Factors Associated with the Low Immunization Coverage in the Second Year of Life in the Central Region of Burkina Faso
Article Information
Daniel KOALA*, 1, Marie-Laure KLEME2, Issa OUEDRAOGO3, Issoufou SAVADOGO3, Wendlasida Thomas OUEDRAOGO4, Alain Komi AHAWO5, Haoua TALL1, Koudmanegré Augustin ZOUNGRANA1
1Agence de Médecine Préventive, Ouagadougou, Burkina Faso
2Senghor University in Alexandria, Egypt
3Immunization Programs, Ministry of Health and Public Hygiene, Burkina Faso
4Regional Health Department of the Centre, Ministry of Health and Public Hygiene, Burkina Faso
5GAVI, Burkina Faso
*Corresponding author: Daniel KOALA, Agence de Médecine Préventive, Ouagadougou, Burkina Faso.
Received: 26 November 2022; Accepted: 05 December 2022; Published: 17 December 2022
Citation: Daniel KOALA, Marie-Laure KLEME, Issa OUEDRAOGO, Issoufou SAVADOGO, Wendlasida Thomas OUEDRAOGO, Alain Komi AHAWO, Haoua TALL, Koudmanegré Augustin ZOUNGRANA. Factors Associated with the Low Immunization Coverage in the Second Year of Life in the Central Region of Burkina Faso. Fortune Journal of Health Sciences 5 (2022): 596-602.
View / Download Pdf Share at FacebookAbstract
Introduction: The second year of life immunization is the administration of vaccines to a child between 12 and 24 months of age. After seven years of implementation of this immunization, the coverage remains low. This study was to understand the factors associated with low immunization coverage in the second year of life in Burkina Faso.
Methods: The LQAS method was used to conduct a cross-sectional household survey of children aged 24 to 35 months in two health districts in the Central region. A two-level random sampling was used. Eighteen health facilities were randomly selected and then in each health facility, 1 to 4 villages were randomly selected for the study. The households were visited to collect the data. In the selected health facilities, the EPI manager and health facilities manager were questioned about vaccination during the second year of life.
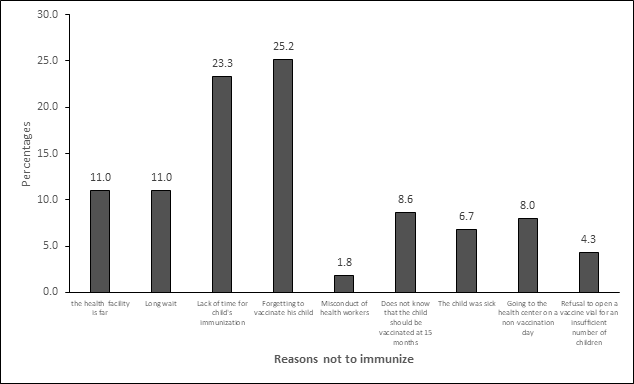
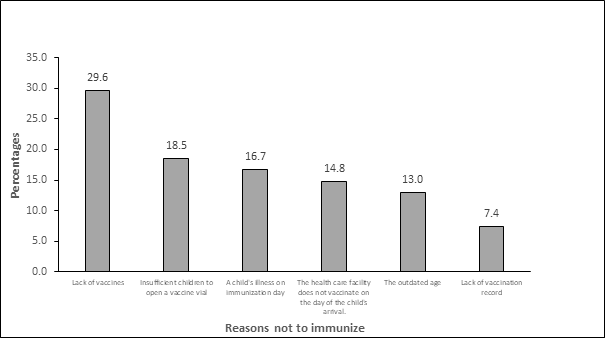
Results: Forgetting to vaccinate the child (25.1%), lack of time to go to health facilities on immunization day (23.3%), long waiting time in health facilities (11.0%) and far distance from the health facilities (11.0%) are the reasons given by mothers whose children did not receive MR2. Multiparous mothers were vaccinated with MR2 than Primiparous mothers (aOR = 2.4 et CI 95%=1.5 – 4.0). According to health workers, the main reasons were the lack of vaccine in 29.6% of cases and that there were not enough children to open 10 doses vial of the vaccine in 18.5% of cases.
Conclusion: Targeted interventions are needed to address these contributing factors to poor immunization coverage.
