Fluoroscopic Defecography Characterization of Floppy Pouch Complex with Clinical and Endoscopic Correlations
Article Information
Hong Yun Ma1*, Hyunjoong William Kim1, Sakshi Khurana1, Stuart Bentley-Hibbert1, Bo Shen2
1Department of Radiology, New York-Presbyterian/Columbia University Irving Medical Center, New York, NY
2Center for Inflammatory Bowel Diseases/Division of Colorectal Surgery; Columbia University Irving Medical Center, New York, NY
*Corresponding Author: Hong Yun Ma. Department of Radiology, Columbia University, Irving Medical Center,622 W 168th Street, New York, New York 10032
Received: 12 December 2023; Accepted: 20 December 2023; Published: 17 January 2024
Citation:
Hong Yun Ma, Hyunjoong William Kim, Sakshi Khurana, Stuart Bentley-Hibbert, Bo Shen. Fluoroscopic Defecography Characterization of Floppy Pouch Complex with Clinical and Endoscopic Correlations. Journal of Radiology and Clinical Imaging 7 (2024): 01-08.
View / Download Pdf Share at FacebookAbstract
Background: For patients with medically refractory ulcerative colitis, proctocolectomy with ileal pouch-anal anastomosis is often performed. This surgery generally improves the quality of life for patients but there are also many pouch-associated complications, including but not limited to infections/inflammations, leaks, fistulas, neoplasia, and obstruction. A new emerging disease category for patients with ileal pouches is known as floppy pouch complex (FPC), which is obstruction resulting from a redundant pouch or loop of bowel. Dynamic fluoroscopic defecography is a common tool for diagnosing structural and functional complications of the pouch. We aimed to provide image-rich case-based radiologic characterization of FPC as well as related pouch-associated complications.
Methods: All patients with a J-pouch who presented for at least one dynamic fluoroscopic defecography examination at our institution were included in the study. Fluoroscopic defecography images were re-interpreted and systematically classified by three radiologists. Retrospective chart review was performed to gather additional data. The diagnosis of FPC, including afferent limb syndrome, pouch intussusception, pouch prolapse, Pouchcele, and pouch twist, was confirmed clinically, endoscopically and/ or fluoroscopically, which were characterized radiographically.
Results: There were 94 patients who underwent 98 dynamic fluoroscopic defecography between December 2013 and November 2022. Average duration of pouch in our patient cohort was 10 years at the time of the fluoroscopic defecography. A total of 77 patients (79%) were not able to completely expel the contrast from the J-pouch. Approximately 73% of examinations demonstrated at least one abnormal categorizable imaging finding and 35% of examinations demonstrated two or more abnormalities. The most common imaging findings seen on fluoroscopic defecography were Pouchcele (N = 27; 28.6%), pouch prolapse (N = 21; 22.3%), and afferent limb abnormalities (N=14; 14.9%).
Conclusion: Most fluoroscopic defecography examinations in patients with J-pouch were abnormal, some with multiple abnormalities. Most common J-pouch dysfunctions captured on fluoroscopic defecography include Pouchcele, pouch prolapse, afferent limb angulation, and stricture. Fluoroscopic defecography provides real-time evaluation of pelvic pouchpouch with true temporal resolution, which plays a unique role in aiding the diagnosis of floppy Pouch Complex.
Keywords
Endoscopy, Familial adenomatous polyposis, Floppy Pouch Complex, Ileal pouch-anal anastomosis, Imaging, Restorative proctocolectomy, Ulcerative colitis.
Endoscopy articles; Familial Adenomatous Polyposis articles; Floppy Pouch Complex articles; Ileal Pouch-Anal Anastomosis articles; Imaging articles; Restorative Proctocolectomy articles; Ulcerative Colitis articles.
Endoscopy articles Endoscopy Research articles Endoscopy review articles Endoscopy PubMed articles Endoscopy PubMed Central articles Endoscopy 2023 articles Endoscopy 2024 articles Endoscopy Scopus articles Endoscopy impact factor journals Endoscopy Scopus journals Endoscopy PubMed journals Endoscopy medical journals Endoscopy free journals Endoscopy best journals Endoscopy top journals Endoscopy free medical journals Endoscopy famous journals Endoscopy Google Scholar indexed journals Familial adenomatous polyposis articles Familial adenomatous polyposis Research articles Familial adenomatous polyposis review articles Familial adenomatous polyposis PubMed articles Familial adenomatous polyposis PubMed Central articles Familial adenomatous polyposis 2023 articles Familial adenomatous polyposis 2024 articles Familial adenomatous polyposis Scopus articles Familial adenomatous polyposis impact factor journals Familial adenomatous polyposis Scopus journals Familial adenomatous polyposis PubMed journals Familial adenomatous polyposis medical journals Familial adenomatous polyposis free journals Familial adenomatous polyposis best journals Familial adenomatous polyposis top journals Familial adenomatous polyposis free medical journals Familial adenomatous polyposis famous journals Familial adenomatous polyposis Google Scholar indexed journals Floppy Pouch Complex articles Floppy Pouch Complex Research articles Floppy Pouch Complex review articles Floppy Pouch Complex PubMed articles Floppy Pouch Complex PubMed Central articles Floppy Pouch Complex 2023 articles Floppy Pouch Complex 2024 articles Floppy Pouch Complex Scopus articles Floppy Pouch Complex impact factor journals Floppy Pouch Complex Scopus journals Floppy Pouch Complex PubMed journals Floppy Pouch Complex medical journals Floppy Pouch Complex free journals Floppy Pouch Complex best journals Floppy Pouch Complex top journals Floppy Pouch Complex free medical journals Floppy Pouch Complex famous journals Floppy Pouch Complex Google Scholar indexed journals Ileal pouch-anal anastomosis articles Ileal pouch-anal anastomosis Research articles Ileal pouch-anal anastomosis review articles Ileal pouch-anal anastomosis PubMed articles Ileal pouch-anal anastomosis PubMed Central articles Ileal pouch-anal anastomosis 2023 articles Ileal pouch-anal anastomosis 2024 articles Ileal pouch-anal anastomosis Scopus articles Ileal pouch-anal anastomosis impact factor journals Ileal pouch-anal anastomosis Scopus journals Ileal pouch-anal anastomosis PubMed journals Ileal pouch-anal anastomosis medical journals Ileal pouch-anal anastomosis free journals Ileal pouch-anal anastomosis best journals Ileal pouch-anal anastomosis top journals Ileal pouch-anal anastomosis free medical journals Ileal pouch-anal anastomosis famous journals Ileal pouch-anal anastomosis Google Scholar indexed journals Imaging articles Imaging Research articles Imaging review articles Imaging PubMed articles Imaging PubMed Central articles Imaging 2023 articles Imaging 2024 articles Imaging Scopus articles Imaging impact