Flexor Pollicis Tendon Rupture After Volar Plating of Distal Radius Fracture
Article Information
Amanda Partap1,?, Trevor Seepaul2, Ryan Raghunanan3
Department of Orthopedics, San Fernando General Hospital, San Fernando, Trinidad
*Corresponding Author: Dr. Amanda Partap, Independence Avenue, San Fernando, Trinidad
Received: 07 May 2020; Accepted: 19 May 2020; Published: 05 June 2020
Citation: Amanda Partap, Trevor Seepaul, Ryan Raghunanan. Flexor Pollicis Tendon Rupture After Volar Plating of Distal Radius Fracture. Journal of Orthopaedics and Sports Medicine 2 (2020): 122-128.
View / Download Pdf Share at FacebookAbstract
Introduction: Distal radius fractures are one of the commonest fractures seen worldwide with a steadily rising incidence. There are numerous treatment options available for their management with the most recent advancement being the use of volar locking plates. These locking plates despite advancement in their design and biomechanical construct have been shown to result in flexor tendon rupture and tenosynovitis in up to 15% of patients.
Case Report: A 70-year-old female underwent open reduction and internal fixation with a 3.5 mm volar locking plate for the treatment of a right intra-articular distal radius fracture with volar displacement. Twenty-six (26) months after the initial procedure she re-presented with the inability to flex her thumb after reaching for an object one month prior. The patient subsequently underwent surgical exploration to address her FPL tendon rupture with reconstruction utilising ipsilateral palmaris longus graft with a Pulvertaft weave for both proximal and distal anastomoses.
Conclusion: The reconstruction technique employed in this case yielded a good functional outcome for this patient. The pulvertaft weave as a proximal and distal anastomosis suture provides a good option for reconstruction once there is sufficient graft length to permit its use on both ends.
Keywords
Distal radius fractures; Volar locking plates; Flexor tendon rupture; Tenosynovitis
Distal radius fractures articles Distal radius fractures Research articles Distal radius fractures review articles Distal radius fractures PubMed articles Distal radius fractures PubMed Central articles Distal radius fractures 2023 articles Distal radius fractures 2024 articles Distal radius fractures Scopus articles Distal radius fractures impact factor journals Distal radius fractures Scopus journals Distal radius fractures PubMed journals Distal radius fractures medical journals Distal radius fractures free journals Distal radius fractures best journals Distal radius fractures top journals Distal radius fractures free medical journals Distal radius fractures famous journals Distal radius fractures Google Scholar indexed journals Wrist fractures articles Wrist fractures Research articles Wrist fractures review articles Wrist fractures PubMed articles Wrist fractures PubMed Central articles Wrist fractures 2023 articles Wrist fractures 2024 articles Wrist fractures Scopus articles Wrist fractures impact factor journals Wrist fractures Scopus journals Wrist fractures PubMed journals Wrist fractures medical journals Wrist fractures free journals Wrist fractures best journals Wrist fractures top journals Wrist fractures free medical journals Wrist fractures famous journals Wrist fractures Google Scholar indexed journals Radiocarpal joint articles Radiocarpal joint Research articles Radiocarpal joint review articles Radiocarpal joint PubMed articles Radiocarpal joint PubMed Central articles Radiocarpal joint 2023 articles Radiocarpal joint 2024 articles Radiocarpal joint Scopus articles Radiocarpal joint impact factor journals Radiocarpal joint Scopus journals Radiocarpal joint PubMed journals Radiocarpal joint medical journals Radiocarpal joint free journals Radiocarpal joint best journals Radiocarpal joint top journals Radiocarpal joint free medical journals Radiocarpal joint famous journals Radiocarpal joint Google Scholar indexed journals Fracture articles Fracture Research articles Fracture review articles Fracture PubMed articles Fracture PubMed Central articles Fracture 2023 articles Fracture 2024 articles Fracture Scopus articles Fracture impact factor journals Fracture Scopus journals Fracture PubMed journals Fracture medical journals Fracture free journals Fracture best journals Fracture top journals Fracture free medical journals Fracture famous journals Fracture Google Scholar indexed journals Tenosynovitis articles Tenosynovitis Research articles Tenosynovitis review articles Tenosynovitis PubMed articles Tenosynovitis