Future Perspectives: A Review of Therapeutic Advances in Recurrent Glioblastoma
Article Information
Ulrich Baumgartner1, 2, 3, Rochelle C J D'Souza1, Carolin Offenhäuser1, Seçkin Akgül1, 4 and Bryan W Day1, 2, 3*
1Cell and Molecular Biology Department, QIMR Berghofer Medical Research Institute, Sid Faithfull Brain Cancer Laboratory, Brisbane, QLD 4006, Australia
2School of Biomedical Sciences, The University of Queensland, Brisbane 4072, Australia
3School of Biomedical Sciences, Faculty of Health, Queensland University of Technology, Brisbane 4059, Australia
4School of Medicine, Griffith University, Gold Coast 4215, QLD, Australia
*Corresponding Author: Bryan W Day, Department of Cell and Molecular Biology, QIMR Berghofer Medical Research Institute, Sid Faithfull Brain Cancer Laboratory, School of Biomedical Sciences, The University of Queensland, Brisbane 4072, Australia, Tel: +61-7-3845-3885
Received: 06 April 2021; Accepted: 30 May 2021; Published: 10 June 2021
Citation:
Ulrich Baumgartner, Rochelle C J DSouza, Carolin Offenhauser, Seckin Akgul, Bryan W Day. Future Perspectives: A Review of Therapeutic Advances in Recurrent Glioblastoma. Journal of Cancer Science and Clinical Therapeutics 5 (2021): 286-308.
View / Download Pdf Share at FacebookAbstract
The outcomes for glioblastoma (GBM) patients remain dismal despite significant increases in our understanding of treatment-naïve disease biology and increased focus on clinical trials. Almost all patients experience disease recurrence. If we hope to develop more durable responses in this aggressive disease cohort, a better understanding of resistance mechanisms and drivers of GBM tumour recurrence will be needed. Here we review the findings to-date of current advances in therapeutic development and biology of recurrent GBM, highlighting recent research and clinical trials breakthroughs.
Keywords
<p>Glioblastoma; Recurrence; Tumour evolution; Blood brain barrier; Cancer stem cells; Tumour heterogeneity; Immune therapy</p>
Glioblastoma articles; Recurrence articles; Tumour evolution articles; Blood brain barrier articles; Cancer stem cells articles; Tumour heterogeneity articles; Immune therapy articles.
Glioblastoma articles Glioblastoma Research articles Glioblastoma review articles Glioblastoma PubMed articles Glioblastoma PubMed Central articles Glioblastoma 2023 articles Glioblastoma 2024 articles Glioblastoma Scopus articles Glioblastoma impact factor journals Glioblastoma Scopus journals Glioblastoma PubMed journals Glioblastoma medical journals Glioblastoma free journals Glioblastoma best journals Glioblastoma top journals Glioblastoma free medical journals Glioblastoma famous journals Glioblastoma Google Scholar indexed journals Recurrence articles Recurrence Research articles Recurrence review articles Recurrence PubMed articles Recurrence PubMed Central articles Recurrence 2023 articles Recurrence 2024 articles Recurrence Scopus articles Recurrence impact factor journals Recurrence Scopus journals Recurrence PubMed journals Recurrence medical journals Recurrence free journals Recurrence best journals Recurrence top journals Recurrence free medical journals Recurrence famous journals Recurrence Google Scholar indexed journals Tumour evolution articles Tumour evolution Research articles Tumour evolution review articles Tumour evolution PubMed articles Tumour evolution PubMed Central articles Tumour evolution 2023 articles Tumour evolution 2024 articles Tumour evolution Scopus articles Tumour evolution impact factor journals Tumour evolution Scopus journals Tumour evolution PubMed journals Tumour evolution medical journals Tumour evolution free journals Tumour evolution best journals Tumour evolution top journals Tumour evolution free medical journals Tumour evolution famous journals Tumour evolution Google Scholar indexed journals Blood brain barrier articles Blood brain barrier Research articles Blood brain barrier review articles Blood brain barrier PubMed articles Blood brain barrier PubMed Central articles Blood brain barrier 2023 articles Blood brain barrier 2024 articles Blood brain barrier Scopus articles Blood brain barrier impact factor journals Blood brain barrier Scopus journals Blood brain barrier PubMed journals Blood brain barrier medical journals Blood brain barrier free journals Blood brain barrier best journals Blood brain barrier top journals Blood brain barrier free medical journals Blood brain barrier famous journals Blood brain barrier Google Scholar indexed journals Cancer stem cells articles Cancer stem cells Research articles Cancer stem cells review articles Cancer stem cells PubMed articles Cancer stem cells PubMed Central articles Cancer stem cells 2023 articles Cancer stem cells 2024 articles Cancer stem cells Scopus articles Cancer stem cells impact factor journals Cancer stem cells Scopus journals Cancer stem cells PubMed journals Cancer stem cells medical journals Cancer stem cells free journals Cancer stem cells best journals Cancer stem cells top journals Cancer stem cells free medical journals Cancer stem cells famous journals Cancer stem cells Google Scholar indexed journals Tumour heterogeneity articles Tumour heterogeneity Research articles Tumour heterogeneity review articles Tumour heterogeneity PubMed articles Tumour heterogeneity PubMed Central articles Tumour heterogeneity 2023 articles Tumour heterogeneity 2024 articles Tumour heterogeneity Scopus articles Tumour heterogeneity impact factor journals Tumour heterogeneity Scopus journals Tumour heterogeneity PubMed journals Tumour heterogeneity medical journals Tumour heterogeneity free journals Tumour heterogeneity best journals Tumour heterogeneity top journals Tumour heterogeneity free medical journals Tumour heterogeneity famous journals Tumour heterogeneity Google Scholar indexed journals Immune therapy articles Immune therapy Research articles Immune therapy review articles Immune therapy PubMed articles Immune therapy PubMed Central articles Immune therapy 2023 articles Immune therapy 2024 articles Immune therapy Scopus articles Immune therapy impact factor journals Immune therapy Scopus journals Immune therapy PubMed journals Immune therapy medical journals Immune therapy free journals Immune therapy best journals Immune therapy top journals Immune therapy free medical journals Immune therapy famous journals Immune therapy Google Scholar indexed journals temozolomide articles temozolomide Research articles temozolomide review articles temozolomide PubMed articles temozolomide PubMed Central articles temozolomide 2023 articles temozolomide 2024 articles temozolomide Scopus articles temozolomide impact factor journals temozolomide Scopus journals temozolomide PubMed journals temozolomide medical journals temozolomide free journals temozolomide best journals temozolomide top journals temozolomide free medical journals temozolomide famous journals temozolomide Google Scholar indexed journals heterogeneous tumours articles heterogeneous tumours Research articles heterogeneous tumours review articles heterogeneous tumours PubMed articles heterogeneous tumours PubMed Central articles heterogeneous tumours 2023 articles heterogeneous tumours 2024 articles heterogeneous tumours Scopus articles heterogeneous tumours impact factor journals heterogeneous tumours Scopus journals heterogeneous tumours PubMed journals heterogeneous tumours medical journals heterogeneous tumours free journals heterogeneous tumours best journals heterogeneous tumours top journals heterogeneous tumours free medical journals heterogeneous tumours famous journals heterogeneous tumours Google Scholar indexed journals trials breakthroughs articles trials breakthroughs Research articles trials breakthroughs review articles trials breakthroughs PubMed articles trials breakthroughs PubMed Central articles trials breakthroughs 2023 articles trials breakthroughs 2024 articles trials breakthroughs Scopus articles trials breakthroughs impact factor journals trials breakthroughs Scopus journals trials breakthroughs PubMed journals trials breakthroughs medical journals trials breakthroughs free journals trials breakthroughs best journals trials breakthroughs top journals trials breakthroughs free medical journals trials breakthroughs famous journals trials breakthroughs Google Scholar indexed journals
Article Details
1. Introduction
Glioblastoma (GBM) is the most common and aggressive form of adult brain cancer. Prognosis is very poor with the majority of patients experiencing tumour recurrence within two years of diagnosis. The current standards of care add minimal survival benefit and include surgery followed by adjuvant radiotherapy and temozolomide (TMZ) chemotherapy [1]. It is now established that GBMs are highly heterogeneous tumours comprising significant numbers of cancer cells that reside in dynamic molecular cell states [2-4]. Among this cellular milieu, lie cancer cells with the ability to evade current therapies either through senescence, DNA repair mechanisms or inherent stem cell-like characteristics [5]. In addition, these brain cancer cells are typically highly invasive and migratory making complete resection practically impossible. Adding complexity, is the fact that radiation and chemotherapy add significant therapy-induced genetic alterations, ultimately increasing the aggressiveness of brain cancer cells and altering tumour evolution at recurrence [6]. During the past 30 years the neuro-oncology research community has largely focused their research efforts on understanding treatment naïve disease. This has left a knowledge gap with respect to resistance mechanism and drivers of GBM tumour recurrence. Recent efforts have sought to close this gap and increase our understanding of the biology of recurrent disease [7-9], better define resistance mechanisms [10] and develop and test new therapeutic approaches to treat this aggressive disease [11-13].
