Factors Influencing Institutional Delivery: An Observational Study
Article Information
Rokshana Begum*,1, Khandoker Abdur Rahim2, A. K. M Shahidur Rahman3, Shihab Md. Rezoyanur Rahman4, Amit Kumar Pramanik5, Md. Hamidul Islam6, Maswood Sarker6, Nazma Akter7, Tanzina Iveen Chowdhury8, Munirunnessa9
1Department of Laboratory Medicine, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
2Department of Orthopaedic surgery, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
3Department of Nephrology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
4Department of Pathology and Blood Transfusion, Gaibandha General Hospital, Gaibandha, Bangladesh
5Department of Transfusion Medicine, Rajshahi Medical College Hospital, Rajshahi, Bangladesh
6Department of Orthopaedic Surgery, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
7Department of Gynaecological oncology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
8Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
9Department of Obstetrics and Gynaecology, Sir Salimullah Medical College & Mitford Hospital (SSMC & MH), Mitford, Dhaka, Bangladesh
*Corresponding author: Dr. Rokshana Begum, Consultant, Department of Laboratory Medicine, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh.
Received: 10 October 2022; Accepted: 12 October 2022; Published: 26 October 2022
Citation: Begum R, Rahim KA, Rahman AKMS, Rahman SMR, Pramanik AK, Islam MH, Sarker M, Akter N, Chowdhury TI, Munirunnessa. Factors Influencing Institutional Delivery: An Observational Stdy. Fortune Journal of Health Sciences 5 (2022): 553-559.
View / Download Pdf Share at FacebookAbstract
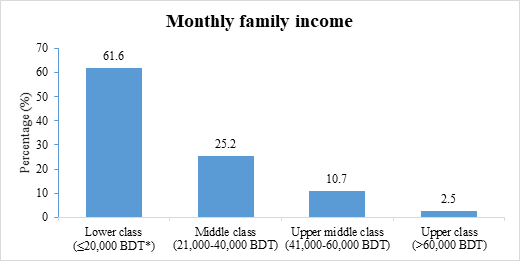
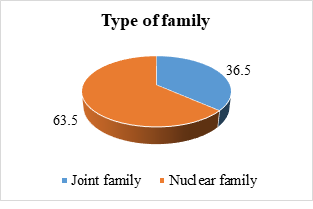
Institutional delivery refers to the delivery that has taken place in a well-equipped medical centre having skilled delivery assistance. This study was designed to identify the factors that influence delivery in institution. This observational study was conducted at the Department of Maternal and Child Health, National Institute of Preventive and Social Medicine (NIPSOM), Dhaka, Bangladesh. A total of 159 case samples were included following selection criteria. Data regarding socio-demographic characteristics, detailed antenatal history and different factors of institutional delivery were collected accordingly. All data were collected by face to face interview. The mean±SD age of the study subjects was 28.4±7.2 years and ranged was 18-38 years. It was observed that, majority (78.7%) of the respondents was at 20-30 years age range and maximum (56.6%) was house wife. Most (37.7%) of them had secondary level education. Their husband (40.3%) and mother in low (40.3%) were equally predominant as decision maker of the family. Majority (61.6%) of the respondents was came from lower economic class and most (63.5%) of them was living in a nuclear family. Different socio-economic factors like- mother's education, family income, occupation, family types, religious believe, place of residence, access to health information, and several antenatal complications were found to be influential for institutional delivery. This study concluded that antenatal complications, different socio-economic factors and access to health information influencing the utilization of maternal health services and institutional delivery.