Keywords
Burkina Faso; Sub Saharan Africa; EPI immunization; second year of life; MCV1, MCV2, MR2; MCAV
Burkina Faso articles; Sub Saharan Africa articles; EPI immunization articles; second year of life articles; MCV1 articles, MCV2 articles, MR2 articles; MCAV articles
Article Details
1. Introduction
The second year of life immunization is the administration of vaccines to a child between 12 and 24 months of age [1]. According to the World health organization’s recommendation this immunization consists of several vaccines integrated into the Expanded Program on Immunization (EPI) Depending on the epidemiological profiles of countries [1]. The second year of life immunization has two main benefits. On the one hand, it strengthens immunity during early childhood and reduces the risk of measles, rubella, and meningococcal meningitis A outbreaks. On the other hand, it enables children to catch up on all the other vaccines they have not received during their first year of life. Thus, to achieve measles elimination, all countries must include the second Dose of the measles vaccine in the EPI. Countries are required to achieve 95% coverage for the first and second doses of the measles vaccine by 2020 to eliminate measles [2]. Following this guideline, countries in the WHO African Region have been phasing in the second dose of the measles vaccine in their routine immunization schedule. Their number increased from six in 2010 to 23 in 2015 and 27 in April 2019[2]–[5]. Immunization coverage varies from one country to another depending on the timing of the introduction of the second dose of vaccine. In general, countries were struggling to meet the region's target of at least 95% coverage by 2020 [4].
Some studies have documented the low immunization coverage of children in the second year of life. Indeed, from 1974 (the date of the WHO's Expanded Program on Immunization) to 2010, routine immunization was only provided in most African countries at age one [6]. Childhood immunization in the second year of life is a new concept for communities and health workers in that part of the world. Mothers' lack of awareness of second-year vaccines and the age of vaccination are reasons for low coverage [7]. Other reasons include discontinuity of immunization services in health facilities, lengthy waiting time on immunization days, unwillingness to open vials due to an insufficient number of children to avoid loss of doses, low level of training of health workers as well as the lack of human resources [1], [7]–[9]. In a study conducted in Ghana in 2017, only a third of the mothers of 18-month-old children attended the health facilities for immunization purposes [10]. In Tanzania, a study showed that offering immunization services less than 3 days per week, vaccine shortages, and unwillingness to open a vaccine vial due to insufficient numbers of children were significantly associated with low immunization coverage in the second year of life [11]. Finding strategies to improve immunization coverage in the second year of life was a priority for scientific and programmatic immunization experts in a 2016 survey [12].
The second year of life immunization began in October 2013 in Burkina Faso. The vaccines involved are the coupled measles, rubella (MR) vaccine, and the meningococcal A conjugate vaccine (MACV), as the country is part of the meningitis belt of Africa. These vaccines are given between 15 and 18 months of age [13]. After seven years of implementation and despite the renewed efforts to promote immunization in the second year of life and to catch up with children, immunization coverage remains low. According to WHO estimation data, coverage for the second dose of measles increased from 17% in 2014 to 71% in 2019 but is still far from the expected 95% target in 2020 [14]. Likewise, the 2020 vaccine coverage reported that the national survey, national MR2 coverage was 67% with MR1-MR2 wastage of 24.1% for a national target of 90% in 2020 [15], [16]. It was, therefore, important to identify factors associated with low immunization coverage in the second year of life to make suggestions for increasing immunization coverage.
2. Materials and Methods
2.1 Study framework
The Central region was purposely chosen for this study. We analyzed the MR2 vaccine coverage of the health districts (HDs) in this region. Data from 2014 to 2020 statistical yearbooks formed the basis of the analysis and were used to identify low-performing districts, which are the health districts of Baskuy and Boulmiougou. These districts formed our setting for the study. The health district of Baskuy is located in the center of the city of Ouagadougou, which is the capital of Burkina Faso. As the health district of Boulmiougou, it is located in the city of Ouagadougou with urban, peri-urban, and rural health facilities.
2.2 Type, period, and study population
We conducted a cross-sectional study from March to August 2021. Mothers of children aged 24 to 35 months interviewed in households and head nurses and EPI managers of the health facilities visited, were included in this study.
2.3 Sampling
The health districts of Boulmiougou and Baskuy have 38 and 9 health facilities that deliver immunization services, respectively. We proceeded with a two-level draw. A simple random draw was used to select 13 health facilities in Boulmiougou and 5 in Baskuy for this study.
2.3.1 Selection of villages and sub-districts
From each health facility, 1 to 4 villages or sub-districts were selected to participate in the implementation. A total of 51 villages and sub-districts were included in the study in the two health districts.