Historically, one of the biggest obstacles which has prevented clinical progress in the neuro-oncology field has been the blood brain barrier (BBB). The BBB works via endothelial cells restricting the passage of both small and large molecules into the brain [14]. This normal neuro-protective mechanism significantly reduces the ingress of almost all molecular and antibody-based therapeutics. Unfortunately, the majority of clinical trials to-date, both in upfront and recurrent disease, have relied largely on systemic routes of administration. This has meant, in most cases, that these trials were destined to fail. In rapidly growing solid tumours such as GBM, vascular hyper-proliferation is common and consequently blood vessel formation is not always tightly regulated [15]. Evidence also exists that tumour cells with stem cell-like properties can differentiate into tumour-derived pericytes and endothelial cells [16]. These abnormal processes lead to the formation of large irregular, often oedematous, blood vessels within recurrent tumours with compromised BBB dynamics. This so-named blood tumour barrier (BTB) may add benefit for therapeutic penetrance in the recurrent setting, although this is a topic of debate [17]. Alternate surgical approaches such as convection-enhanced delivery (CED) rely on intrathecal administration of drugs directly into the tumour site, circumventing the BTB [18]. CED has been used in recurrent GBM patients to administer a modified form of inactivated polio virus (PVS-RIPO) with encouraging results [12]. A trait common to aggressive solid tumours is the ability to evade the immune system, a mechanism now well established in brain cancer [19]. Adjuvant immuno-oncology (IO) has essentially failed in clinical testing in GBM. A recent breakthrough has shown that checkpoint inhibitors when given neo-adjuvantly (prior to tumour resection) greatly increases IO efficacy [13]. This seminal study paves the way for future neo-adjuvant approaches and provides a therapeutic modality with general applicability without the need for specialist techniques such as CED. Here we review the research and clinical trial literature with respect to recent perspectives and developments in recurrent GBM. The scope of this review covers critical aspects of tumour evolution, heterogeneity, BBB penetrance, tumour immunology, and recent clinical trials efforts.
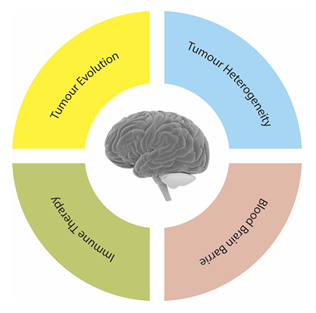
Figure 1: Central obstacles in the development of new therapeutic interventions in recurrent GBM.
2. Tumour Evolution
Understanding the genetic, epigenetic and transcriptomic differences that distinguish primary from recurrent GBM is critical to guide the development of successful targeted therapies. However, while primary GBM has been extensively characterised at the molecular level [2-4, 20-25], similar in-depth analysis is lacking in recurrent disease. Only recently have longitudinal studies begun to shed light on the spatiotemporal evolution of primary and recurrent tumours and studies with larger cohorts are finally beginning to emerge [5, 26].
2.1 Initiating events leading to tumour evolution
Despite significant intra- and inter-tumoural heterogeneity, a common initiating pathway to GBM tumourigenesis involving chromosome 7 (gain) and chromosome 10 (loss) has been established, with copy number variants remaining stable between disease initiation and recurrence [7, 26-31]. Single nucleotide variants (SNVs) occur later during tumour development, classified as either clonal mutations, occurring in all tumour cells, or sub-clonal, occurring in a subset of cells. A prominent example of sub-clonal mutation is the mosaicism of focal amplifications of receptor tyrosine kinases (RTKs) [8, 32-34]. Mutations in PIK3CA, TP53, ATRX and the TERT promoter are mostly clonal, truncal events acquired early during tumour formation and are thought to be responsible for driving early cancer survival and growth [26, 28, 29, 35]. Alternatively, mutations in EGFR, PDGFRA, NF1 and PTEN have been found in both clonal and sub-clonal populations, suggesting these mutations are later events [5, 26, 28, 35]. The frequent sub-clonal occurrence of many known driver gene mutations in pre-treatment and recurrent disease suggests that these accumulate due to convergent evolution caused by common selection pressures rather than being tumour-initiating events. On a global level, the majority of mutations in the primary tumour are retained at recurrence [26, 36]. However, mutations in known driver genes, including EGFR, PDGFRA, the ARF/TP53 pathway, PTEN, NF1 and the INK/RB1 pathway, are disproportionally affected by mutational switching [5, 9, 26, 28, 35, 36]. Driver gene mutations can be lost, acquired, mutated at a different site, or show different amplification/deletion breakpoints. Importantly, Draaisma et al. found that approximately 20% of tumours show mutational changes in genes involved in cell cycle, the PI3K/AKT/mTOR and RTK signalling pathways at recurrence [26]. Mathematical modelling demonstrated that this has important implications for clinical trial design, particularly for therapies that target genes with lower mutation retention frequencies, such as EGFR [26]. Divergence of driver gene alterations was more pronounced in distant compared to local recurrences, suggesting that distant recurrences in particular should be reassessed to ascertain therapeutic vulnerabilities to targeted therapies [36]. Relapse-specific or -enriched alterations are rare [26, 29]. Examples include mutations in MSH6, a component of the DNA mismatch repair (MMR) pathway, LTBP4, a regulator of the TGF-beta pathway, the insulin-like growth factor 1 receptor (IGF1R) and TET2, DNMT3A and PRDM2, which are involved in DNA methylation [5, 26].
Whole genome and exome sequencing of pair-matched primary and recurrent tumours showed that genetic evolution occurs mostly in an idiosyncratic manner [28]. This suggests that large population-based studies are required to characterise patient cohorts with shared evolutionary patterns of recurrence. Nonetheless, two overarching patterns were identified, supporting a model whereby recurrent tumours arises either from an early ancestral clone that branched off during tumour formation (divergent evolution) or from residual disease clones that persist through therapy (linear evolution) [36]. Branched evolution resulted in substantial genomic divergence with a low mutation retention frequency of approximately 25% between the primary and recurrent tumour. Linear evolution, on the other hand, gave rise to tumours with a high mutation retention frequency (~75%) [36]. Comparison of evolution patterns with clinical parameters found that local recurrences typically developed via linear evolution, whereas distant tumours via divergent evolution, accompanied with a small percentage of mutations from the primary tumour [36]. In support of this finding, Lee and colleagues also found greater genetic diversity between distant compared to local recurrences [35]. Together, these studies imply that spatially and/or temporally distant recurrent tumours arise from clones that diverged during early tumour development and underwent extensive clonal selection. However, even in the case of ‘linear’ evolution, Wang et al. reported that dominant clone(s) in recurrent disease are typically not linear descendants of the dominant clone(s) from the primary tumour, but rather are descendants of minor clones that persisted following therapy [5].
Several studies suggest that the clones responsible for tumour recurrence arise early during tumour development [5, 29, 31, 38]. Dominant clones at diagnosis and relapse had evolved separately from a common ancestor many years prior [5]. Early ancestral clones have been described to reside in the subventricular zone (SVZ) and within infiltrating margins [38-40]. Piccirillo et al. demonstrated the presence of ancestral cells with tumour-initiating capacity in the SVZ, a known stem cell niche [39]. The same group later extended this study, demonstrating that residual disease clones in the infiltrating tumour margins had diverged early during tumourigenesis [40]. Phylogenetic analysis of pair-matched samples suggested that these infiltrative sub-clones are/might be the ‘missing link’ between the primary and recurrent tumour [40].
2.2 The effect of temozolomide on tumour evolution and recurrence
Numerous studies have suggested that tumour heterogeneity contributes to treatment failure [31, 33, 34, 40, 41]. Muscat et al. provided evidence for chemoradiation-induced selection of resistant clones by comparing pair-matched primary and recurrent GBM. Therapy reduced the number of sub-clonal variants while expanding resistant sub-populations [6]. An example of this mechanism has been shown for EGFR-targeted therapies, where 82% of patients showed loss of EGFRvIII expression at relapse after receiving treatment that targeted the variant of this receptor [42]. TMZ is an oral alkylating agent that is the first-line chemotherapeutic agent for the treatment of GBM [1]. In the absence of a hypermutation phenotype, Muscat and colleagues found no enrichment of a TMZ-induced mutational signature (CàT transitions at CpC and CpT dinucleotides) following TMZ treatment [6]. Similarly, Koerber et al. reported no enrichment of the TMZ signature in recurrent tumours following TMZ therapy [29]. Together these findings show that TMZ has little influence on the generation of new mutations in recurrent disease in the absence of a hypermutation phenotype. In contrast, hypermutated tumours harbour defects in genes encoding proteins of the DNA mismatch repair (MMR) pathway and showed strong enrichment of the TMZ mutational signature [5, 26, 29]. Hypermutation was found to predominantly affect highly expressed genes, suggesting that TMZ and/or MMR preferentially target areas with open chromatin [5]. Also TMZ-associated hypermutation phenotype was found to be rare in IDH-WT disease suggesting that standard treatment poses little risk of developing hypermutation for patients with primary GBM [6, 27, 37]. This is in stark contrast to the observations made in the less common form of recurrent IDH1-mutant glioma [10]. Two possible explanations for this disparity between IDH1 wild-type and mutant gliomas has been proposed [36, 43]. The cumulative dose of TMZ given to patients with primary GBM is lower than IDH-mutant or low-grade glioma, raising the possibility that long-term exposure to TMZ increases the risk of hypermutation [5, 36]. Secondly, IDH1-mutation may predispose tumours to TMZ-induced hypermutation. IDH1 gain-of-function mutations predispose tumours to MGMT promoter methylation, thereby reducing the chance to repair TMZ-induced mutagenesis and as a result increasing the chance to acquire mutations in MMR pathway genes associated with hypermutation [5, 36]. Overall, longitudinal studies of GBM evolution have revealed a significant amount of evolutionary divergence in recurrent disease. As a corollary, several studies advocate for resampling of the recurrent tumour before selecting targeted therapies for treatment [7, 26, 36].
