTN PubMed journals White coat HTN medical journals White coat HTN free journals White coat HTN best journals White coat HTN top journals White coat HTN free medical journals White coat HTN famous journals White coat HTN Google Scholar indexed journals Cardiovascular control articles Cardiovascular control Research articles Cardiovascular control review articles Cardiovascular control PubMed articles Cardiovascular control PubMed Central articles Cardiovascular control 2023 articles Cardiovascular control 2024 articles Cardiovascular control Scopus articles Cardiovascular control impact factor journals Cardiovascular control Scopus journals Cardiovascular control PubMed journals Cardiovascular control medical journals Cardiovascular control free journals Cardiovascular control best journals Cardiovascular control top journals Cardiovascular control free medical journals Cardiovascular control famous journals Cardiovascular control Google Scholar indexed journals
Article Details
Key Points
- Hypertension (HTN) is the number one global risk for human death.
- Despite over 20 years of focus with multiple global practice guidelines, public information campaigns, unprecedented spending, and the marketing of a constellation of evolving pharmacotherapies and monitoring technologies, the incidence of hypertension continues to increase and BP control remains <23%
- While central haemodynamics (CH) are essential for understanding the aetiology of HTN and are the physiological targets for therapeutic interventions they are omitted from current guidelines
- This study reviewed recommendations for the diagnosis and treatment of HTN in global guidelines and their relationship to the physiology, pathophysiology of the condition
- Addition of CH to current practice is physiologically rational and may improve precision therapeutic strategies and outcomes in HTN
1. Introduction
Hypertension (HTN) is a circulatory disease characterized by an elevated blood pressure (BP) relative to normative data and is the leading cause of cardiovascular disease and deaths globally accounting for approximately 10.4 million deaths annually [1]. Chronic complications of HTN include coronary artery disease, heart failure, atrial fibrillation, cerebrovascular disease and stroke, peripheral arterial diseases, aortic aneurysm and chronic kidney disease. Worldwide 1.28 billion adults aged 30-79 have HTN with ~46% unaware they have the condition [2]. Approximately 32% of the global adult population have HTN, of whom only around 50% have been diagnosed, with 38-47% of these having been treated, and a mere 18-23% of those diagnosed with HTN have their BP controlled [Figure 1] [3].
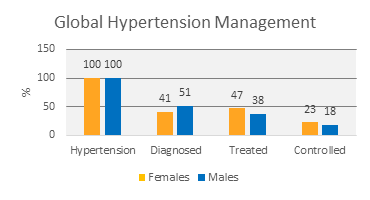
Figure 1: Global gender distinct incidence, diagnosis, treatment and BP control in HTN subjects (100%) defined as ³140/90 and occurring in ~32% of adults worldwide [2,3].
In the US 30-50% of all adults have HTN with less than 50% of these treated, and ~25% treated successfully [4]. While the cost of managing HTN for the US alone in 2018 was $316 billion [5,6], the incidence of HTN and the associated morbidity and mortality continues to increase globally [7,8]. These dismal global outcomes persist despite 20 years of intense focus on improving the clinical care of HTN patients including the promotion of public health programs, publication of multiple global practice guidelines, unprecedented spending, and the marketing of a constellation of evolving pharmacotherapies and BP monitoring technologies. While HTN is commonly a disease of adults, paediatric HTN occurs in ~5% of paediatric patients and is associated with an increasing incidence of cardiovascular symptoms in later life which can be reduced by early BP control [9-11]. The condition is complex and underdiagnosed with a number of unique phenotypes and a lack of consensus on clinical definitions and practice [12,13]. HTN disease in pregnancy (HDP) is a complication of pregnancy occurring in approximately 2-8% of all pregnancies worldwide and responsible for ~16% of global maternal deaths in pregnancy [14] and is the second most common cause of maternal and foetal morbidity and mortality worldwide [15,16] affecting 1 in 7 hospital deliveries [17]. HDP is increasing in incidence despite widespread publicity and substantial public health spending, with women giving birth in 2003 at a 6.7 times the risk of developing severe eclampsia than those giving birth 20 years previously [14]. Additional to these specific applications sub-variants of HTN such as prehypertension and white coat hypertension are clinical entities with specific phenotypes. Prehypertension is a high normal BP, defined as a brachial BP between the 90th and 95th percentile [4], and occurs in 25-50% of adults worldwide [18,19]. White coat HTN (WCHTN) is manifestation of circulatory dysregulation resulting in intermittent HTN associated with clinical BP monitoring and is defined as an elevated office BP on three occasions with normal 24hr or home BP measures in the absence of antihypertensive therapy [19]. Martin and McGrath reported a ~15-45% incidence of WCHTN in untreated HTN patients and an associated 3 fold increased incidence of diabetes and HTN over 10 years. Both Prehypertension and WCHTN are associated with an increased lifetime risk of developing HTN and cardiovascular events and are treated by lifestyle modifications and antihypertensive pharmacotherapy [18,19]. Worldwide HTN is common, dangerous and expensive, occuring in multiple clinical settings with multiple phenotypes. Multiple HTN guidelines have been developed worldwide to steer clinical practice yet outcomes remain poor. This review examined the focus of these guidelines seeking to better understand the challenges and complexities of HTN and identify opportunities that may improve current clinical practice.