factor journals Imaging Scopus journals Imaging PubMed journals Imaging medical journals Imaging free journals Imaging best journals Imaging top journals Imaging free medical journals Imaging famous journals Imaging Google Scholar indexed journals Ulcerative colitis articles Ulcerative colitis Research articles Ulcerative colitis review articles Ulcerative colitis PubMed articles Ulcerative colitis PubMed Central articles Ulcerative colitis 2023 articles Ulcerative colitis 2024 articles Ulcerative colitis Scopus articles Ulcerative colitis impact factor journals Ulcerative colitis Scopus journals Ulcerative colitis PubMed journals Ulcerative colitis medical journals Ulcerative colitis free journals Ulcerative colitis best journals Ulcerative colitis top journals Ulcerative colitis free medical journals Ulcerative colitis famous journals Ulcerative colitis Google Scholar indexed journals Restorative proctocolectomy articles Restorative proctocolectomy Research articles Restorative proctocolectomy review articles Restorative proctocolectomy PubMed articles Restorative proctocolectomy PubMed Central articles Restorative proctocolectomy 2023 articles Restorative proctocolectomy 2024 articles Restorative proctocolectomy Scopus articles Restorative proctocolectomy impact factor journals Restorative proctocolectomy Scopus journals Restorative proctocolectomy PubMed journals Restorative proctocolectomy medical journals Restorative proctocolectomy free journals Restorative proctocolectomy best journals Restorative proctocolectomy top journals Restorative proctocolectomy free medical journals Restorative proctocolectomy famous journals Restorative proctocolectomy Google Scholar indexed journals Crohn’s disease articles Crohn’s disease Research articles Crohn’s disease review articles Crohn’s disease PubMed articles Crohn’s disease PubMed Central articles Crohn’s disease 2023 articles Crohn’s disease 2024 articles Crohn’s disease Scopus articles Crohn’s disease impact factor journals Crohn’s disease Scopus journals Crohn’s disease PubMed journals Crohn’s disease medical journals Crohn’s disease free journals Crohn’s disease best journals Crohn’s disease top journals Crohn’s disease free medical journals Crohn’s disease famous journals Crohn’s disease Google Scholar indexed journals efferent limb syndrome articles efferent limb syndrome Research articles efferent limb syndrome review articles efferent limb syndrome PubMed articles efferent limb syndrome PubMed Central articles efferent limb syndrome 2023 articles efferent limb syndrome 2024 articles efferent limb syndrome Scopus articles efferent limb syndrome impact factor journals efferent limb syndrome Scopus journals efferent limb syndrome PubMed journals efferent limb syndrome medical journals efferent limb syndrome free journals efferent limb syndrome best journals efferent limb syndrome top journals efferent limb syndrome free medical journals efferent limb syndrome famous journals efferent limb syndrome Google Scholar indexed journals Floppy pouch complex articles Floppy pouch complex Research articles Floppy pouch complex review articles Floppy pouch complex PubMed articles Floppy pouch complex PubMed Central articles Floppy pouch complex 2023 articles Floppy pouch complex 2024 articles Floppy pouch complex Scopus articles Floppy pouch complex impact factor journals Floppy pouch complex Scopus journals Floppy pouch complex PubMed journals Floppy pouch complex medical journals Floppy pouch complex free journals Floppy pouch complex best journals Floppy pouch complex top journals Floppy pouch complex free medical journals Floppy pouch complex famous journals Floppy pouch complex Google Scholar indexed journals
Article Details
Abbreviations:
ALS afferent limb syndrome
ARM anorectal manometry
BD barium defecography
CD Crohn’s disease
ELS efferent limb syndrome
FAP Familial adenomatous polyposis
FPC Floppy pouch complex
IPAA Ileal pouch anal anastomosis
PCL Pubococcygeal line
UC Ulcerative colitis
IBD Inflammatory bowel disease
1. Introduction
For patients with medically refractory ulcerative colitis (UC), UC with neoplasia, or familial adenomatous polyposis, the mainstay of treatment is restorative total proctocolectomy with ileal pouch-anal anastomosis (RPC-IPAA) [1]. Approximately 15-25% ulcerative colitis patients will have total colectomy with pouch creation in their life [2]. There are various types of ileo-anal anastomoses, including J, S, and W pouches. J-pouch is the most convenient for both patients and surgeons [3]. While RPC and IPAA significantly improve the patients’ quality of life, complications are common. Structural, inflammatory, and functional disorders are seen often in pouch-created patients [4-7]. The common complications after J pouch surgery include leakage from the pouch (anastomotic leak, pouch fistulas), infection (abscess), stricture/narrowing of the J-pouch, and inflammation of the J-pouch (cuffitis or pouchitis) [1]. These complications can be diagnosed by the combination of symptoms, physical examination, pouchscopy, and imaging studies such as contrast enema, CT or MRI with or without the use of rectal contrast. An emerging disease category for patients with ileal pouches is known as Floppy Pouch Complex (FPC), which is obstruction due to pouch prolapse, Pouchcele, afferent limb syndrome, and/or abnormal pouch folding/twisting. The risk factors for floppy pouch complex are lower body weight and lower BMI and family history of inflammatory bowel disease [2]. Other factors include smoking history, excessive alcohol consumption, the type of surgery J-pouch versus S or W pouch, age at inflammatory bowel disease (IBD) diagnosis, and age at pouch constriction. However, stages of pouch surgery did not have associated risk factors with floppy pouch complex [2]. Fluoroscopy defecography is a diagnostic imaging technique that is used to evaluate problems with bowel movements, including evaluating for J-pouch complications. It is a complementary diagnostic method for the diagnosis of FPC, which can evaluate the function of the J-pouch in real-time. It allows the radiologist to observe the functions of the J-pouch, anus, and indirectly the pelvic floor muscles in real-time. Subsequently, these stored fluoroscopic images can be used to identify any problems that may be causing symptoms such as constipation, fecal incontinence, or incomplete evacuation of the J-pouch. It is a safe and effective procedure that can provide valuable information for the diagnosis and treatment of pouch disorders. MRI defecography has similar functions, but it is more expensive and time consuming. Fluoroscopic defecography is more realistic due to the patient’s sitting position. However, fluoroscopic diagnosis for Floppy Pouch Complex is not well recognized by radiologists and clinicians alike. The aim of this study is to characterize FPC on fluoroscopic defecography.
