Frequency of Atrial Fibrillation in Patients of Hypertension
Article Information
Muhammad Naeem Tariq1*, Muhammad Humayoun Rashid2, Ghoza Chaudhery3, Aqsa Komel4, Azka Aisha4, Ahmad Usman5, Ghulam Yaseen4
1Department of Cardiac Medicine, Punjab Institute of Cardiology, Lahore, Pakistan
2Department of Cardiac Medicine, Chaudhry Pervaiz Elahi Institute of Cardiology, Multan, Pakistan
3Department of Pediatric Medicine, Children’s Hospital, Lahore, Pakistan
4Department of Internal Medicine, Nishtar Hospital, Multan, Pakistan
5Department of General Surgery, Nishtar Hospital, Multan, Pakistan
*Corresponding Author: Muhammad Naeem Tariq, Punjab Institute of Cardiology, Lahore, Pakistan
Received: 09 December 2020; Accepted: 23 December 2020; Published: 11 January 2021
Citation: Muhammad Naeem Tariq, Muhammad Humayoun Rashid, Ghoza Chaudhery, Aqsa Komel, Azka Aisha, Ahmad Usman, Ghulam Yaseen. Frequency of Atrial Fibrillation in Patients of Hypertension. Cardiology and Cardiovascular Medicine 5 (2021): 47-54.
View / Download Pdf Share at FacebookAbstract
Background: Hypertension is a major cause of premature vascular disease leading to cerebrovascular events, ischemic heart disease and peripheral vascular disease. Hypertension and heart failure are most often associated with atrial fibrillation (AF). It together with hypertension proves to be fatal as it leads to stroke and cardiovascular events.
Objective: To determine the frequency of AF in patients of hypertension. Material and methods: It is a cross-sectional study done in Punjab Institute of Cardiology, Lahore and CPE Institute of Cardiology Multan during a duration of six months from 07/02/2020 to 07/08/2020. Data collection: Patients with BP>140/90 mmHg were included. Later on, ECG was taken on a standard 12 lead format. Presence of AF was confirmed. All the data was recorded in a pre-structured proforma.
Results: The mean age of the patients was 48.64 ± 7.74 years. Majority of the cases 148 (74%) were male while 52 (26%) were female. AF was noted in 22 (11%) of cases. AF was significantly higher in patients above 40 years of age (P<0.05) while gender difference and duration of hypertension has insignificant effect on AF (P>0.05).
Conclusion: The frequency of AF is low in hypertensive patients but the value is not ignorable. Periodical screening of AF is required to prevent hazardous consequences.
Keywords
Atrial fibrillation; Hypertension; Diabetes mellitus
Atrial fibrillation articles; Hypertension articles; Diabetes mellitus articles
Article Details
1. Introduction
Hypertension is a well-recognized risk factor for cardiovascular and renal diseases; moreover, even slightly elevated blood pressure (BP) levels lead to increased risk in cardiovascular diseases (CVD) or stroke. Hence, it is one of the leading causes of global burden of disease. As age is an important risk factor for hypertension, the population aging in Western countries exacerbates the situation [1]. The prevalence of hypertension differs substantially by regions [2]. Substantial differences (relative difference >10%) in the prevalence of hypertension were indicated by age group, race/ethnicity, educational attainment, country of birth, family income, health insurance, diabetes, obesity, and disability status [3]. Pakistan National Health Survey showed that the prevalence of hypertension increased from <10% in 18-19 years old to >60% in over 70 years age in males and similarly in females it increased from <5% at 18-19 years to a peak of 70% in 60-69 years age, the prevalence being higher in the female compared to male [4, 5]. There are different risk factors and clinical conditions predisposing to the development of AF, but due to its high prevalence, hypertension is still the main risk factor for the development of AF. Several pathophysiologic mechanisms (like structural changes, neuro hormonal activation, fibrosis, atherosclerosis, etc.) have been advocated to explain the onset of AF. The presence of AF per se increases the risk of stroke but its coexistence with high blood pressure leads to an abrupt increase of cardiovascular complications [6].
Moreover, the activation of renin–angiotensin–aldosterone system activation in patients with hypertension induces left atrial fibrosis and conduction block in the left atrium, resulting in the development of AF. Accordingly, recent studies have shown that effective blockage of renin–angiotensin–aldosterone system by angiotensin converting enzyme inhibitors or angiotensin receptor antagonist may be effective in both primary and secondary prevention of AF in patients with hypertension, although with controversies. In addition, optimal antithrombotic therapy, blood pressure control as well as rate control for AF are key to the management of patients with AF [7].