1.1 BP, haemodynamics and cardiovascular control
The circulation functions to transport oxygen to the cells, with the blood flowing down pulsing BP gradients generated by the coordinated muscular contraction and relaxation of the heart and vessels. Effective delivery of oxygen to the cells is critical to the function and viability of the cells, organs and ultimately the organism. The precise measurement of this flow is central to understanding and managing the circulation in all cardiovascular diseases including HTN. Cardiovascular control (CVC) is complex and variable in the normal and pathological circulation and is controlled by the neurohormonal systems (NHS). The NHS includes the autonomic nervous system (ANS), including the sympathetic and parasympathetic nervous systems, the renin-angiotensin-aldosterone systems, the cardiac natriuretic peptide system and the vascular endothelium, all mediated by the interplay of baroreceptors, chemoreceptors and thermoreceptors to preserve normal perfusion pressures and flow and optimal homeostasis [20-22]. Dysregulation of any of the multifactorial and interdependent vectors of CVC results in circulatory derangement and potentially high, normal or low BP. While HTN is defined and managed by simple brachial BP target values Guyton demonstrated that BP is the product of cardiac and vascular function [23];
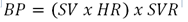
Where BP = blood pressure (mmHg), SV = stroke volume (cm3), HR = heart rate (bpm), SVR = systemic vascular resistance (dynes.s.cm-5).
Therefore, it is axiomatic that HTN, an increased BP, results from elevation of either cardiac or vascular function, or both. The possible haemodynamic computations associated with HTN can be simply conceived as ranging from normal, prehypertensive with normotension and deranged but compensated central haemodynamics (CH), and hypertension of vasogenic, cardiogenic or mixed aetiology (Figure 2).
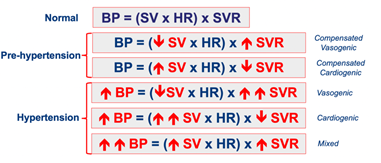
Figure 2: Simplified circulatory models demonstrating the normal circulation and the central haemodynamic derangements of prehypertension and hypertension.
Quantitating CH function is a prerequisite for defining the aetiology of HTN and accurately targeting and guiding therapy.
1.2 Haemodynamics, BP and therapy
Antihypertensive therapies target reduction of elevated CH parameters which reflect cardiovascular dysfunction using the appropriate class of therapy thus potentially reducing BP (Figure 3) [24]. However without quantitative values for SV, HR and SVR choice of preferred therapies and doses remains empirical.
Figure 3: Different therapies and their direct action on CH parameters and the indirect regulatory response of the neurohormonal system (NHS) on cardiac and vascular function. SV = stroke volume (cm3), HR = heart rate (bpm), SVR = systemic vascular resistance (dynes.s.cm-5), CCB = Calcium channel blocker, BB = Beta blocker, ACEI = Angiotensin converting enzyme inhibitor, ARB = Angiotensin-receptor blocker.
Direct and indirect action of therapies on CH is modulated by the neurohormonal system (NHS) thus complicating the choice of and precision of therapeutics. Pathophysiologically the control of elevated CH is achieved by:
- Decreasing the SVR using a vasodilator (ACEI/ARB)
- Reducing preload and thus SV with a diuretic
- Reducing the SV directly using a negative inotrope (CCB)
While this simple therapeutic model is complicated by the compensatory regulation of CVC, quantification of CH is an intuitive and scientific nexus enabling precise choice of therapy and monitoring dose effectiveness (Figure 4) [7,25,26].
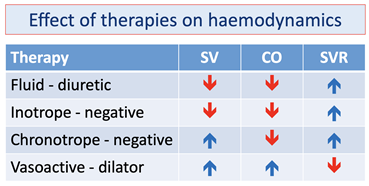
Figure 4: Simplified CH response to different classes of cardiovascular therapies. Directly targeted parameters (red), and compensatory mediated NHS parameters (blue).
The direct and indirect response of CH to different classes of cardiovascular therapy is demonstrated in Figure 3. This simple model demonstrates the potential for non-physiologic treatment to induce iatrogenic complications. For example negative inotropes or diuretics will reduce SV but in vasogenic HTN the baroreceptor driven CVC will increase SVR further preserving or increasing the hypertension. Conversely vasodilation in cases of cardiogenic HTN decreases SVR thus increasing the SV and potentially increasing the HTN. The interaction of therapies and the CVC on the CH determines the post-intervention BP. Smith and Madigan observed that therapeutic non-compliance is common and related to HTN often being asymptomatic and its treatment ineffective [26]. Iatrogenic complications from poly-pharmacotherapies which may have conflicting physiological actions and enhance symptoms may also confuse therapeutic strategies resulting in increased drug-drug interactions, increased adverse events and costs further discouraging patient compliance [27,28].
