Follicular Unit Extraction (FUE) Hair Transplantation in Combination with Platelet Rich Plasma for the Treatment of Scarring Alopecia: A Case Series
Article Information
Suruchi Garg*, Ipsa Pandya, Sonali Bhatt
Aura Skin Institute, Chandigarh, India
*Corresponding Author: Suruchi Garg, Aura Skin Institute, Chandigarh, India
Received: 19 June 2019; Accepted: 11 July 2019; Published: 16 September 2019
Citation: Suruchi Garg, Ipsa Pandya, Sonali Bhatt. Follicular Unit Extraction (FUE) Hair Transplantation in Combination with Platelet Rich Plasma for the Treatment of Scarring Alopecia: A Case Series. Archives of Clinical and Medical Case Reports 3 (2019): 299-308.
View / Download Pdf Share at FacebookAbstract
Objective: To study the effect of addition of platelet rich plasma (PRP) to the hair transplantation for scarring alopecia.
Methods: An evaluation of the patients with detailed history, clinical examination and laboratory investigations was done. Routine baseline investigations and skin biopsy were done in order to rule out any activity of the underlying disease process. Freshly prepared Platelet rich plasma (PRP) using YCELL BIO kit was injected in freshly done slits over recipient area.
Results: A total of 4 cases were studied- A 26 years old male with cleft lip surgical scar with absent hair growth on the middle third of the upper lip, a 22 year old male with a 5 year old post traumatic depressed scar over the junction of medial and lateral third of the right eyebrow, a 17 year old boy with a post burn scar over his left upper lip and adjoining lower cheek area and a 55 years old post menopausal female, an already diagnosed and treated case of frontal fibrosing alopecia (FFA). Hair transplantation was performed with follicular unit extraction (FUE). Freshly prepared PRP was injected intradermally after creating the slits. In all the cases, there was a good survival rate of the healthy hair follicles, accompanied by improvement in the texture of the surrounding skin.
Conclusions: Platelet rich plasma, being a cocktail of growth factors, can bring vitality to the tissue and improve its vascularity, thus making it more receptive to the transplant. Additionally, with the improved vascularity of the recipient bed and activated fibroblasts, there is accelerated hair growth and better cosmetic outcomes of the scar.
Keywords
Hair Transplantation, Follicular Unit Extraction, Hair follicles
Hair Transplantation articles Hair Transplantation Research articles Hair Transplantation review articles Hair Transplantation PubMed articles Hair Transplantation PubMed Central articles Hair Transplantation 2023 articles Hair Transplantation 2024 articles Hair Transplantation Scopus articles Hair Transplantation impact factor journals Hair Transplantation Scopus journals Hair Transplantation PubMed journals Hair Transplantation medical journals Hair Transplantation free journals Hair Transplantation best journals Hair Transplantation top journals Hair Transplantation free medical journals Hair Transplantation famous journals Hair Transplantation Google Scholar indexed journals Follicular Unit Extraction articles Follicular Unit Extraction Research articles Follicular Unit Extraction review articles Follicular Unit Extraction PubMed articles Follicular Unit Extraction PubMed Central articles Follicular Unit Extraction 2023 articles Follicular Unit Extraction 2024 articles Follicular Unit Extraction Scopus articles Follicular Unit Extraction impact factor journals Follicular Unit Extraction Scopus journals Follicular Unit Extraction PubMed journals Follicular Unit Extraction medical journals Follicular Unit Extraction free journals Follicular Unit Extraction best journals Follicular Unit Extraction top journals Follicular Unit Extraction free medical journals Follicular Unit Extraction famous journals Follicular Unit Extraction Google Scholar indexed journals Hair follicles articles Hair follicles Research articles Hair follicles review articles Hair follicles PubMed articles Hair follicles PubMed Central articles Hair follicles 2023 articles Hair follicles 2024 articles Hair follicles Scopus articles Hair follicles impact factor journals Hair follicles Scopus journals Hair follicles PubMed journals Hair follicles medical journals Hair follicles free journals Hair follicles best journals Hair follicles top journals Hair follicles free medical journals Hair follicles famous journals Hair follicles Google Scholar indexed journals health articles health Research articles health review articles health PubMed articles health PubMed Central articles health 2023 articles health 2024 articles health Scopus articles health impact factor journals health Scopus journals health PubMed journals health medical journals health free journals health best journals health top journals health free medical journals health famous journals health Google Scholar indexed journals environment articles environment Research articles environment review articles environment PubMed articles environment PubMed Central articles environment 2023 articles environment 2024 articles environment Scopus articles environment impact factor journals environment Scopus journals environment PubMed journals environment medical journals