Food Fortification in Prevention of Micronutrient Deficiencies of Children Under 5 Years in Bangladesh and its Effects on Sustainable Development Goals
Article Information
Karim Khan*, Mahmudul Hasan Faruque, Biswajit Chowdhury, Monjurul Ahsan, Badruzzaman, A.S.M. Ruhul Quddus
Department of Pediatrics, Community-based Medical College & Hospital, Mymensingh, Bangladesh
*Corresponding Author: Prof. M. Karim Khan, Director, Department of Pediatrics, Community-based Medical College & Hospital, Mymensingh, Bangladesh;
Received: 16 May 2022; Accepted: 23 May 2022; Published: 15 July 2022
Citation: M. Karim Khan, Mahmudul Hasan Faruque, Biswajit Chowdhury, Monjurul Ahsan, Badruzzaman, A.S.M. Ruhul Quddus. Food Label and its Influence among Indian Consumers - A Review. Journal of Food Science and Nutrition Research 5 (2022): 603-611.
View / Download Pdf Share at FacebookAbstract
Micronutrients, which contain vitamins and minerals, are required in minute amounts for overall growth, development, and increased immunity against diseases. Because the body is unable to synthesize them, they must be obtained from external sources. Malnutrition causes poor physical and mental development, in susceptible populations such as young children, pregnant and lactating mothers, and the elderly. By supplying important nutrients in food, food fortification is a safe and effective strategy for increasing macronutrient consumption. The lack of micronutrients has an impact on long-term developmental goals. To teach about the benefits of food fortification, the educational program is necessary to create awareness among the mass population. This article gives a detailed overview of Bangladesh's present micronutrient deficiency status among children and women. The success and present problems of existing intervention programs are also discussed in this study. Anemia affects nearly half of all pregnant and lactating mothers. Some of the key dimensions linked to high levels of deficiencies are ignorance, inadequate nutrition, poor hygiene, illness, malabsorption, and infestation. Multiple interventions are being attempted, and some progress has been made. Problems remain like coverage, quality, and compliance. Micronutrient deficiencies in Bangladesh remain a significant concern, despite the fact that current intervention programs have made some success in addressing severe deficiencies. There is a need for a more well-integrated approach to boost existing intervention programs. Furthermore, new intervention techniques for addressing and preventing particular micronutrient deficits are suggested.
Keywords
Food fortification, Deficiencies, Micronutrients, Sustainable goals, Policy & Programs
Food fortification articles; Deficiencies articles; Micronutrients articles; Sustainable goals articles; Policy & Programs articles
Food fortification articles Food fortification Research articles Food fortification review articles Food fortification PubMed articles Food fortification PubMed Central articles Food fortification 2023 articles Food fortification 2024 articles Food fortification Scopus articles Food fortification impact factor journals Food fortification Scopus journals Food fortification PubMed journals Food fortification medical journals Food fortification free journals Food fortification best journals Food fortification top journals Food fortification free medical journals Food fortification famous journals Food fortification Google Scholar indexed journals Deficiencies articles Deficiencies Research articles Deficiencies review articles Deficiencies PubMed articles Deficiencies PubMed Central articles Deficiencies 2023 articles Deficiencies 2024 articles Deficiencies Scopus articles Deficiencies impact factor journals Deficiencies Scopus journals Deficiencies PubMed journals Deficiencies medical journals Deficiencies free journals Deficiencies best journals Deficiencies top journals Deficiencies free medical journals Deficiencies famous journals Deficiencies Google Scholar indexed journals Micronutrients articles Micronutrients Research articles Micronutrients review articles Micronutrients PubMed articles Micronutrients PubMed Central articles Micronutrients 2023 articles Micronutrients 2024 articles Micronutrients Scopus articles Micronutrients impact factor journals Micronutrients Scopus journals Micronutrients PubMed journals Micronutrients medical journals Micronutrients free journals Micronutrients best journals Micronutrients top journals Micronutrients free medical journals Micronutrients famous journals Micronutrients Google Scholar indexed journals Sustainable goals articles Sustainable goals Research articles Sustainable goals review articles Sustainable goals PubMed articles Sustainable goals PubMed Central articles Sustainable goals 2023 articles Sustainable goals 2024 articles Sustainable goals Scopus articles Sustainable goals impact factor journals Sustainable goals Scopus journals Sustainable goals PubMed journals Sustainable goals medical journals Sustainable goals free journals Sustainable goals best journals Sustainable goals top journals Sustainable goals free medical journals Sustainable goals famous journals Sustainable goals Google Scholar indexed journals Policy & Programs articles Policy & Programs Research articles Policy & Programs review articles Policy & Programs PubMed articles Policy & Programs PubMed Central articles Policy & Programs 2023 articles Policy & Programs 2024 articles Policy & Programs Scopus articles Policy & Programs impact factor journals Policy & Programs Scopus journals Policy & Programs PubMed journals Policy & Programs medical journals Policy & Programs free journals Policy & Programs best journals Policy & Programs top journals Policy & Programs free medical journals Policy & Programs famous journals Policy & Programs Google Scholar indexed journals preschool children articles preschool children Research articles preschool children review articles preschool children PubMed articles preschool children PubMed Central articles preschool children 2023 articles preschool children 2024 articles preschool children Scopus articles preschool children impact factor journals preschool children Scopus journals preschool children PubMed journals preschool children medical journals preschool children free journals preschool children best journals preschool children top journals preschool children free medical journals preschool children famous journals preschool children Google Scholar indexed journals iron insufficiency articles iron