2. Hypertension guidelines and haemodynamics
While the role of CH in HTN is clear its role in current guidelines is not established. Nine current HTN management guidelines from Australia [29], Canada [30], China [31], Europe [32], Japan [33], Singapore [34], UK [35], US [4] and one International Guideline [36] were selected to represent international geographical practice (Figure 5) and reviewed to evaluate the role of BP and CH parameters.

Figure 5: Global geographical coverage of reviewed hypertension guidelines.
Using proprietary word-count functions the nine guidelines, excluding references, were searched for the keywords , , , ,, , , , , , , and and the instances of BP or CH parameters were tabulated as indicative of the focus of current global guidelines. A total of 478,537 words on 695 pages from the nine international HTN guidelines were analysed. In total BP parameters (BP, SBP, DBP, MAP and blood pressure) were counted 7,535 times (99.4%) while CH parameters (SV, stroke Volume, CO, cardiac output, SVR, VR and vascular resistance) were counted 47 times (0.06%) in total (Table 1, Figure 6). All guidelines recommended BP targeted practice while no guidelines recommended CH target values, while four of the nine guidelines omitted any mention of CH. Despite vasodilators being the recommended first choice therapy for HTN, vascular tone (SVR and vascular resistance) was mentioned in only two guidelines but without target values.
Table 1: Word count of CH and BP parameters in all nine reviewed hypertension guidelines [27-33,4,34] demonstrating a disproportionate omission of CH.
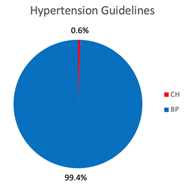
Figure 6: Comparison of references to CH and BP in reviewed global hypertension guidelines [29-35,4,36].
This review of global HTN guidelines confirms uniform recommendation of BP-centric practices in HTN despite <23% of diagnosed and treated subjects achieving effective BP control [3]. While circulatory physiology and the pathophysiology of HTN identifies CH as the scientific targets for pharmacotherapies, CH are overlooked in current guidelines.
3. Effectiveness of BP measurement
While the deficiencies of BP-centric HTN management may be rooted in the non-physiological nature of current concepts, the intrinsic inaccuracy of BP monitoring and examinations may also contribute to its clinical ineffectiveness. For example, despite being ubiquitous in clinical practice, non-invasive automatic office brachial BP (AOBP) measurement taken at the upper arm with an inflatable cuff is only modestly accurate. Kallioinen et al. [37] in a meta-analysis of 328 full text articles identified 29 sources of BP mismeasurement with SBP errors ranging from -23.6mmHg to +33mmHg and DBP errors from -14mmHg to +23mmHg and concluded that “a single BP value outside the expected range should be interpreted with caution and not taken as a definitive indicator of clinical deterioration.” Importantly the majority of reported errors substantially bias toward over-measurement of SBP and DBP and therefore the over-diagnosis of HTN, while only 14-17% of errors led to under-diagnosis. It is universally assumed that commercially available AOBP devices are validated for accuracy, yet Picone et al. [38] in a study of 2,486 devices sold globally found only 10% were validated for accuracy and 73% had no validation at all. The authors concluded that a “Lack of validation may undermine optimal medical practice through increased potential for incorrect hypertension diagnosis and inappropriate care.”
Brachial AOBP devices are validated by comparison of measurements with those from reference standards, or by proof of equivalence against existing validated devices [38]. While high fidelity micromanometer tipped intra-arterial pressure monitoring of the aortic root is the gold standard BP reference [39] the brachial cuff measurement site is 25-35cm separate and characterised by distinct pressure and flow waveforms [40]. Of further complication the flow in the ascending aorta is not laminar but helical with velocity and pressure vortices associated with varying arterial morphology and branching. This makes positioning of the transducer mid-stream in the aortic flow cross-section critical for accurate measurement, particularly as the aorta pulses throughout the cardiac cycle effectively shifting the catheter back and forward across the aortic flow from wall to wall during systole and diastole [41]. Despite invasive validation being the gold standard for validation these sources of error combine to create significant variations between invasive aortic and invasive brachial BP measurements, and invasive aortic and non-invasive brachial values. Nakagami et al. [42] found that invasive aortic SBP was 17.7mmHg greater than non-invasive brachial SBP, and invasive brachial measures of SBP were on average 22.2mmHg greater than non-invasive brachial SBP values. Pelazza and Filho found central aortic catheter transducers measured 3-8% greater values than those measurement by AOBP in the clinically relevant 40 to 80± year olds [43]. In a meta-analysis of 74 studies comparing invasive central aortic BP to brachial AOBP measurements in 3,073 subjects Picone et al. found that on average SBP was under-measured by 5.7mmHg and DBP was over-measured by 5.5mmHg by non-invasive brachial measurement [44]. Critically they calculated that a 5.0mmHg difference in measured BP may result in misdiagnosis of 48M subjects in the US alone and concluded that there was “uncertainty as to whether cuff BP accurately measures intra-arterial BP”. These disagreements between invasive and cuff based brachial measurements, and between invasive central BP measurements and brachial AOBP measurements undermine the reliability of the brachial BP measurement on which HTN guidelines rely.
