Feasibility of Transnasal dental Implant Placement Determined by PLACATE Guidelines
Article Information
Dan Holtzclaw*, David Zelig, David Bulot, Steven Nelson, Alex Nguyen
Private practice, 4010 Sandy Brook Drive, Round Rock, Texas, 78665, USA
*Corresponding Author: Dan Holtzclaw, Private practice, 4010 Sandy Brook Drive, Round Rock, Texas, 78665, USA.
Received: 30 January 2025; Accepted: 11 February 2025; Published: 17 February 2025
Citation: Dan Holtzclaw, David Zelig, David Bulot, Steven Nelson, Alex Nguyen. Feasibility of transnasal dental implant placement determined by PLACATE guidelines. Dental Research and Oral Health. 8 (2025): 12-17.
View / Download Pdf Share at FacebookAbstract
Introduction: Transnasal dental implant treatment is a relatively new manner of addressing severely atrophic maxillae. These implants involve anatomic features which are not common to traditional implant dentistry such as inferior conchae, prelacrimal bone, and nasolacrimal ducts. To date, there is no systematic manner for presurgical anatomic evaluation of transnasal dental implant feasibility. This paper remedies this deficiency with the PLACATE guidelines.
Methods: A sequential review of 300 CBCT scans of patients referred for advanced full arch implant treatment was performed to determine feasibility for transnasal dental implant placement according to PLACATE guidelines. The following parameters were measured: 1) Simmen classification; 2) Prelacrimal bone width; 3) Subnasal bone height; 4) Distance from subnasal bone to prelacrimal bone engagement point. Additionally, the following anatomic data pertinent to transnasal dental implants was collected: 1) Diameter of nasolacrimal canals; 2) Distance from nasal aperture to nasolacrimal canal; 3) Angle of nasolacrimal canal relative to maxilla; 4) Patency of nasolacrimal canals.
Results: A total of 300 CBCT scans were evaluated for 117 men and 183 women with an average age of 62.1 years (range 31-87). Using PLACATE Guidelines, 30.54% of scans were found to be appropriate for transnasal dental implant treatment. The most common reason for patient disqualification from transnasal dental implant treatment was insufficient prelacrimal bone width.
Conclusion: Using PLACATE guidelines as a systematic method for evaluating full arch patients for transnasal dental implant feasibility, patient safety may be improved by treating only those patients who anatomically qualify.
Keywords
Dental implants, Nasolacrimal duct, Anatomy, Oral surgery, Cone-beam computed tomography
Dental implants articles; Nasolacrimal duct articles; Anatomy articles; Oral surgery articles; Cone-beam computed tomography articles
Article Details
Introduction
In 2019, the first cases of “transnasal” implant use for treatment of severely atrophic maxillae were published in dental literature (Figure 1) [1]. Transnasal implants are typically 20-25mm long and are unique in the fact they traverse tangentially along the interior of the lateral nasal wall until reaching the base of the inferior conchae (Figure 2) [1-9]. These fixtures often achieve high insertion torque via engagement of dense bone at the confluence of the inferior concha, lateral nasal wall and frontal process of the maxilla [1-9]. Transnasal engagement of these prelacrimal osseous structures is not without risk, however, as the nasolacrimal duct is in close proximity [4,5]. Violation of the nasolacrimal duct with dental implants has the potential for severe consequences such as dacryostenosis, which in turn, can result in epiphora and dacryocystitis [4,10,11]. As such, careful presurgical anatomic evaluation and planning is necessary to ensure safe use of transnasal dental implants [7-9]. Additionally, assessment of the unique osseous structures engaged by transnasal implants is required to ensure appropriate case selection for fixture survival.
To date, there is no published systematic approach for presurgical evaluation of potential transnasal dental implant candidates. In this paper, the authors present guidelines which they have used in their practices to evaluate patients for successful transnasal implant placement: (P)re(LAC)rimal (A)ssesment of (T)ransnasal Implant (E)ngagement – PLACATE [4].