In a study conducted by the Mitchta I the prevalence of AF was 45.5% among the cases who were having hypertension [8]. In another study it was sated that the prevalence of AF was noted in 14% of cases who have the hypertension [9]. On contrary, AF was found in 3% (1/32) patient with hypertension and no other risk factors for AF [10]. It is evident from the above-mentioned studies that there is no consensus on the actual frequency of patients who have AF with hypertension. Moreover, there is no local study available so far that has evaluated the same in our local population. There are studies that have evaluated that the frequency of AF in cases with hypertension varies from region to region [6-8]. If the frequency of AF was found high than it can be advised to check all the patients of hypertension for AF.
1.1 Objective
To determine the frequency of AF in patients who are presenting with hypertension.
2. Materials and Methods
2.1 Study Design
Cross sectional study.
2.2 Setting
Punjab Institute of Cardiology, Lahore. CPE Institute of Cardiology, Multan.
2.3 Duration
Six months i.e. From: 07/02/2020 to 07/08/2020.
2.4 Sample Size
Sample size of 200 cases is estimated using 95% confidence level and 6% margin of error taking expected frequency of AF as 14%.
2.5 Sample Technique
Non probability consecutive sampling.
2.6 Inclusion Criteria
Patients of age between 20-60 years of both genders with hypertension (BP≥140/90 mmHg 4 hours apart on two occasions) diagnosed at least 6 months ago.
2.7 Exclusion Criteria: Patients with bleeding disorders, congenital abnormalities, already undergone CABG or who have been treated for any cardiac disease were excluded from the study.
2.8 Data Collection Procedure
All the patients were evaluated for the history of taking anti-hypertensive medication at the time of presentation of patients. Later on, ECG was taken on a standard 12 lead format (electrocardiogram model ECG-1112 Carewell electronics, Shenzhen). Presence of AF was confirmed as there is no p wave present on 12 lead ECG and unequal R-R interval and QRS complex <120 ms. All the data was recorded in a pre-structured proforma. Patients with AF were managed as per hospital protocol.
2.9 Data Analysis Procedure
Descriptive statistics for data would be computed using SPSS version 21. Frequency and percentages would be calculated for categorical variables like gender, diabetes and AF. Mean ± S.D would be calculated for continuous variables like age and duration of hypertension. Data was stratified for (i) age, (ii) gender, (iii) diabetes (iv) duration of hypertension and (v) medication for hypertension to control effect modifiers. Post stratification chi square test was applied keeping a –value < 0.05 as significant.
3. Results
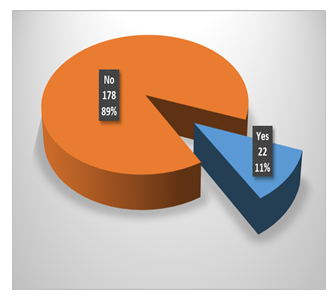
The mean age of the patients was 48.64 ± 7.74 years. There were 148 (74%) males while 52 (52%) females. The male to female ratio was 2.8:1. The mean duration of hypertension was 4.09 ± 1.56 years. There were 70 (35%) diabetics while 130 (65%) were non-diabetic in whole group Table 1. AF was noted in 22 (11%) of cases, while 178 (89%) did not had AF. Figure 1 Data was stratified for age and gender of patients and duration of hypertension. It was noticed that in patients of age 20-40 years, no patient had AF while among patients of age 41-60 years, 22 (13%) cases had AF. There was significant difference between both age groups for AF i.e. p=0.033. In male patients, 18 (12.2%) patient had AF while among female patients, 4 (7.7%) cases had AF. There was insignificant difference between both genders for AF i.e. p=0.376. In 1-4years of hypertension, 14 (11.5%) patient had AF while among 5-8 years hypertension, 8 (10.3%) cases had AF. There was insignificant difference between both genders for AF i.e. p=0.788 Table 2.
|
n |
200 |
|
Age (Years) |
48.64 ± 7.74 |
|
Male |
148 (74%) |
|
Female |
52 (26%) |
|
Duration of hypertension (Years) |
4.09 ± 1.56 |
|
Diabetes |
70 (35%) |
Table 1: Baseline characteristics of patients.
|
Comparison |
AF |
P-value |
||
|
Yes |
No |
|||
|
Age (years) |
20-40 |
0 (0%) |
31 (100%) |
0.033 |
|
41-60 |
22 (13%) |
147 (87%) |
||
|
Sex |
Male |
18 (12.2%) |
130 (87.8%) |
0.376 |
|
Female |
4 (7.7%) |
48 (92.3%) |
||
|
Duration of HTN (years) |
1-4 |
14 (11.5%) |
108 (88.5%) |
0.788 |
|
5-8 |
8 (10.3%) |
70 (89.7%) |
||
Table 2: Comparison of AF in different groups.