3.1 Physiologic variability of BP
Further challenging the accuracy of BP measurements is that circulatory physiology and its component measures, BP, SV, CO and SVR are dynamic variables with significantly wide normal ranges and standard deviations between and within subjects. These disparities may reflect normal variability associated with cardiovascular regulation and physiology such as in respiration, excitement and exercise, or pathophysiologic changes [45]. As SBP and DBP are measured non-contemporaneously during cuff deflation, the accuracy of brachial AOBP measurements will be significantly influenced by the stage of the respiratory cycle at which the measurements are taken. Inspiration increases the SBP, DBP, the pulse pressure and the SV, while they decrease during expiration [46] at a rate correlating with the depth of respiration and the intra-thoracic pressure changes [47]. As the resting adult respiratory cycle is 4-8 seconds and a normal cuff inflation and deflation cycle of an AOBP is in the order of 5-10 seconds, the SBP and DBP measurements will be acquired from separate phases of the cardiac cycle, including from the apex and nadir of respiration ensuring maximum inaccuracy and variability of measurements. Normal SV variability is <12% and therefore contributing an additional ±6% physiologic variability to BP measurements assuming the BP measures are exact [48]. AOBP devices measure arterial BP at the level of the upper arm, yet the extremities undergo extreme blood volume redistribution under control of the NHS, particularly in response to changes in ambient temperature [20]. Rowell et al. demonstrated that elevating skin temperature in normal subjects from 37.2°C to 38.7°C resulted in a reduction of total peripheral resistance by 64%, and an accompanying increase in CO of 133% thus confirming a significant dissociation between central and brachial BP during thermoregulation [20]. This redistribution of peripheral blood volume as the NHS adjusts regional vascular resistance limits the effectiveness of brachial AOBP and demonstrates that central BP measurements are a more physiological choice for therapeutic guidance. Roman et al. confirmed that central and brachial BP differed significantly and that “central pulse pressure is more strongly related to vascular hypertrophy, extent of atherosclerosis, and cardiovascular events than is brachial BP” [49]. While Sharman et al. in a randomised controlled trial concluded “guidance of hypertension management with central BP results in a significantly different therapeutic pathway than conventional cuff BP with less use of medication to achieve BP control and no adverse effects…..” [50]. This evidence demonstrates that central and brachial BP are not interchangeable and that the dynamic effect of CVC ensures their dissociation and non-linear relationship. The recent development of non-invasive cuff-based AOBP devices that measure central BP (cBP) and central pulse pressure waveforms potentially addresses this source of error and may contribute to improving the clinical utility of BP measurements. Cheng et al. derived and validated a cBP threshold of 130/90 with optimal cBP of 120/80. (51).
3.2 Atrial fibrillation, hypertension and BP monitoring
Atrial fibrillation (AF) like HTN is positively associated with age occurring in ~25% of subjects aged >55years [52]. HTN is identified as an independent cause for AF with the population attributable risk linking HTN with AF being >20% [52]. Yet brachial AOBP is only valid for subjects with slow and regular AF and measurements averaged from three or more observations, with accuracy diminishing as HR and HR variability increase [53]. So as the incidence and severity of HTN increases with age the effectiveness of AOBP monitoring diminishes secondary to an increased incidence and severity of AF, thus limiting the effectiveness of AOBP in the most vulnerable cohort. Su et al. simply concluded that “more effort is needed to create a new and accurate BP measurement method for AF patients” [53].
3.3 Brachial BP: utility in clinical care
These multiple errors and limitations of brachial AOBP measurement vary within and across subjects, operators and devices, and result in summed errors in clinical measurement of at least ±20% [37,], an error likely to result in significant misclassification of HTN status. International ISO 81060-2:2018(E) guidelines for the clinical investigation of intermittent automated measurement of non-invasive sphygmomanometers recommends equivalence validation values within ±5mmHg with an SD of <8mmHg between AOBP device and manual auscultation for accurate assessment of clinical HTN. Given the preceding technical and physiological findings, this degree of agreement may be unattainable. In addition to brachial BP being a physiologically suboptimal target for monitoring circulatory dysregulation its clinical resolution is inadequate for the implementation of precision therapeutics, both of which may conspire to impair outcomes in HTN.