insufficiency Research articles iron insufficiency review articles iron insufficiency PubMed articles iron insufficiency PubMed Central articles iron insufficiency 2023 articles iron insufficiency 2024 articles iron insufficiency Scopus articles iron insufficiency impact factor journals iron insufficiency Scopus journals iron insufficiency PubMed journals iron insufficiency medical journals iron insufficiency free journals iron insufficiency best journals iron insufficiency top journals iron insufficiency free medical journals iron insufficiency famous journals iron insufficiency Google Scholar indexed journals deficiency-related brain damage articles deficiency-related brain damage Research articles deficiency-related brain damage review articles deficiency-related brain damage PubMed articles deficiency-related brain damage PubMed Central articles deficiency-related brain damage 2023 articles deficiency-related brain damage 2024 articles deficiency-related brain damage Scopus articles deficiency-related brain damage impact factor journals deficiency-related brain damage Scopus journals deficiency-related brain damage PubMed journals deficiency-related brain damage medical journals deficiency-related brain damage free journals deficiency-related brain damage best journals deficiency-related brain damage top journals deficiency-related brain damage free medical journals deficiency-related brain damage famous journals deficiency-related brain damage Google Scholar indexed journals cereals articles cereals Research articles cereals review articles cereals PubMed articles cereals PubMed Central articles cereals 2023 articles cereals 2024 articles cereals Scopus articles cereals impact factor journals cereals Scopus journals cereals PubMed journals cereals medical journals cereals free journals cereals best journals cereals top journals cereals free medical journals cereals famous journals cereals Google Scholar indexed journals
Article Details
Introduction
According to the estimates of the World Health Organization Globally more than 2 billion people have deficiencies in key vitamins and nutrients, particularly vitamin A, iodine, iron, and zinc [1]. Pregnant and lactating women and young children are found to be the most vulnerable groups affected by micronutrient deficiencies. Populations from developed countries are being affected where micronutrient deficiencies co-exist [2]. Food fortification can be defined as a strategy that can prevent vitamin and mineral deficiencies and can be used safely and effectively for better health. According to WHO estimations, 190 million preschool children and 19.1 million pregnant women over the world were vitamins A deficient (serum retinol less than 0.70 mol/l) [3]. Iodine insufficiency affects nearly 100 million women of reproductive age and 82 percent of pregnant women throughout the globe do not get enough zinc to satisfy their needs [4]. Iron deficiency was common, with 1.62 billion persons anemic worldwide, with apex pervasiveness among preschool children (47%) led by pregnant mothers (42%). According to WHO data, 0.8 million people die each year as a result of iron insufficiency, and a comparable number of people die as a result of vitamin A deficiency. Nutritional deficiencies like goiter, rickets, beriberi, and pellagra can be treated through food fortification. Emergent Folic acid deficiency induces neural tube abnormalities, zinc stunts infant growth, and selenium promotes cancer, and the effects are not restricted to health parameters; they can have an economic impact due to physical and mental disorders that impede job productivity [5]. According to the Lancet series on maternal and child nutrition published in 2013, iodine deficiency affects 28.5 percent of the world's population or 1.9 billion people. While this number mostly represents those with minor deficiencies (defined as a urine iodine concentration of 50-99 ug/L), the World Health Organization estimates that around 50 million people suffer from mental impairment as a result of iodine deficiency. In 2012, over 34 million babies were shielded against the lifetime effects of iodine deficiency-related brain damage. Additionally, around 1.62 billion individuals are anemic, primarily owing to iron deficiency. The extent of the problem is substantially larger in underdeveloped nations, where several micronutrient deficiencies frequently arise simultaneously as a result of inadequate bioavailability and micronutrient concentration in diets. Micronutrient deficits are widespread throughout life, but they are more frequent in children and pregnant and lactating women, who have higher micronutrient needs to sustain development and reproduction. Wheat, wheat products, corn, rice, milk, and milk products, salt, sugar, cooking oils, sauces, and morning cereals are the most often fortified foods. They offer channels for delivery of micronutrients and are within the reach of the market in developing countries such as Bangladesh, India, Srilanka and so many. U.S. Preventive Service Task Force published updated guidelines in 2009. In rich nations, these tactics were universal, and many middle-income countries adopted them as well. Nutrient deficiencies have been abolished in developed nations thanks to a rich diet and the intake of fortified goods such as juices, salt, wheat, margarine, sugar, and milk. In Bangladesh, including vitamin A, iron, iodine, and zinc, most people's diets are lacking in one or more micronutrients [6-10]. Because much of the food consumed by the poor is plant-based, the bioavailability of micronutrients, particularly iron, zinc, and vitamin A, is low. Poor dietary quality, not quantity, is thought to be the most important predictor of reduced micronutrient status in this group. Micronutrient deficits are more common in young children and pregnant and breastfeeding mothers. Despite the fact that numerous methods have been taken over the years to address the situation, the incidence of micronutrient insufficiency remains high and is regarded as a major public health issue. The recently completed National Micronutrients Status Survey 2011-2012 (NMS 2011- 2012) has provided a chance to analyze the present micronutrient status of children and women in the country, as well as the accomplishments and challenges of existing programs. The suggested intervention techniques for the prevention and control of micronutrient deficiencies in Bangladesh and their effects on Sustainable development goals (SDG) are also discussed in this paper.