environment free journals environment best journals environment top journals environment free medical journals environment famous journals environment Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals tissue articles tissue Research articles tissue review articles tissue PubMed articles tissue PubMed Central articles tissue 2023 articles tissue 2024 articles tissue Scopus articles tissue impact factor journals tissue Scopus journals tissue PubMed journals tissue medical journals tissue free journals tissue best journals tissue top journals tissue free medical journals tissue famous journals tissue Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals platelets articles platelets Research articles platelets review articles platelets PubMed articles platelets PubMed Central articles platelets 2023 articles platelets 2024 articles platelets Scopus articles platelets impact factor journals platelets Scopus journals platelets PubMed journals platelets medical journals platelets free journals platelets best journals platelets top journals platelets free medical journals platelets famous journals platelets Google Scholar indexed journals corticosteroids articles corticosteroids Research articles corticosteroids review articles corticosteroids PubMed articles corticosteroids PubMed Central articles corticosteroids 2023 articles corticosteroids 2024 articles corticosteroids Scopus articles corticosteroids impact factor journals corticosteroids Scopus journals corticosteroids PubMed journals corticosteroids medical journals corticosteroids free journals corticosteroids best journals corticosteroids top journals corticosteroids free medical journals corticosteroids famous journals corticosteroids Google Scholar indexed journals
Article Details
1. Introduction
Healthy hair on the scalp is an expression of one’s identity, wellbeing and self-image. Hair loss or alopecia may result in considerable psychological disturbances and low self-esteem. Alopecia is categorized into scarring/cicatricial and nonscarring/noncicatricial forms. Cicatricial alopecia includes various disorders characterized by the complete and irreversible destruction of the hair follicles. Scarring is invariably associated with cicatricial alopecia and hair transplantation is an important reconstructive method for scar camouflage as well as hair restoration. In this case series it has been shown that the addition of platelet rich plasma (PRP) to the hair restoration surgeries for scar camouflage increases the survival rate of the transplanted hair by its direct action on the hair follicle stem cells and also has an indirect positive effect on the survival of transplanted hair grafts by improving environment of the surrounding scar tissue.
1.1 Preoperative work up
All the patients enrolled in the study were evaluated with detailed history, clinical examination and laboratory investigations. They were given baseline investigations like complete hemogram, renal function tests, liver function tests, fasting blood sugar, vitamin D, vitamin B12, thyroid function tests, Iron studies and lipid profile. Skin biopsy was done in order to rule out any activity of underlying disease process if applicable.
1.2 Preparation of PRP
Platelet rich plasma was freshly prepared using YCELL BIO kit during the surgery. Twenty ml of whole blood was collected from the antecubital vein. Two PRP kits each containing 1.5 ml acid citrate dextrose A (ACDA) anticoagulant solution were mixed with 10 ml blood each and processed in a centrifuge. Single spin at 3200 rpm for 4 min was done following which buffy coat along with PRP was harvested. Thus, 3 ml PRP was collected from each PRP kit. After the creation of the slits, 0.2-0.3 ml PRP was injected in freshly done slits over recipient area by an insulin syringe at a gap of 1cm each to a level of deep dermis. No activator was used as the blood oozing from these sites itself acted as stimulus for the degranulation of platelets.
2. Case 1-Post Cleft Lip Surgery Scar
A 26 years old male came to us with cleft lip surgical scar with associated irregularity and retraction of the lip border as shown in the figure (Figure 1). He had ample hair on his upper lip moustache except on the middle third of the upper lip, literally accentuating the surgical scar. This had led to low self-esteem, thereby affecting his quality of life. After analyzing the rest of the moustache, approximately 70% of the usual moustache hair density was transplanted to the scarred area. Hair transplantation was performed with follicular unit extraction (FUE) technique under local anesthesia. The submental beard region was selected as the donor area so as to obtain hair of similar quality as that of the hair on the upper lip. The density given was 35-40 FU/cm2 keeping in mind that 40-60/cm2 is the natural density of moustache. After local anesthesia in the beard area about 150 FU grafts were extracted using the Harris SAFE system. These grafts were kept in chilled ringer lactate solution. Eighteen gauge needles were employed to create 150 small, closely spaced slits at the recipient site keeping in mind the natural direction and angle of the hair in the upper lip. Freshly prepared PRP was injected intradermally after creating the slits.