4. Discussion
AF is the most frequently occurring sustained cardiac arrhythmia and is related to many cardiac diseases. Patients with hypertension have an increased risk of developing AF of 42% and patients with AF have increased cardiovascular morbidity and mortality. Due to the high prevalence of hypertension, it accounts for more cases of AF than any other risk factor. Hypertension is associated with left ventricular hypertrophy, impaired ventricular filling, slowing of atrial conduction velocity, structural changes and enlargement of the left atria [11]. All these changes in cardiac structure and physiology favor development of AF and increase the risk of thromboembolic complications. In the following we will review possible mechanisms for the increased risk of AF in hypertensive patients and look into the effect of different anti-hypertensive treatment with special focus on blockade of the renin-angiotensin-system [12]. AF is a disease of aging as its prevalence doubles with each decade after 50 years and approaches 10% in those more than 80 years of age. As the general population is aging, the prevalence of AF is expected to rise in the future and methods to prevent or to postpone AF development may be of clinical, prognostic, and economic importance. However, prevention is a new strategy in the treatment of AF as it earlier has been more focus on rate and rhythm-control and anticoagulation therapy to prevent cardiovascular endpoints [13].
In 21st century, AF an “old” arrhythmia that was first identified in 1909 has assumed increasing importance as the global demographic tide results in a burgeoning population of elderly individuals. Indeed, Braunwald, in his Shattuck lecture, referred to the growing “epidemic” of AF. The impact of AF on mortality and morbidity is substantial, as are the socio-economic consequences in relationship to hospital admissions, chronic disease management and disabilities [14, 15]. These adverse trends, nonetheless, are superimposed on a background of potentially exciting new therapeutic options. Consequently, an understanding of the epidemiology and natural history of AF is crucial to the future allocation of resources and the utilization of an expanding range of therapies aimed at reducing the impact of this disease on a changing patient population [16].
AF currently affects approximately 2.2 million patients in the U.S. and is the most common rhythm disorder among U.S. patients hospitalized with a primary diagnosis of an arrhythmia [17, 18]. The median age of patients is 75 years; approximately 70% of patients are between the ages of 65 and 85 years, and 84% are older than 65 years [17]. Pooled data from studies of chronic AF in North America, Britain and Iceland suggest a prevalence of 0.5% to 1% in the general population [19]. In two separate studies restricted to patients older than 60 years, the prevalence was 5% to 9% after 5 to 15 years of follow-up [20]. Thus, the genesis of this epidemic was initially attributed to alterations in the age-related composition of the population, with an expanding elderly population accounting for the increasing incidence and prevalence of AF. However, during the past two decades, additional factors seem to have influenced the frequency of this disease. The Framingham study found an increasing prevalence of AF even after adjusting for age, gender and other comorbidities; but underlying explanations are unclear, and further studies in other populations are needed. From a recent population-based study in subjects older than 65 years, the prevalence in men (9.1%) was greater than that in women (4.8%) [21, 22].
In the Framingham study, after adjustment for age and other risk factors, AF developed in men at 1.5 times the rate in women. The reason for the greater susceptibility to AF in men is unexplained. Previous reports indicate that prevalence of AF in western populations is generally greater than Asian populations [23, 24]. There was no clear explanation for this but it could be related to genetic predisposition reported by previous studies on specific polymorphisms that related to AF [25]. A study was planned to find prevalence of AF in the Thai hypertensive population since hypertension is a common cardiovascular risk factor and predisposes individuals to AF [25].
Prevalence of AF in a study was an over-estimate in general population, but is likely to be a valid estimate for the Thai hypertensive population. Prevalence of AF in our study was 11%, which is greater than 1.21% and 1.3% prevalence of AF in general population in Thailand, 0.65% for China, 0.56% for Japan and 0.95% and 1.2% prevalence of AF in the United States and United Kingdom [22-25]. Similarly in another study conducted by Davies and colleagues which reported the prevalence of 5.1% in male and 2.6% in female [20].
Prevalence of AF increases with age due to degenerative process of the atrial muscle and conducting cells [21]. The results of our study were different with those conducted on both western and other Asian populations. The finding on more predominance in males is also consistent with previous reports [22]. We noticed a significant interaction of age and gender on the prevalence of AF. Male gender was more likely to have AF compared to female in the age group less than 60 years, but no such association after the age of 70. This finding was not found in previous reports from Europe and United States. However, similar interaction has been reported from Taiwan. Therefore, the effect of male gender on the increased prevalence of AF in Asian population may disappear after the age of 70 years [23].
Results of our study have some clinical implications. Our main objective was to get an accurate estimate of prevalence of AF in hypertensive population. Our prevalence estimate 11% AF in the hypertensive population is high considering the malignant course of this disease that might cause a serious thrombo-embolic stroke.
5. Conclusion
Hence, the frequency of AF is low in hypertensive patients. But the value is not ignorable. Thus, we can recommend the periodically screening of AF in hypertensive patients, so that prevention and early intervention can be made to prevent the patients from developing hazardous consequences.