2. Patients and Methods
2.1 Data source
All patients with a J-pouch who presented for at least one dynamic fluoroscopic defecography examination at NewYork-Presbyterian/Columbia University Irving Medical Center were included in the study; MModal Catalyst was used to extract the initial data. Patients who underwent dynamic fluoroscopic defecography studies between December 2013 and November 2022 were selected. Fluoroscopic defecography images were re-interpreted by three radiologists. The findings were categorized in a systematic manner. Additional medical histories, clinical visits notes, operation records, pouchscopy results and other medical records were also carefully reviewed and classified. Representative fluoroscopic images were then used to highlight the various pathologies. All J pouch surgery patients with post-surgical fluoroscopic defecography were included in this study. Patients with partial colectomy, S or W pouch surgery were not included in this study.
2.2 Fluoroscopy techniques
No bowel preparation is necessary before the fluoroscopy defecography procedure. Patient changes into a hospital gown and was instructed to empty the bladder prior to the examination. Only radiologists who perform the study with a chaperone are allowed in the fluoro-room to provide privacy for patients. After the patient lies in the left lateral decubitus position on the table, approximately 120-240 mL high density barium paste contrast material (usually barium sulfate) is instilled into the J-pouch via rectal tube. The radiologist can obtain a quick fluoroscopic image to check the contrast volume after administration. It is critical to insert enough contrast paste to opacify the pouch to see the pouch inlet. Radiopaque markers, such as a nipple marker, may be placed on the skin surrounding the anus as a landmark; however, it is not usually helpful. Once contrast paste has been administered, the patient sits on the portable radiolucent commode between the x-ray tube and the image intensifier and covered with a shade for maximum privacy. Spot image is first obtained at rest. Under fluoroscopic observation, the patient performs three maneuvers, which are Kegel, Vasava, and evacuation of the contrast. Cine and spot images are obtained to record each of these maneuvers. Post-evacuation spot image is obtained to look for residual contrast. The whole procedure takes approximately 20 minutes. The fluoroscopy time is approximately 30-60 seconds, a little bit of variation case-by-case.
2.3 Normal appearance of the J-pouch
Normal J-pouch is approximately 10 cm in length with capacity approximately 180-240 ml. However, it is variable due to the operative techniques. At rest, the anal canal should be closed. Patients should not have any contrast leaking at the rest, Kegel or Vasava phases. The pelvic floor should be at or above the level of the PCL line. The afferent limb-pouch anastomotic site and ileoanal anastomotic sites should be widely patent. The anorectal junction (ARJ) and anorectal angle (ARA) are normally present due to most patients' reserve minimal rectal cuff. The changes of anorectal angles during Kegel, Vasava maneuvers are still expected. Anorectal angle ranges between 70-140 degrees (mean angle of 92-114). The anorectal angle was elevated and decreased 15-20 degrees during Kegel maneuver, and downward move and increase 15-20 degree during Vasava maneuver. During the evacuation phase, the anal canal was straightened, the contrast evacuated out of the patient (Figures 2, 3). Minimal contrast residual was set at normal (Figure 4).
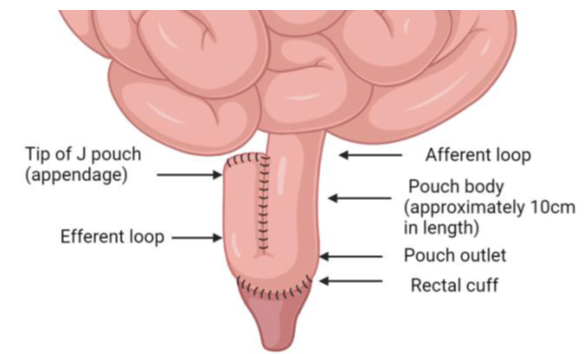
Figure 1: Illustrate of J pouch anatomy.
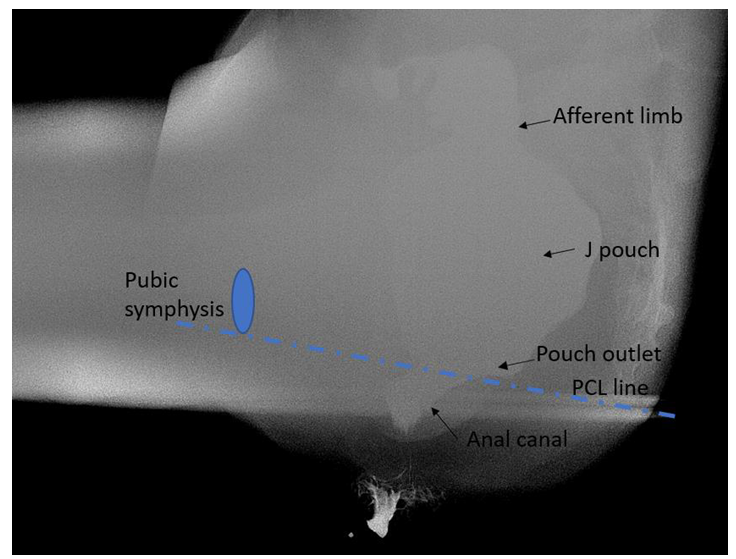
Figure 2: Lateral view of normal J pouch filled with contrast. Landmarks for defecography interpretation include anorectal junction, PCL line, and pubic symphysis.
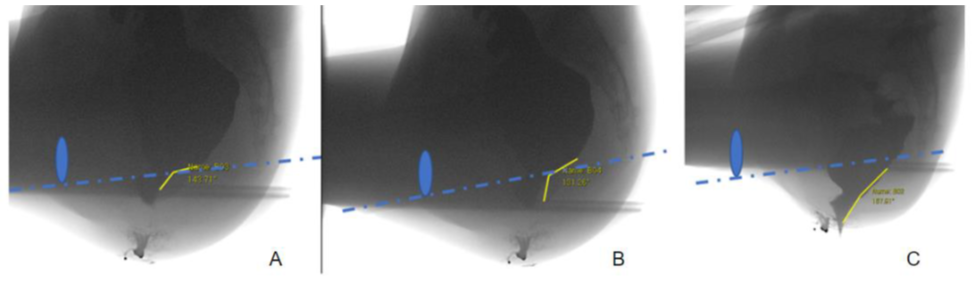
Figure 3: Cine records of normal J pouch physiological changes during defecography. A, at rest, B Kegel maneuver, C, evacuation. There is normal pelvic floor elevation during Kegel maneuver and decreased anorectal angle 12 degree. During evacuation, the pelvic floor is descended, and anorectal angel is straightened, the anal canal is open, allowing contrast past.