3. Tumour Heterogeneity
Intratumoural heterogeneity describes a phenomenon where individual cells or compartments within a single tumour mass are associated with different subgroups or molecular characteristics, (reviewed in [44]). Surgical multisampling of spatially separated GBM tumours has identified both unique and common genetic, epigenetic, and transcriptional alterations [31, 45]. On a transcriptional level GBM heterogeneity is characterised by three transcriptional subtypes, namely classical, proneural and mesenchymal [3, 4]. Each subtype is enriched for specific genetic alterations, classical GBM shows a high frequency in EGFR alterations and 95% of classical GBM exhibit a homozygous deletion of CDKN2A (INK4a/ARF) [4]. The proneural subtype is associated with IDH1 mutation, and TP53, PDGFRA amplification or mutations. IDH1 mutations are relatively rare in primary de novo GBM and even more so in recurrent GBM [46, 47]. Mesenchymal GBM shows a high level of heterogeneity and alterations in tumour suppressor genes such as Neurofibromatosis 1 (NF1), TP53 and loss of phosphatase and tensin homolog (PTEN); 30-49% of GBM tissues can be classified as mesenchymal [4, 24]. This is of importance, since patients with this subtype, both at the primary and recurrent state of the disease, tend to have a worse survival rate compared to classical and proneural subtypes [48]. Several studies have elegantly stratified GBM into molecular subtypes [3, 4, 24]. This concept has recently been extended by Suva and colleagues using single cell RNASeq. In this study they defined four dynamic cell states with the ability to recapitulate the tumour mass post-therapy [2]. Among these classifications, the mesenchymal subtype has been associated with a more stem cell-like phenotype and has been linked to radioresistance and GBM recurrence [48]. Moreover, two-thirds of primary GBMs classified as a proneural or classical switch towards the mesenchymal subtypes at tumour recurrence [5]. Several well-known markers have been associated with a mesenchymal phenotype in GBM such as vimentin and CD44. More recently other receptors such as EphA3 and dystroglycan have been shown to be enriched in mesenchymal GBM tissue and linked to tumour recurrence [49-52]. Phase I EphA3-targeting trials have shown promise with significant levels of EphA3-positive tumour tissue detected in recurrent GBM patients [53].
Glioma stem cells (GSCs) comprise a small population of cancer cells that are present in tumour tissue and are characterised by high tumorigenicity and self-renewal capacity [54]. It is now well-described that GSCs, harbour the capacity to differentiate into other tumour cell types giving rise to the diverse and dynamic heterogeneity observed within GBM [2, 5, 23, 31, 55]. In addition, GSCs have been associated with resistance to therapy and tumour recurrence [56]. Seminal studies conducted by Rich and colleagues showed that CD133+ GSCs could effectively promote radioresistance [56, 57]. More recently, GSCs have been shown to promote chemoresistance at nearly every pharmacologic level [58]. Secretion of exosomes, activation of autophagy [59], cell metabolism [60], ROS production [61] drug efflux [62], and microRNA expression [63, 64] are also altered in GSCs and can further enhance therapeutic resistance. Significant effort has been leveraged to tackle GBM heterogeneity by defining therapeutic strategies to target the GSC pool in effect targeting the tumour at its roots. An alternate strategy, could be approaches which induce differentiation of the entire tumour cell population delaying growth [65]. Hence, constraining GSCs to a limited transcriptional program as cells differentiate and reduce available escape routes from therapy [66]. Differentiation therapy has shown clinical promise in acute promyelocytic leukemia (APL) with the use of all trans retinoic acid (ATRA) [67]. Bone morphogenetic protein (BMP) signalling triggers cell-cycle exit and astrocyte differentiation of GSCs and might therefore be useful as a differentiation therapy [68]. A BMP-mimicking peptide GBMP1a, induces astroglial differentiation of GSCs in vitro [69]. However, these cells show limited differentiation commitment and remain vulnerable to cell-cycle re-entry, retaining stem cell-like DNA methylation patterns [70]. Moreover, Blocking WNT and SHH signalling in combination with BMP treatment has been shown to supress GSC self-renewal capacity and extended survival of tumour-bearing mice [71]. Clinical translation of differentiation therapies in brain cancer still appears difficult and further investigation into the mechanisms by which tumour cells evade differentiation commitment is needed.
4. Blood Brain Barrier (BBB)
The BBB is a brain-specific complex architecture comprising endothelial cells, pericytes, astrocytes, neurons, and extracellular matrix components. Tight junctions between endothelial cells and pericytes form the BBB to restrict the diffusion of larger molecules (>180 Daltons) from entering the brain [14]. This naturally occurring protective mechanism prevents or significantly reduces the ingress of many therapeutic agents. In addition, the BBB expresses high levels of drug efflux pumps posing a further problem. BBB integrity is partially compromised in brain tumours, commonly referred to as the blood–tumour barrier (BTB) [72]. The BTB can be detected during magnetic resonance imaging (MRI) by measuring the diffusion of gadolinium. Despite being leakier than the BBB, the BTB is heterogeneously permeable to most chemotherapeutic agents and is the rate-limiting factor in clinically effective therapy. The BTB is often more disrupted in recurrent disease and is likely the main reason why novel therapies that fail in the upfront setting show promise in a recurrent cohort [73, 74]. A recent example is Depatux-M (ABT-414) monotherapy that showed improved progression-free survival in the recurrent setting but then failed in newly diagnosed patients and the trial was subsequently ceased [11].
Numerous efforts have been made to bypass the BBB to improve drug uptake. Targeting low-density lipoprotein receptor-related protein 1 (LRP1) on the cell surface of BTB cells has shown some efficacy in recurrent GBM studies [75]. An interesting report in the recurrent disease showed that Bevacizumab globally reduced permeability, but had a positive effect in leaky regions allowing better delivery of TMZ [76]. Success of studies combining chemotherapeutic agents with drugs that inhibit efflux pumps suggest that more potent inhibitors could increase drug penetration across the BTB [77]. Physical approaches to breach the BTB are garnering recent renewed interest. Magnetic resonance-guided focused ultrasound (MRgFUS) is at the forefront of these technologies and has demonstrated great success in clinical studies. MRgFUS employs short ultrasound pulses with circulating microbubbles to transiently disrupt the BTB thus increasing permeability for 6-8 hours, allowing a window for increased drug uptake [15, 78]. Phase II clinical studies have not only confirmed preclinical findings but also demonstrated the safety and efficacy of this novel technology in recurrent disease [79, 80]. Nanotechnology has also shown promise as an emerging technology. A recent study showed the successful transport of TMZ and an anticancer drug JQ1 packaged in a liposomal nanoparticle using mouse orthotopic glioma models [81]. The study reported stable drug circulation in the bloodstream when encapsulated by nanoparticles with higher drug accumulation in xenografted tumours and improved animal survival. Nanoparticles have also been successfully delivered directly to the brain via the intranasal route, bypassing systemic circulation [82].
A recent phase II clinical trial showed very promising results in a small cohort of recurrent GBM patients [12]. The trial was based on the expression of the poliovirus receptor CD115 in GBM that was recognised by a recombinant poliovirus. The polio vaccine PVS-RIPO was infused directly into the patient’s tumour via convection- enhanced delivery (CED). CED employs a syringe pump connected to a catheter implanted at the tumour site to exert a constant pressure differential to drive drug-laden fluid throughout the tumour [18]. The success of this trial has driven renewed interest in CED and similar approaches as it enables a platform to test novel approaches and to re-test numerous intravenously administered drugs that have failed in clinical trial. A recent study used MR imaging to monitor CED in real time using iron oxide nanoparticles, showing broader distribution of a glioma-specific targeting therapy [83]. Many other CED and FUS based trials are currently in progress in recurrent disease and will reveal if these approaches will bring more durable responses in the future.
5. Immune Therapy
The immune system in the brain follows different principles from the immune system elsewhere. Most apparent reasons are the limited access to the tumour facilitated by the BBB, and the substantial endogenous and treatment-induced immunosuppression of the host. The CNS was once considered an immune-privileged site on the basis that non-syngeneic tissues are not rejected when implanted into the brains of mice; a perception that has only recently been disproved [84-87]. It is now clear that the brain is accessible to the afferent and efferent arms of the immune system, and thus to immune therapy, reviewed in [88].