2.3.2 Household selection
The Lot Quality Assurance Sampling (LQAS) method was used. This is a statistical method of batch sampling. In each household, all targeted children were surveyed. The sampling was conducted in each locality with the support of a field guide.
All households in a village or sub-districts with fewer than 20 households were numbered. The first household is selected using a random number table. This is done by pointing to the table without looking and then moving across the table from near to right, reading the contiguous numbers in pairs. The first (two-digit) number between 1 and 20 is chosen as the number of the first household to be visited. When leaving the first household, we turned right and then skipped a household to survey the next household. If there was no target child, the next household immediately following was visited.
A village or sub-district with more than 20 households is divided into 4 zones. One of the 4 zones is chosen using the random number table. The team goes to the center of the chosen area and then flips a pen around to determine the direction of travel. The first household found in that direction is considered the starting point. Upon exiting the household, the team would also turn right, skipping two households. In a multi-story building, a floor is chosen with the random number table and then an apartment on that floor is chosen as the household to be surveyed.
The sample size of mothers is calculated with the Schwartz formula. Using the 2020 Central Region MR2 coverage of 59.1%, 95% confidence, and a 5% non-respondent rate, we obtained a sample size of 390 mothers of children aged 24 to 35 months. On average, 22 mothers should be surveyed in each health facility to meet the sample size.
As for the health workers, each health facility has only one manager and one EPI manager. Thus, out of the 18 health facilities, 36 health workers are expected to be in the sample.
An oral interview grid and semi-structured questionnaire were used to collect data from mothers and health workers respectively. This was a mobile data collection. The Open Data Kit (ODK) collect application was used. A total of 9 interviewers and 3 supervisors were recruited and trained to conduct the questionnaires and to use the Open Data Kit (ODK) collect on smartphones. The data collection took place from July 6 to 10, 2021 in households and health facilities. The questionnaires were entered directly into ODK collect. They were equipped with GPS coordinates to ensure the geographic position of the interviewer in the households. Once collected, the data were compiled in the form of an Excel table. These data were processed and analyzed using Epi info version 7.2. To investigate factors associated with MR2 immunization, we used logistic regression. Prevalence Odds-Ratio (ORP) and 95% confidence intervals (95% CI) were then calculated.
2.4 Ethical issues
Prior approval from the Ethics Committee for Health Research in Burkina Faso and clearance for collection from the Central Regional Health Department were obtained before starting the study. Participants in the study were informed of the relevance of the study and their informed consent was collected before the questionnaires were administered.
3. Outcomes
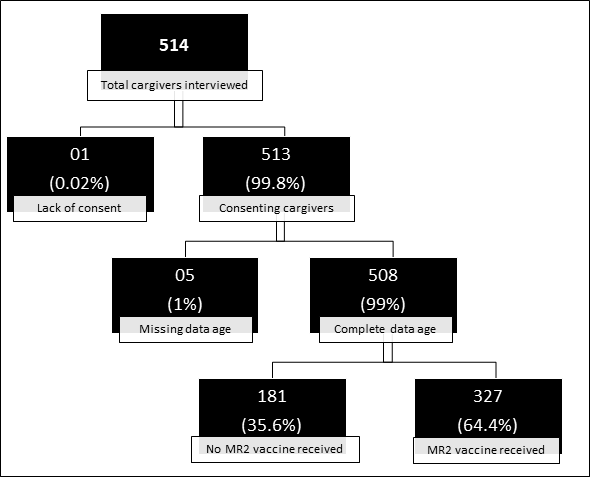
Altogether 514 mothers of children aged 24 to 35 months visited in the 18 health facilities in the districts of Baskuy and Boulmiougou. After validation of consent and age data, as many as 508 were considered for further analysis. The number of mothers interviewed varied from 8 to 43 per health facility visited. Only two health facilities failed to achieve the required number of 22 mothers. Among the health agents, 32 out of the 36 scheduled for the survey answered the questions, including 15 health facilities managers and 17 EPI managers. Figure 1 provides details of the data.
3.1 Interviewing the mothers
3.1.1 Socio-demographic profiles of mothers and children
The mean age of the mothers was 28.9 years (SD ± 5.8). Seventy-eight percent (78.0%) of them were multiparous. Almost half (40.3%) of the mothers had no formal education. The majority (85.6%) of the mothers lived within 30 minutes of the nearest health facility that offers vaccination services. Of the 508 children surveyed, 51.2% were girls and 48.8% were boys. Of these children surveyed, 329 had vaccination records, or 64.7%. Table 1 summarizes the socio-demographic profiles of the mothers and their children surveyed.
