Global Association of Obesity and COVID-19 Death Rates
Article Information
Mary Adams*
On Target Health Data LLC, Hartford, CT, 06093, USA
*Corresponding Author: Mary Adams. On Target Health Data LLC, Hartford, CT, 06093, USA
Received: 13 September 2022; Accepted: 19 September 2022; Published: 26 September 2022
Citation: Mary Adams. Global Association of Obesity and COVID-19 Death Rates. Journal of Food Science and Nutrition Research 5 (2022): 664-668.
View / Download Pdf Share at FacebookAbstract
COVID-19 was responsible for an enormous global death toll with large variation among countries, and obesity noted in many studies as a key risk for complications. This study was conducted to estimate the contribution of obesity to COVID deaths prior to vaccine distribution by measuring associations between obesity rates and COVID deaths/million population through 2/25/2021.
Methods: Using Excel, COVID deaths/million for 167 countries grouped by population size, continent or obesity rate were regressed separately on their obesity rate in 2016. Using the least squares formula for the best fit for each model, components of the formula, R2, and the percentage of world population represented, were documented for each group.
Results: Obesity rates ranged from 2.1% to 37.9% and death rates ranged from 0.4/million to 1,892/million. Results for groups ranked by population and for Asia and Africa had R2 from 0.30 to 0.90 with slopes of the fitted line ranging from 11.1-51.0. Countries with obesity rates <15% all had death rates ≤233/million, R2 of 0.003, and slope of the line=1.01.
Conclusions: For most countries, ≥ 30% of the difference in COVID death rates was explained by obesity rates, while in countries with obesity <15% (all in Asia or Africa), consistently low death rates were not associated with obesity. Differences in obesity rates are likely related to diet and exercise while death rates can be affected by many factors. Reduced obesity rates especially below 15% could potentially have lowered the COVID death
Keywords
COVID-19, Obesity, COVID deaths, Asia, Africa
COVID-19 articles; Obesity articles; COVID deaths articles; Asia articles; Africa articles
COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Obesity articles Obesity Research articles Obesity review articles Obesity PubMed articles Obesity PubMed Central articles Obesity 2023 articles Obesity 2024 articles Obesity Scopus articles Obesity impact factor journals Obesity Scopus journals Obesity PubMed journals Obesity medical journals Obesity free journals Obesity best journals Obesity top journals Obesity free medical journals Obesity famous journals Obesity Google Scholar indexed journals COVID deaths articles COVID deaths Research articles COVID deaths review articles COVID deaths PubMed articles COVID deaths PubMed Central articles COVID deaths 2023 articles COVID deaths 2024 articles COVID deaths Scopus articles COVID deaths impact factor journals COVID deaths Scopus journals COVID deaths PubMed journals COVID deaths medical journals COVID deaths free journals COVID deaths best journals COVID deaths top journals COVID deaths free medical journals COVID deaths famous journals COVID deaths Google Scholar indexed journals Asia articles Asia Research articles Asia review articles Asia PubMed articles Asia PubMed Central articles Asia 2023 articles Asia 2024 articles Asia Scopus articles Asia impact factor journals Asia Scopus journals Asia PubMed journals Asia medical journals Asia free journals Asia best journals Asia top journals Asia free medical journals Asia famous journals Asia Google Scholar indexed journals Africa articles Africa Research articles Africa review articles Africa PubMed articles Africa PubMed Central articles Africa 2023 articles Africa 2024 articles Africa Scopus articles Africa impact factor journals Africa Scopus journals Africa PubMed journals Africa medical journals Africa free journals Africa best journals Africa top journals Africa free medical journals Africa famous journals Africa Google Scholar indexed journals death rate articles death rate Research articles death rate review articles death rate PubMed articles death rate PubMed Central articles death rate 2023 articles death rate 2024 articles death rate Scopus articles death rate impact factor journals death rate Scopus journals death rate PubMed journals death rate medical journals death rate free journals death rate best journals death rate top journals death rate free medical journals death rate famous journals death rate Google Scholar indexed journals US adults