Food Fortification
According to the World Health Organization, food fortification is the addition of one or more ingredients to food, whether or not they are already present in the food, in order to prevent or improve a known deficiency associated with one or more ingredients in the general population or specific groups of the general population. Food fortification is the practice of identifying widely consumed and centrally processed items in order to assure fortification during the manufacture and distribution of food [11]. Because condiments and basic foods are consumed by a larger portion of the population, they are good fortification choices. Vitamins A, D, iodine, iron, folic acid, zinc, and B-complex vitamins can all be utilized for fortification. On a large scale, the fortification of staple foods is cost-effective. The fortification of a few pricey basic items results in a wider distribution of micronutrients across the population, particularly among the poor. Targeted fortification includes foods consumed by certain demographic subgroups, such as newborns, that contribute to increased consumption for that group. The fortification of supplemental meals for young children is handled in a targeted manner. Micronutrients that are required by the majority of the population are the focus of mass and targeted fortification [12]. The most extensively utilized food vehicles are classified as follows: staples (wheat, oils, and rice), condiments (salt, soy sauce, sugar), and processed commercial foods (noodles, newborn supplementary meals, and dairy products). Vitamin A, a fat-soluble vitamin that is added to basic foods like rice, cereal grains, and oils, is crucial for the immune system and eyesight. Vitamin A fortification helps to prevent vitamin A deficiency, which can lead to vision problems and increased susceptibility to sickness. Fortification of wheat, maize flour, and rice is done to avoid nutritional anemia, brain and spine birth abnormalities, and to increase production, which leads to economic advancement and demonstrates the impacts of fortification of wheat, flour, and maize. The primary goal of food fortification was to reduce the development of nutritional deficiencies, notably those caused by a lack of adequate access to key elements. Due to dependence on soil area or intrinsic adequacy from a regular diet, staple foods produced in a given region may be deficient in certain nutrients. Micronutrients can be added to condiments and staples to avoid illness deficiency on a big scale. Another benefit is that food fortification eliminates the cost of shipping perishable commodities like vegetables and fruits, meats, and dairy products to far-flung parts of the globe [13]. The government of the United States and European nations outlaws the fortification of meat, poultry, and fish products, as well as the fortification of unprocessed foods (UN), 1995). Vitamin D is not received in adequate amounts from diets, and most individuals are not exposed to sunshine, resulting in a significant prevalence of vitamin D insufficiency in many nations [14]. Yogurt, bread, spaghetti, and juice are among the vitamin D-fortified foods. Fortified meals raise blood vitamin D and 25-hydroxyvitamin D levels, and fortified foods and pharmaceutical preparations have comparable vitamin D bioavailability. Instead of pushing customers to modify their behaviors, fortification makes commonly consumed items more nutritious, and this is what makes it effective. Food fortification is a thoughtful public health strategy that may reach a higher number of at-risk people using existing food delivery networks without requiring big changes in current consumption habits. It is a cost-effective technique to increase nutritional intake in the population, and fortified foods have the added benefit of maintaining constant body storage [15,16].
|
Micronutrients |
Functions |
||
|
Folic acid (vitamin B9) |
Reduces neural tube birth defects |
||
|
Zinc |
Strengthens immune system |
||
|
Niacin (vitamin B3) |
Prevents Pellagra, a skin disease |
||
|
Riboflavin (vitamin B2) |
Boosts carbohydrates, proteins, and fats metabolism |
||
|
Thiamine (vitamin B1) |
Prevents beriberi, a nervous system disease |
||
|
Vitamin B12 |
Enables functioning of the brain and nervous system |
||
|
Vitamin D |
Improves bone health by allowing absorption of calcium |
||
|
Vitamin A |
Childhood blindness lowers the ability of individuals to tackle infections |
||
|
Calcium |
Makes bones stronger, helps nerve muscles to transmit messages, functioning of muscles and blood clotting |
||
|
Selenium |
Helps in thyroid gland functioning and reproduction |
||
|
Vitamin B6 |
Metabolism involves enzyme reactions |
||
|
Zinc |
Largely estimated in the developing countries |
Poor pregnancy outcome, impaired growth (Stunting), genetic disorders, decreased resistance to infectious disease |
Breakfast cereals, infant formulas, cookies, and diet beverages |
|
Vitamin A |
254 million preschool children |
Night blindness, xerophthalmia, increased risk of mortality in children and pregnant women |
Milk, margarine, yogurts, soft cheese, sugar, monosodium glutamate and tea |
|
Folate (Vitamin B9) |
Insufficient data |
Megaloblastic anemia, neural tube, and other birth defects, heart disease, stroke, impaired cognitive function, depression |
Wheat and corn flours, bread, pasta, rice, cookies, and infant formulas |
|
Cobolamine (Vitamin B12) |
Insufficient data |
Megaloblastic anemia (associated with Helicobacter pylori-induced gastric atrophy) |
Breakfast cereals, diet beverages, Wheat and corn flours, bread, pasta, rice |
|
Thiamine (VitaminB1) |
Insufficient data estimated as in developing countries and in famines, displaced persons |
Beriberi (cardiac and neurologic), Wernicke’s, and Korsakov syndromes (alcoholic confusion and paralysis) |