4. Central haemodynamic monitoring technology
The adoption of CH-led approaches in HTN depends on the availability of a non-invasive technology with clinical resolution more accurate than that of AOBPs. Continuous wave Doppler ultrasound (CW) is well validated with a sensitivity of ±3% in string phantoms [54,55]. An anthropometrically calibrated CW (USCOM 1A, Uscom Ltd, Australia) has been validated from 0.12l/min to 18.7l/min across multiple clinical applications [56-62], is non-invasive, simple to use and interpret, with an examination time of less than five minutes [57] and with age referenced normal CH values from neonates to 87 years [57]. The technology is effective in free breathing and ventilated subjects and those in sinus rhythm and with atrial fibrillation [59], conditions which may confound BP monitoring [53]. The technology generates multiple beat to beat parameters of cardiovascular performance, including SV, CO and SVR [63], and displays values from each stroke or as an average value from a 14 second acquisition, thus limiting the impact of respiratory variation and increasing the reliability of measurements and its sensitivity to change (Figure 7).
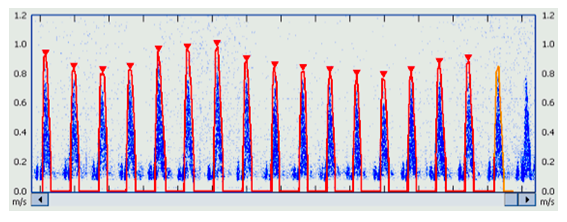
Figure 7: Transaortic Doppler flow profile demonstrating normal respiratory SV variability.
Normal SV variability (SVV) generates an up to 15% BP variability contributing to an increased standard deviation of BP measurements as BP is a direct function of SV. This normal variability is an indication of sensitivity, and is directly measured by averaging multiple CW observations, but not by single oscillometric measures. This variability is further increased in subjects with hypovolemia where SVV may exceed 20%. Elderly subjects with an increased incidence of HTN may also have pre-existing background hypovolemia or may be on therapeutic diuretics for HTN or heart failure and which may increase SVV and BPV making BP measures decreasingly accurate in the elderly cohort with the highest incidence of hypertension. These physiological variations are captured by CW as demonstrated in Figure 6. The averaging of multiple observations reduces the effect of observational variability and increases the sensitivity of comparison measures, the value of which can be predicted using generalizability theory and the number of averaged observations [64]
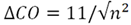
Where DCO = the change in CO detected between consecutive measures, n = number of cycles averaged to create each single measure, and 11 is the single measure sensitivity for detecting change using CW [64].
Plotting this equation demonstrates an exponential curve with increasing sensitivity accompanying increasing observations approaching an asymptote at approximately 10 averaged CO measures (Figure 8). This equation predicts a three fold increase in sensitivity from 11% to 3.3% by averaging 10 consecutive measures with an ~3% sensitivity limit from additional observations beyond 10.
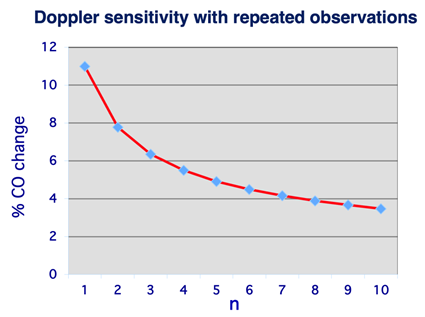
Figure 8: Assuming a sensitivity of 11% between two single repeated CO/SV measures generalizability theory predicts a ~3% sensitivity from 10 averaged CW beats repeated.
Using 10 average measures in vivo sensitivity of ±5% was demonstrated in sheep studies against surgically implanted ultrasonic flow probes over a six-fold range of outputs (1.9L/min to 11.7L/min) varied using inotropes and vasoactives [56]. This high in vivo sensitivity to therapeutic change facilitates the early detection and management of CH enhancing its application in prehypertension (18), dysrhythmias, white-coat HTN (19), pediatric HTN [65] and preeclampsia [62,66]. This 5% sensitivity of CH measurements contrasts with that of brachial AOBP measurements with an estimated sensitivity of 20% at best in subjects in sinus rhythm [37].
5. Strengths and Limitations
While the choices of practice guidelines for this review were discretionary, it was based on geographic and reputational criteria. Additional guidelines may have been included, however the reviewed guidelines were uniform in principle with no recommendations for inclusion of CH, so it is unlikely additional guidelines would have revealed significantly different clinical practices. The assumption that practice guidelines are widely adopted may also be flawed, with current poor HTN outcomes potentially reflecting incomplete adoption of effective practice guidelines rather than ineffective guidelines being widely implemented. The contrary hypothesis that the inclusion of CH-led concepts in current guidelines may improve outcomes may also be flawed and requires clinical evaluation. However the physiological, technical and clinical proposition is compelling and the value of CH-led monitoring in pilot applications such as HDP, paediatric HTN, and adult and paediatric ICU is positive. An option for the effective adoption of CH-led HTN care would require delivery in bespoke hypertensive clinics, with specialised clinicians and technicians combined with an expanded national data archiving and monitoring database. While this would require increased public health spend, even a small improvement in clinical HTN outcomes, particularly in early detection and implementation of precision therapy will offset any costs of establishment.