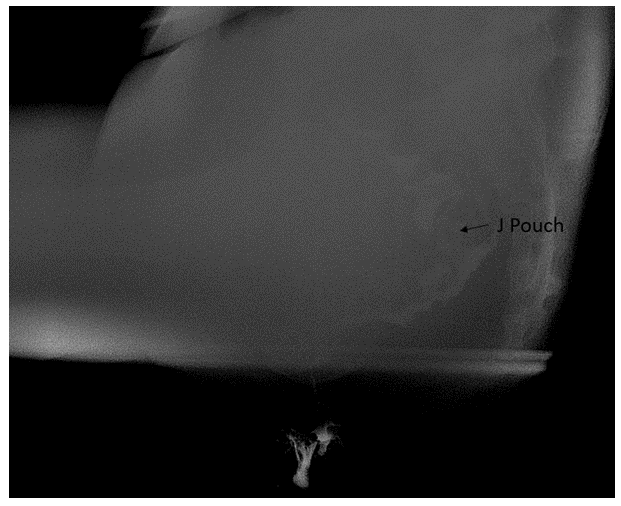
Figure 4: Post evacuation of normal J pouch with minimal residual contrast.
2.4 Fluoroscopic Diagnostic Criteria for Floppy Pouch Complex
Floppy pouch complex includes the following phenotypes: pouch prolapse, Pouchcele, afferent limb syndrome, efferent loop syndrome, redundant loop, and folded or twisted pouch (3, 4).
1. Pouch prolapses: On fluoroscopic defecography, pouch prolapse is defined as pouch below PCL line, exaggerated by Vasava maneuver and evacuation phase (Figure 5). Pouch prolapses is the most common phenotype of floppy pouch complex [4]. The intussusception of the distal pouch that can block the outlet or even come through the anorectal ring (overt pouch prolapse) (Figure 6). Pouch prolapses can be mucosal or full thickness. It is usually caused by weakened muscle, and tissues around the pouch due to aging, pregnancy, childbirth, surgery, constipation of chronic coughing.
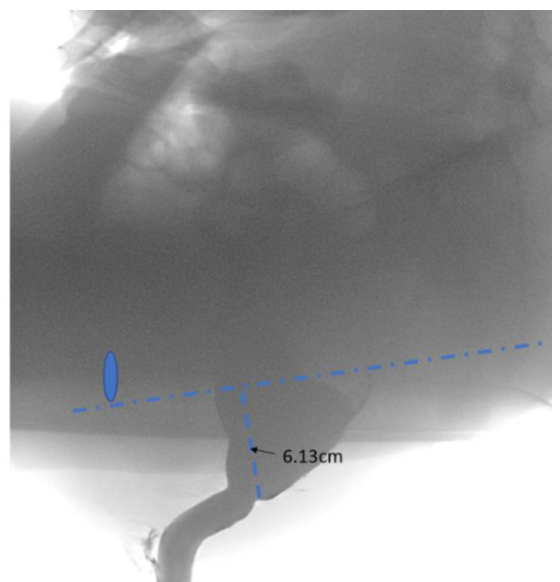
Figure 5: Patient with pain and constipation. At the maximal Vasava maneuver, the anorectal angel is 6.3 cm below PCL line, consistent with severe pouch prolapse.
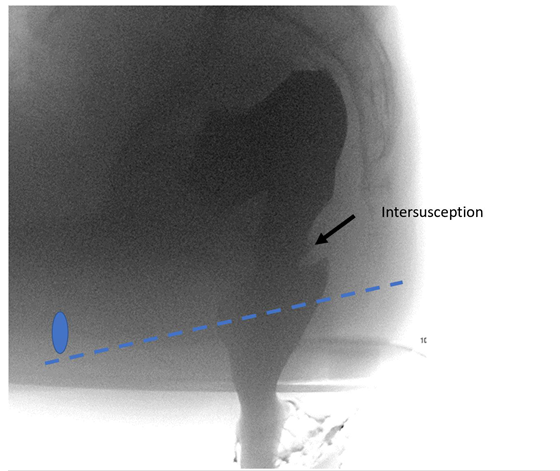
Figure 6: Patient with history of inflammatory bowel disease, status post RPC-IPAA, presenting with obstructive defecation. Patient underwent pouchoscopy, which was unremarkable. Dynamic fluoroscopic defecography demonstrates mild J-pouch intussusception slightly superior to the level of anastomosis. Patient was reassured and was managed conservatively.
2. Pouchcele: On fluoroscopic defecography, pouchcele is defined as focal bulging of the anterior pouch wall (Figure 7). It is graded as small (0-2 cm), medium (2-4 cm), and large (4-6 cm), depending on the size. Patients may feel pressure or fullness in the pelvic area, sensation of something falling-out of the vagina, difficulty to empty bowel, constipation, or pain during the bowel movement.
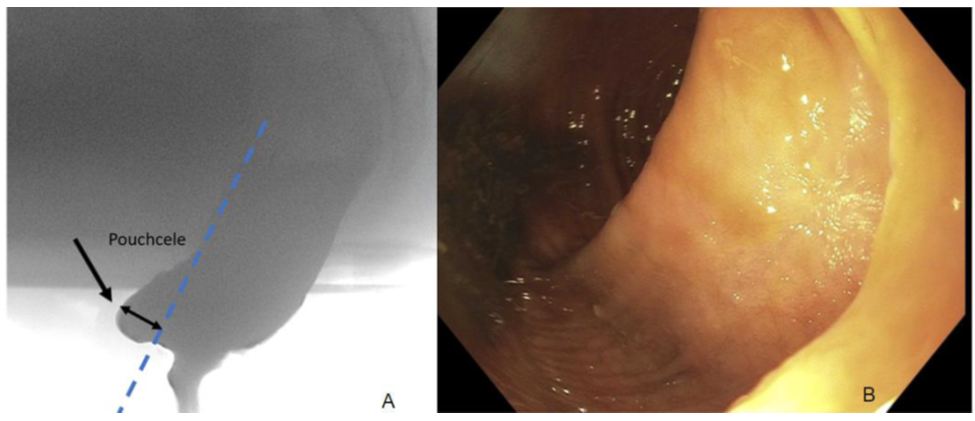
Figure 7: 47-year-old female with refractory ulcerative colitis status post IPAA presenting with incomplete evacuation and dyschezia. Dynamic fluoroscopic defecography (A) demonstrates an anterior pouchocele of 3 cm. Patient underwent a pouchoscopy (B), which confirmed the anterior pouchocele. Pouch mucosa was normal. Pouchocele was treated with banding x 4 with D50 cushion.