References
- Lacruz ME, Kluttig A, Hartwig S, et al. Prevalence and Incidence of Hypertension in the General Adult Population: Results of the CARLA-Cohort Study. Medicine 94 (2015): 952.
- Schipf S, Werner A, Tamayo T, et al. Regional differences in the prevalence of known Type 2 diabetes mellitus in 45-74 years old individuals: Results from six population-based studies in Germany (DIAB-CORE Consortium). Diabetic Medicine 29 (2012): 88-95.
- Gillespie CD, Hurvitz KA. Prevalence of hypertension and controlled hypertension-United States, 2007-2010. MMWR Surveill Summ 62 (2013): 144-148.
- Aziz KU. Evolution of systemic hypertension in pakistani population. Journal of the College of Physicians and Surgeons--Pakistan: JCPSP 25 (2015): 286-291.
- Rottlaender D, Motloch LJ, Schmidt D, et al. Clinical impact of atrial fibrillation in patients with pulmonary hypertension. PloS one 7 (2012): 33902.
- Manolis AJ, Rosei EA, Coca A, et al. Hypertension and atrial fibrillation: diagnostic approach, prevention and treatment. Position paper of the Working Group ‘Hypertension Arrhythmias and Thrombosis’ of the European Society of Hypertension. Journal of hypertension 30 (2012): 239-252.
- Lau Y, Yiu K, Siu C, et al. Hypertension and atrial fibrillation: epidemiology, pathophysiology and therapeutic implications. Journal of human hypertension 26 (2012): 563-569.
- Gorczyca-Michta I, Wozakowska-Kaplon B, Tomasik E. Prevalence and predisposing conditions for atrial fibrillation in hospitalised patients with hypertension. Kardiologia polska 71 (2012): 352-358.
- Andrade J, Khairy P, Dobrev D, et al. The clinical profile and pathophysiology of atrial fibrillation relationships among clinical features, epidemiology, and mechanisms. Circulation research 114 (2014): 1453-1468.
- Samol A, Masin M, Gellner R, et al. Prevalence of unknown atrial fibrillation in patients with risk factors. Europace 15 (2013): 657-662.
- Kannel WB, Wolf PA, Benjamin EJ, et al. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates 1. American Journal of Cardiology 82 (1998): 2N-9N.
- Aksnes TA, Kjeldsen SE, Julius S. Atrial fibrillation and hypertension. Archives of Medical Science Special Issues (2009): 272.
- Investigators AFF-uIoRM. A comparison of rate control and rhythm control in patients with atrial fibrillation. New England Journal of Medicine 347 (2002): 1825-1833.
- Silverman ME. From rebellious palpitations to the discovery of auricular fibrillation: contributions of Mackenzie, Lewis and Einthoven. American Journal of Cardiology 73 (1994): 384-389.
- Braunwald E. Cardiovascular medicine at the turn of the millennium: triumphs, concerns, and opportunities. New England Journal of Medicine 337 (1997): 1360-1369.
- Gersh B. The epidemiology of atrial fibrillation and atrial flutter. Atrial Arrhythmias: State of the Art Armonk, New York: Futura Publishing (1995): 1-22.
- Freinberg W, Blackshear J, Laupacis A, et al. Prevalence, age distribution, and gender of patients with atrial fibrillation. Arch Intern Med 155 (1995): 469-473.
- Investigators SPiAFSG. Preliminary report of the stroke prevention in atrial fibrillation study. New England Journal of Medicine 322 (1990): 863-868.
- Wolf PA, Dawber TR, Thomas HE, et al. Epidemiologic assessment of chronic atrial fibrillation and risk of stroke The fiamingham Study. Neurology 28 (1978): 973-977.
- McLaughlin SA, Wright MJ, Morris KT, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. Journal of Clinical Oncology 26 (2008): 5213-5219.
- Wolf PA, Benhamin EJ, Belanger AJ, et al. Secular trends in the prevalence of atrial fibrillation: The Framingham Study. American heart journal 131 (1996): 790-795.
- Arnold M, Karim-Kos HE, Coebergh JW, et al. Recent trends in incidence of five common cancers in 26 European countries since 1988: analysis of the European Cancer Observatory. European journal of cancer 51 (2015): 1164-1187.
- Chiang C-E, Zhang S, Tse HF, et al. Atrial fibrillation management in Asia: from the Asian expert forum on atrial fibrillation. International journal of cardiology 164 (2013): 21-32.
- Tse H-F, Wang Y-J, Ai-Abdullah MA, et al. Stroke prevention in atrial fibrillation-an Asian stroke perspective. Heart rhythm 10 (2013): 1082-1088.
- Smith JG, Newton-Cheh C, Almgren P, et al. Genetic polymorphisms for estimating risk of atrial fibrillation in the general population: a prospective study. Archives of internal medicine 172 (2012): 742-744.