Keywords
Influencing Factors; Institutional Delivery; Maternal Health Services; Socio-Economic Factors
Influencing Factors articles; Institutional Delivery articles; Maternal Health Services articles; Socio-Economic Factors articles
Article Details
1. Introduction
Appropriate delivery care is crucial for both maternal and child health and increasing skilled attendance at birth is a central goal of the safe motherhood and child survival movements [1]. It is important that mothers deliver their babies in an appropriate setting, where life-saving equipment and hygienic conditions are available [2]. These facilities can also help reduce the risk of complications that may cause death or illness to mother and child [1, 2]. The risk of a women dying as a result of complication related to pregnancy in developing countries can be as much as hundred times that of women in Western Europe or North America [1]. It was reported that, 75% of maternal deaths are due to direct obstetric causes and less than 5% of women with complications have access to emergency obstetric care (EOC) [3] [4]. Reducing maternal mortality ratio (MMR) by two-thirds between 1990 and 2015 was the target under the Millennium Development Goals (MDG) [3, 4]. Bangladesh has a high maternal mortality ratio (MMR), with 194 deaths per 100,000 live births [5]. There are about 11,000 to 12,000 women dying from pregnancy or childbirth complications every year in Bangladesh [5]. The high MMR directly relates to the high perinatal (newborn) mortality rate in the country [5]. The tragic consequence of these deaths is about 75% of the babies born to these women also die within the first week of their lives [5]. Although a high proportion of such deaths are attributed to a lack of emergency obstetric services and trained personnel [4, 5]. The World Health Organization (WHO) estimates that about 536,000 women of reproductive age die each year from pregnancy related complications [4]. Nearly all of these deaths (99%) occur in the developing world [4-6]. Skilled attendance at delivery was an important indicator in monitoring progress towards Millennium Development Goal 5 to reduce the maternal mortality ratio by three quarters between 1990 and 2015 [3, 7]. In addition to professional attention, it is important that delivery in an appropriate setting help reduce the risk of complications to mother and child health [8]. Over the past decade interest has grown in examining influences on care-seeking behavior with a particular focus on assessing the relative importance of community access and economic status [9]. Early and regular check-ups by health professionals are essential in assessing the physical status of women during pregnancy and ensuring appropriate interventions during delivery [9]. In spite of several national and global efforts at curbing down the maternal morbidity and mortality through safe motherhood initiatives, the phenomenon is still on the ascendancy in many developing countries [9, 10]. The United Nations International Children's Emergency Fund (UNICEF) estimates that yearly about 515,000 women die of pregnancy and childbirth complications [10]. In Bangladesh, only 15% of births take place at health facilities [5]. Most deliveries in Bangladesh take place at home by traditional birth attendant (TBA) or by family members [5]. Untrained/medically non-competent birth attendants conduct about 85% of all deliveries in this country [5]. A large number of maternal deaths can be attributed to unhygienic and dangerous delivery practices and inadequate pre and postnatal cares [11]. Women are most in need of skilled care during delivery and immediate post-partum period [11]. Traditional birth attendants (TBA), whether trained or untrained, can neither predict nor cope with serious complications [5, 11]. Several studies confirmed that use of skilled birth attendants at every delivery is the best process indicator that correlates with maternal mortality and poor delivery outcome [5, 11, 12]. On the other hand, an institutional delivery refers to the delivery that has taken place in a well-equipped medical centre having skilled delivery assistance along with all life-saving facilities for new born babies [11, 12]. All public hospital, private hospital, and well equipped maternity clinics provide modern delivery care [5, 11, 12]. Institutional delivery is a good practice for reducing the maternal mortality rate and ensuring healthy newborns [3]. In this study, an attempt had been made to explore the factors influencing institutional delivery.
2. Methods
This observational study was conducted to assess the factors influencing institutional delivery. The study was conducted at the Department of Maternal and Child Health, National Institute of Preventive and Social Medicine (NIPSOM), Dhaka, Bangladesh. A total of 159 case samples were included in this study from Department of Obstetrics and Gynecology, Jamalpur Sador Hospital, Jamalpur, Bangladesh and Department of Obstetrics and Gynecology, Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh. All pregnancies resulting in live births at institution during a six months study period were included following purposive sampling technique.
2.1 Research instrument
A structured questionnaire was developed in English. The questionnaire was developed using the selected variables according to the specific objectives. The questionnaire was translated into Bangla and it was pretested. This Bangla translation was evaluated by a team comprises of respective professionals and an expert in English literature whose native language is Bangla. The questionnaire was then finalized after necessary modification according to the findings of pretesting.
2.2 Data collection and analysis technique
The data were collected by face to face interview of the respondents. The interview was conducted by maintaining privacy as far as possible. Before preceding the data collection, the detail of the study was explicitly explained to each eligible respondent and written consents were taken from the respondents. Data regarding socio-demographic characteristics, detailed antenatal history and different factors of institutional delivery were collected accordingly. Then all collected data were checked and verified at the end of work in each day. Any inaccuracy and inconsistency was corrected in the next working day. Data processing and analyses were done using computer based software Statistical Package for Social Sciences (SPSS).