PubMed Central articles Tenosynovitis 2023 articles Tenosynovitis 2024 articles Tenosynovitis Scopus articles Tenosynovitis impact factor journals Tenosynovitis Scopus journals Tenosynovitis PubMed journals Tenosynovitis medical journals Tenosynovitis free journals Tenosynovitis best journals Tenosynovitis top journals Tenosynovitis free medical journals Tenosynovitis famous journals Tenosynovitis Google Scholar indexed journals FPL tendon rupture articles FPL tendon rupture Research articles FPL tendon rupture review articles FPL tendon rupture PubMed articles FPL tendon rupture PubMed Central articles FPL tendon rupture 2023 articles FPL tendon rupture 2024 articles FPL tendon rupture Scopus articles FPL tendon rupture impact factor journals FPL tendon rupture Scopus journals FPL tendon rupture PubMed journals FPL tendon rupture medical journals FPL tendon rupture free journals FPL tendon rupture best journals FPL tendon rupture top journals FPL tendon rupture free medical journals FPL tendon rupture famous journals FPL tendon rupture Google Scholar indexed journals Graft articles Graft Research articles Graft review articles Graft PubMed articles Graft PubMed Central articles Graft 2023 articles Graft 2024 articles Graft Scopus articles Graft impact factor journals Graft Scopus journals Graft PubMed journals Graft medical journals Graft free journals Graft best journals Graft top journals Graft free medical journals Graft famous journals Graft Google Scholar indexed journals Volar plate articles Volar plate Research articles Volar plate review articles Volar plate PubMed articles Volar plate PubMed Central articles Volar plate 2023 articles Volar plate 2024 articles Volar plate Scopus articles Volar plate impact factor journals Volar plate Scopus journals Volar plate PubMed journals Volar plate medical journals Volar plate free journals Volar plate best journals Volar plate top journals Volar plate free medical journals Volar plate famous journals Volar plate Google Scholar indexed journals Pulvertaft articles Pulvertaft Research articles Pulvertaft review articles Pulvertaft PubMed articles Pulvertaft PubMed Central articles Pulvertaft 2023 articles Pulvertaft 2024 articles Pulvertaft Scopus articles Pulvertaft impact factor journals Pulvertaft Scopus journals Pulvertaft PubMed journals Pulvertaft medical journals Pulvertaft free journals Pulvertaft best journals Pulvertaft top journals Pulvertaft free medical journals Pulvertaft famous journals Pulvertaft Google Scholar indexed journals Osteoporosis articles Osteoporosis Research articles Osteoporosis review articles Osteoporosis PubMed articles Osteoporosis PubMed Central articles Osteoporosis 2023 articles Osteoporosis 2024 articles Osteoporosis Scopus articles Osteoporosis impact factor journals Osteoporosis Scopus journals Osteoporosis PubMed journals Osteoporosis medical journals Osteoporosis free journals Osteoporosis best journals Osteoporosis top journals Osteoporosis free medical journals Osteoporosis famous journals Osteoporosis Google Scholar indexed journals Fracture collapse articles Fracture collapse Research articles Fracture collapse review articles Fracture collapse PubMed articles Fracture collapse PubMed Central articles Fracture collapse 2023 articles Fracture collapse 2024 articles Fracture collapse Scopus articles Fracture collapse impact factor journals Fracture collapse Scopus journals Fracture collapse PubMed journals Fracture collapse medical journals Fracture collapse free journals Fracture collapse best journals Fracture collapse top journals Fracture collapse free medical journals Fracture collapse famous journals Fracture collapse Google Scholar indexed journals Iatrogenic injury articles Iatrogenic injury Research articles Iatrogenic injury review articles Iatrogenic injury PubMed articles Iatrogenic injury PubMed Central articles Iatrogenic injury 2023 articles Iatrogenic injury 2024 articles Iatrogenic injury Scopus articles Iatrogenic injury impact factor journals Iatrogenic injury Scopus journals Iatrogenic injury PubMed journals Iatrogenic injury medical journals Iatrogenic injury free journals Iatrogenic injury best journals Iatrogenic injury top journals Iatrogenic injury free medical journals Iatrogenic injury famous journals Iatrogenic injury Google Scholar indexed journals Injuries articles Injuries Research articles Injuries review articles Injuries PubMed articles Injuries PubMed Central articles Injuries 2023 articles Injuries 2024 articles Injuries Scopus articles Injuries impact factor journals Injuries Scopus journals Injuries