articles US adults Research articles US adults review articles US adults PubMed articles US adults PubMed Central articles US adults 2023 articles US adults 2024 articles US adults Scopus articles US adults impact factor journals US adults Scopus journals US adults PubMed journals US adults medical journals US adults free journals US adults best journals US adults top journals US adults free medical journals US adults famous journals US adults Google Scholar indexed journals world population articles world population Research articles world population review articles world population PubMed articles world population PubMed Central articles world population 2023 articles world population 2024 articles world population Scopus articles world population impact factor journals world population Scopus journals world population PubMed journals world population medical journals world population free journals world population best journals world population top journals world population free medical journals world population famous journals world population Google Scholar indexed journals
Article Details
Introduction
Globally, the COVID-19 death toll through February 25. 2021 (before vaccines were widely available) was over 2.5 million worldwide with death rates ranging from 0.4/million population in Viet Nam to 1,892/million in Belgium [1]. The reason for such wide variation is still not well understood but there are some clues. Early in the pandemic, it was noted that people who reported certain underlying health conditions were more likely to be hospitalized and die from COVID-19 [2]. Initial US estimates of those likely to develop complications or die from COVID were based on data from China where the pandemic started and where obesity rates are low. Data from the US found that adults with obesity, hypertension, chronic lung disease, diabetes, and cardiovascular disease were disproportionately hospitalized with COVID-19 [3]. Based on those results, estimates of US adults with underlying conditions increasing risk of complications from COVID were made finding that an estimated 56% of US adults had one or more of the conditions listed above [4]. Including obesity along with chronic diseases as a condition related to COVID deaths appears to blur the usual distinction between chronic and infectious diseases and suggested potential studies. Figure 1 [5] indicates the relationship between most of the separate underlying conditions and risk factors for obesity which include diet and physical inactivity. The objective for this study was to analyze the association of obesity with death rates to estimate the contribution of obesity to the variation in COVID death rates among countries.
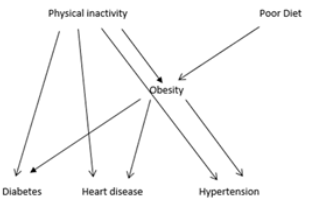
Figure 1:
Methods
COVID death rates through February 25, 2021 (prior to the wide distribution of vaccines) [1] and obesity rates in 2016 [6] for 167 countries for which data were available for both obesity and deaths were included in the study. Countries were grouped by population size into multiples of 10 countries in each of 8 groups, which included 90.9% of the world population. Results were compared with 57 countries with obesity rates <15% which were also included in the relevant population groups. Using Excel, equations for linear least squares trend lines and estimates of the coefficient of determination (R2) were made from regression of COVID deaths/million population on obesity rates for each group. A subset of the 100 most populous countries were similarly analyzed by continent with 26 in Asia, 33 in Africa, and 41 in the rest of the world.
Results
Obesity rates across the 167 countries ranged from 2.1% in Viet Nam to 37.9% in Kuwait. Death rates ranged from 0.4/million in Viet Nam to 1,892/million in Belgium. Figure 2 shows the graph with trendline and data points, with R2 of 0.356, and formula for the line for the 60 most populous countries representing 87.6% of the world population. The US is represented by the point @ 1562 deaths/million at obesity rate of 36.2%. This figure is typical for the 8 graphs based on population but with varying R2. Results for the 57 countries with obesity rates <15% had R2=0.0033, a slope=1.01 and a constant term of +33; all death rates were ≤233/million and most were below 100/million. Results are summarized in table 1.
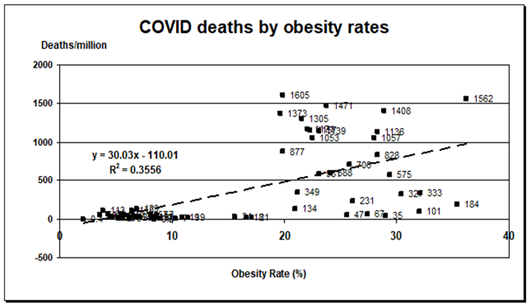
Figure 2: Graph of COVID-19 deaths through 2/25/2021 by 2016 obesity rates for the 60 most populous countries with data for both. Formula and R2 for least squares fit line from regression in Excel.