Methods
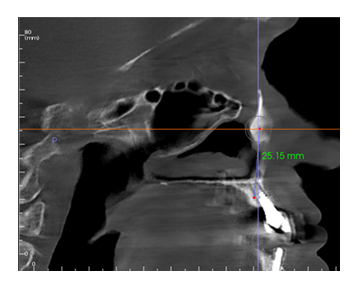
In this retrospective review, anonymized cone beam computer tomography (CBCT) scans from 300 sequential referrals were reviewed by the authors using PLACATE guidelines to determine transnasal dental implant feasibility. Inferior conchae were initially located in the coronal plane and imaging crosshairs were positioned just superior to this structure in the axial plane. To evaluate the ipsilateral and contralateral transnasal engagement points, imaging crosshairs were next positioned over each concha in the sagittal plane. This prelacrimal engagement point, sometimes referred to as the “Z-Point”, [4,5] was then evaluated according to PLACATE guidelines as follows: 1) Simmen classification [12] determined by measurement from the external aspect of the frontal maxilla to the most anterior aspect of the nasolacrimal canal (Figure 3); 2) Mediolateral measurement of prelacrimal bone width (Figure 4); 3) Vertical measurement of subnasal bone height (Figure 5); 4) Vertical measurement from subnasal bone to prelacrimal bone engagement point (Figure 6). To be considered an appropriate candidate for transnasal dental implants, the following parameters had to be met: 1) Simmen 2 or 3 classification; 2) Prelacrimal bone width ≥3mm; 3) Subnasal bone height ≥2mm; 4) Vertical measurement from residual subnasal bone, or anticipated anterior alveolar ridge reduction level, to prelacrimal bone engagement point that does not exceed 25mm. Failure to meet all four PLACATE criteria prevented a patient from being an appropriate transnasal implant.
After PLACATE parameters were assessed, CBCT scans were evaluated for: 1) Nasolacrimal canal diameter at its widest aspect (Figure 7); 2) Dorsoventral distance from the nasal aperture to the most anterior aspect of the nasolacrimal canal (Figure 8); 3) Angle of the nasolacrimal canal relative to the maxillary frontal process (Figure 9); 4) Nasolacrimal canal patency. Supplementary data including patient age and sex were also obtained. Data obtained for this retrospective observational study was gathered in adherence to Helsinki Guidelines as revised by the 64th WMA General Assembly, Fortaleza, Brazil, October 2013 [13].
Results
A total of 300 anonymized CBCT scans were evaluated by the following authors: 1) DH 200 scans; 2) AN 25 scans; 3) DZ 25 scans; 4) SN 25 scans; 5) DB 25 scans. Scans comprised a total of 176 female and 124 male subjects with an average age of 61.6 years (range 31-88). Using PLACATE guidelines, 30.54% of patients qualified for treatment with transnasal dental implants. PLACATE anatomic measurements are presented in table 1. Mean nasolacrimal canal diameters were 7.36mm (±1.39) and 7.41mm (±1.50) for the right and left canals respectively. Mean dorsoventral distances from the nasal aperture to the most anterior aspect of the nasolacrimal canal were 14.06mm (±2.59) and 13.92mm (±2.83) for the right and left canals respectively. Mean angle measurements of the nasolacrimal canal relative to the maxillary frontal process were 73.72° (±5.36) and 73.63° (±5.78) for the right and left canals respectively. Patency was noted in 29.94% and 32.93% for the right and left nasolacrimal canals respectively. In all anatomic measurements recorded, no statistically significant differences were noted between the right and left sides.
|
Nasolacrimal Canal Diameter |
Nasal Aperture to Nasolacrimal Canal Distance |
Nasolacrimal Canal Descent Angle |
Nasolacrimal Canal Patency |
|
|
Right |
7.36mm (±1.39) |
14.06mm (±2.59) |
73.72° (±5.36) |
29.94% |
|
Left |
7.41mm (±1.50) |
13.92mm (±2.83) |
73.63º (±5.78) |
32.93% |
Table 1: CBCT anatomic measurements.