3. Afferent loop syndrome: On fluoroscopic defecography, afferent loop syndrome is defined as a sharp angulation at the pouch inlet causing luminal narrowing with or without dilation of the proximal bowel (Figure 8). It can cause partial small bowel obstruction and dysphasia (4). Fluoroscopy is the diagnosis imaging study.
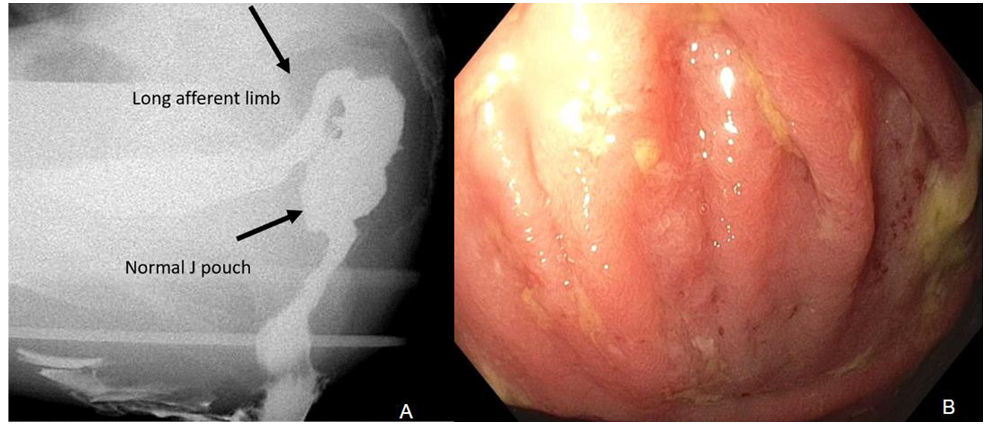
Figure 8: 30-year-old male with ulcerative colitis, status post proctocolectomy with IPAA. Patient demonstrated pouch dysfunction with a sense of incomplete evacuation and difficulty in evaluation. Defecography demonstrates long afferent limb, and sharp angle between the afferent limb and pouch. After evaluation (A), a large amount of residual contrast was present within the afferent limb and in the pouch. Pouchscopy (B) confirm the fluoroscopic findings and identified pouch folds in the outlet.
4. Efferent loop syndrome: On fluoroscopic defecography, efferent loop syndrome is defined as long efferent limb causing a sharp angulation between the pouch body and efferent limb, leading to outlet obstruction and difficult and painful defecation (Figure 9) (5). Conservative treatments of efferent limb syndrome include topical anti-inflammatory or corticosteroids. Surgical treatments include revision or shortening of the efferent limb or conversion to continent ileostomy.
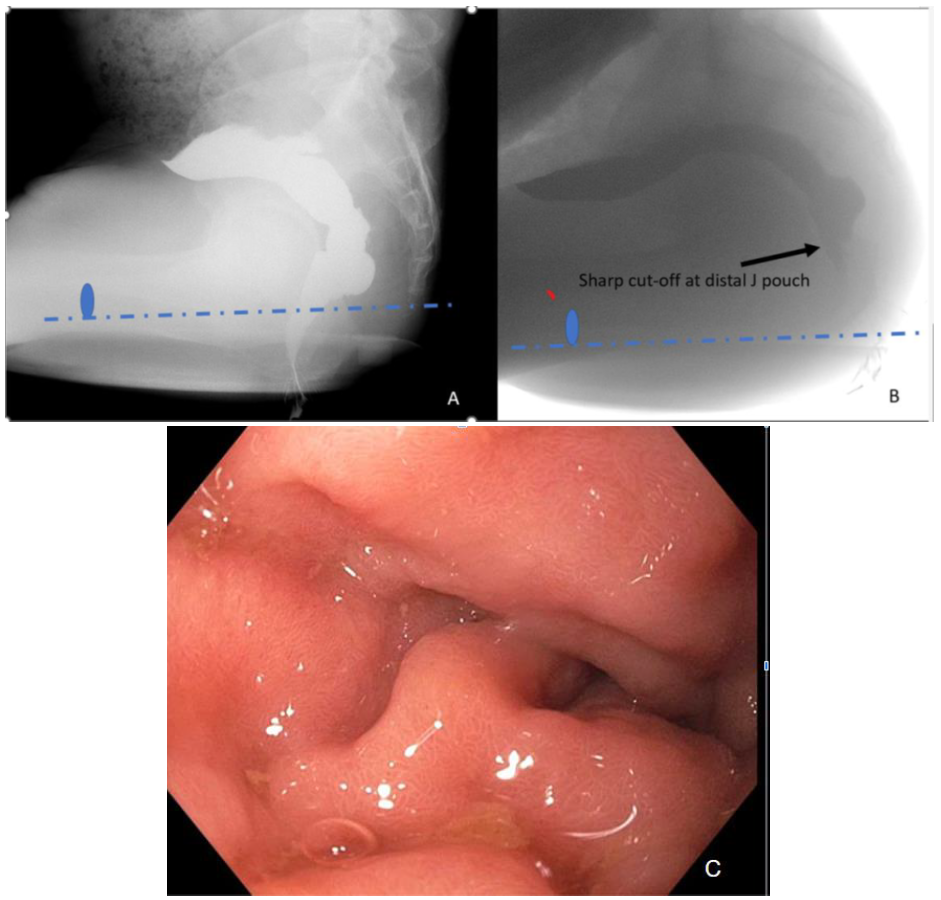
Figure 9: 69-year-old male with ulcerative colitis status post RPC-IPAA in 1983. Patient presents gradually with dyschezia and bloating. Fluoroscopic defecography demonstrated J pouch normal at rest (A). Dynamic evacuation (B) demonstrates a sharp cut-off at the distal pouch leading to incomplete evacuation. The sharp kinking of the efferent limb is not opacified presumably due to the obstruction on the fluoroscopy. This is confirmed by endoscopic evaluation (C), a long efferent limb (>10 cm) was noted with angulation at the junction of the pouch and efferent limb. Patient was offered surgical intervention of either shortening the efferent limb or K pouch conversion, which at the time of this writing had not occurred. Patient is currently managed conservatively with biofeedback and topical calmoseptine.