Table 1: Summary of results for association between obesity and COVID death rates/million, adding countries to each group in order of highest population or top 100 sorted by continent.
|
|
|
Fitted equation |
|
|
|
Number in group |
R2 |
Slope |
+/- |
% Total pop |
|
10 |
0.905 |
51 |
-263.2 |
58 |
|
20 |
0.539 |
34.1 |
-111.6 |
70.5 |
|
30 |
0.494 |
37.2 |
-107 |
76.6 |
|
40 |
0.351 |
30 |
-47.5 |
81.3 |
|
50 |
0.322 |
28.5 |
-92 |
85 |
|
60 (Figure 2) |
0.356 |
30 |
-110 |
87.6 |
|
70 |
0.356 |
29.5 |
-116 |
89.5 |
|
80 |
0.304 |
27.9 |
-94.8 |
90.9 |
|
167 |
0.203 |
26.4 |
-62.6 |
~100 |
|
Obesity <15% (n=57) |
0.003 |
1.01 |
33 |
65.6 |
|
Top 100 in population |
||||
|
Africa (n=33) |
0.437 |
14 |
-66.7 |
16.8 |
|
Asia (n=26) |
0.393 |
11.1 |
-12.7 |
56.3 |
|
Rest (n=41) obesity ≥19.5% |
0.0004 |
3 |
798 |
22.1 |
When the data for the top 100 countries were broken down for analysis by continent, only Africa and Asia included countries with obesity rates < 15% and the R2 for those continents were 0.44 and 0.39 respectively (Table 1). The 41 countries outside Africa and Asia all had obesity rates ≥19.5% and analyzed together had R2 = 0.0004. Slopes for these areas were 14 for Africa, 11 for Asia and 3 for the rest of the world. The constant terms were -67, -13 and +798 respectively (Table 1).
Discussion
Results do not fully answer the question of how much of the difference in death rates is due to obesity, but they should make quite clear that obesity matters. Except for regression analysis limited to countries with low or high obesity rates, most results indicate that obesity explains one-third or more of the difference in death rates between countries, with R2 ranging as high as 0.91 for the group including 58% of the world population. Data from separate continents adds more information. In Africa and Asia which include all countries with obesity <15%, results suggest that 39-40% of the difference in COVID death rates can be explained by obesity rates but the slopes are lower than when all countries are included. This suggests that in Africa and Asia, death rates associated with a particular obesity rate are lower than they are when all countries are included in the model. The similarity in results for these 2 continents may reflect similarities in diet, culture, lifestyle, economy, or other factors and the difference between results for these 2 continents and those including all continents may reflect differences in these same measures.
Regression results for the 57 countries with obesity rates <15%, and the 41 countries outside Asia and Africa with obesity rate all above 19.5% had R2 of 0.003 and 0.0004 respectively, indicating little or no association between country death rates and obesity. Slopes of the fitted lines of 1.0 and 3.0 respectively indicate that increasing obesity rates between the range of values of 0 to 15% for the <15% equation and 19.5%-36.2% for the equation for the 41 countries outside Asia and Africa will have little effect on death rates. In the latter case the equation indicates that all death rates for these countries will be at least 798/million. These results suggest that any studies of the association of obesity and death rates that do not include countries with both low (only from Asia or Africa) and high obesity rates may not accurately estimate the impact of obesity.