3. Results and observations
This study was intended to assess the influencing factors of institutional delivery at two tertiary care hospitals in Bangladesh. A total of 159 subjects were included in this study. Mean(±SD) age of the study subjects was 28.4±7.2 years and ranged was 18-38 years. Majority (44.7%) of them was at the age group of 20-25 years followed by 25-30 years age group (34%), 14.4% was above 30 years and 6.9% was between 18 to 20 years (Table- 1). Regarding occupation of the respondents; majority (56.6%) was house wife followed by 27.0% was service holder, 13.2% was garments worker and 3.2% was day laborer (Table- 1). Educational status of the respondents showed, majority (37.7%) of the respondents had secondary level education, 33.4% had graduation and above level education, 15.7% of the respondents had up to college level education, 6.3% had primary level education and 6.9% was able to put their sign only (Table- 1). Among the respondents, 64.2% was Muslim and 35.8% was belongs to Hindu religion (Table- 1). About husband’s occupation of the respondents; majority (26.4%) was garments workers followed by 20.8% was businessman and government service each, and 19.5% was in private service (Table- 1). It was found that husband (40.3%) and mother in low (40.3%) were equally predominant as decision maker of the respondent’s family (Table- 1).
|
Variables |
Frequency (n) |
Percentage (%) |
|
Age (years) |
||
|
Mean±SD (years) |
28.4±7.2 |
|
|
Range (years) |
18-38 |
|
|
Age group |
||
|
18 to 20 years |
11 |
6.9 |
|
20-25 years |
71 |
44.7 |
|
25-30 years |
54 |
34 |
|
>30 years |
23 |
14.4 |
|
Occupation |
||
|
Housewife |
90 |
56.6 |
|
Day laborer |
5 |
3.2 |
|
Service holder |
43 |
27 |
|
Garments worker |
21 |
13.2 |
|
Educational status |
||
|
Able to put sign only |
11 |
6.9 |
|
Primary (1-5) |
10 |
6.3 |
|
Secondary (6-10) |
60 |
37.7 |
|
College (11,12) |
25 |
15.7 |
|
Graduation level and above |
53 |
33.4 |
|
Religion |
||
|
Muslim |
102 |
64.2 |
|
Hindu |
57 |
35.8 |
|
Husband’s occupation |
||
|
Unemployed |
5 |
3.1 |
|
Day laborer |
6 |
3.8 |
|
Rickshaw puller |
9 |
5.7 |
|
Garments worker |
42 |
26.4 |
|
Businessman |
33 |
20.8 |
|
Government service |
33 |
20.8 |
|
Private service |
31 |
19.4 |
|
Decision maker in their family |
||
|
Husband |
64 |
40.3 |
|
Both |
31 |
19.4 |
|
Mother in law |
64 |
40.3 |
Table- 1: Basic characteristics of the respondents (N=159).
It was observed that, majority (61.6%) of the respondents had came from lower economic class (monthly family income up to 20,000 BDT*) followed by 25.2% from middle class (monthly family income 21,000-40,000 BDT), 10.7% from upper middle class (monthly family income 41,000-60,000 BDT) and 2.5% from upper class (monthly family income >60,000 BDT) (Figure- 1).
It was found that, majority (89.9%) of the respondents were taking antenatal care (ANC) regularly during their last pregnancy (Table- 2). Most (91.8%) of the respondents received two or more tetanus toxoid injections during their last pregnancy, while 8.2% did not received it (Table- 2). Among the study subjects, 20.8% respondents had history of institutional delivery in the past and 79.2% respondent had no such history (Table- 2).
|
Previous antenatal history |
Frequency (n) |
Percentage (%) |
|
Regular antenatal care (ANC) |
||
|
Yes |
143 |
89.9 |
|
No |
16 |
10.1 |
|
Received tetanus toxoid injections |
||
|
Yes |
146 |
91.8 |
|
No |
13 |
8.2 |
|
Past institutional delivery |
||
|
Yes |
33 |
20.8 |
|
No |
126 |
79.2 |
Table- 2: Distribution of the respondents according to their previous antenatal history (N= 159).