Table 1: Socio-demographic data of mothers and their children
|
Variables |
Frequency |
Percentage % |
|
Mean age of mother |
28.9 |
± 5.8 |
|
Mother's education |
||
|
Did not attend school |
205 |
40.3 |
|
Primary |
162 |
31.9 |
|
Secondary education and more |
141 |
27.8 |
|
Parity |
||
|
Primiparous |
112 |
22.1 |
|
Multiparous |
394 |
77.9 |
|
Time to get to the nearby health facility that vaccinates |
||
|
< 30 minutes |
435 |
85.6 |
|
≥ 30 minutes |
73 |
14.4 |
|
Gender of the child |
||
|
Male |
260 |
51.2 |
|
Female |
248 |
48.8 |
|
Is the child's health booklet available? |
||
|
Yes |
329 |
64.8 |
|
No |
179 |
35.2 |
3.1.2 Childhood immunization coverage indicators
It is worth noting that the gross immunization coverage (based on the vaccination record and the parents' recall) for the first dose of MR is 86.8%. The coverage for the second dose of MR and meningococcal A vaccine were 64.4% and 61.2%, respectively;
The MR1-MR2 dropout rate was 26.7%. Of the total of 508 children, 306 were fully vaccinated according to the EPI vaccine schedule, i.e. 60.2%.
The Table 2 below shows the gross vaccination coverage and the booklet by antigen.
Table2: indicators of gross immunization coverage and according to the child's immunization record
|
Indicators |
Antigens |
Proportion (%) |
CI to 95% |
|
Immunization coverage by a vaccination record |
MR1 |
94.5 |
91.5 – 96.5 |
|
MR2 |
69 |
63.8 – 73.7 |
|
|
MCAV |
66.6 |
61.3 – 71.4 |
|
|
Gross immunization coverage (reminder and vaccination record) |
MR1 |
86.8 |
83.6 – 89.5 |
|
MR2 |
64.4 |
60.1 – 68.4 |
|
|
MCAV |
61.2 |
57.0 – 65.4 |
Table 3: Factors associated with MR2 immunization
|
Variables |
Immunized with MR2 |
Not immunized with MR2 |
ORP |
CI to 95 % |
|
Mother's education level |
||||
|
Primary and more |
142 |
57 |
1 |
|
|
Did not attend school |
85 |
45 |
1.3 |
0.8 – 2.1 |
|
Parity of the mother |
||||
|
Primipare |
63 |
13 |
1 |
|
|
Multipare |
162 |
89 |
2.6 |
1.4 – 5.2* |
|
Time to get to the nearby health facility that vaccinates |
||||
|
< 30 minutes |
29 |
10 |
1 |
|
|
≥ 30 minutes |
198 |
92 |
1.3 |
0.6 – 3.0 |
|
Gender |
||||
|
Female |
120 |
41 |
1 |
|
|
Male |
107 |
59 |
1.5 |
0.9 – 2.4 |
3.1.3 Reasons accounting why children are not immunized and associated factors
Several reasons were given by mothers of children who were not up to date with immunization in the second year of life. Figure 2 shows the distribution of reasons for failure to be immunized.
No significant correlation was found between mothers' education, time to get to the immunizing health facility, and gender with MR2 gross immunization coverage according to the logistic regression. However, parity (aOR = 2.4; 95% CI = 1.5 to 4.0) was significantly associated with MR2 immunization coverage. The logistic regression data are summarized in Table 3.
3.2 Interviewing health workers
3.2.1 Profiles of health workers
The median age of the health workers was 46.6 years, with a minimum and maximum of 38 to 54 years, respectively. Half (53.0% or 17 agents) of the health workers were the expanded program on immunization managers in the health facilities. Of the 17 of the EPI managers, 15 were itinerant health workers (The lowest level of the paramedical profession in Burkina Faso).
3.2.2 Knowledge of health workers
Thirty workers (94%) reported being familiar with childhood immunization in the second year of life. Among them, 26 health workers (87%) were familiar with the appropriate age of administration and the types of vaccines to be administered during this period.
Approximately one-third (28%) of the health workers had not received immunization training that included a module on the second year of life immunization.
3.2.3 Reasons accounting why children are not immunized
All of the 32 health workers surveyed reported reasons for not administering vaccines during the second year of life in the health facilities. The most common reasons given were the out-of-stock of vaccines and the insufficient number of children that does not meet the required number to open a 10-dose vial for immunization. Figure 3 shows the reasons for non-immunization according to health workers.
