Factors Affecting Mortality in the Transfusion of Concentrate of Hemacies in Pediatric Patients: A Systematic Review
Article Information
Eduardo Manoel Pereira, Woryk de Souza Schröder Nowak*, Caciano Vinicius Krenchinski, Lucas Renato Rocha
School of Medicine, Department of Clinical Pharmacology, University of the Region of Joinville, Joinville, Brazil
*Corresponding Author: Woryk de Souza Schröder Nowak, University of the Region of Joinville, School of Medicine, R. Ministro Calógeras, 439-Centro, Joinville, SC, Brazil
Received: 30 September 2019; Accepted: 18 October 2019; Published: 29 November 2019
Citation:
Eduardo Manoel Pereira, Woryk de Souza Schröder Nowak, Caciano Vinicius Krenchinski, Lucas Renato Rocha. Factors Affecting Mortality in the Transfusion of Concentrate of Hemacies in Pediatric Patients: A Systematic Review. Journal of Pediatrics, Perinatology and Child Health 3 (2019): 194-200.
View / Download Pdf Share at FacebookAbstract
Objectives: To present the impact of the various factors that affect mortality in pediatric patients who require red blood cell transfusion in the most diverse situations.
Method: This is a systematic review, conducted according to the PRISMA methodology, linking randomized controlled trials and meta-analyzes of the last ten years in the English language, through a search in the electronic indexer PUBMED. The selected studies included patients of both sexes, without race restrictions, aged 18 years or less, submitted to a red cell transfusion procedure, regardless of the cause of transfusion, in articles published between 2006 and 2016.
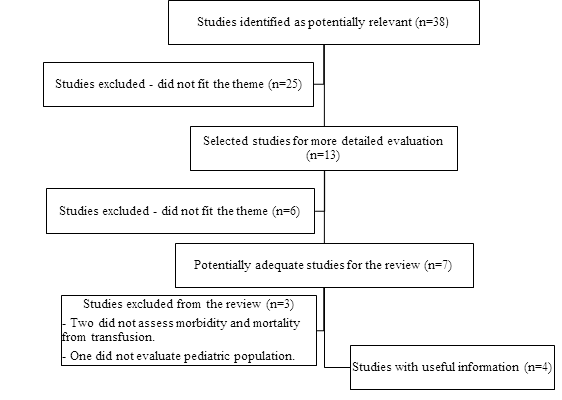
Results: 38 articles were searched, of which 34 were excluded after the selection screen, resulting in 4 articles for the analysis. The main results found reinforce the efficacy of transfusion restriction protocols compared to liberal protocols in relation to hemoglobin values. Also, no relationship was found between storage time and mortality. It has been identified that the main cause of mortality for chronically transfused patients is due to infections.
Conclusions: Red blood cell transfusion in pediatric populations is a subject that needs further studies to measure the real impact on mortality.
Keywords
Transfusion, Pediatric Patients, Mortality
Article Details
1. Introduction
The red blood cell transfusion consists in an infusion of red blood cells to restore a condition of acute or chronic anemia [1-3]. Red blood cell transfusion leads to better tissue oxygenation by increasing the amount of red blood cells and blood volume in cases of significant loss. Therefore, it is able to reduce the signs and symptoms associated with cases of severe anemia, including the cardiac effects related to the bad distribution of oxygen [2]. Blood transfusion is associated with complications that may occur even after administration of small volumes such as acute transfusional hemolytic reaction [1], nonhemolytic febrile transfusion reaction [4], urticaria and anaphylaxis as acute forms of presentation and late transfusion hemolytic reaction, autoimmunization by human leukocyte antigen, graft in comparison of host transfusion disease, and iron overload as forms of late presentation [1]. Seeking the best treatment, the pediatric population should receive special attention to cases of transfusion need to follow strict protocols due to greater sensitivity of these patients to the intrinsic risks of transfusion, such as the unpredictability of acute transfusion reactions [1, 5]. Considering the risks involved in the blood transfusion procedure and the different characteristics of the pediatric patients that make them subject to complications, this paper intends to present the impact of the several factors that affect mortality in pediatric patients who require blood transfusion in the most diverse situations.
2. Methodology
This is a systematic review study, conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) 6]. Randomized controlled clinical trials and meta-analyzes of the last ten years were selected in English using of the electronic indexer PUBMED with the following keywords: “Blood Transfusion” and “Mortality” with age filters “infant”, “child” and “adolescent”. After conducting the research in the database, a first selection of the results was performed by means of the title. The resulting articles moved to the next step where the selection was made by summary. In cases where the summary reading was not sufficient to evaluate the possibility of inclusion, the article was read in its entirety by two of the researchers to determine their eligibility. In case of disagreement a third researcher evaluated the article. After this step, all the resulting articles were read in full, and the finalists were elected for that study. The selected studies included patients of both sexes, without race restrictions, aged 18 years or less, submitted to a red cell transfusion procedure, regardless of the cause of transfusion, in articles published between 2007 and 2017. We excluded studies that did not refer to the population defined above and did not present as outcome the mortality and morbimortality.