Discussion
Treatment of the atrophic maxilla has undergone numerous permutations over the past 40 years. In the late 1980’s, Brånemark et al. performed the first zygomatic implants to forgo cumbersome maxillary bone grafting procedures that often produced low dental implant survival rates [14,15]. Bothur continued evolution of this treatment in 2003 with intentional placement of multiple zygomatic implants in the malar processes to treat even the most deteriorated maxillae [16]. While this treatment, now commonly referred to as a “quad-zygo”, has proven successful with implant survival rates approaching those of conventional dental implants [4], anatomic irregularities such as limited zygomatic bone mass, aberrant infraorbital nerves, or accentuated concavities of the anterior maxilla sometimes prevent placement of multiple zygomatic implants [1-9]. In such situations, transnasal implant fixtures may offer an alternative that ameliorates the need for anterosuperior fixtures in a quad-zygomatic implant configuration [1-9].
Due to their anchorage in osseous structures previously unused in implant dentistry and propinquity to sensitive structures such as the nasolacrimal canal, careful CBCT evaluation is necessary to determine transnasal dental implant feasibility [1-3]. In the current study, 69.46% of patients were found to be unsuitable candidates for transnasal fixtures due to anatomic insufficiencies. The most common reason for treatment disqualification was inadequate prelacrimal bone volume, which eliminated 49.71% of patients. Fixtures used for transnasal implants typically have platform diameters of 3.5-3.75mm with corresponding apical dimensions ranging from 2.0-2.45mm [1-9]. As the apical portions of these implants engage dense bone at the confluence of the inferior concha, lateral nasal wall, and frontal process of the maxilla, 3+ mm of prelacrimal osseous width ensures that the implant apex will be primarily housed in bone. The second most common reason for transnasal implant disqualification was excessive subnasal bone height, which eliminated 28.74% of patients. The longest implants of appropriate diameters currently available for transnasal fixtures are 25mm in length. While at least 2mm of dense subnasal bone height is recommended for coronal anchorage of transnasal fixtures [4,6]. excessive subnasal bone height obviates the ability of contemporary dental implants to reach prelacrimal bone for bicortical apical anchorage. For such patients, use of shorter anterior implants engaging the piriform rim, nasal rim, or maxillary nasal crest may be more appropriate [4,19,20]. Alternatively, alveolar ridge reduction may be accomplished to facilitate a 25mm long implant reaching the Z-point. The third most common reason for transnasal implant disqualification was Simmen 1 classification, which eliminated 22.16% of patients. Simmen Classification measures the distance from the anterior wall of the maxilla to the nasolacrimal canal and is commonly used in ENT workups to assess surgical safety [6,12]. Simmen 1 patients have 3mm or less prelacrimal bony thickness, making them high risk for iatrogenic violation of the nasolacrimal canal [12]. While a previously published study evaluating 200 nasolacrimal canals found Simmen 1 prevalence of 31.5% [12], the current study evaluating 600 canals had lower findings. A possible explanation for this difference may be the different patient populations of these studies with the current study primarily evaluating patients with atrophic maxillae and the former study evaluating patients for endoscopic sinus surgery.