6. Conclusion
This review identified substantial and increasingly ineffective management of HTN globally despite widespread and detailed clinical guidelines and abundant evolving clinical therapies. These results can be attributed to multiple causes including BP-centric practice recommendations, inaccuracy of BP technologies, the complexity of the underlying pathophysiology, and the inadequacy of examination and monitoring techniques. The physiology and pathophysiology of the hypertensive circulation identified CH parameters as essential for accurate diagnosis and targeting of precision therapy despite their omission from current HTN guidelines. The increased sensitivity of CH monitoring of the circulatory changes of HTN also suggest an increased application in clinical environments in which BP monitoring remains unclear such as prehypertension, dysrhythmias, white-coat HTN, pediatric HTN and preeclampsia. Continuing to manage HTN based on current precepts and in the absence of CH measurements is likely to preserve current clinical outcomes. The addition of CH monitoring to HTN guidelines and treatment algorithms is a physiologically rational next step for the incremental improvement of clinical practice for what is, at least as far as effective therapeutics are concerned, arguably an orphan disease.
Review criteria
For this study nine current HTN management guidelines from Australia [27], Canada [28], China [29], Europe [30], Japan [31], Singapore [32], UK [33], US [4] and one International Guideline [34] were reviewed. Using the Microsoft Word and Adobe word count functions, the nine guidelines, excluding references, were searched for the keywords , , , ,, , , , , , , and and the results tabulated from the 695 pages and 478,537 words searched. HDP guidelines from ACC, AHA, ACOG, ESC and Nice [14,63-65,30], plus one pediatric HTN guideline [13], two sepsis guidelines [75,79] and eight review articles [1,5,7-9,19,26,35] were referenced. This review focused on evaluating the current knowledge in the field of HTN including the contents and recommendations of global guidelines, clinical recommendations and review articles and the clinical effectiveness of HTN management worldwide. Alongside this evidence physiology and pathophysiology was considered and recent relevant clinical science and additions to current guidelines were discussed.
Data availability:
The datasets generated for this study are available on request from the corresponding author
Acknowledgments
Thanks to Malcolm West for his enduring inspiration, support and encouragement. His wisdom is sadly missed.
Author Contributions
- Rob Phillips conceived the study, collected and analysed the data, prepared the manuscript, coordinated collaborators, and revised and approved the final manuscript.
- Stephane Carlier reviewed and analysed the data, collaborated in writing and reviewing the manuscript, and approved the final manuscript.
- Alessandro Scalia reviewed and analysed the data, collaborated in writing and reviewing the manuscript, and approved the final manuscript.
- Philippe Delmotte reviewed and analysed the data, collaborated in writing and reviewing the manuscript, and approved the final manuscript.
- Giles Cattermole reviewed and analysed the data, collaborated in writing and reviewing the manuscript, and approved the final manuscript.
- Joe Brierley reviewed and analysed the data, collaborated in writing and reviewing the manuscript, and approved the final manuscript.
Ethical Approval
This review of public domain peer reviewed publications did not require the acquisition of additional human or animal data.
Competing Interests
Dr Phillips is a shareholder and executive of Uscom Limited, and holds patents in advanced haemodynamic and blood pressure monitoring. He receives no direct benefit from publication of this manuscript.
Dr Carlier has no conflicts of interest to declare.
Dr Scalia has no conflicts of interest to declare.
Dr Delmotte has no conflicts of interest to declare.
Dr Cattermole has no conflicts of interest to declare.
Dr Brierley has no conflicts of interest to declare.
Funding
No financial assistance or re-imbursement of any kind was received by any of the authors to support this study.
References
- Global Burden of Disease Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 392 (2018): 1923-1994.
- World Health Organisation. Hypertension fact sheet. accessed 2nd August 2022
- Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. NCD Risk Factor Collaboration (NCD-RisC). Lancet. 398 (2021): 957-980.
- Whelton PK, Carey RM. 2017 Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Col Cardiol, 71 (2018): 127-248.
- Wierzejska E, Giernas B, Lipiak A, et al. A global perspective on the costs of hypertension: a systematic review. Arch Med Sci, 16 (2020): 1078-1091.
- Elizabeth B Kirkland, Marc Heincelman, Kinfe, G Bishu, et al. Trends in Healthcare Expenditures Among US Adults with Hypertension: National Estimates, 2003-2014. J Am Heart Assoc,7 (2018): e008731
- Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation, 134 (2016): 441-450.
- Non-Communicable Disease Risk Factor Collaboration. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 389 (2017): 37-55
- Song P, Zhang Y, Yu Y, et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr.173 (2019): 1154-1163.
- Urbina EM, Khoury PR, Bazzano L, et al. Relation of blood pressure in childhood to self-reported hypertension in adulthood, (in eng). Hypertension.73 (2019):1224-1230.
- Basalely A, Hill-Horowitz T, Sethna CB. Ambulatory Blood Pressure in Pediatrics, an Update on Interpretation and Classification of Hypertension Phenotypes. Current Hypertension Reports, 25 (2023): 1-11.