Wheat and corn flours, bread, pasta, rice, infant formulas and cookies, breakfast cereals, vegetable mixtures, and amino acids |
|
Riboflavin (Vitamin B2) |
Insufficient data, estimated as in developing countries |
Non-specific-fatigue, eye changes, dermatitis, brain dysfunction, impaired iron absorption |
Wheat and corn flours, bread, pasta, rice, vegetable mixtures, amino acid breakfast cereals, and infant formulas and cookies |
|
Niacin (Vitamin B3) |
Insufficient data, estimated as in developing countries |
Pellagra (dermatitis, diarrhea, dementia, death) |
Wheat and corn flours, bread, pasta, rice, breakfast cereals, |
Table 1: Role of vitamins and minerals used in flour and rice fortification includes
|
Micronutrient |
Deficiency Pervasiveness |
Major Deficiency Disorders |
Fortifying vehicle |
|
Iodine |
2 billion at risk |
Goiter, hypothyroidism, iodine deficiency disorders, increased risk of stillbirth, birth defects infant mortality, cognitive impairment |
Salt, bread |
|
Iron |
2 billion famines, displaced persons |
Iron deficiency, anemia, reduced learning, and work capacity, increased maternal and infant mortality, low birth weight |
Wheat and corn flours, bread, pasta, rice, salt, infant formulas and cookies |
|
Vitamin B6 |
Insufficient data, estimated as in developing countries and in famines, displaced persons |
Dermatitis, neurological disorders, convulsions, anemia, elevated plasma homocysteine |
Wheat and corn flours, bread, pasta, rice, infant formulas, cookies, and breakfast cereals |
|
Vitamin C |
Common famines, displaced person |
Scurvy (fatigue, hemorrhages, low resistance to infection, anemia) |
Diet beverages, juices, and substitute drinks |
|
Vitamin D |
Extensive in all age groups, low exposure to ultraviolet rays of the sun |
Rickets, osteomalacia, osteoporosis, colorectal cancer |
Diet beverages, juices, and substitute drinks |
|
Calcium |
Insufficient data, estimated to be widespread |
Decreased bone mineralization, rickets, osteoporosis |
Soymilk, breakfast cereals, infant formulas and cookies, juices, diet beverages and substitute drinks |
|
Selenium |
Insufficient data, common in Asia, Scandinavia, Siberia |
Cardiomyopathy, increased cancer and cardiovascular risk, osteoarthropathy |
Milk, pasta, corn and wheat flours, breakfast cereals, infant formulas, and cookies, juices and spreads |
|
Fluoride |
Widespread |
Increased dental decay risk |
Infant formulas and cookies, breakfast cereals, wheat, and rice flour, milk, juices |
Table 2: Micronutrient deficiencies with disorders and their prevalence around the world
Micronutrient Deficiencies
Micronutrient deficits afflict people of all genders and ages in both industrialized and developing nations, affecting 2 billion people. Micronutrient insufficiency has been linked to a wide range of nonspecific physiological problems, including lower infection resistance, metabolic abnormalities, and physical and psychomotor development [17-21]. Vitamin A deficiency was found in 21% of children over the world, with higher mortality rates from diarrhea, measles, and malaria. Vitamin A deficiency caused over 800,000 deaths in infants and pregnant women worldwide, as well as 1.8 percent of eye problems. Inadequate micronutrient intake can have a significant influence on a child's healthy growth and development, especially if it happens during critical growth years. Micronutrient deficits have subtle effects at first, but they steadily worsen with time, culminating in physical symptoms or clinical indications Worst of all, by the time it manifests themselves as symptoms, the harm has already been done. Some of these effects/consequences are irreversible, such as the child's cognitive development being stunted.
Figure 1: Consequences of Micronutrient deficiencies
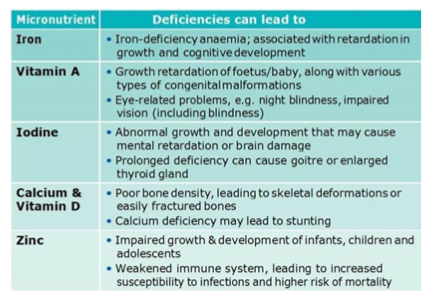
Figure 2: Consequences of Micronutrient deficiencies
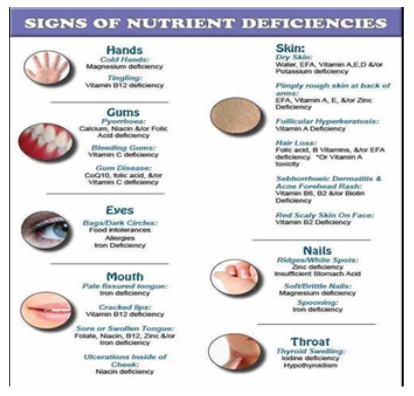
Figure 3: Consequences of Micronutrient deficiencies
In Bangladesh, the usual diets consumed are typically deficient in one or more micronutrients, notably vitamin A, iron, iodine, and/or zinc. The major predictor of decreased micronutrient status in this group is poor dietary quality, not quantity. Micronutrient deficits are more common in young children, pregnant and lactating women, and the elderly. According to the National Micronutrient Survey (NMS) 2011-12, a high number of preschool children suffer from numerous micronutrient deficiencies, with one in every five preschool children suffering from vitamin A deficiency. The prevalence of zinc insufficiency is considerable, with 44% of preschool children suffering from it, and two out of every five preschool children suffering from vitamin D deficiency. Preschool children have a prevalence of calcium deficiency of 24.4 percent, and one-third of them have anemia of which 7.2 percent have iron deficiency anemia. Overall, household food insecurity, poor quality diet (predominantly plant-based foods with minimal animal foods), poor dietary diversity, lack of knowledge about food value and diversity, intra- and inter-household disparity, gender inequality and inequity, and lack of social positioning of vulnerable and marginalized populations are identified as the major underlying causes of micronutrient deficiencies in all segments of the population [22-25]. Furthermore, the most significant risk factors are increased rural-to-urban migration and population density, which is accompanied by a lack of basic living standards (water, sanitation, etc); being a slum dweller or rural resident; lack of affordable diversified foods, particularly animal food sources; and lack of awareness about the consequences of deficiencies and the health benefits of adequate micronutrient intake.