5.1 Tumour microenvironment
Relative to other solid tumours, CNS tumours display low numbers of tumour-infiltrating lymphocytes (TILs) and other immune effector cells [89]. This ‘cold tumour’ phenotype is associated with inadequate responses to immune checkpoint inhibitors (ICIs) [90]. Also, TILs that are present frequently display an exhausted phenotype [91]. Unlike in peripheral organs, unrestrained inflammation and increased intracranial pressure pose a threat to the brain. For this reason, both inflammatory and adaptive immune responses are tightly regulated in the CNS. This regulation involves a variety of immunosuppressive mechanisms at both the molecular and cellular levels [92]. In response to inflammation, brain stromal cells produce high levels of immunosuppressive cytokines, transforming growth factor β (TGFβ) and interleukin-10 (IL-10), thereby counteracting inflammatory cytokines to maintain homeostasis [93, 94]. Glioma cells regulate tryptophan levels in the microenvironment by the expression of indolamine 2,3-dioxygenase (IDO). Which in turns leads to the accumulation of regulatory T (Treg) cells and the suppression of T cell activity [95, 96]. Both microglia and tumour-infiltrating macrophages produce high levels of arginase, thereby depleting arginine in the tumour tissue. Low arginine levels have an inhibitory effect on T cell proliferation and function [97]. Specific inhibition of immunosuppressive factors in combination with other therapies are currently under investigation in patients with brain tumours. Targeting TGFβ with antisense oligonucleotides [98] or blocking antibodies [99], as well as kinase inhibitors targeting the TGFβ receptor 1 (TGFβR1) [85] have failed. Several ongoing studies are examining the use of IDO inhibitors in brain tumours. Clinical trials of arginase inhibitors in solid tumours are also underway, but none is specific for brain tumours. Targeting the immunosuppressive cells within the tumour microenvironment represents an alternative strategy. Up to 30% of a GBM tumour is composed of tumour-associated macrophages (TAMs) [87]. Data from mouse models and human samples show that the vast majority of TAMs in GBM arise from circulating monocytes (85%), with a minor portion being of microglial (<15%) origin [100-102]. The anti-inflammatory M2 macrophage phenotype and the number of infiltrating TAMs positively correlate with GBM grade and negatively with tumour prognosis [103, 104]. Both TAMs and GSCs are enriched in perivascular regions and hypoxic niches in GBM [37, 105, 106], suggesting a close interaction between these cell types [107]. Moreover, GSCs facilitate a pro-tumour microenvironment by promoting the survival of TAMs [108]. Interestingly, both GSC and TAM populations are elevated in recurrent tumours after irradiation [56, 109]. The close association between TAMs and GSCs strongly suggests a reciprocal molecular crosstalk that is crucial for GBM malignant progression. Although macrophages are important in modulating the immune system, targeting TAMs alone is not sufficient to elicit an effective immune response. Additionally, many existing treatment modalities affect and are affected by the myeloid compartment, therefore, emphasising the need for combination with myeloid targeting to prevent myeloid-mediated therapy resistance.
5.2 Checkpoint inhibitors
Checkpoint inhibitors work by releasing a natural brake on the immune system allowing anticancer CD8+ T cells to recognise and eliminate tumours. Targeting PD1 (programmed death 1), its ligand PD1L1 (PD1 ligand 1) or cytotoxic T lymphocyte-associated antigen 4 (CTLA4) have demonstrated activity in a variety of solid tumours [110, 111]. Although numerous preclinical studies reported positive results [89, 112, 113], a phase III clinical trial (CheckMate-143) comparing anti-PD1 therapy nivolumab with bevacizumab (anti-vascular endothelial growth factor A (VEGFA)) in the treatment of recurrent GBM did not show a benefit over bevacizumab? [114]. CheckMate-489 a phase III study in newly diagnosed patients with O6-methylguanine-DNA-methytransferase (MGMT) promoter-unmethylated GBM showed similarly disappointing results (NCT02617589). In this study, nivolumab in combination with radiation was compared to standard-of-care. A third study (CheckMate-548) evaluating nivolumab in combination with TMZ in patients with MGMT-methylated GBM, is still pending (NCT02667587).
More promising are the results of an early phase clinical trial evaluating immune response and survival following neoadjuvant and/or adjuvant therapy with pembrolizumab in 35 patients with recurrent, surgically resectable GBM. Patients receiving neoadjuvant pembrolizumab, with continued adjuvant therapy showed a significant increase in overall survival compared to adjuvant PD-1 blockade alone. This result was associated with the T cell-mediated interferon response, which resulted in a downregulation of cell-cycle-related genes within the tumour cells. The study also showed that pre-surgical checkpoint inhibition resulted in a systemic expansion of tumour-specific T lymphocytes resulting in a greater initial T cell diversity, which in turn potentiated responsiveness to PD-1 blockade [13]. Although no obvious clinical benefit was observed in a single-arm phase II clinical trial using neoadjuvant nivolumab treatment, enhanced expression of chemokine transcripts, higher immune cell infiltration and increased clonal T cell receptor diversity among tumour-infiltrating T cells indicate a local immunomodulating effect of treatment [92]. Neoadjuvant administration/treatment promises significant improvements in patient’s outcome with minimal changes to treatment modality.
5.3 Vaccines
Cancer vaccine therapy aims to activate the patient’s immune system to recognise tumour-associated antigens and destroy the tumour. Vaccines encompass a range of treatments, including systemic exposure to autologous or allogeneic antigens as well as the induction of a tumour-specific immune response by dendritic cell (DC) vaccination. The advantage of this approach is the potential for eliciting a widespread and durable response. GBM-specific antigens are rare, and some of these antigens are restricted by HLA types, limiting the patient population in which these vaccines may be considered. Peptide vaccines targeting a single tumour antigen, such as EGFRvIII, IDHR132H and Wilms tumour 1 (WT1) led to substantial increase in survival in an uncontrolled phase II trial, but no benefit was observed in a randomised phase III trial [115]. Single-peptide vaccinations harbour the potential for tumour immune escape. An EGFRvIII vaccine study revealed that the majority of patients with recurrence lost EGFRvIII expression [42]. Multi-peptide vaccines are considered to resolve the problem of antigen loss, but none of these clinical trials investigating multi-peptide vaccines have given a clear indication of efficacy [116, 117]. SL701 a vaccine consisting of short synthetic peptides targeting IL-13Rα2, EphA2, and Survivin, showed a median overall survival of 12 month in a phase II study in recurrent GBM. The study reported that 8/28 patients mounted a target-specific CD8 response, which was associated with longer survival [118]. Given that GBM-specific antigens are rare a number of tumour-associated antigens are being studied in GBM. Although being not specific to tumour cells, limited expression elsewhere makes these safe targets to exploit [119]. Immunisation with whole GBM tissue lysate was lethal when studied in animal models [120]; however, vaccines formulated from heat shock proteins (HSP) and DC vaccines, have been well-tolerated with promising early results. A detailed review of completed vaccine trials in GBM was recently published [119].
5.4 Oncolytic viral therapy
Oncolytic viruses (OVs) are viruses that are naturally cancer-selective or can be genetically modified to reduce pathogenicity, increase lytic potential, as well as induce innate and adaptive anti-tumour immune response. Initially designed as a mechanism of gene delivery to provide tumour cells with susceptibility to chemotherapy, is now recognised as a form of immunotherapy. Viruses are recognised by the immune system through pathogen-associated molecular patterns and pattern recognition receptors. Furthermore, viruses often activate macrophages through receptors, such as TLRs [121]. As a secondary effect, activated myeloid cells can improve the infiltration of T cells into tumours to promote an inflamed microenvironment. As a result, viral therapies are a very interesting approach to overcoming the immunosuppression of GBM. The excitement about this therapy is largely driven by the population of long-term survivors which was recently reviewed [122]. To-date, two therapeutic viruses have entered testing in phase III clinical trial, ASPECT and Toca5. Initial results on ASPECT, a replication-deficient adenovirus, showed prolonged time to death or to reintervention. However, no difference in median overall survival was observed [123]. Toca5 a non-lytic retrovirus expressing cytosine deaminase was compared to standard therapies in recurrent high-grade gliomas(NCT01470794). 5 patients out of 23 who received Toca 511 showed durable responses and as of August 2017, all of those patients were still alive, one over 4 years [124]. Several other viral therapies that include replication competent HSV1 (G207), parvovirus (ParvOryx01), adenovirus (DNX-2401), and poliovirus (PVS-RIPO) [12], have reported durable responses in patients with GBM [122]. The future direction of oncolytic viral therapies seems to be focused on combinations with immunotherapy strategies, to potentially induce a durable anti-cancer immune response initiated by the viral infection and to elicit prolonged clinical responses.