Analysis of the complications of the respondents during antenatal period revealed that; 25.16% had excessive vomiting, 13.21% had bleeding, 12.57% had burning sensation during micturition, 9.43% had abnormal position of fetal head, 9.43% had backache, 7.55% had delivery after 2 weeks of expected date of delivery (EDD), 6.29% had twin pregnancy, 3.14% had convulsion/fits, but 13.20% had no complication during their antenatal period (Table- 3).
|
Complications in antenatal period |
Frequency (n) |
Percentage (%) |
|
Bleeding during Antenatal period |
21 |
13.21 |
|
Convulsion/Fits |
5 |
3.14 |
|
Abnormal position of fetal head |
15 |
9.43 |
|
Twin pregnancy |
10 |
6.29 |
|
Delivery after 2wks of EDD |
12 |
7.55 |
|
Burning micturition |
20 |
12.57 |
|
Excessive vomiting |
40 |
25.16 |
|
Backache |
15 |
9.43 |
|
No complication |
21 |
13.2 |
|
Total |
159 |
100 |
Table- 3: Distribution of the respondents by pattern of complications during antenatal period (N=159).
Analysis of complications which were arising previous delivery of the respondents showed that; 21.9% had excessive bleeding, 21.1% had perineal tear, 16.4% had developed urinary incontinence, 12.5% had birth injury of their child, 8.6% had prolonged labour, 3.9% had retained placenta, 15.6% had other complications and 19.49% had no complications (Table- 4).
|
Complications during previous delivery |
Frequency (n) |
Percentage (%) |
|
Perineal tear |
27 |
21.1 |
|
Urinary incontinence |
21 |
16.4 |
|
Birth injury of child |
16 |
12.5 |
|
Retained placenta |
5 |
3.9 |
|
Excessive bleeding |
28 |
21.9 |
|
Prolonged labour |
11 |
8.6 |
|
Others |
20 |
15.6 |
|
No complication |
31 |
19.49 |
|
Total |
159 |
100 |
Table- 4: Distribution of the respondents by complications that arising in previous delivery except the last one (N=159).
About the reason of institutional delivery it was found that, 48.41% came to avoid delivery related complications, 26.98% came for better delivery care and 24.61% came for safe delivery (Table- 5).
|
Reasons of institutional delivery |
Frequency (n) |
Percentage (%) |
|
For better care |
43 |
26.98 |
|
For safe delivery |
39 |
24.61 |
|
To avoid complications |
77 |
48.41 |
|
Total |
159 |
100 |
Table- 5: Distribution of the respondents according to the reasons of institutional delivery (N=159).
Analyzing the respondent’s source of influence about institutional delivery revealed that; 49.7% was influenced by their doctors, 27.1% was influenced by mass media (radio/television/cinema), 13.2% was by nurses and 10.0% by trained birth attendant (TBA) (Table- 6).
|
Influence about institutional delivery |
Frequency (n) |
Percentage (%) |
|
Doctors |
79 |
49.7 |
|
Radio/Television/Cinema |
43 |
27.1 |
|
Nurses |
21 |
13.2 |
|
Trained birth attendant (TBA) |
16 |
10 |
|
Total |
159 |
100 |
Table- 6: Distribution of the respondents on their source of influence about institutional delivery (n=159).
Data analysis revealed that 43.4% respondents had barrier for institutional delivery, but 56.6% had no barrier for institutional delivery (Table- 7).
|
Barrier for institutional delivery |
Frequency (n) |
Percentage (%) |
|
Yes |
69 |
43.4 |
|
No |
90 |
56.6 |
|
Total |
159 |
100 |
Table- 7: Distribution of the respondents according to barrier for institutional delivery (N=159)
Among the respondents [69 (43.4%)] having barrier for institutional delivery; we found 33.34% respondents had religious restriction, 30.43% had economic problem, 20.29% had decision making problem and 15.94% had distance barrier (Table- 8).
|
Barriers of institutional delivery |
Frequency (n) |
Percentage (%) |
|
Cost |
21 |
30.43 |
|
Decision |
14 |
20.29 |
|
Distance |
11 |
15.94 |
|
Religious restriction |
23 |
33.34 |
|
Total |
69 |
100 |
Table- 8: Distribution of the respondents according to causes of barrier in institutional delivery (n=69).