5. Folded or twisted pouch: On fluoroscopic defecography, folded or twisted pouch is defined as a condition that a sharp horizontal bend or spiral turn in the defecographic evacuation phase (ie, volvulus-like) (Figures 10, 11). Patients may have obstructive evacuation symptoms. The treatment for folded or twisted pouch is conservative.
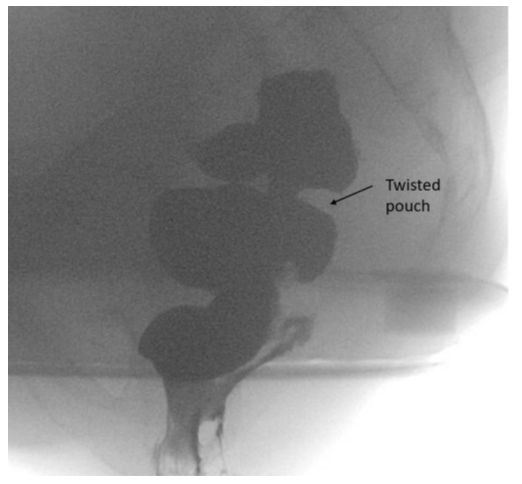
Figure 10: (MRN 1400108143) 51-year-old female with Crohn’s disease status post RPC-IPAA presents with dyschezia. Pouchoscopy is significant for moderate stricture of the pouch inlet and twisted pouch outlet. Dynamic fluoroscopic defecography demonstrating pouch inlet stricture as well as twisted configuration of the pouch.
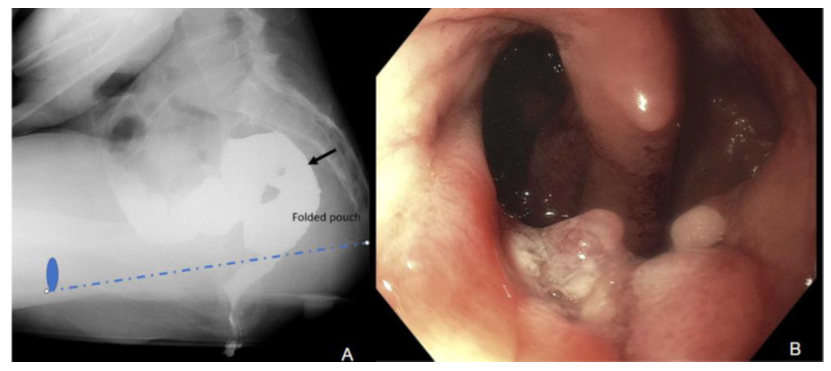
Figure 11: 51-year-old female had history of ulcerative colitis, status post proctocoloectomy and IPAA. Fluoroscopic defecography (A) demonstrates horizontal bend (paper clip pouch) of J pouch. Patient underwent pouchscopy (B), which confirmed folded pouch. Septectomy was performed during endoscopy.
2.5 Pouchscopy evaluation
Pouchscopy is an important procedure for follow-up care after the creation of pouch. The use of an endoscopy with a camera the tip allows the doctors to closely exam the inside of the pouch and performs necessary diagnostic or treatment procedures, such as biopsy, removal polyps, removal extra mucosa, or fistula closure. The procedure can be done with or without sedation, depends on patient’s needs. Adequate visualization is crucial, so bowel cleaning is required beforehand. All patients in this study have undergone pouchscopy in their follow up.
2.6 Statistical analysis
Excel was used for data analysis and calculating categorical variables. Excel charts were applied to visual the distribution of category data.
3. Results
A total of 94 patients underwent 98 fluoroscopic examinations over the nine-year period. 47 were female and 47 patients were male (Table 1). The average age of patients was 50 years old. Among the patient’s population, 66 of them were non-Hispanic (70.2%), 2 Hispanic and 26 patients of unknown ethnicity (29%). Nine patients (9.6%) had BMI categorized as underweight, 53 patient (56.3%) healthy, and 32% patients obese. Among these patients, 72 patients (75%) are never smoking, and 12 patients (12.7%) current or former smokers. 80 patients (85.1%) are diagnosed as ulcerative colitis, other patients are Crohn’s disease (3.1%) and FAP (6.3%). It is average 11 years of disease before colectomy. The indications for colectomy were refractory of disease 81 (86.7%), FAP 5 (5.3%), and neoplasia 7 (7.4%). The average duration of pouch was 13 years. Total 48 patients (51%) demonstrated paradoxical activity on anorectal manometry (ARM) and 37 patients (39.4%) were normal. Only 5 patients (5.3%) demonstrated balloon expulsion on ARM (anorectal manometry), whereas 82 patients (87.2%) failed the balloon expulsion test.