5.5 CAR T-Cell therapy
Chimeric antigen receptor (CAR) T-cell therapy has achieved tremendous successes in treatment of haematological malignancies [125]. CAR T-cell therapy has the advantage of bypassing the need for MHC antigen presentation, the development of an adaptive immune response and hence, the need for co-stimulatory signals. Despite the success in haematological malignancies the response to CAR T-cell therapy in solid tumours including GBM have been disappointing. This has been attributed to the complexity of solid tumours. This therapy faces multiple obstacles in solid tumours such as the hostile tumour microenvironment, on-tumour/off-tumour toxicities, and undesired antigen specificity, reviewed in [126]. The tumour antigens that have been most investigated for CAR T therapy in GBM to-date are EGFRvIII, HER2 and IL-13Rα2. Encouragingly, none of the clinical trials in GBM using CAR T-cell therapy reported unmanageable CNS side effects, a concern that arose in CAR T-cell therapy in B cell lymphoma which led to elevated intracranial pressure and associated encephalopathy [127]. Various CAR T-cell constructs and routes of administration are currently under investigation. We summarise here the results of three recent reports. As mentioned/noted above, EGFRvIII has also been targeted using CAR T-cell therapy. Infiltration of CAR T-cells showed elevated levels of intratumoural EGFRvIII CAR T-cell DNA and a decrease in EGFRvIII expression, suggesting effective infiltration of the tumour [128]. Although CAR T-cells efficiently infiltrated and eliminated EGFRvIII+ tumour cells, no partial or complete responses were observed [128]. CAR T-cells targeting HER2, a receptor tyrosine kinase with high expression in a proportion of GBM, has been explored [129]. A phase I clinical trial, enrolling 10 adult and 7 paediatric patients, with heavily pre-treated recurrent HER2+ GBM were treated with HER2-specific CAR T-cells [130]. The study demonstrated relative safety and persistence of HER2 virus-specific CAR T-cells in peripheral blood for up to one year. One patient had a partial response for more than 9 months and seven patients had stable disease for between 8 weeks to 29 months. The median overall survival was 11.1 months from the first T-cell infusion and 24.5 months after diagnosis [130]. A safety and efficacy trial of CAR T-cells targeting IL-13Rα2 in GBM was performed on a group of three patients. IL-13Rα2 modulates activation of the rapamycin pathway and is typically associated with a worse overall prognosis in GBM [131, 132]. Patients received an intracranial infusion post-resection, followed by an intertumoural infusion and an intraventricular infusion. Two out of three GBM patients showed a radiological response and a significant decrease in IL13Rα2 expression after therapy [133]. One patient with recurrent multifocal IDH1 wild-type, MGMT non-methylated GBM showed a dramatic response that lasted for 7.5 months. However, disease ultimately recurred in this patient [134]. An important observation in this study was that the route of delivery appeared decisive with complete regression of multi-focal tumours following intraventricular administration. This CAR T target is continuing to be studied in combination with check point inhibitors (NCT04003649).
|
Category |
Therapy |
Target |
Phase |
Clinical trials |
|
Immune checkpoint inhibition |
Nivolumab |
PD-1 |
III III III |
NCT02017717 NCT02617589 NCT02667587‡ |
|
Pembrolizumab |
PD-1 |
II |
NCT02337491 |
|
|
Durvalumab |
PD-L1 |
I |
NTC02866747 |
|
|
Ipilimumab |
CTLA-4 |
I |
NCT03233152 |
|
|
Anti-LAG3 |
LAG3 |
I |
NCT02658981 |
|
|
Vaccines |
Rindopepimut |
EGFRvIII |
II III |
NCT01498328 NCT03068650 |
|
DC-Vax |
tumour lysate antigen vaccine |
II |
NCT03014804 |
|
|
DSP-7888 in combination with bevacizumab |
Wilms tumour gene 1 (WT1) protein + anti-VEGFA |
II |
NCT03149003 |
|
|
IDH1 peptide vaccine |
IDH1 |
I |
NCT02193347 |
|
|
CMV pp65 DC |
pp65 |
I |
NCT03299309 |
|
|
CMV pp65 DC in combination with bevacizumab nivolumab |
pp65 + PD-1 |
I |
NCT02529072 |
|
|
TVI-Brain-1 |
cancer cell vaccine |
II |
NCT01290692 |
|
|
HSPPC-96 |
tumor-derived heat shock protein peptide-complex |
II |
NCT00905060‡ |
|
|
ICT-107 |
tumor associated antigens |
III |
NCT02546102‡ |
|
|
SL701/poly-ICLC |
IL-13Ra2, ephrin A2, survivin |
I |
NCT02078648 |
|
|
PVS-RIPO |
Poliovirus |
I |
NCT01491893‡ |
|
|
ASPECT [123] |
Adenovirus-mediated |
III |
2004-000464-28 |
|
|
Toca511 |
Retroviral replicating vector |
I |
NCT01470794 |
|
|
CAR T-Cells |
EGFR-806 |
EGFRvIII |
I |
NCT03638167 |
|
HER2-specific CAR T-cells |
HER2 |
I |
NCT03500991 |
|
|
IL-13Ra2-specific CAR T-cells |
IL-13Ra2 |
I |
NCT04003649 NCT02208362 |
|
|
CMV-specific CAR T-cells |
CMV specific antigens |
I |
ACTRN12609000338268 |
Table 1: Representative immune therapy clinical trials in recurrent glioblastoma (‡ studies on newly-diagnosed glioblastoma). Interventions are categorised based on their mode of action.
Multiple studies indicate the human cytomegalovirus (CMV) is a contributing factor to glioma progression [135]. This finding is further emphasised by the presence of CMV sequences in malignant T-cells [136, 137] and that vaccination with autologous GBM lysate elicited a CMV-specific immune response. A clinical phase I trial for adoptive immunotherapy using CMV-specific T-cells in patients with recurrent GBM proved the safety of adoptive immunotherapy and was coincident with disease stabilisation [138]. Studies of recurrent GBM have revealed resistance mechanisms at all phases of the immune response. Intrinsic resistance prevents the initiation of a response, adaptive resistance deactivates tumour-infiltrating immune cells and acquired resistance protects a tumour from specific targeting. Future trials utilising immune therapy will target multiple antigens in each patient in an attempt to address tumour antigen heterogeneity in the recurrent setting.
6. Future Directions
Multiple small-cohort clinical trials using specialist techniques have shown promising results in recurrent disease, often with responses only observed in a subset of enrolled patients. The challenge moving forward will be to select the best candidate approaches, define tests to determine which patients will respond and broaden patient access. Technical approaches that improve BBB therapy penetrance such as CED and MgFUS hold significant promise and revive previously failed systemic therapy-based clinical trials. In theory, all previously targeted agents and antibodies that have failed in the vein could be reassessed using CED or MgFUS. These approaches are not without limitation, requiring specialist CED surgical techniques or equipment and expertise in the case of MgFUS. A significant cost is also attached to these procedures and scalability is an issue. Interestingly, the BTB appears to be less stringent in the recurrent setting compared to upfront disease. This is hopeful for therapeutic interventions at recurrence. Depatux-M (ABT-414), developed by Abbvie, showed significant promise during initial testing in a recurrent cohort but was subsequently ceased during phase III clinical trial in the upfront setting. Pharmaceutical companies could be encouraged through federal incentive schemes to continue therapies that show positive signals in recurrent GBM, as the need is so great and almost all patients invariably experience relapse.
The success of immunotherapy in GBM faces several obstacles including the highly immunosuppressive nature of GBM and the limitations of the immune response in the central nervous system. Learning from phase III clinical trial failures, the future of immunotherapy for GBM appears most hopeful for combination therapies driven by biomarkers for appropriate patient selection. Given the extreme need for improved survival in GBM, current clinical trials are evaluating checkpoint inhibition in combination with novel therapies including vaccines, CAR-T cell therapy, and viral therapy. The biggest breakthrough in recent times in recurrent GBM has been the use of neoadjuvant IO. This relies on the existing recurrent tumour acting as sink of both immune cells and tumour cells to raise an appropriate response prior to surgical resection. The benefits of neoadjuvant IO include accessibility, scalability, well-established toxicity profiles with minimal changes to standard practices. A number of clinical trials are either underway or in preparation and the effectiveness of these approaches will be further refined in the coming years. Deciphering the biology driving recurrent GBM might harbour the promise of targeted therapy at the stage of the primary disease. Hence, preventing recurrence by managing the initial disease. Here we summarise exciting biological discoveries and recent progress in the treatment of patients with recurrent GBM. GBM remains a particularly challenging disease as little progress has been made towards improving patient outcomes and survival. A better understanding of the origins of this cancer and the molecular biology driving glioma genesis at recurrence is still needed to develop therapies addressing the main obstacles discussed in this review.
7. Conclusions
Now is time for hope for brain cancer sufferers. A significant build up in our knowledge of the disease has occurred in the past decade. This, in essence, has “primed the pump” and will lead future discoveries and clinical trial design into the future. Substantial financial support through federal programs such as the Cancer Moon-Shot in the United States and Australian Brain Cancer Mission (ABCM) have been leveraged to bring discoveries from bench to bedside. These programs have also strengthened awareness and community philanthropic support. Based on the advances discussed in this review the next decade should see significant breakthroughs for patients suffering from this aggressive disease.
Funding
This review was funded by generous philanthropic support from Christine Sadler and the Sid Faithfull Group.
Conflicts of Interest
Authors declare no conflict of interest.
References
- Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. The New England journal of medicine 352 (2005): 987-996.
- Neftel C, Laffy J, Filbin MG, et al. An Integrative Model of Cellular States, Plasticity, and Genetics for Glioblastoma. Cell 178 (2019): 835-849.e821.
- Wang Q, Hu B, Hu X, et al. Tumor Evolution of Glioma-Intrinsic Gene Expression Subtypes Associates with Immunological Changes in the Microenvironment. Cancer Cell 32 (2017): 42-56.e46.
- Verhaak RG, Hoadley KA, Purdom E, et al. Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell 17 (2010): 98-110.
- Wang J, Cazzato E, Ladewig E, et al. Clonal evolution of glioblastoma under therapy. Nat Genet 48 (2016): 768-776.
- Muscat AM, Wong NC, Drummond KJ, et al. The evolutionary pattern of mutations in glioblastoma reveals therapy-mediated selection. Oncotarget 9 (2018): 7844-7858.