PubMed journals Injuries medical journals Injuries free journals Injuries best journals Injuries top journals Injuries free medical journals Injuries famous journals Injuries Google Scholar indexed journals Fibrotic tissue articles Fibrotic tissue Research articles Fibrotic tissue review articles Fibrotic tissue PubMed articles Fibrotic tissue PubMed Central articles Fibrotic tissue 2023 articles Fibrotic tissue 2024 articles Fibrotic tissue Scopus articles Fibrotic tissue impact factor journals Fibrotic tissue Scopus journals Fibrotic tissue PubMed journals Fibrotic tissue medical journals Fibrotic tissue free journals Fibrotic tissue best journals Fibrotic tissue top journals Fibrotic tissue free medical journals Fibrotic tissue famous journals Fibrotic tissue Google Scholar indexed journals Index finger articles Index finger Research articles Index finger review articles Index finger PubMed articles Index finger PubMed Central articles Index finger 2023 articles Index finger 2024 articles Index finger Scopus articles Index finger impact factor journals Index finger Scopus journals Index finger PubMed journals Index finger medical journals Index finger free journals Index finger best journals Index finger top journals Index finger free medical journals Index finger famous journals Index finger Google Scholar indexed journals
Article Details
1. Introduction
Distal radius fractures are one of the commonest fractures seen worldwide with a steadily rising incidence [1]. They are commonly termed “wrist fractures” which are described as fractures occurring within 3 cm of the radiocarpal joint [2]. These injuries can be intra-articular or extra-articular that are associated with a bimodal age distribution [3]. In women over the age of 40 years the incidence of these injuries has been found to increase rapidly when compared to men within the same age category [4]. There are numerous treatment options available for their management with the most recent advancement being the use of volar locking plates. Recently; the design of the plates used for fixation of these injuries has evolved to accommodate for their use in a variety of different fracture patterns. However, despite these advancements there is a 15% risk of tendon rupture and tenosynovitis after volar plating procedures. This discussion will review the risk factors and management of flexor pollicis longus (FPL) tendon rupture secondary to volar plate fixation of distal radius fractures.
2. Case
Mrs. G.M. a 70-year-old female suffered a right intra-articular distal radius fracture with volar displacement secondary to a fall on her outstretched hand. Open reduction and internal fixation with a 3.5 mm volar locking plate was performed seven (7) days post-injury. The procedure was performed through a modified Henry's approach to the distal radius with the pronator quadratus repaired over the plate during closure. She was reviewed routinely in the outpatient clinic and at one year she was discharged. Her function had returned to normal at this point and there was both clinical and radiographic evidence of fracture union without collapse of the distal fragment (Figure 1).

Figure 1: Radiograph of Mrs. G.M. Distal radius volar plate.
The patient presented twenty-six (26) months after the initial procedure complaining of an inability to flex her thumb which occurred after reaching for an object one month prior. On examination, she was unable to flex her right thumb at the interphalangeal joint but her wrist was pain-free with a normal range of motion with a well-healed surgical scar. The patient subsequently underwent surgical exploration to address her FPL tendon rupture. A modified Henry’s approach which was extended distally to the carpal tunnel was utilized. On exploration, the distal edge of the plate was found to be uncovered despite the pronator quadratus having been repaired over the plate. (Figure 2) The FPL tendon was ruptured over the distal end of the plate as well as the frayed tendon edges were localised and debrided. The ipsilateral palmaris longus tendon was harvested and used as a graft.
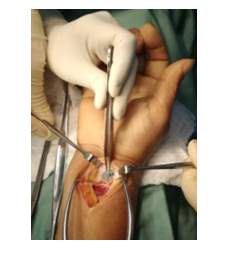
Figure 2: Intra operative picture of Mrs. G.M. showing the uncovered distal end of the volar plate.

Figure 3: Intra operative image of palmaris longus graft (white arrow) repair of flexor pollicis longus tendon.
The patient’s tendon was repaired using the tendon graft with a pulvertaft weave for both proximal and distal anastomoses. (Figure 3) She was immobilized in a thumb spica for four weeks after which range of motion exercises were started.