Estimates made at both ends of the obesity spectrum using the figures provided in table 1 offer even more insight. Estimating the expected death rate for the US with obesity rate of 36.2 from the formula in figure 2 would estimate 976 COVID deaths/million. Using the formula from the 41 countries of 100 not in Asia or Africa the estimated death rate=907/million ((3 X 36.2) +798). Both estimates underestimate the actual value of 1,562 deaths/million by a large percentage. This suggests that other factors not measured in this study such as how the pandemic was handled, the age structure of the population and access to health care might help explain the discrepancy with actual death rates. Using Kenya with an obesity rate of 7.1% and regression equation figures in table 1 for either Africa, countries with <15% obesity, or the figure 2 formula yields estimates of 32.7, 40.2, and 103 deaths/million respectively. With an actual death rate of 34.0/million, the first 2 estimates are close to actual, while the one based on figure 2 is off by a factor of about 3. Thus, it appears that the formula in figure 2 is good for countries with higher obesity rates, but for obesity rates ≤15% it might be best to use the formula obtained from those data. It is unclear why the regression results for Asia and Africa would be quite similar to each other but different from the rest of the world with lower slopes and constants. It may relate to diet, lifestyle, and economy as mentioned earlier, and being the only regions with any obesity rates <15%. This might warrant more investigation to determine what factors likely related to diet and exercise produce obesity rates consistently under 15%. These results also suggest that estimates of how much COVID deaths might be reduced by lowering obesity rates will likely be more accurate at lower obesity rates. And any country with an obesity rate above 15% that reduced its obesity rate below 15% could almost certainly have reduced its COVID death rate to <200/million at that point in the pandemic.
It should also be noted that these figures and any estimates only apply for the time-period used in this study which pre-dated the wide use of vaccines. A US study has shown that from 4/19/2021 -2/28/2022 when vaccines were assumed to be available, vaccines had the greatest impact on state death rates among three factors: state COVID vaccination rates, a measure including the 6 underlying conditions [3,4] and states grouped by how they voted in the 2016 presidential election. The latter alone explained 60% of the difference in state death rates [9] or nearly double the apparent effect of obesity alone in this current study. The R2 just for vaccines in that US study [9] was 0.46 for comparison.
These results are consistent with data on hospitalizations and deaths from COVID-19 in the US [3] and worldwide [7]. Not only is obesity one of 6 underlying conditions increasing risk of COVID hospitalizations [3], it is also a known risk factor for 4 others: asthma, cardiovascular disease, diabetes, and hypertension [5,8] so high rates of obesity are also associated with more of these other conditions. Further evidence of the role of obesity in COVID-19 deaths comes from the World Obesity Federation (WOF), which found that in countries with overweight rates >50%, the death rate from COVID was about 10 times that in countries where overweight was <50% [10]. Results showed a nearly flat line for deaths vs. overweight rates for countries with overweight <50%, with the slope rising dramatically above 50%, akin to the findings in this study for obesity. The WOF found that countries with less active populations who consumed higher amounts of animal fats, vegetable oils, sugars, and sugar-sweetened beverages were also more likely to have higher death rates from COVID-19 [10]. A study of 30 industrialized nations [11] found that a regression model including obesity, population density, the age structure of the population, population health, GDP, ethnic diversity, and how the pandemic was handled explained 63% of the difference in COVID death rates between countries. While the results don’t indicate what fraction of the 63% is due to obesity, those results are like those referenced above [9] and not inconsistent with the R2 values found in this current study.
Lowering the obesity rate in countries where it is >15% could potentially reduce deaths from COVID-19, a future pandemic, and from many chronic diseases [8]. At least in the US, this would not be easy as obesity rates are currently increasing [12], but as recently as 1990 the US obesity rate was 11.5% and overweight rate was 44.5% [13]. These are both in the range where COVID death rates are very low as shown in these results and by the WOF [10] and suggest those rates might be attainable again with successful behavior change [14]. Other factors that might contribute to the COVID death rate such as racial, ethnic, and age differences, and health care capacity and quality, would likely be at least as difficult to change and appear not to have much effect in countries with obesity rates <15%. Results from the WOF [10] implicating diets high in animal fats, vegetable oils, sugars, and sugar-sweetened beverages in raising obesity rates might be a good place to start with interventions. Also, results for some countries (e.g. the US) showing that the estimated death rate is much lower than actual, suggests that other factors should be considered as targets for interventions. Handling of the pandemic until vaccines can be developed and distributed is likely a key factor. Study results also raise questions: Is there something special about obesity rates <15%? Why are there so few countries with obesity rates between 10% and 15%? What is unique about Asia and Africa that leads to generally lower obesity and COVID death rates on those continents?