Figure 1: Cleft lip surgical scar (Pre-treatment).

Figure 2: Cleft lip surgical scar (Five months post-treatment).
Finally, the grafts were placed into the recipient slits using jeweler’s forceps. The second figure (Figure 2) shows the 5 months post-operative picture of the patient with cleft lip scar showing growth and good survival rate of the healthy hair follicles which had completely camouflaged the previous scar area. The scar tissue is not an ideal ground for graft survival, so often it is difficult to accomplish good results with a single-session of transplantation. However, growth factors enriched PRP injection into scarred upper lip in the same sitting with hair transplantation helped to solve this problem. There was also an associated improvement in the lip volume, lip irregularity and the skin texture across the right upper lip. The probable explanation is the presence of growth factors in PRP leading to neocollagen formation and angiogenesis, thereby improving the overall contour of the lip. To the best of our knowledge, this is the first case report of cleft lip hair transplantation using FUE technique in combination with PRP.
3. Case 2-Post Traumatic Eyebrow Scar
A 22 year old male presented to us with a post traumatic depressed scar over the junction of medial and lateral third of the right eyebrow (Figure 3), which was present since 5 years. To camouflage the scar, hair transplantation was planned with FUE technique. Under local anesthesia about 50 FU grafts were taken from the temporal area of the scalp. This area was chosen as temporal hair is considered closest to eyebrow hair in their characteristic. A 21G hypodermic needle was used for creating 50 slits in the recipient scarred site. This was followed by the injection of PRP into the recipient area. The grafts were then carefully implanted into the recipient sites with a density of 30-40 FU/cm2. After 5 months, the patient showed almost complete growth of hair follicles camouflaging the scar completely (Figure 4). There was a visible improvement in the texture and quality of the scar also. These results could be attributed to the various growth factors in PRP which improved the vascularity of the recipient bed and activated fibroblasts, resulting in accelerated hair growth and better cosmetic outcomes of the scar. This is the first case report describing the successful eyebrow hair restoration surgery for post traumatic scar performed in conjunction with PRP.

Figure 3: Post traumatic scar (Pre- treatment).

Figure 4: Post traumatic scar (Six months post-treatment).
4. Case 3-Post Burn Scar
A 17 year old boy came to us with a post burn scar over his left upper lip and adjoining lower cheek area (Figure 5). The scar was pigmented and atrophic with abrupt margins. Rest of the upper lip was covered with the low density of moustache hair. The scar had a significant negative effect on the self-image of the patient and he had dropped out of school due to the same distress. We planned hair transplantation along with PRP in this patient. About 125 follicular units (FU) were extracted from the temporal area as sub mental area was not very strong and slits were made using 18 gauge needles. Recipient incisions were made oblique due to scant underlying dermal tissue and PRP was injected into the recipient area, followed by transplantation of grafts into the slits at a density of 20-30 FU/cm2. After 3 months, the reconstructed moustache had a complete natural appearance, and the patient was very satisfied (Figure 6). The fibrotic scar tissue resulting after burn injuries usually is not an ideal ground for hair grafting due to scanty blood supply. However, the addition of growth factors from PRP not only aided the growth of transplanted hair follicles but also improved the quality of the atrophic scar. The scar texture became more elastic as well as pliable and the color more closely resembled that of the surrounding healthy skin. The quality of the new hair, as expected, was slightly different than the original hair in terms of the texture and direction of growth. This, however, did not significantly change the appearance of the area and overall it looked much better than before. We also planned for 3 sessions of pixel Erbium-YAG laser to resurface the adjoining burnt skin.

Figure 5: Post burn scar moustache (Pre-treatment).

Figure 6: Post burn scar moustache (Three months post treatment).
5. Case 4- Frontal Fibrosing Alopecia Hair Transplantation
A 55 years old post menopausal female presented to us with bilaterally symmetric fronto- temporal hairline recession extending as far as the retro auricular region, with loss of follicular orifices and uniform smoothness of the skin with few violaceous patches (Figure 7). There was no involvement of other body areas. She was already a diagnosed and treated as a case of frontal fibrosing alopecia (FFA) from outside. She was in her disease free period for last 3 years. Hair transplantation in the affected area was planned after disease inactivity was proven histopathologically. Two thousand follicular units were transplanted using the FUE technique in the frontal and temporal hairline at a low density of 25-30 FU/cm2. This was combined with PRP injection in the same sitting. The transplanted hair grafts survived and grew well after 8 months as can be seen in the picture (Figure 8). In the follow up period, no disease activity in the form of itching, erythema or hair loss was noted at the recipient site.