4. Discussion
Childhood immunization in the second year of life has been implemented in Burkina Faso since 2013 with the introduction of the second dose of the measles vaccine. In 2015 the rubella vaccine was combined with the measles vaccine (MR). In 2017, the meningococcal A conjugate vaccine (MCVA) was introduced into the immunization schedule. These shots are given between 15 and 18 months of age. Until 2021, there are no guidelines for childhood immunization in the second year of life. And, immunization coverage is low. We estimated the immunization coverage and investigated the factors associated with low coverage in the central region of the country.
MR1 (86.8%) and MR2 (64.3%) coverages are low to ensure group immunity toward eliminating measles. These coverage levels in the study are very close to those in the administrative data for these two districts in 2020. Similar immunization coverage was found in studies in the Northern Region of Ghana in 2017, and in Malawi in 2016 [7], [10]. Lower coverage was found in a similar study in Tanzania where less than 50% of children were immunized with the second dose of measles [11]. In general, sub-Saharan Africa has low second-dose measles immunization coverage. As a result of the recent introduction of the second dose, some parents still believe that immunization is limited to 9 months of age in Burkina Faso. Mothers resume their daily activities as their children gain some motor autonomy after one year of age. Immunization after this period is no longer a priority or they forget about it because of their busy lives.
A total of 125 children in this study did not receive a dose in the second year of life. The most common reasons reported by mothers were, in descending order, forgetting to immunize the child, lack of time to get to the health facility, and lengthy waiting time for immunization. In the 2020 Burkina Faso Immunization Coverage Survey, the reasons for not immunizing were classified into three categories for children aged 24 to 35 months. The top ranking was the lack of information with 55% of the reasons, the second was barriers (insecurity; busy mother/caregiver; covid-19 epidemic, and long distance to immunization services) with 27% and the third was lack of motivation with 12% [15]. In our context, failure to immunize children is not related to carelessness but rather to parents' lack of information and the constraints they face in fully immunizing their children. The time that elapses between the MR1 and MR2 immunization is quite long enough for a mother to remember her child's immunization date. In addition to forgetting the date, at 15 months of age, the child becomes increasingly independent and the mother returns to full-time activities after extended months of missed and irregular work. Since vaccination hours and working hours are the same, it is difficult for a working mother to wait for long periods in a health facility to immunize her child. Hence the interest in setting up strategies to remind mothers of the timing of their children's immunization and to involve men in the process of immunizing their children. In Tanzania, unawareness of the 15-18 months contact, unwillingness to open a vial for a few children, and lengthy waiting time were significantly associated with failure to immunize with MR2 [11]. Multiparous mothers were more likely to have their children immunized in the second year of life than primiparous mothers. Very often, multiparous mothers have already been in contact with immunization services, are more familiar with the immunization schedule, and know the benefits of immunization. Unlike young mothers who are in their first contact with immunization services and have to be educated about everything.
For health workers, the potential reason for not immunizing in the second year of life is the limited number of children required before a 10-dose vial can be opened, in addition to vaccine shortages. Results from other studies in Burkina Faso, sub-Saharan Africa, and Cambodia corroborate our findings [7]–[9], [17]. The recommended vaccine wastage rate is an EPI performance indicator set at 25%. Thus, opening a 10-dose vial of measles-rubella vaccine or meningococcal A vaccine for one or two children is a huge waste and decreases the performance of the health facility. During a qualitative study conducted in Burkina Faso in 2018, a health worker said, «If it is one child or two children, you cannot open the 10-dose vial. A minimum of 5 children must be gathered to open it. However, if we only have 2 or 3 children attending a vaccination session, then we ask the mother to come back the following week, and that discourages them. In the same study, a district EPI manager said: "Imagine that I have 3 children for MR1 and 2 for MR2, for a total of 5 children. The minimum number of children required to open my 10-dose MR vial is met. On the other hand, it is not enough to open the MCVA vial as I only have 2 eligible children. Opening and administering 2 doses will result in a waste of 8 doses. Under such a situation, what should be done to minimize the wastage?" [9]. Reducing the number of doses per vial would reduce wastage and motivate healthcare providers to administer more doses at immunization sessions. In a study conducted in Zambia and released in 2020, health facilities were selected to receive 5-dose vials of measles vaccine for an assessment of the impact on immunization coverage compared to health facilities using 10-dose vials. The findings show an intervention effect of 5 percentage points for the first dose and an effect of 3.5 percentage points for the second dose. The wastage rate was 16.2% in facilities using 5-dose vials and 30.5% in those using 10-dose vials [8].