4. Discussion
It is important that mothers deliver their babies in an appropriate setting, where life-saving equipment and hygienic conditions are available that can help to reduce the risk of perinatal complications to mother and child [13, 14]. The risk of maternal death in developing countries is forty times higher than that of the developed world [15]. Bleeding, obstructed labor, hypertensive disorder, unsafe abortion and infection contribute for up to 80% of maternal deaths with resultant increased fetal loss, perinatal mortality and poor survival of new born babies [16]. This observational study was conducted in two separate centers namely- Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh and Jamalpur Sador Hospital, Jamalpur, Bangladesh. A total of 159 cases were selected by purposive sampling technique to identify the factors influencing institutional delivery. Developed countries are endowed with the appropriate health facilities; the demand for institutional/supervised delivery is more than a developing country [14, 17].
In this study mean(±SD) age of the study subjects was 28.4±7.2 years and the range was 18-38 years. In this series most (44.7%) of the respondents was in 20-25 years age group, the lowest (6.9%) number of respondents was in 18-20 years age group and 34% respondents was in 25-30 years age group. Of them majority (56.6%) was house wife followed by 27.0% was service holder, 13.2% was garments worker and 3.2% was day laborer. About educational status of the study population; majority (37.7%) of the respondents had secondary level education (Class 6-10), 33.4% had graduation and above level education, 15.7% of the respondents had up to college level education (class 11 to 12), 6.3% had primary level education (Class 1-5) and 6.9% was able to put their sign only. Among the respondents; 64.2% was Muslim and 35.8% was belongs to Hindu religion. Analyses of their husband’s occupation revealed that majority (26.4%) were garments worker, 20.8% were businessman and government service holder each and 19.5% were private service holder. Their husband (40.3%) and mother in low (40.3%) were equally predominant as decision maker of the family. It was observed that, majority (61.6%) of the respondents had came from lower economic class (monthly family income up to 20,000 BDT) and most (63.5%) of them were living in a nuclear family. These findings were consistent with related previous studies [14, 18, 19].
A study on prevalence of home deliveries and antenatal care coverage showed that there was a significant relation of place of delivery with family income of the respondents [20]. It was found that lower family income groups were preferred more home delivery [20, 21]. This current study shows that low income group respondents were came for the institutional delivery due to complications. In our study; types of family living among the study population showed 63.5% were in nuclear family. Predominant role in decision making of their family was husband and mother-in-law. In this context, in a previous study it was found that, husband's advice was the dominant feature for institutional delivery [19]. Furthermore, in many parts of Africa, women's decision making power is extremely limited, particularly in matters of reproduction and sexuality [22]. In this regard, decisions about maternal care are often made by husbands or other family members that supports to our study. It was reported that, a number of socio-demographic characteristics of the individual affect the underlying tendency to seek health care [23, 24]. Maternal education has been shown to be positively associated with the utilization of maternity care services which was similar to our study [23-25]. Although, in general, women in higher socioeconomic groups tend to exhibit patterns of more frequent use of maternal health services than women in the lower socioeconomic groups, factors such as education appear to be an important mediator [23, 24]. Another important factor in the utilization of maternity care services is the cultural background of the woman [26]. The cultural perspective on the use of maternal health services suggests that medical need is determined not only by the presence of physical disease but also by cultural perception of illness [23]. The use of modern health services in such a context is often influenced by individual perceptions of the efficacy of modern health services [27]. In this series 89.9% respondents of our study was taking antenatal care (ANC) regularly during their last pregnancy, majority (91.8%) of them received two or more tetanus toxoid injections during their last pregnancy. These finding were supported by a couple of related previous study [28, 29]. Analysis of complications of the respondents during their antenatal period revealed that, 25.16% had excessive vomiting followed by bleeding (13.21%), burning sensation during micturition (12.57%), abnormal position of fetal head (9.43%), backache (9.43%), childbirth after 2 weeks of expected date of delivery (7.55%), twin pregnancy (6.29%) and convulsion/fits (3.14%), while 13.20% had no complication during their antenatal period. In a related study it was found that, 16% of the respondents had complications during antenatal period [14]. Absence of complications during antenatal period was one of the reasons for avoiding institutional delivery [14]. Analysis of complications that arising previous delivery of the respondents showed that, 21.9% had excessive bleeding, 21.1% had perineal tear, 16.4% had developed urinary incontinence, 12.5% had birth injury of their child, 8.6% had prolonged labour, 3.9% had retained placenta, 15.6% had other complications and 19.49% had no complications. In this series, 23.22% of the respondents had to face complications in their past deliveries as reported in a previous study [30]. About the nature of complications as reported, prolong labour was the commonest than excessive bleeding were the second most common, perineal tear as the third ranking, and then retained placenta [14, 30]. In a previous study, complications during home delivery and postpartum period occurred in 24.32% of the complications, where prolonged labour was the most common [14]. Other complications were postpartum hemorrhage, perineal tear, uterine prolapsed, convulsion etc [14]. In Papua New Guinea, a high rate of obstetric complications was found amongst apparently normal pregnancies delivering at home and that study correlated to our study [31].