Vitamin A deficiency
Since the 1960s, Bangladesh has recognized VAD as a severe public health issue. Despite the fact that the severity of the problem has significantly diminished over the last decade, the prevalence of VAD (defined by the WHO as a serum retinol concentration of 070 mol/l) has remained stable, particularly among preschool-age (6–59 months) children. Vitamin A is a vital micronutrient for normal visual system functioning, growth and development, epithelial cellular integrity maintenance, and immune functioning and reproduction. Only 5.4 percent of non-pregnant and non-lactating women have low serum retinol concentrations, according to the National Micronutrient Survey 2011-12, which is comparable to what was documented in the 1997-98 National Vitamin A Survey. According to a study from 2011-2012, roughly 34% of NPNL women had insufficient vitamin A status (Serum retinol 1.005 mol/L), up from 29% in 1997-98. Bangladesh's government has been running a National Vitamin A Plus Campaign for children aged 6 to 59 months since 2011. Children aged 6 to 11 months get VAC (100,000 IU retinol equivalent) and children aged 12 to 59 months receive VAC (200, 000 IU). Global research shows that after a high-dose vitamin A supplementation, vitamin A reserves in people with VAD can fall below ideal levels in three to six months; nevertheless, dosing at four to six-month intervals is thought to be sufficient to prevent major VAD outcomes. Low socioeconomic status, living in a slum, a lack of knowledge of vitamin A-rich foods and/or their health benefits, low intake of animal sources of vitamin A, particularly by households with severe food insecurity, and a preponderance of plant-based vitamin A with low bioavailability have all been linked to VAD in all population groups.
Iodine Deficiency
Iodine deficiency illnesses have been recognized as a public health concern in Bangladesh for decades, although good data is difficult to come by. The nationwide prevalence of iodine insufficiency in school-aged children, as determined by mean urine iodine concentration (UIC) below 100 g/L (ICDDR, 2014), is as high as 40%, a prevalence that has remained basically stable since 1999. While there is no current data on the prevalence of severe iodine deficiency (goitre rates) in school-aged children, prior studies showed a significant reduction in goitre prevalence from 50% in 1993 to 6.3 percent in 2004-05 (Yusuf HK, 2007). Household food insecurity, lack of access to iodized packaged salt, rural residency, low levels of awareness about the health benefits of I and iodized salts, consumption of industrial salt (non-iodized), and lack of preservation knowledge about iodized salts have been identified as the major risk factors of I deficiency in the Bangladeshi population.
Anemia and iron deficiency
According to the NMS 2011-2012, 33 percent of children aged 6-59 months and 26 percent of NPNL women had anemia, defined as a Hb concentration of 120 g/l in NPNL women and 110 g/l in children aged 6-59 months. These statistics show a considerable drop from the prevalence reported in 1997-1998 (47 percent in children aged 6–59 months and 45 percent in NPNL women) and 2003 (557% in children aged 6-59 months and 45 percent in NPNL women). The deficiency of iron causes anemia and the symptoms are pale inner eyelids, nailbeds, gums, tongue, lips, and skin. Other symptoms are tiredness, headaches, and breathlessness. Pregnant women and young children are found to be at great risk. Iron deficiency can cause early neonatal mortality and maternal mortality.
Zinc deficiency
According to the NMS 2011–2012, there is a 446 percent prevalence of Zn deficiency among preschool-age children and a 573% prevalence among NPNL women, with the slums having the greatest rate. According to the International Zinc Consultative Group, Zn deficiency was defined as a serum concentration of 109 mmol/l in preschool-age children and a serum concentration of 101 mmol/l in NPNL women. Because serum Zn is homeostatically controlled and incapable of detecting marginal deficit, a large prevalence of low serum Zn is thought to be a plausible signal of a very severe deficiency. Low socioeconomic status, household food insecurity, low intake of animal sources of Zn, and high intake of a plant-based diet with a very high content of phytate (an inhibitor of Zn absorption) are the main drivers behind poor Zn nutrition.
Vitamin D deficiency
Vitamin D is essential in our bodies because it helps to maintain proper calcium and phosphate levels in the blood, which aids bone mineralization, muscular contraction, nervous system activity, and cellular functioning. Based on a blood vitamin D level of less than 50.0 nmol/L, 39.6% of preschool children and 45.5 percent of school-age children had vitamin D insufficiency. The poorest and most severely food insecure households had the highest rate of vitamin D insufficiency in preschool children. For school-aged children, however, it is highest among the wealthiest and most food-secure households. Furthermore, the National Rickets Survey in 2008 found a 1% incidence of rickets among children aged 1 to 15 years, with children under the age of five accounting for 62% of the rachitic cases. There is currently no national policy or program in place to prevent vitamin D insufficiency among the country's high-risk demographic groups. The willingness of the government to work with stakeholders, adequate sunlight across the country, adequate water bodies for fish culture, a homogeneous society, the presence of common fortification food vehicles, women's empowerment, and a potential school feeding program are all identified as possible interventions. However, considerable political commitment is necessary to improve vitamin D status at the population level. It is crucial to highlight that the WHO does not presently suggest vitamin D supplementation during pregnancy as part of standard prenatal care.