Intimate knowledge of certain paranasal anatomic features is beneficial for the placement of transnasal implants and can improve safety of the procedure. Previous anatomic studies have measured distances to the nasolacrimal canal orifice from structures such as the anterior extent of the inferior concha [21] or the anterior nasal spine [21,22]. Unfortunately, these structures are not always readily visible intrasurgically or during presurgical CBCT planning. The current study remedied this problem by using the nasal aperture, a readily accessible structure, as a fixed reference point. The mean distance from the nasal aperture to the nasolacrimal canal orifice was 13.99mm, which provides adequate safety for transnasal implant placement. Concerning the angle of the nasolacrimal canal as it traverses from the lacrimal sac to the inferior meatus of the nasal cavity, a mean inferoposterior angle of 73.4° was noted. This finding is very similar to those published by Sieskiewicz et al. who found mean angle measurements ranging from 72.4-74.7 degrees [23]. This inferoposterior angle of the nasolacrimal canal is important in the fact that previously published studies show prelacrimal bony thickness decreases an average of 34.5% as the canal moves superiorly towards the lacrimal sac [24]. Essentially, the more superiorly the apex of a transnasal implant is placed, the higher the chance of engaging the nasolacrimal canal. In this study, the mean diameter of the nasolacrimal canal was 7.51mm which is similar to previously published studies [12,25]. As transnasal dental implants are commonly of diameters ranging from 3.5-3.75mm [1-9], iatrogenic engagement of the nasolacrimal canal may not result in complete physical obstruction due to the differences in size between the canal and the fixture. Resultant inflammation of the nasolacrimal canal epithelial lining, however, may complete this obstruction and result in dacryostenosis [10,11]. Finally, regarding nasolacrimal canal patency on CBCT analysis, 68.37% had opacity, though no patients in this study demonstrated any symptoms of presurgical nasolacrimal duct obstruction. This finding is consistent with previous studies that documented nasolacrimal duct opacity in large unaffected populations [26-28], suggesting this may be a normal finding.
Conclusion
For patients with proper anatomic features, transnasal dental implants may be an alternative to anterosuperior fixtures of quad-zygomatic implant placement. Careful CBCT analysis using PLACATE guidelines provides a systematic approach to determining appropriate candidates for transnasal dental implant procedures. Use of these guidelines may improve patient safety and outcomes for these unique fixtures.
References
- Vanderlim BC, Baptista D, Manfro R. Transnasal Implant (Vanderlim Technique) as an option to the second zygomatic implant. Solucoes Clinicas para Reabilitacoes Totais Sobre Implantes Sem Enxertos Osseos 12 (2019): 199-215.
- Vanderlim BC, Baptista D, Almeida JR. Transnasal implants: Vanderlim technique as an alternative to the Zygoma Quad technique in atrophic total jaws - series of 12 cases in immediate load and follow-up of two to 26 months. Implant News 6 (2021): 1-14.
- Almeida PHT, Cacciacane SH, Arcazas Junior A. Extra-long transnasal implants as alternative for Quad Zygoma: Case report. Ann Med Surg (Lond) 68 (2021): 102635.
- Holtzclaw D. Remote Anchorage Solutions for Severe Maxillary Atrophy: Zygomatic, Pterygoid, Transnasal, Nasal Rim, Piriform Rim, Nasopalatine, and Trans-Sinus Dental Implants. Austin, Texas: Zygoma Partners (2023).
- Oh S, Zelig D, Aalam AA, et al. Case report: utilization of Z-Point fixture "Trans-nasal" implants. Ann Med Surg (Lond) 85 (2023): 1959-1965.
- Nunes M, De Araújo Nobre M, Camargo V. All-on-4 Hybrid with Extra-Long Transnasal Implants: Descriptions of the Technique and Short-Term Outcomes in Three Cases. J Clin Med 13 (2024): 33-48.
- Şahin O. Treatment of Severely Atrophic Maxilla by Using Zygomatic, Pterygoid, and Transnasal Implants. J Craniofac Surg 20 (2023): 12.
- Sales P, Amaral G. The use of the Transnasal implant associated with the zygomatic implants in the treatment of atrophic maxilla: A Case Report. Eur J Stomatol Oral Fac Surg 1 (2024): 1-6.
- Camargo VB, Grossi J, Meurer E, et al. A Transnasal Implant Technique. Inside Dent 19 (2023): 22-26.