3. Discussion
The utilization of the volar plating technique for the management of distal radius fractures is preferred over dorsal plating by most surgeons in an attempt to minimize the high risk of tendon rupture that is seen with dorsal plating [5-9]. Literature reviews have revealed few studies reporting tendon rupture after the use of volar plates for the fixation of distal radius fractures. In 2013 a systematic review was undertaken and found only forty-seven (47) reported cases of ruptured tendons after volar distal radius plating with FPL tendon rupture being the most common tendon rupture followed by flexor digitorum profundus to the index finger [10]. The true prevalence of flexor tendon ruptures associated with volar plating of distal radius fractures remains unknown. Of the cases reported, fifty percent occurred at 6-26 months after the index operation in the literature [10].One-third of the reported cases were seen in patients between 60-70 years with a female predominance which is in keeping with an increased incidence of distal radius fractures in the older population as well as the presence of osteoporosis [10, 11].
Numerous factors have been attributed to the rupture of flexor tendons after the treatment of distal radius fractures. The commonly reported factors include the placement of the plate distal to the transverse ridge, prominent distal edge of the plate, screw head prominence, malreduction of fracture, and incorrect usage of plate, fracture collapse, tendinopathy and iatrogenic injury [12-16]. The position of the plate has been suggested to be one of the major risk factors for tendon rupture due to irritation of the tendons that overlie the distal end of the plate. The transverse ridge or “watershed line” is located distal to the pronator quadratus muscle, approximately 2 mm from the joint line on the ulnar side of the radius and 10-15 mm from the radial sided articular surface [17]. The placement of a volar plate distal to this line can result in impingement of the traversing flexor tendons which leads to their irritation and potential rupture.
In 2011, a classification system to determine the presence of plate prominence in relation to the watershed line was developed [18]. The postoperative radiographs for the above patient revealed that the distal edge of the plate was distal to the “watershed line” and would be classified as a Soong grade 2. It was found that patients with a Soong grade 2 volar prominence had an increased incidence of flexor tendon ruptures [18, 19]. The volar prominence of this patient’s plate may have attributed to the eventual rupture of her FPL tendon after repetitive irritation caused by the gliding of the tendon over the distal edge of the plate. One recommendation to decrease the risk of tendon attrition by a prominent distal plate end is to repair the pronator quadratus muscle over the plate [16, 20, 21]. The pronator quadratus is found in the deepest muscle layer of the anterior compartment of the forearm and serves to protect the flexor tendons from prominent hardware. In the case described the muscle layer although repaired was still deficient over the distal edge of the plate thus leaving this critical point exposed to the overlying tendons. One study of volar plating for dorsally comminuted distal radius fractures observed that the size of the pronator quadratus varies in individuals especially in middle-aged women who were noted to have the thinnest muscle layer [22, 23]. FPL tendon ruptures although uncommon sequelae of volar plate fixation of these injuries still exists despite recent advancements in the design of these plates A meticulous surgical technique and appropriate plate selection are necessary to aid in the prevention of this complication. Various techniques of repair have been described for these injuries ranging from primary repair, tendon grafting, and tendon transfers. Patients who present with a FPL rupture as a result of friction against the plate have been found to have tenosynovium hypertrophy and a tendon defect with fibrotic tissue as well as tendon retraction. These patients are more likely to benefit from tendon grafting or transfer as performed in the case described above.
4. Conclusion
A variety of tendon graft donor options are available but the commonest tendon graft used is the ipsilateral palmaris longus tendon [24]. There are numerous tendon suturing techniques which can be employed for anastomosis of the tendon graft. However, the pulvertaft weave has been the most commonly used technique for the proximal suture anastomosis of flexor tendon grafts [25, 26]. This technique was employed in the case presented for both the proximal and distal anastomosis. Based on the outcome of this case the pulvertaft weave as a proximal and distal anastomosis suture is a good option once there is sufficient graft length to permit its use on both ends.
Conflict of Interest
The Authors declare that there is no conflict of interest and no funding was received.
References
- Nellans KW, Kowalski E, Chung KC. The epidemiology of distal radius fractures. Hand Clin 28 (2012):113-125.
- Hoare CP, Dickson DR, Armstrong DJ, et al. Internal fixation for treating distal radius fractures in adults. In: Watts AC, editor. Cochrane Database of Systematic Reviews [Internet]. Chichester, UK: John Wiley and Sons, Ltd., (2014).
- Meena S, Sharma P, Sambharia AK, et al. Fractures of distal radius: an overview. J Fam Med Prim care 3 (2014): 325-332.
- McQueen M, Court-Brown C. Increasing age and fractures of the distal radius. Curr Orthop 17 (2003): 360-368.