Among the study subjects, 20.8% respondents had history of institutional delivery in the past and 79.2% respondent had no such history. About the reason of institutional delivery it was found that, 48.41% came to avoid delivery related complications, 26.98% came for better delivery care and 24.61% came for safe delivery. Analyzing the respondent’s source of influence about institutional delivery revealed that; 49.7% was influenced by their doctors, 27.1% was influenced by mass media (radio/television/cinema), 13.2% was by nurses and 10.0% by trained birth attendant (TBA). Among total study subjects; 43.4% had barrier for institutional delivery but 56.6% had no barrier. Of them, 33.34% respondents had religious restriction, 30.43% had economic problem, 20.29% had decision making problem and 15.94% had distance barrier for institutional delivery. These findings were supported by a couple of previous study [21, 27]. Study by Wanjira et al. among 409 participants showed that 12.5% had never delivered in a health facility, of them; 27.5% said that they were willing to deliver in a maternity facility in future while 72.5% were not [27]. The most frequently mentioned reasons for never delivering in a health facility were; perceived delays in being attended (56.9%), fear of episiotomy (25.5%) while 17.9% felt it was risky to deliver at home and were therefore willing to deliver in a health facility [27].
Health information is a knowledge acquired whether through formal or informal education. Just like education, access to health information enable women to break away from tradition to utilize modern health facilities [32]. Therefore each pregnant woman could realize that an institutional delivery is safeguarding the health of their children and themselves [32].
5. Conclusion
This study investigated the factors for institutional delivery among Bangladeshi expectant mothers. We find out the evidence of income and access to health information in explaining the utilization of maternal health services and institutional delivery. Mother's education, monthly family income, antenatal complications had effect on institutional delivery. Socio-economic factors like- husband’s occupation, family types, religious believe, place of residence etc are found to be influencing for institutional delivery.
Limitation of the study
It was only two centers study with relatively short duration. Most of the respondents were from urban areas. So the findings were not the actual picture of entire country especially in the rural area of Bangladesh.
Recommendations
Institutional delivery is very much essential to prevent maternal complications. This study identified a lot of barrier obstructing institutional delivery. Proper antenatal care should be taken to prevent complication. Female education must be encouraged to improve the status of the women and to improve their knowledge level regarding maternal health services. Health education should provide to every pregnant woman to raise awareness about the danger signs of pregnancy and its consequences.
Conflict of interest
The authors declare no conflicts of interest regarding the publication of this paper.
References
- Who UNFPA U., Maternal Mortality in 2000: Estimates developed by WHO, UNICEF and UNFPA. Geneva, Department of Reproductive Health and Research, WHO(2004).
- Campbell OM, Graham WJ, Lancet Maternal Survival Series steering group. Strategies for reducing maternal mortality: getting on with what works. The lancet368 (2006):1284-1299.
- World Health Organization. The millennium development goals report.
- World Health Organization. Improving maternal, newborn and child health in the South-East Asia region. WHO Regional Office for South-East Asia(2005).
- Chowdhury AR, Mahbub A, Chowdhury AS. Skilled attendance at delivery in Bangladesh: an ethnographic study. Research and Evaluation Division, BRAC(2003).
- Shah IH, Say L. Maternal mortality and maternity care from 1990 to 2005: uneven but important gains. Reproductive health matters 15 (2007):17-27.
- Bhatia JC, Cleland J. Determinants of maternal care in a region of South India. Health transition review1(1995):127-142.
- Navaneetham K, Dharmalingam A. Utilization of maternal health care services in Southern India. Social science & medicine 55(2002):1849-1869.
- Gwatkin DR, Bhuiya A, Victora CG. Making health systems more equitable. The Lancet 64(2004):1273-1280.