- Baysan M, Woolard K, Cam MC, et al. Detailed longitudinal sampling of glioma stem cells in situ reveals Chr7 gain and Chr10 loss as repeated events in primary tumor formation and recurrence. International journal of cancer 141 (2017): 2002-2013.
- Nickel GC, Barnholtz-Sloan J, Gould MP, et al. Characterizing Mutational Heterogeneity in a Glioblastoma Patient with Double Recurrence (Genomic Heterogeneity in Recurrent Glioblastoma). PloS one 7 (2012): e35262.
- Schafer N, Gielen GH, Rauschenbach L, et al. Longitudinal heterogeneity in glioblastoma: moving targets in recurrent versus primary tumors. Journal of Translational Medicine 17 (2019).
- Johnson BE, Mazor T, Hong C, et al. Mutational analysis reveals the origin and therapy-driven evolution of recurrent glioma. Science 343 (2014): 189-193.
- van den Bent M, Gan HK, Lassman AB, et al. Efficacy of depatuxizumab mafodotin (ABT-414) monotherapy in patients with EGFR-amplified, recurrent glioblastoma: results from a multi-center, international study. Cancer Chemother Pharmacol 80 (2017): 1209-1217.
- Desjardins A, Gromeier M, Herndon JE, et al. Recurrent Glioblastoma Treated with Recombinant Poliovirus. The New England journal of medicine 379 (2018): 150-161.
- Cloughesy TF, Mochizuki AY, Orpilla JR, et al. Neoadjuvant anti-PD-1 immunotherapy promotes a survival benefit with intratumoral and systemic immune responses in recurrent glioblastoma. Nat Med 25 (2019): 477-486.
- Daneman R, Prat A. The blood-brain barrier. Cold Spring Harb Perspect Biol 7 (2015): a020412-a020412.
- Brighi C, Reid L, White AL, et al. MR-guided focused ultrasound increases antibody delivery to nonenhancing high-grade glioma. Neurooncol Adv 2 (2020): vdaa030-vdaa030.
- Cheng L, Huang Z, Zhou W, et al. Glioblastoma Stem Cells Generate Vascular Pericytes to Support Vessel Function and Tumor Growth. Cell 153 (2013): 139-152.
- Sarkaria JN, Hu LS, Parney IF, et al. Is the blood-brain barrier really disrupted in all glioblastomas? A critical assessment of existing clinical data. Neuro Oncol 20 (2018): 184-191.
- Bobo RH, Laske DW, Akbasak A, et al. Convection-enhanced delivery of macromolecules in the brain. Proceedings of the National Academy of Sciences of the United States of America 91 (1994): 2076-2080.
- Brown NF, Carter TJ, Ottaviani D, et al. Harnessing the immune system in glioblastoma. Br J Cancer 119 (2018): 1171-1181.
- Brennan Cameron w, Verhaak Roel g.W, McKenna A, et al. The Somatic Genomic Landscape of Glioblastoma. Cell 155 (2013): 462-477.
- Frattini V, Trifonov V, Chan JM, et al. The integrated landscape of driver genomic alterations in glioblastoma. Nat Genet 45 (2013): 1141-1149.
- Noushmehr H, Weisenberger DJ, Diefes K, et al. Identification of a CpG Island Methylator Phenotype that Defines a Distinct Subgroup of Glioma. Cancer Cell 17 (2010): 510-522.
- Patel AP, Tirosh I, Trombetta JJ, et al. Single-cell RNA-seq highlights intratumoral heterogeneity in primary glioblastoma. Science 344 (2014): 1396-1401.
- Phillips HS, Kharbanda S, Chen R, et al. Molecular subclasses of high-grade glioma predict prognosis, delineate a pattern of disease progression, and resemble stages in neurogenesis. Cancer Cell 9 (2006): 157-173.
- Sturm D, Witt H, Hovestadt V, et al. Hotspot Mutations in H3F3A and IDH1 Define Distinct Epigenetic and Biological Subgroups of Glioblastoma. Cancer Cell 22 (2012): 425-437.
- Draaisma K, Chatzipli A, Taphoorn M, et al. Molecular Evolution of IDH Wild-Type Glioblastomas Treated With Standard of Care Affects Survival and Design of Precision Medicine Trials: A Report From the EORTC 1542 Study. Journal of Clinical Oncology 38 (2020): 81-99.
- Aubry M, de Tayrac M, Etcheverry A, et al. From the core to beyond the margin: a genomic picture of glioblastoma intratumor heterogeneity. Oncotarget 6 (2015): 12094-12109.
- Kim H, Zheng S, Amini SS, et al. Whole-genome and multisector exome sequencing of primary and post-treatment glioblastoma reveals patterns of tumor evolution. Genome Res 25 (2015): 316-327.
- Körber V, Yang J, Barah P, et al. Evolutionary Trajectories of IDH WT Glioblastomas Reveal a Common Path of Early Tumorigenesis Instigated Years ahead of Initial Diagnosis. Cancer Cell 35 (2019): 692-704.e612.
- Ozawa T, Riester M, Cheng Y-K, et al. Most Human Non-GCIMP Glioblastoma Subtypes Evolve from a Common Proneural-like Precursor Glioma. Cancer Cell 26 (2014): 288-300.
- Sottoriva A, Spiteri I, Piccirillo SG, et al. Intratumor heterogeneity in human glioblastoma reflects cancer evolutionary dynamics. Proceedings of the National Academy of Sciences of the United States of America 110 (2013): 4009-4014.
- Francis JM, Zhang CZ, Maire CL, et al. EGFR variant heterogeneity in glioblastoma resolved through single-nucleus sequencing. Cancer Discov 4 (2014): 956-971.
- Snuderl M, Fazlollahi L, Le Long p, et al. Mosaic Amplification of Multiple Receptor Tyrosine Kinase Genes in Glioblastoma. Cancer Cell 20 (2011): 810-817.
- Szerlip N, Pedraza A, Chakravarty D, et al. Intratumoral heterogeneity of receptor tyrosine kinases EGFR and PDGFRA amplification in glioblastoma defines subpopulations with distinct growth factor response. Proceedings of the National Academy of Sciences, USA 109 (2012): 3041-3046.
- Lee JK, Wang J, Sa JK, et al. Spatiotemporal genomic architecture informs precision oncology in glioblastoma. Nat Genet 49 (2017): 594-599.
- Kim J, Lee IH, Cho HJ, et al. Spatiotemporal Evolution of the Primary Glioblastoma Genome. Cancer Cell 28 (2015): 318-328.
- Jin-Ku L, Jiguang W, Jason KS, et al. Spatiotemporal genomic architecture informs precision oncology in glioblastoma. Nature Genetics 49 (2017).
- Li Y, Li B, Li W, et al. Murine models of IDH-wild-type glioblastoma exhibit spatial segregation of tumor initiation and manifestation during evolution. Nat Commun 11 (2020): 3669.
- Piccirillo SG, Spiteri I, Sottoriva A, et al. Contributions to drug resistance in glioblastoma derived from malignant cells in the sub-ependymal zone. Cancer research 75 (2015): 194-202.
- Spiteri I, Caravagna G, Cresswell GD, et al. Evolutionary dynamics of residual disease in human glioblastoma. Annals of Oncology 30 (2019): 456-463.
- Nathanson DA, Gini B, Mottahedeh J, et al. Targeted therapy resistance mediated by dynamic regulation of extrachromosomal mutant EGFR DNA. Science 343 (2014): 72-76.
- Sampson JH, Heimberger AB, Archer GE, et al. Immunologic escape after prolonged progression-free survival with epidermal growth factor receptor variant III peptide vaccination in patients with newly diagnosed glioblastoma. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 28 (2010): 4722.
- Ramaswamy V, Taylor Michael d. The Amazing and Deadly Glioma Race. Cancer Cell 28 (2015): 275-277.
- Almendro V, Marusyk A, Polyak K. Cellular heterogeneity and molecular evolution in cancer. Annual review of pathology 8 (2013): 277-302.
- Parker NR, Hudson AL, Khong P, et al. Intratumoral heterogeneity identified at the epigenetic, genetic and transcriptional level in glioblastoma. Sci Rep 6 (2016): 22477.
- Hegi ME, Murat A, Lambiv WL, et al. Brain tumors: molecular biology and targeted therapies. Annals of oncology: official journal of the European Society for Medical Oncology 17 (2006): 191-197.
- Ohgaki H, Dessen P, Jourde B, et al. Genetic pathways to glioblastoma: a population-based study. Cancer Res 64 (2004): 6892-6899.
- Bhat KPL, Balasubramaniyan V, Vaillant B, et al. Mesenchymal differentiation mediated by NF-κB promotes radiation resistance in glioblastoma. Cancer cell 24 (2013): 331-346.
- Day BW, Stringer BW, Al-Ejeh F, et al. EphA3 maintains tumorigenicity and is a therapeutic target in glioblastoma multiforme. Cancer Cell 23 (2013): 238-248.
- Offenhäuser C, Al-Ejeh F, Puttick S, et al. EphA3 Pay-Loaded Antibody Therapeutics for the Treatment of Glioblastoma. Cancers (Basel) 10 (2018).
- Day BW, Lathia JD, Bruce ZC, et al. The dystroglycan receptor maintains glioma stem cells in the vascular niche. Acta Neuropathol 138 (2019): 1033-1052.