- Perez Y, Patel BC, Mendez MD. Nasolacrimal Duct Obstruction. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2024).
- Makselis A, Petroska D, Kadziauskiene A, et al. Acquired nasolacrimal duct obstruction: clinical and histological findings of 275 cases. BMC Ophthalmol 22 (2022): 12.
- Simmen D, Veerasigamani N, Briner HR, et al. Anterior maxillary wall and lacrimal duct relationship - CT analysis for prelacrimal access to the maxillary sinus. Rhinology 55 (2017): 170-174.
- WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects. 18th WMA General Assembly, Helsinki, Finland, June 1964; amended by the 64 WMA General Assembly, Fortaleza, Brazil, October (2013): 1-4.
- Miglioranca R. History of Zygomatic Implants: A Systematic Review and Meta-Analysis. Dent Oral Craniofac Res 5 (2019): 1-9.
- Brånemark PI, Gröndahl K, Ohrnell LO, et al. Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scand J Plast Reconstr Surg Hand Surg 38 (2004): 70-85.
- Bothur S, Jonsson G, Sandahl L. Modified technique using multiple zygomatic implants in reconstruction of the atrophic maxilla: a technical note. Int J Oral Maxillofac Implants 18 (2023): 902-904.
- Jensen OT, Cottam JR, Ringeman JL, et al. Angled dental implant placement into the vomer/nasal crest of atrophic maxillae for All-on-Four immediate function: a 2-year clinical study of 100 consecutive patients. Int J Oral Maxillofac Implants 29 (2014): e30-35.
- Jensen OT, Adams MW, Butura C, et al. Maxillary V-4: Four implant treatment for maxillary atrophy with dental implants fixed apically at the vomer-nasal crest, lateral pyriform rim, and zygoma for immediate function. Report on 44 patients followed from 1 to 3 years. J Prosthet Dent 114 (2015): 810-817.
- Garcia-Denche JT, Abbushi A, Hernández G, et al. Nasal Floor Elevation for Implant Treatment in the Atrophic Premaxilla: A Within-Patient Comparative Study. Clin Implant Dent Relat Res 17 (2015): e520-30.
- Khairnar M, Gaur V. Evidence of bone formation in the nasal floor around polished surface bi-cortical screw implants after indirect nasal lift in an atrophied maxilla: Cone beam computed tomography-based case report. J Indian Soc Periodontol 19 (2015): 236-238.
- Tatlisumak E, Aslan A, Cömert A, et al. Surgical anatomy of the nasolacrimal duct on the lateral nasal wall as revealed by serial dissections. Anat Sci Int 85 (2010): 8-12.
- Elshaarawy EA. Morphological and morphometrical study of the nasal opening of nasolacrimal duct in man. Folia Morphol (Warsz) 73 (2014): 321-330.
- Sieskiewicz A, Buczko K, Janica J, et al. Minimally invasive medial maxillectomy and the position of nasolacrimal duct: the CT study. Eur Arch Otorhinolaryngol 274 (2017): 1515-1519.
- Kashlan K, Craig J. Dimensions of the medial wall of the prelacrimal recess. Int Forum Allergy Rhinol 8 (2018): 751-755.
- Andrianakis A, Moser U, Wolf A, et al. Gender-specific differences in feasibility of pre-lacrimal window approach. Sci Rep 11 (2021): 77-91.
- Choi SC, Lee S, Choi HS, et al. Preoperative Computed Tomography Findings for Patients with Nasolacrimal Duct Obstruction or Stenosis. Korean J Ophthalmol 30 (2016): 243-250.
- Loftus WK, Kew J, Metreweli C. Nasolacrimal duct opacity on CT. Br J Radiol 69 (1996): 630-631.
- Russell EJ, Czervionke L, Huckman M, et al. CT of the inferomedial orbit and the lacrimal drainage apparatus: normal and pathologic anatomy. AJR Am J Roentgenol 145 (1985): 1147-1154.