Figure 7: Frontal fibrosing alopecia (Pre-treatment).

Figure 8: Frontal fibrosing alopecia (Eight months post-treatment).
6. Cicatricial Alopecia
CicatricialAlopecias (CA) consist of a diverse group of inflammatory hair disorders characterized by irreversible loss of hair, thereby having a negative impact on the self-esteem of the patient. Clinically, there is effacement of follicular orifices which is occasionally accompanied by epidermal atrophy. Histologically, there is replacement of the pilosebaceous structures by fibrotic stellae along with either hyalinization or fibrosis of the surrounding collagen
Cicatricial alopecias are divided into two groups as “primary” and “secondary” cicatricial alopecias. In primary cicatricial alopecia, the hair follicle is the primary target of the destructive inflammatory process leading to permanent loss of hair. There is destruction of the stem cells in the bulge area of the hair follicle [2]. In secondary cicatricial alopecias, the hair follicle is destroyed as a part of a generalized inflammatory process which also involves the surrounding skin and its appendages. This ultimately destroys the hair follicle stem cell based capacity for regeneration [3, 4].
6.1 Hair transplantation in cicatricial alopecia
Hair transplant comprises of harvesting hair from a donor area in the form of either a single strip or individual follicular units (Follicular unit extraction [FUE]) and grafting them into the recipient site. The availability of donor hair can sometimes be a limiting factor, but FUE offers the advantage of using hair from areas such as the beard, chest or other hairy sites when needed [5-7]. Hair transplant in cicatricial alopecia can be challenging owing to thin skin, lack of vasculature and sometimes subcutis also which otherwise is essential to hold the grafts and provides nutrients to transplanted follicles [6]. Secondary cicatricial alopecia is usually stable, whereas primary cicatricial alopecia, due to ongoing inflammatory processes, can be unstable. A biopsy, therefore, is mandatory to ensure lack of disease activity. It is imperative to counsel the patient for the occurrence of reactivation of the disease before performing a hair transplant [6, 8]. The recommendation is to wait for a period of at least one year or more when the patient is off medications and there are no signs of disease activity [8, 9].
One of the precautions to be taken into account when performing a hair transplant on scarred tissue is that the density of transplanted follicles should be less than that of normal scalp transplant (30-40 units/cm2), because of the risk of follicles competing for the reduced blood flow through the scar tissue. Areas with a compromised blood supply should have a density of at most 15-20 FU/cm2 [1, 8]. We believe that since PRP promotes angiogenesis, thereby significantly increasing the blood circulation around hair follicles, we can extend this number up to 20-40 FU/cm2 depending upon the density of recipient area by combining hair transplant with PRP. There are many limitations to the success of hair transplantation in cicatricial alopecia like disproportionate donor-recipient area ratio, decreased survival of hair grafts due to reduced vascular supply, and the possibility of relapses of the disease process leading to new areas of scarring alopecia [4].
6.2 PRP in cicatricial alopecia
The first cells to arrive at the site of tissue injury are platelets [10]. They are the most active in the early inflammatory phases of the healing process. Platelets, after degranulation, release platelet-derived growth factor (PDGF), transforming growth factor-β1 (TGF-β1), vascular endothelial growth factor (VEGF), basic fibroblastic growth factor (bFGF), and epidermal growth factor (EGF) from alpha granules [11-14]. With the help of these granules, they mediate homeostasis, through cell membrane adherence, aggregation, clot formation, and release of substances that promote tissue repair and reactivity of blood vessels and blood cells in angiogenesis and inflammation [15, 16]. Platelet derived growth factor is chemotactic for fibroblasts. Growth factors like TGF, EGF and VEGF help in mediating angiogenesis. Moreover, EGF is also mitogoneic for fibroblasts, endothelial cells and keratinocytes. Additionally, FGF and HGF (Hepatocytic growth factor) also help in tissue remodeling and regeneration. With this cocktail of growth factors, PRP can play a pivotal role in the remodeling of scarred tissue [17].