- Orbay JL, Fernandez DL. Volar Fixation for Dorsally Displaced Fractures of the Distal Radius: A Preliminary Report. J Hand Surg Am 27 (2002): 205-215.
- Monaco NA, Dwyer CL, Ferikes AJ, et al. Hand Surgeon Reporting of Tendon Rupture Following Distal Radius Volar Plating. Hand (N Y) 11 (2016): 278-286.
- Herron M, Faraj A, Craigen MAC. Dorsal plating for displaced intra-articular fractures of the distal radius. Injury 34 (2003): 497-502.
- ASchnur DP, Chang B. Extensor tendon rupture after internal fixation of a distal radius fracture using a dorsally placed AO/ASIF titanium pi plate. Arbeitsgemeinschaft für Osteosynthesefragen/Association for the Study of Internal Fixation. Ann Plast Surg 44 (2000): 564-566.
- Ring D, Jupiter JB, Brennwald J, et al. Prospective multicenter trial of a plate for dorsal fixation of distal radius fractures. J Hand Surg 22 (1997): 777-784.
- Asadollahi S, Keith PPA. Flexor tendon injuries following plate fixation of distal radius fractures: A systematic review of the literature. J Orthop Traumatol 14 (2013): 227-234.
- Brogren E, Petranek M, Atroshi I. Incidence and characteristics of distal radius fractures in a southern Swedish region. BMC Musculoskelet Disord 8 (2007): 48.
- Bell JS, Wollstein R, Citron ND. Rupture of flexor pollicis longus tendon: a complication of volar plating of the distal radius. J Bone Joint Surg Br 80 (1998): 225-226.
- Cho C-H, Lee K-J, Song K-S, et al. Delayed rupture of flexor pollicis longus after volar plating for a distal radius fracture. Clin Orthop Surg 4 (2012): 325-328.
- Fok MWM, Klausmeyer MA, Fernandez DL, et al. Volar plate fixation of intra-articular distal radius fractures: a retrospective study. J Wrist Surg 2 (2013): 247-254.
- Arora R, Lutz M, Hennerbichler A, et al. Complications Following Internal Fixation of Unstable Distal Radius Fracture With a Palmar Locking-Plate. J Orthop Trauma 21 (2007): 316-322.
- Duncan SF WA. Delayed rupture of the flexor pollicis longus tendon after routine volar placement of a T-plate on the distal radius A Case Report and amp; Literature Review. Am J Orthop 36 (2008): 669-670.
- Berglund LM, Messer TM. Complications of volar plate fixation for managing distal radius fractures. J Am Acad Orthop Surg 17 (2009): 369-377.
- Soong M, Earp BE, Bishop G, et al. Volar Locking Plate Implant Prominence and Flexor Tendon Rupture. J Bone Jt Surgery-American 93 (2011): 328-335.
- Selles CA, Reerds STH, Roukema G, et al. Relationship between plate removal and Soong grading following surgery for fractured distal radius. J Hand Surg 43 (2018): 137-141.
- Tahririan MA, Javdan M, Motififard M. Results of pronator quadratus repair in distal radius fractures to prevent tendon ruptures. Indian J Orthop 48 (2014): 399-403.
- Swigart CR, Badon MA, Bruegel VL, et al. Assessment of Pronator Quadratus Repair Integrity Following Volar Plate Fixation for Distal Radius Fractures: A Prospective Clinical Cohort Study. J Hand Surg Am 37 (2012): 1868-1873.
- Douthit JD. Volar plating of dorsally comminuted fractures of the distal radius: a 6-year study. Am J Orthop (Belle Mead NJ) 34 (2005): 140-147.
- Brown EN, Lifchez SD. Flexor pollicis longus tendon rupture after volar plating of a distal radius fracture: pronator quadratus plate coverage may not adequately protect tendons. Eplasty 11 (2011): e43.
- Freilich AM, Chhabra AB. Secondary Flexor Tendon Reconstruction, A Review. J Hand Surg Am 32 (2007): 1436-1442.
- Hashimoto T, Thoreson AR, An K-N, et al. Comparison of step-cut and Pulvertaft attachment for flexor tendon graft: a biomechanics evaluation in an in vitro canine model. J Hand Surg Eur 37 (2012): 848-854.
- Guy Pulvertaft R. Tendon Grafts for Flexor Tendon Injuries. J Bone Jt Surg Br 38 (1956): 175-194.