Table 1: Clinical Characteristics of 94 patients
|
Median age (years) |
50 |
|
Gender |
|
|
Male |
47 (50%) |
|
female |
47 (50%) |
|
Ethnicity |
|
|
Not Hispanic |
66 (70.2%) |
|
Hispanic |
2 (2.1%) |
|
Unknown |
26 (27.6%) |
|
BMI |
|
|
Underweight (<18,5) |
9 (9.6 %) |
|
Healthy (18.5-24.9) |
53 (56.3%) |
|
Overweight (25.0-29.9) |
21 (22.3%) |
|
Obese (>30.0) |
9 (9.6%) |
|
Unknown |
2 (2%) |
|
Smoking history |
|
|
Never |
72 (75%) |
|
Current |
1 (1 %) |
|
Former |
11 (11.7%) |
|
Unknown |
10 (10.6%) |
|
Underlying diagnosis |
|
|
UC |
80 (85.1%) |
|
CD |
3 (3.1%) |
|
FAP |
6 (6.3%) |
|
Indeterminate colitis |
4 (4%) |
|
Other |
1 (1%) |
|
Average years of disease before colectomy |
11 (11.7%) |
|
Colectomy Indication |
|
|
Refractory |
81(86.7%) |
|
FAP |
5(5.3%) |
|
Neoplasia |
7 (7.4%) |
|
Other |
1 (1%) |
|
Stage of IPAA |
|
|
One stage |
5 (4%) |
|
Two stages |
42(4%) |
|
Three stages |
28 (4%) |
|
Redo pouch |
9 (4%) |
|
Unknown |
10 (4%) |
|
Average years of duration of pouch |
13 |
|
Paradoxical activity on ARM |
|
|
Yes |
48 (51%) |
|
No |
37 (39.4%) |
|
Unavailable |
9 (9.6 %) |
|
Balloon expulsion on ARM |
|
|
Yes |
5 (5.3%) |
|
No |
82 (87.2%) |
|
Unavailable |
7 (7.4%) |
A total of 7 examinations were terminated prematurely resulting in incomplete evaluation, mostly due to pain or inability to hold onto the contrast material. A total of 74 patients (79%) were not able to completely expel the contrast from the J-pouch (Figure 12). Approximately 73% of examinations demonstrated at least one abnormal categorizable imaging finding and 35% of examinations demonstrated two or more abnormalities. Most common imaging findings seen on fluoroscopic defecography were Pouchcele, pouch prolapse, afferent limb abnormalities, and strictures. On fluoroscopic defecography (Table 2), 21 patients (22.3%) were diagnosed with prolapse, 27 patients (28.6%) with Pouchcele, 14 patients (14.9%) with afferent limb angulation, 13 (13.8%) with stricture, 12 patients (11.6%) with twisted pouch or folded/paperclip pouch, 8 patients (8.5%) with filling defects or separations, and 7 patients (7.3%) with sinus tract or fistula. The complication rate of strictures after IPAA diagnosed with fluoroscopic defecography in this patient cohort was similar to the rate seen in literature, which was about 11% [8].
All patients had at least one pouchscopy report. Total 37 patients (39.3%) demonstrated prolapse, 17 patients (18%) demonstrated Pouchcele, 10 patients (10.6%) demonstrated afferent limb angulation, 26 patients (27.7%) demonstrated stricture, 6 patients (6.4%) with fistula, 25 patients (26.6%) with pouchitis, 13 patients (13.8%) with cuffitis, and 5 patients (5%) with afferent limb or prepouch ileum inflammation (Table 3).
Table 2: Fluoroscopic defecography findings (total 94 patients)
|
Prolapse |
21 (22.3%) |
|
Pouchcele |
27 (28.6%) |
|
Afferent limb angulation |
14 (14.9%) |
|
Stricture |
13 (13.8%) |
|
Sinus tract |
1 (1%) |
|
Fistula |
6 (6.3%) |
|
Twisted pouch |
6 (6.3%) |
|
Folded or paperclip pouch |
5 (5.3%) |
|
Ileopouch |
7 (7.4%) |
|
Filling defects/septations |
8 (8.5%) |
Table 3: Pouchscopy findings (total 94 patients)
|
Prolapse |
37 (39.4%) |
|
Pouchcele |
17 (18%) |
|
Afferent limb angulation |
10 (10.6%) |
|
Stricture |
26 (27.7%) |
|
Sinus tract |
6 (6.3%) |
|
Fistula |
13 (13.8%) |
|
Pouchitis |
25 (26.6 %) |
|
Cuffitis |
13 (13.8%) |
|
Afferent limb inflammation |
5 (5.3%) |
The correlation between fluoroscopic defecography and pouchscopy is demonstrated on Figure 13. In this figure, pouchscopy findings are demonstrated as blue columns, and fluoroscopic defecography findings are demonstrated as yellow columns. Pouchscopy is more sensitive to diagnose pouch prolapse than fluoroscopy defecography (N=37 versus N=21), stricture (N=26 versus N=13), sinus tract (N=6 versus N=1), fistula (N=13 versus N=6), pouchitis (N=25 versus N=0), cuffitis (N=13 versus N=0 ) and afferent limb inflammation (N=5 versus N=0). However, fluoroscopic defecography was more sensitive to detect functional obstruction abnormalities, such as afferent limb angulation (N=14 versus N=10), twisted pouch (N=6 versus N=0), folded or paperclip pouch (N=5 versus N=0), filling defects/septations (N=8 versus N=0).
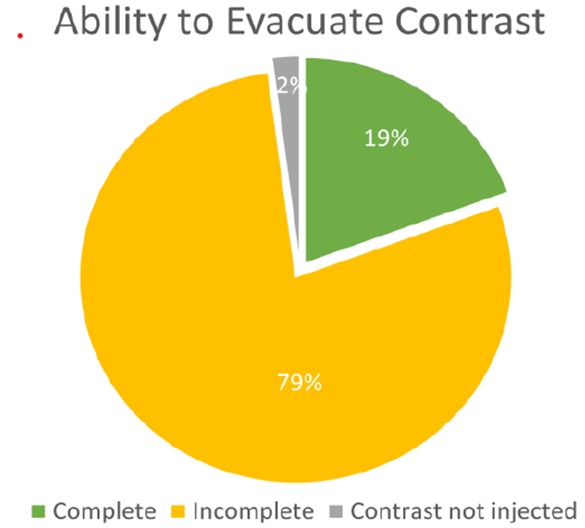
Figure 12: patient’s ability to evacuate contrast.
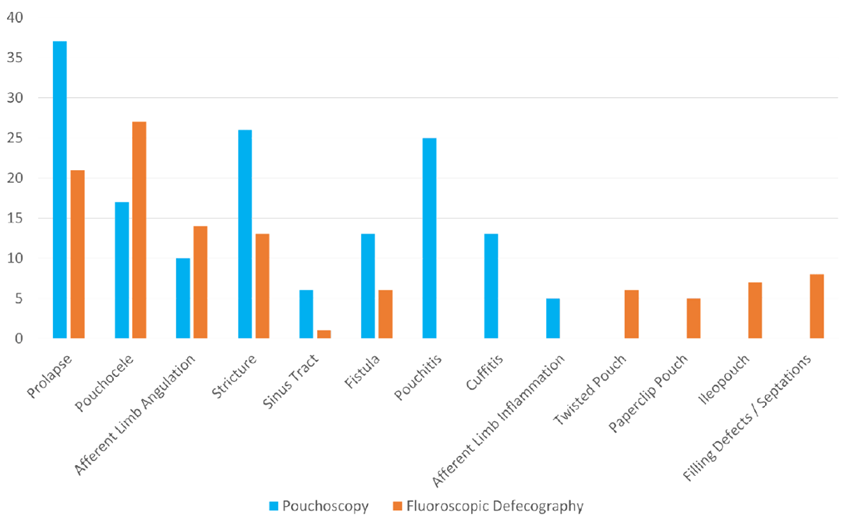
Figure 13: the correlation findings between fluoroscopic defecography and pouchoscopy.