Scarred tissue is a poor graft recipient due to compromised blood supply. The percentage of grafted follicles that survive depends to a great extent on the blood supply of the vascular bed. PRP, being a rich source of anagen-maintaining factors such as insulin-like growth factor 1 (IGF-1), basic fibroblast growth factor (bFGF), and vascular endothelial growth factor (VEGF), has shown to improve the ischaemic tissue and considerably increase the blood flow around the hair follicles [6]. In the bulge area of the hair follicle (HF), primitive stem cells of ectodermal origin are found which express a protein called nephronectin which is known to mediate the interactions with the receptor α8β1 integrin, which is expressed in Dermal Papillae (DP) and arrectorpili muscle (APM ) which are mesenchymal in origin [18].
It is believed that the deposition of nephronectin in basement membrane creates a unique niche leading to a series of signals, causing, ‘the lock and key’ attachment between bulge region of ectodermal HF and mesenchymal APM and again lower portion of ectodermal hair follicle and mesenchymal DP. Here the basement membrane, stem cells & bulge portion of APM may prove as a “golden anchorage” for HF survival and integrity. Growth factors from PRP act on all these targets and contribute towards hair follicle integrity and survival (Figure 9) [19]. The interactions between the cells of DP and Bulge area as well as with binding growth factors (PDGF, TGF-β, and VEGF) activate the proliferative phase of the hair, giving rise to the future follicular unit [20]. Akdaq et al. had combined follicular unit extraction and autologous fat grafting for camouflaging cleft lip scar. Twenty patients who had both a scar and alopecia in the cleft lip were studied. They underwent fat grafting from the periumblical region and hair transplantation was done three months after the fat injection, with hair from the submental area and scalp. Patients were followed for 12 months. The scar was hidden well and overall patient and observer satisfaction was very good [21].
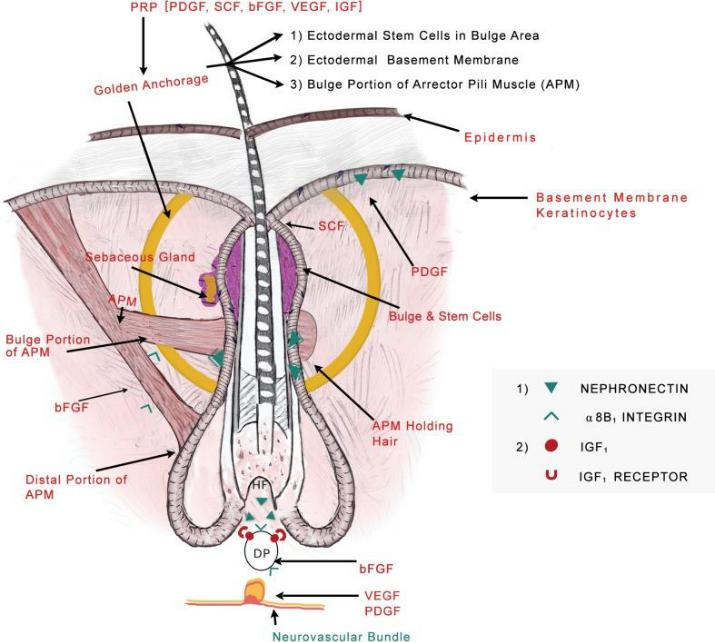
Figure 9: The Hair model showing Golden anchorage and molecular locking and also highlighting the role of various growth factors in PRP working on various levels to enhance hair follicle integrity and survival [19].
In an Indian study by Rajput RJ, 18 cases of cleft palate were given moustache restoration using FUE. Hair growth along the scar began 4-5 months after the transplant, and complete growth was seen by 6 months along with loss of 7-10% grafts. Hair growth in our study began at the end of 2 months and complete growth was attained by 5-6 months [22]. Malek et al. did a comparative study of PRP and silicone preparations in cases having post burn scars. Intradermal injections of PRP were given monthly for 3 months to one group and the other group was given silicone based products for local application. At the end of 3 months, response by intralesional PRP injection was found to be better than that by Silicone-based products, especially in terms of itching, pigmentation and pliability [23]. Similar improvement was also observed in our study of the post burn scar when the adjoining skin improved in texture, colour and pliability. Saxena et al. combined scalp and beard hair transplant along with platelet rich plasma in histologically proven case of lichen planopilaris. They worked on a test patch initially. After 10 months of the success in the test patch, the remaining patches were covered by FUE hair grafts from the beard and the scalp. Five mL of PRP was injected in all recipient patches. Eighty percent of the transplanted grafts from the scalp as well as from the beard area survived and showed optimal growth [6].
The limitation of our study is that there was no objective evaluation of the hair follicles that survived after the transplant. However, follow-up at 2 weeks post-transplant showed approximately more than 95% actively growing grafts and there were no overtly visible gaps in the treated areas after 6 months. The patient satisfaction was high and there was no need for a revision surgery in any of these cases.