B vitamin deficiencies
To date, no data are available on the national level estimates of B vitamin deficiencies among infants and children. According to the NMS 2011-2012, 9 % of NPNL women are deficient in folate, and 23 % of these women have some degree of vitamin B12 deficiency.
Aetiology of micronutrient deficiency
The vast majority of Bangladeshis have a diet that is mostly composed of plant-based foods. They have limited dietary diversity and consume a little number of animal goods such as eggs, milk, and milk products. As a result, a poor-quality diet with low bioavailability may be the leading cause of micronutrient deficiencies in the country. A study of dietary micronutrient intake among young children and their primary female carers in rural Bangladesh found a relatively low overall mean prevalence of sufficiency of micronutrient intake in children (43%) and women (26%) based on estimated average needs. Limited diversity owing to low socio-economic status and family food insecurity, low levels of awareness in connection to an adequate diet and hygienic habits, as well as illness and infestation have all been recognized as key underlying causes of micronutrient deficiencies in the nation.

Figure 4: Consequences of Micronutrient deficiencies
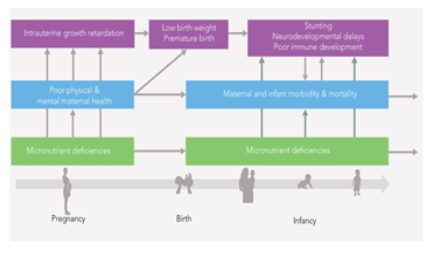
Figure 5: Consequences of Micronutrient deficiencies

Figure 5: Consequences of Micronutrient deficiencies
Effect on Sustainable Development Goals (SDG)
To eradicate dietary deficits in vulnerable populations, organizations such as UNICEF, the WHO, the US Centers for Disease Control and Prevention (CDC), the Global Alliance for Improved Nutrition (GAIN), and Nutrition International advocate fortification. The United Nations adopted. 17 Sustainable Development Goals (SDGs) in September 2015 and fortification of grain products is the first step toward accomplishing SDGs. The SDGs can be accomplished by addressing vitamin and mineral shortages. By adding iron, zinc, and B vitamins such as folic acid, niacin, riboflavin, thiamine, B12, and vitamin B6 to rice, wheat, and maize flour, grain fortification helps to address eight of the 17 SDCs. In a population suffering from anemia, productivity is predicted to be 17 percent lower in heavy physical labor and 5% lower in other manual labor. Iron deficiency causes children's mental ability to be underdeveloped, affecting their academic potential and performance. Furthermore, childhood anemia causes a 2.5 percent decline in adult salaries, as well as slowed productivity and economic growth. Malnutrition is responsible for 45 percent of mortality among children under the age of five. Stunting affects around 2 billion individuals, with the risk of stunting increasing with vitamin and mineral deficits. Adult productivity rises with proper nutritional intake, resulting in increased agricultural production, increased food availability, and famine relief. Zinc deficiency increases the risk of malaria, pneumonia, and diarrhea. According to 2012 data, the world population faces a 17 percent risk of low zinc consumption. Zinc deficiency was linked to 18 percent of malaria cases, 16 percent of lower respiratory tract infections, and 10% of diarrhea cases globally. Infants born anemic during pregnancy have low birth weights, weigh less than 2500 grams (5.5 pounds), and are at a higher risk of mortality and illness. Females are more affected by anemia largely than males. Rates of anemia remain higher in females by the end of puberty and through reproductive years than in males. Low and middle-income nations bear the brunt of nutritional deficiency, resulting in a higher risk of mortality, morbidity, and vulnerability to severe health effects that might be avoided. Fortification helps to attain goals of maternal and newborn health, infectious disease, and non-communicable diseases [26,27]. According to the Global Nutrition Report 2017, fortifying foods has a 16:1 benefit to cost ratio is poor and middle-income nations. Folic acid fortification reduces healthcare costs associated with the treatment of congenital abnormalities of the brain and spine. The following are the main contributors to effective fortification programs and addressing the difficulties of nutritional inadequacies in vulnerable populations, among others:
- dominant individual to support fortification
- an institution with research capacity to monitor the impact
- food industry to fortify food
- policymakers to ensure nationwide fortification
- regulatory agencies for ensuring and monitoring compliance
The vital element for fortification is a national alliance in the country, which is followed by engagement from the public, private, and civic sectors, resulting in a better knowledge of the health and economic advantages of fortification.
Current policies and intervention programs
The current intervention programs and their coverage rates for the prevention and control of micronutrient deficiencies in Bangladesh are given below:
Programs aiming at changing the eating habits of infants and young children
The government of Bangladesh, UN agencies, non-governmental organizations, and donors have supported interventions aimed at improving infant and young child feeding (IYCF) practices from birth, when exclusive breastfeeding is encouraged, through the various stages of complementary food introduction from 6 months and beyond, using a variety of means and methods. In certain circumstances, these initiatives are combined with others that address health, food, livelihoods, water, sanitation, and hygiene.