- Witter S, Ensor T, Thompson R, Jowett M. Health Economics for Developing Countries. A Practical Guide. MacMillan Education(2000).
- Goodburn EA, Chowdhury M, Gazi R, Marshall T, Graham W. Training traditional birth attendants in clean delivery does not prevent postpartum infection. Health policy and planning 15(2000):394-399.
- Hossain I, Hoque M. Determinants of choice of delivery care in some urban slums of Dhaka City. Pakistan Journal of Social Sciences 3(2005):469-475.
- Montagu D, Yamey G, Visconti A, Harding A, Yoong J. Where do poor women in developing countries give birth? A multi-country analysis of demographic and health survey data. PloS one 6(2011):e17155.
- De Brouwere V, Richard F, Witter S. Access to maternal and perinatal health services: lessons from successful and less successful examples of improving access to safe delivery and care of the newborn. Tropical Medicine & International Health 15(2010):901-909.
- Mageda K, Mmbaga EJ. Prevalence and predictors of institutional delivery among pregnant mothers in Biharamulo district, Tanzania: a cross-sectional study. Pan African Medical Journal 21 (2015).
- Nigussie M, Mariam DH, Mitike G. Assessment of safe delivery service utilization among women of childbearing age in north Gondar Zone, North West Ethiopia. Ethiopian Journal of health development 18(2004):145-152.
- Abebe F, Berhane Y, Girma B. Factors associated with home delivery in Bahirdar, Ethiopia: a case control study. BMC research notes 5 (2001):1-6.
- Titaley CR, Hunter CL, Dibley MJ, Heywood P. Why do some women still prefer traditional birth attendants and home delivery?: a qualitative study on delivery care services in West Java Province, Indonesia. BMC pregnancy and childbirth 10 (2010):1-4.
- Furuta M, Salway S. Women's position within the household as a determinant of maternal health care use in Nepal. International family planning perspectives 1(2006):17-27.
- Barbhuiya MA, Hossain S, Hakim MM, Rahman SM. Prevalence of home deliveries and antenatal care coverage in some selected villages. Bangladesh Medical Research Council Bulletin 27 (2001):19-22.
- Bolam A, Manandhar DS, Shrestha P, Ellis M, Malla K, et al. Factors affecting home delivery in the Kathmandu Valley, Nepal. Health policy and planning 13(1998):152-158.
- World Health Organization (WHO). Improved access to maternal health services. World Health Organization (WHO), Geneva, Switzerland(1998).
- Addai I. Determinants of use of maternal–child health services in rural Ghana. Journal of biosocial science 32 (2000):1-5.
- Celik Y, Hotchkiss DR. The socio-economic determinants of maternal health care utilization in Turkey. Social science & medicine 50(2000):1797-1806.
- Stewart K, Sommerfelt AE. Utilization of maternity care services: A comparative study using DHS data. In Proceedings of the Demographic and Health Surveys World Conference 3 (1991): 1645-1668.
- Leslie J, Gupta GR. Utilization of formal services for maternal nutrition and health care. Washington DC: International Center for Research on Women (1989).
- Wanjira C, Mwangi M, Mathenge E, Mbugua G, Ng'ang'a Z. Delivery practices and associated factors among mothers seeking child welfare services in selected health facilities in Nyandarua South District, Kenya. BMC public health 11(2011):1-9.
- Akhtar HH. Review of performance of trained TBAs. Bangladesh Institute of Research for Promotion of Essential & Reproductive Health and Technologies(1995).
- Skinner J, Chandra A. Geography and racial health disparities. National bureau of economic research 95 (2003):13.
- Althabe F, Moore JL, Gibbons L, Berrueta M, Goudar SS, Chomba E, Derman RJ, Patel A, Saleem S, Pasha O, Esamai F. Adverse maternal and perinatal outcomes in adolescent pregnancies: The Global Network’s Maternal Newborn Health Registry study. Reproductive health 12 (2015):1-9.
- Garner P, Lai D, Baea M. Childbirth in rural areas: maternal deaths, village deliveries and obstetric service use. Papua and New Guinea medical journal. 37 (1994):166-172.
- Cleland JG, Van Ginneken JK. Maternal education and child survival in developing countries: the search for pathways of influence. Social science & medicine 27(12):1357-1368.