4. Discussion
A total of 94 patients with J pouch creation were included in this retrospective study. Average duration of pouch in our patient cohort was 10 years at the time of the fluoroscopic defecography. Total 77 patients 79% were not able to completely expel the contrast from the J-pouch due to pain or complications. Approximately 73% of examinations demonstrated at least one abnormal categorizable imaging finding and 35% of examinations demonstrated two or more abnormalities. Most common imaging findings seen on fluoroscopic defecography were Pouchcele (N = 27; 28.6%), pouch prolapse (N = 21; 22.3%), and afferent limb abnormalities (N=14; 14.9%). Many other diagnoses can be shown on fluoroscopic defecography, including strictures, fistulas, ileopouch, and abnormal pouch folding. The most common complications identified on pouchscopy were prolapse (N=37; 39.4%), stricture (N=26; 27.7%), pouchitis (N=25; 26.6%), and cuffitis (N=13; 13.8%).
As expected, 85% of the underlying diagnosis of the included J-pouch patients was ulcerative colitis. Remainder of the patients’ underlying diagnoses included Crohn’s Disease, Familial Adenomatous Polyposis, and indeterminate colitis. Most common reason for the J-pouch procedure was due to refractive Inflammatory Bowel Disease; the remaining portion was because of polyposis or neoplasia. Patients on average were afflicted with Inflammatory Bowel Disease 11 years prior to undergoing total colectomy with J-pouch creation but some underwent the procedure as early as a few months to a year, but others lasting for 30 to 40 years of disease prior to surgery. Patients on average presented for a fluoroscopic examination 13 years after undergoing J-pouch creation. However, some patients presented as early as one year after J-pouch creation and others last for 30 to 40 years before presentation.
FPC is a newly recognized disease complex, includes pouch prolapse, Pouchcele, afferent limb syndrome, efferent loop syndrome, redundant loop, and folded or twisted pouch. There is a lack of published literature on FPC and the role of fluoroscopy in diagnosis of floppy pouch complex. The goal of this paper is to introduce the concept of FPC so clinicians and radiologists alike can think of looking for these possible complications in patients with J-pouch. Fluoroscopic defecography examinations are not as commonly performed, as evidenced by only 98 examinations in the past nine years at a large tertiary academic center. This may be partly due to lack of familiarity with the concept of Floppy Pouch Complex and fluoroscopy as a tool for diagnosis.
One advantage of fluoroscopic defecography comes from the ability to diagnose abnormal folding or twisting of the pouch, as pouchscopy may not elucidate these abnormalities. Another advantage includes the ability to better elucidate Pouchcele(9). On the other hand, because of the real-time, dynamic nature of the examinations, some of these pathologies may not be elucidated and thus, correlation with pouchscopy is helpful. Pouchscopy is more sensitive to detect pouch prolapse, and mucosal infectious/inflammatory processes, such as pouchitis, cuffitis and afferent limb inflammation, whereas fluoroscopic examination cannot.
There were limitations in this study. First, the sample pool was small, with only 94 patients included in this study. Second, there was a lack of control samples in this study. Third, most fluoroscopic defecography examinations in patients with J-pouch were abnormal, noting some with multiple abnormalities. This may not be a typical experience for other hospitals, as patients with complications disproportionately present to CUIMC, an expert IBD center.
Keep in mind that pre-test probability for an abnormal fluoroscopic defecography is very high in this patient population. For example, only 5% of the patients were able to expel the balloon, which is a normal finding. Additionally, more than 50% of patients showed abnormal paradoxical activity on anorectal manometry. 79% of patients were not able to completely evacuate the contrast material from the J-pouch.
5. Conclusion
In our patient cohort with an average pouch duration of 10 years, the most common J-pouch dysfunctions captured on fluoroscopic defecography include Pouchcele, pouch prolapse, afferent limb angulation, and stricture. Fluoroscopic defecography provides real-time evaluation of J-pouch with true temporal resolution, which plays a unique role in aiding the diagnosis of Floppy Pouch Complex. This is a great help for clinical physicians in diagnosis of pouch complications, complimentary to pouchscopy findings.
References
- Freeha K, Bo S. Complications Related to J-Pouch Surgery. Gastroenterol Hepatol (N Y) 14 (2018): 571-576.
- Freeha K, Gao XH, Hull TL, et al. Characterization of risk factors for floppy pouch complex in ulcerative colitis. Int J Colorectal Dis 34 (2019): 1061-1067.
- Sherman J, Greenstein AJ. Ileal j pouch complications and surgical solutions: a review. Inflamm Bowel Dis 20 (2014): 1678-1685.
- Fazio VW, Kiran RP, Remzi FH, et al. Ileal pouch anal anastomosis: analysis of outcome and quality of life in 3707 patients. Ann Surg 257 (2013): 679-685.
- Shen B, Kochhar GS, Kariv R, et al. Diagnosis and classification of ileal pouch disorders: consensus guidelines from the International Ileal Pouch Consortium. Lancet Gastroenterol Hepatol 6 (2021): 826-849.
- Shen B, Kochhar GS, Rubin DT, et al. Treatment of pouchitis, Crohn's disease, cuffitis, and other inflammatory disorders of the pouch: consensus guidelines from the International Ileal Pouch Consortium. Lancet Gastroenterol Hepatol 7 (2022): 69-95.
- Shen B, Kochhar GS, Navaneethan U, et al. Endoscopic evaluation of surgically altered bowel in inflammatory bowel disease: a consensus guideline from the Global Interventional Inflammatory Bowel Disease Group. Lancet Gastroenterol Hepatol 6 (2021): 482-497.
- Santiago P, Barnes EL, Raffals LE. Classification and Management of Disorders of the J Pouch. Am J Gastroenterol (2023).
- Khan F, Hull TL, Shen B. Diagnosis and management of floppy pouch complex. Gastroenterol Rep (Oxf) 6 (2018): 246-256.