Anemia-control program for children aged 6-59 months
The National Strategy for the Prevention and Control of Anaemia in Bangladesh recommends using multiple micronutrient powder (MNP) in the diet of children aged 6 to 23 months (and 24 to 59 months if resources are available) to avoid anemia and other micronutrient deficiencies. Currently, the Bangladesh Rural Advancement Committee (BRAC)/Global Alliance for Improved Nutrition (GAIN) is supporting one large-scale area-based MNP program that employs the government-approved five-component (Fe, folic acid, zinc, and vitamins A and C) powder. BRAC's community health workers (Shasthya Shebika) delivered 145 million MNP sachets to rural areas through home visits in 2013.
Vitamin A fortification in edible oil
In December 2011, Bangladesh began fortifying edible oils with vitamin A. Only sixteen of the twenty-two edible-oil refineries make vitamin A-fortified edible oil. While the government adopted the 'National Edible Oil Fortification Law 2013', which ensures that all refined edible oil is fortified with vitamin A, the program has failed to meet its coverage goals.
Iron-folic acid supplementation
While the NMS 2011–2012 shows that children and NPNL women in Bangladesh had low Fe deficiency and IDA, a Fe–folic acid (IFA) supplementation program for pregnant women has been in place for decades to prevent and manage Fe deficiency and anemia. From the second trimester until 90 days after birth, pregnant women get IFA supplements (60 mg Fe and 400 g folic acid daily). One of the components of the Health, Population, and Nutrition Sector Development Program is IFA supplementation (HPNSDP). According to a 2011 survey on Bangladesh's Food Security and Nutrition, 37% of pregnant women did not take any IFA supplements (James P, 2012) and more than half of those who did started in the third trimester.
Promotion of diversified diet
Many government and non-government organizations in Bangladesh have backed a number of initiatives and programs aimed at improving the diet's diversity and quality. The Bangladesh Country Investment Plan is defined as a "roadmap toward investment in agriculture, food security, and nutrition," and its Plan of Action 2008–2015 specified twelve programs. The Bangladesh Country Investment Plan encourages community-based homestead gardening, small-scale animal husbandry, aquaculture, and education, with the goal of increasing family food supply and access in general, but particularly to micronutrient-rich foods. Targeting, outcome monitoring, and greater communication interventions will be necessary to maximize the potential of these programs to address micronutrient deficiencies. Although the National Nutrition Services supports mass media campaigns, social mobilization, and behavior change communication activities at the health facility and community clinic levels, the Ministry of Agriculture and other food-related ministries must also reinforce these specific nutrition-related messages.
|
Intervention program |
Target group |
Current coverage rate |
Comments |
|
Vitamin A supplementation |
Children under 5 years |
Infantsaged 6-11 months: 85·4 % |
No remarkable variation in coverage between urban and rural areas |
|
Fortification of edible oil with vitamin A |
Whole population |
Children aged 12-59 months: 93·7 % |
Recently initiated, no monitor-pregnant able |
|
Fe–folate supplementation |
Pregnant women/ adolescent girls and non-pregnant women |
Not available |
ANC care is weak - less than 30 % of women attend ANC in the first trimester, and attendance at 4+ visits is around Inadequate supply at ANC or inadequate knowledge and practice of the providers -very weak counseling. Poor monitoring. No nationwide program for adolescent girls and non-pregnant women 30% |
|
Universal iodination salt |
Whole population |
Pregnant women: received IFA through ANC: around 60% |
Coverage is lowest in rural areas due to the availability of non-iodized salts which are less costly |
|
Home fortification with MNP |
Children under 5 years |
Adequately iodized salt Retailer’s level: 66·4 % Household level: 57·6 % (>20 ppm) |
A small study conducted in an intensive program area |
|
Promotion of diversified diet |
Whole population |
N/A |
Policies are in place to improve diversified agriculture, fisheries and aquaculture and livestock development, and community-based nutrition programs, but much stronger efforts are needed to achieve goal |
Table 3: Current intervention programs for the prevention and control of various micronutrient deficiencies in Bangladesh
Discussion
NMS 2011-2012, Bangladesh's most recent national survey, provided crucial data for decision-making and programming in the fields of public health and nutrition. At the technical and operational levels, it has also presented a number of challenges. While the government pushed forward with developing a new strategy, a number of concerns need to be discussed, analyzed, and researched further. First, despite the country's high coverage of a 6-monthly vitamin A capsule supplementation program for children aged 6-59 months, one out of every five children suffer from VAD, with the highest prevalence among children living in slums. A 6- monthly high-dose vitamin A capsule can only generate a temporary and tiny rise in serum retinol that can last for approximately 2 months, according to many studies. Second, recent results on the relationship between groundwater natural Fe concentration and Fe status have posed new issues for public health programs. Due to varying Fe levels in groundwater, there is obvious variation in the frequency of Fe insufficiency across the Third, MNP programs for children aged 6-59 months should be carefully assessed to see if there is a need for adjustment in the composition of MNP, given the variety in the prevalence of Fe deficiency and IDA in the nation based on the most current micronutrient survey. Fourth, the USI program in Bangladesh is a fantastic example of an area where we know exactly what has to be done; nonetheless, despite considerable resources invested and an apparently strong commitment to execution, results have been less than the ideal nation. Finally, there is a discussion in Bangladesh and throughout the world over short/medium-term versus long-term approaches to addressing vitamin deficiencies. In the months and years ahead, it will be critical to keep a careful eye on the situation and ensure that the right combination of treatments is implemented using evidence-based methods. In food-related programs, it will become more vital to identify particular nutrition-related indicators, ensuring that interventions first recognize and then address specific dietary deficiencies, whether seasonal or for certain categories of individuals (e.g., age or wealth). Agriculture and horticulture programs that improve food quality and variety must be supplemented with supplements programs particularly tailored to alleviate nutritional inadequacies in the near term to suit the unique requirements of vulnerable populations.