7. Conclusion
The degenerative changes & reduced vascularity of the scarred tissue impose a considerable challenge for the growth of new hair on it. Platelet rich plasma, with the cocktail of growth factors, can bring vitality to the tissue and improve its vascularity, thus making it more receptive to the transplant. This study paves way for further studies to investigate the role of PRP as a potential adjuvant to hair transplant in cases of scarring alopecia.
References
- Kutlubay Z, Murat K, Engin B. Hair transplantation in the cicatricial alopecias. Hair Ther Transplant 3 (2013): 109.
- Ohyama M. Primary cicatricial alopecia: Recent advances in understanding and management. J Dermatol 39 (2012): 18-26.
- Paus R, Olsen E, Messenger A. Hair growth disorders. In Eds.: Wolff K, Goldsmith LA, Katz SI, et al. Fitzpatrick’s Dermatology in General Medicine. (7th Edn) New York: McGraw-Hill (2008): 753.
- Dogra S, Sarangal R. What’s new in cicatricial alopecia? Indian J Dermatol Venereol Leprol 79 (2013): 576-590.
- Meyer-Gonzalez T, Bisanga C. Body-hair transplant for cicatricial alopecia. Actas Dermosifiliogr 103 (2012): 163-165.
- Saxena K, Saxena DK, Savant SS. Successful hair transplant outcome in cicatricial lichen planus of the scalp by combining scalp and beard hair along with platelet rich plasma. J Cutan Aesthet Surg 9 (2016): 51-55.
- Dahdah MJ, Iorizzo M. The Role of Hair Restoration Surgery in Primary Cicatricial Alopecia. Skin Appendage Disorders 2 (2016): 57-60.
- Unger W, Unger R, Wesley C. The surgical treatment of cicatricial alopecia. Dermatol Ther 21 (2008): 295-311.
- Saxena K, Savant SS. Body to scalp: Evolving trends in body hair transplantation. Indian Dermatol Online J 8 (2017): 167-175.
- Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res 37 (2009): 1528-1542.
- Frechette JP, Martineau I, Gagnon G. Platelet-rich plasmas: growth factor content and roles in wound healing. J Dent Res 84 (2005): 434-439.
- Eppley BL, Woodell JE, Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. Plast Reconstr Surg 114 (2004): 1502-1508.
- Kazakos K, Lyras DN, Verettas D, et al. The use of autologous PRP gel as an aid in the management of acute trauma wounds. Injury 40 (2009): 801-805.
- Cole BJ, Seroyer ST, Filardo G, et al. Platelet-Rich Plasma: Where Are We Now and Where Are We Going? Sports Health 2 (2010): 203-210.
- Borregaard N, Cowland JB. Granules of the human neutrophilic polymorphonuclear leukocyte. Blood 89 (1997): 3503-3521.
- Murphy G, Bretz U, Baggiolini M, et al. The latent collagenase and gelatinase of human polymorphonuclear neutrophil leucocytes. Biochem J 192 (1980): 517-525.
- Arshdeep, Kumaran M Platelet-rich plasma in dermatology: Boon or a bane?. Indian J Dermatol Venereol Leprol 80 (2014): 5-14.
- Fujiwara H, Ferreira M, Donati G, et al. The basement membrane of hair follicle stem cells is a muscle cell niche. Cell 144 (2011): 577-589.
- Garg S, Manchanda S. Platelet-rich plasma-an “Elixir” for treatment of alopecia: personal experience on 117 patients with review of literature. Stem Cell Investigation 4 (2017): 64.
- Gentile P, Garcovich S, Bielli A, et The Effect of Platelet-Rich Plasma in Hair Regrowth: A Randomized Placebo-Controlled Trial. Stem Cells Transl Med 4 (2015): 1317-1323.
- Akdag O, Evin N, Karamese M, et al. Camouflaging Cleft Lip Scar Using Follicular Unit Extraction Hair Transplantation Combined With Autologous Fat Grafting. Plast Reconstr Surg 141 (2018): 148-151.
- Rajput RJ. Moustache restoration after cleft lip repair. J Cleft Lip Palate Craniofac Anomal 2 (2015): 129-132.
- Malek E, Mohamed AM, Amr M, et al. Evaluation of the Effect of Platelet-Rich Plasma on Post-Burn Scars. Open Access J Surg 5 (2017).