Limitations
There are several limitations to this study. Quality of the data for different countries may vary in how it was collected and what standards were used. Other factors may affect death rates including quality of the healthcare system, access to care, racial and ethnic disparities that lead to differences in developing COVID, presence of other underlying conditions in the population (including heart disease, hypertension, diabetes, and those not listed such as smoking), how the pandemic was handled in each country, legislative mandates, mask wearing practices, and geographic and cultural differences that might affect transmission. However, those factors do not appear to appreciably affect death rates among counties with obesity rates <15%.
Conclusions
For most of the world, approximately one-third or more of the variation in COVID-19 death rates among countries can be explained by obesity rates. By contrast, for 57 countries in Asia and Africa with obesity rates <15%, death rates are low and only slightly associated with obesity based on an R2=0.003. The 41 countries in the top 100 countries by population outside Asia & Africa that all have obesity rates >19.5% also have a low R2, this time=0.0004. These results suggest that any studies that exclude Africa and Asia (and thus obesity rates < 15%) from studies of COVID deaths may lead to erroneous conclusions. For countries with obesity rates >15%, COVID-19 deaths could have potentially been reduced considerably with lower obesity rates while more study is needed to understand other factors that might be involved. Although it is likely too late for COVID-19, prioritizing reducing obesity rates could lower deaths from future pandemics which are also expected to be associated with obesity [10]. In the meantime, lowering obesity rates should reduce morbidity and mortality from chronic conditions for which obesity is a known risk factor [8,14]. Diet and exercise are key factors to target in reducing obesity rates [8,10,14].
Declarations
No funding was received for this study.
The author declares no conflicts of interest.
References
- COVID-19 Coronavirus Pandemic (2021).
- Ortiz PE, Simbaña RK, Gómez BL, et al. Clinical, molecular, and epidemiological characterization of the SARS-CoV-2 virus and the Coronavirus Disease 2019 (COVID-19), a comprehensive literature review. Diagn Microbiol Infect Dis 98 (2020): 115094.
- Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019-COVID-NET. MMWR Morb Mortal Wkly Rep 69 (2020): 458-464.
- Adams ML, Katz DL, Grandpre J. Updated estimates of chronic conditions affecting risk for complications from coronavirus disease, United States. Emerg Infect Dis 11 (2020): 56-69
- Adams ML. Accounting for the Origins and Toll of COVID 19 The key role of Overweight in COVID-19. Am J Health Promot 36 (2020): 385-387.
- Central Intelligence Agency. The World Factbook. Country comparison: obesity - adult prevalence rate 2016 (2021).
- Popkin BM, Du S, Green WD, et al. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes Rev 21 (2020): e13128.
- Adams M, Grandpre J, Katz D, Shenson D. The impact of key modifiable risk factors on leading chronic conditions. Prev Med 120 (2019): 113-118.
- Adams M. Implications of red state/blue state differences in COVID-19 death rates. Preprint at Medrxiv.org posted 4/10/2022.
- COVID-19 and Obesity. The 2021 Atlas. World Obesity Federation, London. UK, (2021).
- Gardiner J, Oben J, Sutcliffe A. Obesity as a driver of international differences in COVID-19 death rates. Diabetes Obes Metab 21 (2021): 41-52
- Pernenkil V, Wyatt T, Akinyemiju T. Trends in smoking and obesity among US adults before, during, and after the great recession and Affordable Care Act roll-out 102 (2017): 86-92.
- Behavioral Risk Factor Surveillance System (BRFSS) (Atlanta, Georgia). Centers for Disease Control and Prevention. 1990 Survey Data and Documentation. CDC - BRFSS 1990 Survey Data and Documentation (2021).
- Brownson RC, Remington PL, Wegner, MV. Chronic Disease Epidemiology and Control. (4th edtn), Washington, DC: American Public Health Association (2016).