Conclusions
While the severity of many micronutrient deficiencies has dropped dramatically in Bangladesh over the last several decades, a considerable fraction of the population, particularly children and women, remains deficient in important micronutrients. The review also demonstrated the implications of fortification of foods with vitamins and minerals essential for the health of individuals. Food fortification is a nutritional intervention program with a specified target demographic, and its success is determined by whether the fortified food is accepted, purchased, and eaten by the target population. Several intervention programs, particularly for vitamin A, Fe, and I deficiency, are in place to address the problem of micronutrient deficiencies. The success of these initiatives, on the other hand, is far from acceptable. Given the complex nature of the variables that contribute to micronutrient deficiencies in Bangladesh, as in other low-income countries, nutrient-specific nutrition policies and programs are unlikely to prevent and control micronutrient insufficiency. It's also vital to have enough resources and coordination between health and food sector employees, which is critical for assuring quality service delivery and accurate monitoring and reporting for improved results in terms of targeted groups' micronutrient status.
References
- Health Systems: Improving Performance. Geneva: World Health Organization. World Health Report (2000).
- Black RE. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371 (2008): 243-260.
- The global prevalence of vitamin A deficiency in populations at risk 1995-2005. WHO global database on vitamin A deficiency. Geneva: World Health Organization (2009): 55.
- Caulfield LE. The potential contribution of maternal zinc supplementation during pregnancy to maternal and child survival. Am Journal Clin Nutr 68 (1998): 499.
- Das JK. Micronutrient fortification of food and its impact on woman and child health: a systematic review. Systematic reviews 2 (2013): 67.
- Fortify to Address Sustainable Development Goals (2018).
- Kortman G. Nutritional iron turned inside out intestinal stress from a gut microbial perspective. FEMS Microbiol Rev 38 (2014): 1202-1204.
- Allen LD. Guidelines on Food Fortification with Micronutrients. Geneva, Switzerland: WHO and FAO (2006): 306.
- Fortified food: should we really be pumping bread with Vitamin D (2015).
- UN F.A.O. Food Fortification: Technology and Quality Control. Am J Clin Nutr 74 (1995): 108.
- Ahmed F. Micronutrient deficiencies among children and women in Bangladesh: progress and challenges. Journal of Nutritional Science 5 (2016): 1-12.
- Bhutta ZA. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost. Lancet 382 (2013): 452-477.
- ICDDR B. National Rickets Survey, Bangladesh 2008. ICDDR. Health and Science Bulletin 7 (2009): 7-11.
- What Are the Dangers of Fortified Foods and Supplements? (2013).
- Linpisarn S. Iron deficiency and anemia in children with a high prevalence of hemoglobinopathies: implications for screening. Int J Epidemiol 25 (1996): 1262-1265.
- Eneroth H. Maternal multiple micronutrient supplementation has a limited impact on the micronutrient status of Bangladeshi infants compared with standard iron-folic acid supplementation. Journal of Nutrition 140 (2010): 6-18.
- ICDDR B. GAIN (Global Alliance for Improved Nutrition), and UNICEF (United Nations Children’s Fund). The National Micronutrient Survey 2011-12. UNICEF (2014).
- Mason J. Vitamin A policies need rethinking. Int J Epidemiol 44 (2015): 283-292.
- Micronutrient deficiency- an underlying cause of morbidity and mortality. Bulletin of the World Health Organization 81 (2003).
- ICDDR B. International Centre for Diarrhoeal Diseases Research, Bangladesh, Global Alliance for Improved Nutrition (GAIN), The United Nations Children’s Fund (UNICEF). The National Micronutrients Status Survey (2013).
- Sahu SK. Malnutrition among under-five children in India and strategies for control. J Nat SciBiol Med 6 (2015): 28-30.
- Yusuf HK. National survey on iodine deficiency disorders and universal salt iodization survey of Bangladesh 2004-5. Dhaka: Institute of Public Health Nutrition (2007): 158.
- Zimmermann MB. The effect of iron fortification on the gut microbiota in African children: a ran domized control trial in Cote d’Ivoire. Am J Clin Nutr 32 (2010): 1406.
- Merrill RD. High prevalence of anemia with lack of iron deficiency among women in rural Bangladesh: a role for thalassemia and iron in groundwater. Asia Pac J Clin Nutr 21 (2012): 416-422.
- Bangladesh National Nutrition Survey 1995-96. Institute of Nutrition and Food Science, University of Dhaka (1998).
- Advances in metal-induced oxidative stress and human diseases. Toxicology (2013): 283.
- Rahman S. Determinants of iron status and Hb in the Bangladesh population: the role of groundwater iron. Public Health Nutr 19 (2016): 1862-1874.