- Hamdani G, Mitsenefes MM, Flynn JT, et al. Pediatric and adult ambulatory blood pressure thresholds and blood pressure load as predictors of left ventricular hypertrophy in adolescents. Hypertension. 78 (2021): 30
- Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents, (in eng). Pediatrics. 140 (2017).
- American College of Obstetricians and Gynecologists' Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 133 (2019): e26-e50.
- Hutcheon JA, Lisonkova S, Joseph KS. Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol. 25 (2011): 391-403.
- Aspirin Use to Prevent Preeclampsia and Related Morbidity and Mortality. US Preventive Services Task Force Recommendation Statement. JAMA. 326 (2021): 1186-1191.
- CDC Press Release: Hypertensive disorders in pregnancy affecting 1 in 7 deliveries. US Department of Health and Human Services 2022.
- Egan B, Stevens-Fabry S. Prehypertension—prevalence, health risks, and management strategies. Nat Rev Cardiol,12 (2015): 289-300.
- Martin CA, McGrath BP. White-coat hypertension. Clin Exp Pharmacol Physiol, 41 (2014): 22-29.
- Rowell LB. Human Cardiovascular Control. Oxford University Press, New York, 1993.
- Bader M. Tissue Renin-Angiotensin-Aldosterone Systems: Targets for Pharmacological Therapy. Annual Review Pharmacology Toxicology, 50 (2010): 439-465.
- Goetze JP, Bruneau BG, Ramos HR, et al. Cardiac natriuretic peptides. Nat Rev Cardiol 2020;17 (2020):698-717.
- Guyton AC, Lindsey AW, Kaufmann BN. Effect of mean circulatory filling pressure and other peripheral circulatory factors on cardiac output. Am J Physiol, 180 (1955): 463-468.
- Phillips RA, Ma Z, Kong B, et al. Maternal Hypertension, Advanced Haemodynamics and Therapeutic Precision: Principles and Illustrative Cases. Current Hypertension Reports, 22 (2020): 49.
- Bager JE, Manhem K, Andersson T, et al. Hypertension: Sex-related differences in drug treatment, prevalence and blood pressure control in primary care. 2023 J Human Hypert.
- Smith BE, Madigan VM. Understanding the Haemodynamics of Hypertension. Current Hypertension Report, 20 (2018): 29.
- Neutel JM, Smith DHG. Improving Patient Compliance: A Major Goal in the Management of Hypertension. J Clin Hypertension, 5 (2003):127-132.
- Mukete BN, Ferdinand KC. Polypharmacy in older adults with hypertension: A comprehensive review. J Clin Hypertens, 18 (2016): 10-18.
- National Heart Foundation of Australia. Guidelines for the diagnosis and management of hypertension in adults 2016.
- Rabi DM, et al. Guidelines Hypertension Canada’s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Canadian Journal of Cardiology.36 (2020): 596-624.
- Joint Committee for guideline revision. 2019 Chinese guideline for the management of hypertension in the elderly. J Geriatr Cardiol, 16 (2019): 67-99.
- ESH/ESC - The Task Force for the management of arterial hypertension of ESC and EHS. 2018 ESC/ESH Guidelines for the management of arterial hypertension. European Heart Journal, 39 (2018): 3021-3104.
- The Task Force for the Japanese Society of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertension Research, 42 (2019):1235-1481.
- Tay JC, Sule AA, Chew D, et al. Ministry of Health Clinical Practice Guidelines: Hypertension. Singapore Med J, 59 (2018): 17-27.
- Committee for the Nice Guidelines. Hypertension in adults: diagnosis and management (NG136). accessed 23rd July 2022.
- Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension.75 (2020):1334-1357.
- Kallioinen N, Hill A, Horswill MS, et al. Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings: a systematic review. J Hypertens. 35 (2017): 421-441.
- Piccone DS, Campbell NRC, Schutte AE, et al. Validation Status of Blood Pressure Measuring Devices Sold Globally. JAMA, 327 (2022): 680-681.
- Scalia A, Ghafari C, Navarre W, et al. High Fidelity Pressure Wires Provide Accurate Validation of Non-Invasive Central Blood Pressure and Pulse Wave Velocity Measurements. Biomedicines, 11 (2023): 1235.
- Guyton AC, Hall JE. Textbook of Medical Physiology, Saunders Co, 11th Edition, 2004
- Shahcheraghi N, Dwyer HA, Cheer AY, et al. Unsteady and Three-dimensional Simulation of Blood Flow in the Human Aortic Arch. J Mech Engineering, 124 (2002): 378-387.
- Nakagami A, Okada S, Shoji T, et al. Comparison of invasive and brachial cuff based noninvasive measurements for the assessment of blood pressure amplification. Hypertension Res, 40 (2017): 237-242.