Limitations of the study
Our sample included only two health districts in the central region. Thus, the Central Region is not representative of Burkina Faso, which has 13 health regions.
In addition, data collection took place during the rainy period. In rural and semi-urban areas, families were busy with rural activities. Some mothers were not available.
Some data on children's immunization status were collected based on the mother's recall and not based on the immunization record. Recall biases may influence raw immunization coverage.
5. Conclusion
Not remembering to immunize a child, not having enough time to get to the health facility, waiting a long time for immunization sessions, and being a primiparous are community factors associated with poor immunization coverage in the second year of life. At the health system level, other than vaccine shortages, insufficient numbers of children to open a 10-dose vial, illness of the child on the day of immunization, and coming to the health facility outside of immunization days are the major factors associated with poor immunization coverage.
Targeted interventions are needed to address these contributing factors to poor immunization coverage. A needs assessment study of the community and of the health facilities that are involved in immunization activities to strengthen the immunization of children in the second year of life would be useful.
Conflicts of Interest
The authors declare no conflicts of interest
Acknowledgments
We thank the Ministry of Health and Public Hygiene for allowing us to conduct this study, the Senghor University of Alexandria for its educational support, and the Agence de Médecine Préventive (AMP) of Burkina Faso for its technical and financial support.
References
- WHO, UNICEF, « Establishing and strengthening immunization in the second year of life: immunization practices beyond infancy », WHO (2018).
- BG Masresha, R Luce, J Okeibunor, ME Shibeshi, R Kamadjeu et A. Fall, « Introduction of the Second Dose of Measles Containing Vaccine in the Childhood Vaccination Programs Within the WHO Africa Region – Lessons Learnt », J Immunol Sci (2018): 113-121.
- M K Patel et al., « Progress Toward Regional Measles Elimination — Worldwide, 2000–2019 », MMWR Morb Mortal Wkly Rep 69 (2020): 1700-1705.
- B Masresha, R Luce, P Tanifum, E Lebo, A Dosseh, et al. « The African Region early experience with structures for the verification of measles elimination – a review », Pan Afr Med J 35 (2020).
- BG Masresha et al., « Progress Toward Measles Elimination - African Region, 2013-2016 », MMWR Morb Mortal Wkly Rep 66 (2017).
- K VanderEnde, M Gacic-Dobo, MS Diallo, LM Conklin, et al. « Global Routine Vaccination Coverage - 2017 », MMWR Morb Mortal Wkly Rep 67 (2018).
- G Chirwa, KA Wilkins, et al. « Descriptive study of measles vaccination second dose reporting and barriers to improving coverage in six districts in Malawi », Pan Afr Med J 35 (2020).
- K Krudwig et al., « The effects of switching from 10 to 5-dose vials of MR vaccine on vaccination coverage and wastage: A mixed-method study in Zambia », Vaccine 38 (2020).
- SF Nkwenkeu et al., « Health workers’ perceptions and challenges in implementing meningococcal serogroup a conjugate vaccine in the routine childhood immunization schedule in Burkina Faso », BMC Public Health 20 (2020).
- M Nyaku et al., « Immunization delivery in the second year of life in Ghana: the need for a multi-faceted approach », Pan Afr Med J 27 (2017).
- R Magodi, EJ Mmbaga, J Massaga, D Lyimo, A Mphuru, et al,. « Factors associated with non-uptake of measles-rubella vaccine second dose among children under five years in Mtwara district council, Tanzania, 2017 », Pan Afr Med J 33 (2019): 67.
- JL Kriss et al., « Research priorities for accelerating progress toward measles and rubella elimination identified by a cross-sectional web-based survey », Vaccine 37 (2019).
- Ministry of Health, "Immunization Guide for Health Care Workers. " May (2018).
- WHO, World Health, « Immunization Country Profile » (2020).
- Ministry of Health, "Results of the routine immunization coverage survey of children aged 12 to 35 months in Burkina Faso," Ministry of Health, Ouagadougou (2020).
- Ministry of Health, " Complete Multi-Year Plan 2016-2020 Burkina Faso," October (2015).
- S. Wallace et al., « Assessment of vaccine wastage rates, missed opportunities, and related knowledge, attitudes and practices during introduction of a second dose of measles-containing vaccine into Cambodia’s national immunization program », Vaccine, 36 (2018): 4517-4524.