- Qazi MA, Vora P, Venugopal C, et al. Cotargeting Ephrin Receptor Tyrosine Kinases A2 and A3 in Cancer Stem Cells Reduces Growth of Recurrent Glioblastoma. Cancer Res 78 (2018): 5023-5037.
- Gan H, Cher L, Inglis P, et al. Abstract CT063: Preliminary findings of a Phase I safety and bioimaging trial of KB004 (ifabotuzumab) in patients with glioblastoma. Cancer Research 79 (2019): CT063.
- Lathia JD, Mack SC, Mulkearns-Hubert EE, et al. Cancer stem cells in glioblastoma. Genes Dev 29 (2015) 1203-1217.
- West J, Bianconi G, Severini S, et al. Differential network entropy reveals cancer system hallmarks. Sci Rep 2 (2012): 802.
- Bao S, Wu Q, McLendon RE, et al. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature 444 (2006): 756-760.
- Chen J, Li Y, Yu T-S, et al. A restricted cell population propagates glioblastoma growth after chemotherapy. Nature 488 (2012): 522-526.
- Auffinger B, Spencer D, Pytel P, et al. The role of glioma stem cells in chemotherapy resistance and glioblastoma multiforme recurrence. Expert Rev Neurother 15 (2015): 741-752.
- Lomonaco SL, Finniss S, Xiang C, et al. The induction of autophagy by gamma-radiation contributes to the radioresistance of glioma stem cells. International journal of cancer 125 (2009): 717-722.
- Saga I, Shibao S, Okubo J, et al. Integrated analysis identifies different metabolic signatures for tumor-initiating cells in a murine glioblastoma model. Neuro Oncol 16 (2014): 1048-1056.
- Kim SH, Kwon CH, Nakano I. Detoxification of oxidative stress in glioma stem cells: mechanism, clinical relevance, and therapeutic development. Journal of neuroscience research 92 (2014): 1419-1424.
- Bleau AM, Hambardzumyan D, Ozawa T, et al. PTEN/PI3K/Akt pathway regulates the side population phenotype and ABCG2 activity in glioma tumor stem-like cells. Cell stem cell 4 (2009): 226-235.
- Haemmig S, Baumgartner U, Glück A, et al. miR-125b controls apoptosis and temozolomide resistance by targeting TNFAIP3 and NKIRAS2 in glioblastomas. Cell death & disease 5 (2014): e1279.
- Godlewski J, Nowicki MO, Bronisz A, et al. Targeting of the Bmi-1 oncogene/stem cell renewal factor by microRNA-128 inhibits glioma proliferation and self-renewal. Cancer Res 68 (2008): 9125-9130.
- Enane FO, Saunthararajah Y, Korc M. Differentiation therapy and the mechanisms that terminate cancer cell proliferation without harming normal cells. Cell death & disease 9 (2018): 912.
- Furusawa C, Kaneko K. Chaotic expression dynamics implies pluripotency: when theory and experiment meet. Biology Direct 4 (2009): 17.
- Wang Z-Y, Chen Z. Acute promyelocytic leukemia: from highly fatal to highly curable. Blood 111 (2008): 2505-2515.
- Piccirillo SG, Reynolds BA, Zanetti N, et al. Bone morphogenetic proteins inhibit the tumorigenic potential of human brain tumour-initiating cells. Nature 444 (2006): 761-765.
- Rampazzo E, Dettin M, Maule F, et al. A synthetic BMP-2 mimicking peptide induces glioblastoma stem cell differentiation. Biochimica et biophysica acta. General subjects 1861 (2017): 2282-2292.
- Carén H, Stricker SH, Bulstrode H, et al. Glioblastoma Stem Cells Respond to Differentiation Cues but Fail to Undergo Commitment and Terminal Cell-Cycle Arrest. Stem Cell Reports 5 (2015): 829-842.
- Jin X, Jin X, Kim LJY, et al. Inhibition of ID1–BMPR2 Intrinsic Signaling Sensitizes Glioma Stem Cells to Differentiation Therapy. Clinical Cancer Research 24 (2018): 383-394.
- Nduom EK, Yang C, Merrill MJ, et al. Characterization of the blood-brain barrier of metastatic and primary malignant neoplasms. Journal of neurosurgery 119 (2013): 427-433.
- Lyle LT, Lockman PR, Adkins CE, et al. Alterations in Pericyte Subpopulations Are Associated with Elevated Blood-Tumor Barrier Permeability in Experimental Brain Metastasis of Breast Cancer. Clinical cancer research : an official journal of the American Association for Cancer Research 22 (2016): 5287-5299.
- Lockman PR, Mittapalli RK, Taskar KS, et al. Heterogeneous blood-tumor barrier permeability determines drug efficacy in experimental brain metastases of breast cancer. Clinical cancer research: an official journal of the American Association for Cancer Research 16 (2010): 5664-5678.
- Drappatz J, Brenner A, Wong ET, et al. Phase I Study of GRN1005 in Recurrent Malignant Glioma. Clinical Cancer Research 19 (2013): 1567.
- Gerstner ER, Emblem KE, Chang K, et al. Bevacizumab Reduces Permeability and Concurrent Temozolomide Delivery in a Subset of Patients with Recurrent Glioblastoma. Clinical cancer research: an official journal of the American Association for Cancer Research 26 (2020): 206-212.
- Kim M, Kizilbash SH, Laramy JK, et al. Barriers to Effective Drug Treatment for Brain Metastases: A Multifactorial Problem in the Delivery of Precision Medicine. Pharmaceutical Research 35 (2018): 177.
- Meairs S. Facilitation of Drug Transport across the Blood-Brain Barrier with Ultrasound and Microbubbles. Pharmaceutics 7 (2015): 275-293.
- Idbaih A, Canney M, Belin L, et al. Safety and Feasibility of Repeated and Transient Blood-Brain Barrier Disruption by Pulsed Ultrasound in Patients with Recurrent Glioblastoma. Clinical Cancer Research (2019).
- Carpentier A, Canney M, Vignot A, et al. Clinical trial of blood-brain barrier disruption by pulsed ultrasound. Sci Transl Med 8 (2016): 343re342.
- Lam FC, Morton SW, Wyckoff J, et al. Enhanced efficacy of combined temozolomide and bromodomain inhibitor therapy for gliomas using targeted nanoparticles. Nature Communication 9 (2018): 1991.
- Van Woensel M, Mathivet T, Wauthoz N, et al. Sensitization of glioblastoma tumor micro-environment to chemo- and immunotherapy by Galectin-1 intranasal knock-down strategy. Sci Rep 7 (2017): 1217.
- Stephen ZR, Chiarelli PA, Revia RA, et al. Time-Resolved MRI Assessment of Convection-Enhanced Delivery by Targeted and Nontargeted Nanoparticles in a Human Glioblastoma Mouse Model. Cancer Res 79 (2019): 4776-4786.
- Cserr HF, Harling-Berg CJ, Knopf PM. Drainage of brain extracellular fluid into blood and deep cervical lymph and its immunological significance. Brain Pathol 2 (1992): 269-276.
- Aspelund A, Antila S, Proulx ST, et al. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. The Journal of experimental medicine 212 (2015): 991-999.
- Louveau A, Herz J, Alme MN, et al. CNS lymphatic drainage and neuroinflammation are regulated by meningeal lymphatic vasculature. Nature neuroscience 21 (2018): 1380-1391.
- Louveau A, Smirnov I, Keyes TJ, et al. Structural and functional features of central nervous system lymphatics. Nature 523 (2015): 337-341.
- Britta E, Peter V, Roy OW. The movers and shapers in immune privilege of the CNS. Nature Immunology 18 (2017).
- Zeng J, See AP, Phallen J, et al. Anti-PD-1 Blockade and Stereotactic Radiation Produce Long-Term Survival in Mice With Intracranial Gliomas. Int. J. Radiat. Oncol. Biol. Phys 86 (2013): 343-349.
- Wu A, Maxwell R, Xia Y, et al. Combination anti-CXCR4 and anti-PD-1 immunotherapy provides survival benefit in glioblastoma through immune cell modulation of tumor microenvironment. Journal of Neuro-Oncology 143 (2019): 241-249.
- Jackson CM, Lim M. Immunotherapy for Glioblastoma: Playing Chess, Not Checkers. Clinical Cancer Research, 24 (2018): 4059-4061.
- Schalper KA, Rodriguez-Ruiz ME, Diez-Valle R, et al. Neoadjuvant nivolumab modifies the tumor immune microenvironment in resectable glioblastoma. Nat Med 25 (2019): 470-476.
- Bauer H-C, Krizbai IA, Bauer H, et al. "You Shall Not Pass"-tight junctions of the blood brain barrier. Front Neurosci 8 (2014): 392.
- Spector R. Nutrient transport systems in brain: 40 years of progress. J Neurochem 111 (2009): 315-320.
- Coureuil M, Lécuyer H, Bourdoulous S, et al. A journey into the brain: insight into how bacterial pathogens cross blood-brain barriers. Nat Rev Microbiol 15 (2017): 149-159.
- Jackson CM, Lim M, Drake CG. Immunotherapy for brain cancer: recent progress and future promise. Clinical Cancer Research 20 (2014): 3651-3659.