- Pelazza BB, Filho SRF. Comparison between the central and brachial blood pressure values in patients with hypertension undergoing cineangiocoronarography. J Bras Nefrol, 34 (2012): 266-271.
- Picone DS, Shultz MG, Otahal P, et al. Accuracy of Cuff-Based Measurement of Blood Pressure. J Am Coll Cardiol, 70 (2017): 572-586.
- Dornhorst AC, Howard P, Leathart GL. Respiratory Variations in Blood Pressure. Circulation, 6 (1952): 553-558.
- Parati G, Stergiou GS, Dolan E, et al. Blood pressure variability: clinical relevance and application. J Clin Hypertens. 20 (2018): 1133-1137.
- Herakova N, Nwobodo NHN, Wang Y, et al. Effects of respiratory pattern on automated clinical blood pressure measurements: an observational study with normotensive subjects. Clinical Hypertension, 23 (2017): 15
- Teboul JL, Monnet X, Chemia D, Michard F. Arterial Pulse Pressure Variation with Mechanical Ventilation. Am J Resp Crit Care Med, 199 (2018): 22-31.
- Roman M, Devereaux RB, Kizer JR, et al. Central Pressure More Strongly Relates to Vascular Disease and Outcomes Than Does Brachial Pressure: The Strong Heart Study. Hypertension, 50 (2007): 197-203.
- Sharman JE, Marwick TH, Gilroy D, et al. Randomized Trial of Guiding Hypertension Management Using Central Aortic Blood Pressure Compared With Best-Practice Care; Principal Findings of the BP GUIDE Study. Hypertension, 62 (2013): 1138-1145.
- Cheng HM, Chuang SY, Sung SH, et al. Derivation and validation of diagnostic thresholds for central blood pressure measurements based on long-term cardiovascular risks. J Am Coll Cardiol. 62 (2013): 1780-1787.
- Elliott A.D., Middeldorp M.E., Van Gelder I.C. et al. Epidemiology and modifiable risk factors for atrial fibrillation. Nat Rev Cardiol 2023.
- Su, H., Guo, Z. Accuracy of non-invasive blood pressure measurement in patients with atrial fibrillation. J Hum Hypertens, 36 (2022): 229-234.
- Walker AR, Phillips DJ, Powers JE. Evaluating Doppler devices using a moving string test target. J Clin Ultrasound, 10 (1982): 25-30.
- Phillips DJ, Hossack J, Beach KW, et al. Testing ultrasonic pulsed Doppler instruments with a physiologic string phantom. J Ultrasound Med, 9 (1990): 429-436.
- Phillips RA, Hood SG, Jacobson BM, et al. Pulmonary artery catheter (PAC) accuracy and efficacy compared with flow probe and transcutaneous Doppler (USCOM): An ovine validation. Crit Care Res Prac 2012.
- Cattermole GN, Leung PYM, Ho GYL, et al. The normal ranges of cardiovascular parameters measured using the ultrasonic cardiac output monitor. Physiol Rep, 5 (2017): e13195.
- Deep A, Goonasekera CDA, Wang Y, et al. Evolution of haemodynamics and outcome of fluid refractory septic shock in children. Int Care Med, 39 (2013):1602-1609.
- Thiel SW, Kollef MH, Isakow W. Non-invasive stroke volume measurement and passive leg raising predict volume responsiveness in medical ICU patients: an observational cohort study. Critical Care, 39 (2009): 666-688.
- Siu CW, Tse HF, Lee K, et al. Cardiac Resynchronization Therapy Optimization by Ultrasonic Cardiac Output Monitoring (USCOM) Device. Pacing and Clinical Electrophysiology (PACE). 30 (2007): 50-55.
- He SR, Sun X, Zhang C, et al. Measurement of systemic oxygen delivery and inotropy in healthy term neonates with the Ultrasonic Cardiac Output Monitor (USCOM). Early Hum Dev, 89 (2013): 289-294.
- Vinayagam D, Patey O, Thilaganathan B, et al. Cardiac output assessment in pregnancy: comparison of two automated monitors with echocardiography. Ultrasound in Obs and Gynae. 49 (2017): 32-38
- Phillips RA, Smith BE, Madigan VM. Stroke Volume Monitoring: Novel Continuous Wave Doppler Parameters, Algorithms and Advanced Noninvasive Haemodynamic Concepts. Curr Anesthesiol Rep. (2017): 387-398.
- Kusumoto F, Venet T, Schiller NB, et al. Measurement of Aortic Blood Flow by Doppler Echocardiography: Temporal, Technician and Reader Variability in Normal Subjects and the Application of Generalizability Theory in Clinical Research. J Am Soc Echocardiogr, 8 (1995): 647-653
- Brierley J, Marks SD. Treating the causes of paediatric hypertension using non-invasive physiologic parameters. Medical Hypotheses, 75 (2010) :439-441.
- Gongora MC, Sharma G, Yang E. Hypertension During Pregnancy and After Delivery: Management, Cardiovascular Outcomes and Future Directions. 2018.