- Hutter G, Theruvath J, Graef CM, et al. Microglia are effector cells of CD47-SIRPα antiphagocytic axis disruption against glioblastoma. Proceedings of the National Academy of Sciences 116 (2019): 997-1006.
- Goldmann J, Kwidzinski E, Brandt C, et al. T cells traffic from brain to cervical lymph nodes via the cribroid plate and the nasal mucosa. Journal of Leukocyte Biology 80 (2006): 797-801.
- Widner H, Jönsson BA, Hallstadius L, et al. Scintigraphic method to quantify the passage from brain parenchyma to the deep cervical lymph nodes in rats. European journal of nuclear medicine 13 (1987): 456-461.
- Da Mesquita, S, Fu, Z, Kipnis, J. The Meningeal Lymphatic System: A New Player in Neurophysiology. Neuron 100 (2018): 375-388.
- Da Mesquita S, Louveau A, Vaccari A, et al. Functional aspects of meningeal lymphatics in ageing and Alzheimer's disease. Nature 560 (2018): 185-191.
- Han S, Zhang C, Li Q, et al. Tumour-infiltrating CD4(+) and CD8(+) lymphocytes as predictors of clinical outcome in glioma. Br J Cancer 110 (2014): 2560-2568.
- Prosniak M, Harshyne LA, Andrews DW, et al. Glioma Grade Is Associated with the Accumulation and Activity of Cells Bearing M2 Monocyte Markers. Clinical Cancer Research 19 (2013): 3776.
- Lu-Emerson C, Snuderl M, Kirkpatrick ND, et al. Increase in tumor-associated macrophages after antiangiogenic therapy is associated with poor survival among patients with recurrent glioblastoma. Neuro Oncol 15 (2013): 1079-1087.
- Li Z, Bao S, Wu Q, et al. Hypoxia-Inducible Factors Regulate Tumorigenic Capacity of Glioma Stem Cells. Cancer Cell 15 (2009): 501-513.
- Zhou W, Ke SQ, Huang Z, et al. Periostin secreted by glioblastoma stem cells recruits M2 tumour-associated macrophages and promotes malignant growth. Nat Cell Biol 17 (2015): 170-182.
- Wu A, Wei J, Kong L-Y, et al. Glioma cancer stem cells induce immunosuppressive macrophages/microglia. Neuro Oncol 12 (2010): 1113-1125.
- Tao W, Chu C, Zhou W, et al. Dual Role of WISP1 in maintaining glioma stem cells and tumor-supportive macrophages in glioblastoma. Nature Communications 11 (2020): 3015.
- Deininger MH, Pater S, Strik H, et al. Macrophage/microglial Cell Subpopulations in Glioblastoma Multiforme Relapses are Differentially Altered by Radiochemotherapy. Journal of Neuro-Oncology 55 (2001): 141-147.
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. The New England journal of medicine 373 (2015): 23-34.
- Robert C, Schachter J, Long GV, et al. Pembrolizumab versus Ipilimumab in Advanced Melanoma. The New England journal of medicine 372 (2015): 2521-2532.
- Reardon DA, Gokhale PC, Klein SR, et al. Glioblastoma Eradication Following Immune Checkpoint Blockade in an Orthotopic, Immunocompetent Model. Cancer immunology research 4 (2016): 124-135.
- Wainwright DA, Chang AL, Dey M, et al. Durable therapeutic efficacy utilizing combinatorial blockade against IDO, CTLA-4, and PD-L1 in mice with brain tumors. Clinical cancer research: an official journal of the American Association for Cancer Research 20 (2014): 5290-5301.
- Filley AC, Henriquez M, Dey M. Recurrent glioma clinical trial, CheckMate-143: the game is not over yet. Oncotarget 8 (2017): 91779-91794.
- Oji Y, Hashimoto N, Tsuboi A, et al. Association of WT1 IgG antibody against WT1 peptide with prolonged survival in glioblastoma multiforme patients vaccinated with WT1 peptide. International journal of cancer 139 (2016): 1391-1401.
- Pollack IF, Jakacki RI, Butterfield LH, et al. Antigen-specific immune responses and clinical outcome after vaccination with glioma-associated antigen peptides and polyinosinic-polycytidylic acid stabilized by lysine and carboxymethylcellulose in children with newly diagnosed malignant brainstem and nonbrainstem gliomas. J Clin Oncol 32 (2014): 2050-2058.
- Rampling R, Peoples S, Mulholland PJ, et al. A Cancer Research UK First Time in Human Phase I Trial of IMA950 (Novel Multipeptide Therapeutic Vaccine) in Patients with Newly Diagnosed Glioblastoma. Clinical Cancer Research 22 (2016): 4776.
- Peereboom DM, Nabors LB, Kumthekar P, et al. Phase 2 trial of SL-701 in relapsed/refractory (r/r) glioblastoma (GBM): Correlation of immune response with longer-term survival. Journal of Clinical Oncology 36 (2018): 2058-2058.
- Lim M, Xia Y, Bettegowda C, et al. Current state of immunotherapy for glioblastoma. Nat Rev Clin Oncol 15 (2018): 422-442.
- Bigner DD, Pitts OM, Wikstrand CJ. Induction of lethal experimental allergic encephalomyelitis in nonhuman primates and guinea pigs with human glioblastoma multiforme tissue. Journal of neurosurgery 55 (1981): 32-42.
- Akira S, Takeda K, Kaisho T. Toll-like receptors: critical proteins linking innate and acquired immunity. Nat Immunol 2 (2001): 675-680.
- Chiocca EA, Nassiri F, Wang J, et al. Viral and other therapies for recurrent glioblastoma: is a 24-month durable response unusual?. Neuro Oncol 21 (2019): 14-25.
- Westphal M, Ylä-Herttuala S, Martin J, et al. Adenovirus-mediated gene therapy with sitimagene ceradenovec followed by intravenous ganciclovir for patients with operable high-grade glioma (ASPECT): a randomised, open-label, phase 3 trial. The Lancet. Oncology 14 (2013): 823-833.
- Cloughesy TF, Landolfi J, Vogelbaum MA, et al. Durable complete responses in some recurrent high-grade glioma patients treated with Toca 511 + Toca FC. Neuro Oncol 20 (2018): 1383-1392.
- Reiss SN, Yerram P, Modelevsky L, et al. Retrospective review of safety and efficacy of programmed cell death-1 inhibitors in refractory high grade gliomas. J Immunother Cancer 5 (2017): 99.
- Ma S, Li X, Wang X, et al. Current Progress in CAR-T Cell Therapy for Solid Tumors. Int J Biol Sci 15 (2019): 2548-2560.
- Neelapu SS, Tummala S, Kebriaei P, et al. Chimeric antigen receptor T-cell therapy - assessment and management of toxicities. Nat Rev Clin Oncol 15 (2018): 47-62,
- O'Rourke DM, Nasrallah MP, Desai A, et al. A single dose of peripherally infused EGFRvIII-directed CAR T cells mediates antigen loss and induces adaptive resistance in patients with recurrent glioblastoma. Sci Transl Med 9 (2017): eaaa0984.
- Ahmed N, Salsman VS, Kew Y, et al. HER2-specific T cells target primary glioblastoma stem cells and induce regression of autologous experimental tumors. Clinical cancer research: an official journal of the American Association for Cancer Research 16 (2010): 474-485.
- Ahmed N, Brawley V, Hegde M, et al. HER2-Specific Chimeric Antigen Receptor-Modified Virus-Specific T Cells for Progressive Glioblastoma: A Phase 1 Dose-Escalation Trial. JAMA oncology 3 (2017): 1094-1101.
- Thaci B, Brown CE, Binello E, et al. Significance of interleukin-13 receptor alpha 2-targeted glioblastoma therapy. Neuro Oncol 16 (2014): 1304-1312
- Brown CE, Starr R, Aguilar B, et al. Stem-like tumor-initiating cells isolated from IL13Rα2 expressing gliomas are targeted and killed by IL13-zetakine-redirected T Cells. Clinical cancer research: an official journal of the American Association for Cancer Research 18 (2012): 2199-2209.
- Brown CE, Badie B, Barish ME, et al. Bioactivity and Safety of IL13Rα2-Redirected Chimeric Antigen Receptor CD8+ T Cells in Patients with Recurrent Glioblastoma. Clinical cancer research: an official journal of the American Association for Cancer Research 21 (2015): 4062-4072.
- Brown CE, Alizadeh D, Starr R, et al. Regression of Glioblastoma after Chimeric Antigen Receptor T-Cell Therapy. The New England journal of medicine 375 (2016): 2561-2569.
- Michaelis M, Baumgarten P, Mittelbronn M, et al. Oncomodulation by human cytomegalovirus: novel clinical findings open new roads. Medical microbiology and immunology 200 (2011): 1-5.
- Bhattacharjee B, Renzette N, Kowalik TF. Genetic Analysis of Cytomegalovirus in Malignant Gliomas. Journal of Virology 86 (2012): 6815.
- Ranganathan P, Clark PA, Kuo JS, et al. Significant Association of Multiple Human Cytomegalovirus Genomic Loci with Glioblastoma Multiforme Samples. Journal of Virology 86 (2012): 854.
- Schuessler A, Smith C, Beagley L, et al. Autologous T-cell Therapy for Cytomegalovirus as a Consolidative Treatment for Recurrent Glioblastoma. Cancer Res 74 (2014): 3466.