3. Results
After applying the search strategy described above were identified thirty-eight articles, of which twenty-five were excluded after analysis of securities by explicitly not relate to the subject or do not involve the population studied. Of the thirteen remaining articles, six were excluded after reading the abstracts, as they did not correlate with the theme or population proposed for the study. The remaining seven articles were for a more thorough review by the authors with the full text reading and of these two were excluded by significant differences in the outcome since they did not evaluate the factors that interfered in the mortality by transfusion of packed red blood cells, but in the use of a clotting factor to avoid transfusion. In addition, one article was excluded because it did not refer to pediatric patients. The process can be visualized through the organization chart of Figure 1. Four articles were selected for this study, represented in Table 1.
|
Author, year |
Locality |
Study design |
Sample |
|
Cholette et al. [7] |
Rochester, New |
Cohort |
One hundred and twenty-eight patients |
|
Kirpalani et al. [8] |
Canada, United States |
Randomized controlled trial |
Seven hundred and ninety-five patients with birth |
|
Karam et al. [9] |
USA, Canada, UK |
A prospective, multicenter, |
One hundred and thirty seven stable pediatric patients |
|
Mokhtar et al. [10] |
Cairo, Egypt |
Retrospective study |
Four hundred and forty-seven patients with |
Table 1: Selected articles for the study.
In the study by Cholette et al., a retrospective cohort of children under the age of eighteen who underwent palliative or reparative surgeries with cardiopulmonary bypass, analyzed one hundred twenty-eight transfusions to demonstrate the impact of the storage time of red cells in morbimortality. All blood products were pre-stocked irradiated and with ABO identical. Perioperative management, anesthesia and postoperative management were performed as usual. The cardiac surgeons were blinded to avoid bias in the surgical treatment. Obvious differences in the packaging and labeling of blood products prevented the blushing of perfusionists and anesthesiologists [7]. All patients were managed intraoperatively with unfractionated heparin adjusted according to coagulation time and reversed with protamine. All patients received epsilon acid with aminocaproic acid. Conventional ultrafiltration was employed for all study subjects. All subjects affected by deep hypothermic circulatory arrest and children younger than or equal to six months received intravenous corticosteroids (solumedrol 0.5 mg/kg). Vasoactive drugs were used to maintain hemodynamics during the procedure, at the discretion of the cardiac surgery team [7].
Of the one hundred and sixty-two participants, thirty-four (21%) received no blood products, seventeen in each group. About 58% received less than or equal to two transfusions [7]. Mortality was low (4.9%) and no association was found between the storage time of packed red blood cells and survival. The postoperative infection rate was significantly higher in children who received blood with longer storage times (25 to 38 days) compared to blood with shorter storage times (7 and 15 days) (34% versus 7%; p=0.004) [7]. In the study by Kirpalani et al., a randomized controlled trial was conducted in which four hundred fifty-one premature children with low weight, selected from ten pediatric intensive care units from the USA, Canada and Australia, with lower birth weight at 1000 g, gestational age less than thirty-one weeks and with less than two days of birth were divided into two groups, elaborated according to the Guideline of the Canadian Society of Pediatrics, with different levels of hemoglobin (one of high threshold and another low threshold) for indication of red blood cell transfusion [8]. The purpose of the study was to verify if there was a significant difference in the clinical outcome in the first weeks of life of children with low birth weight undergoing red blood cell transfusion considering the hemoglobin threshold [8].
The low transfusion threshold group presented central capillarity with respiratory support varying from values less than or equal to 77 g/L up to 115 g/L and without respiratory support, of values less than or equal to 68 g/L up to 100 g/L. In those with a higher threshold, with respiratory support values less than or equal to 90 up to 135 g/L and without respiratory support from 77 g/L up to 120 g/L [8]. The two groups were similar in relation to maternal and infant variables, including those that reflect the severity of the disease [8]. From initially similar levels, hemoglobin declined over time in both treatment groups, but with a consistently higher weekly mean in the high threshold group [8]. As a result of maintaining a reduced level of hemoglobin, the low threshold group received fewer red blood cell transfusions (mean 4.9 units) than the high threshold group (mean 5.7 units), this difference did not reach significance (p<0.070). However, the mean number of transfusions was significantly lower in the low threshold group. The total number of these transfusions was 7.4% in the low-threshold versus 3.1% in the high-threshold [8]. The primary endpoint analyzed was the combination of death or survival with bronchopulmonary dysplasia, retinopathy of severe prematurity, or brain injury [8]. During the neonatal period, 74.0% of the low threshold group had any of the outcomes evaluated (bronchopulmonary dysplasia, retinopathy of severe prematurity, or brain injury) compared to 69.7% of infants allocated to the high threshold cohort. Regarding mortality, the low threshold group presented 21.5% of deaths compared to 17.5% in the high threshold group. However, none of these results presented statistical significance [8].
Karam et al., in a prospective multicenter, randomized controlled trial conducted in pediatric intensive care units in four countries (Belgium, United States, United Kingdom and Canada) analyzed the outcome of red blood cell transfusion in pediatric patients with sepsis severe or septic shock by means of two conduits: one restrictive and one liberal [9]. The authors defined the protocol applied in the study considering as eligible children aged between three days and fourteen years with hemoglobin concentration less than or equal to 9.5 g/dL within the first seven days in the pediatric ICU and hemodynamically stabilized. Patients with systemic arterial pressure of not less than two standard deviations for age and who have not received cardiovascular support (fluids, vasoactive and inotropic drugs) for at least two hours before being selected for the study were considered stable [9].
The authors defined a hemoglobin threshold for transfusional indication of 7 g/dL for hemoglobin as a target for hemoglobin values between 8.5 and 9.5 g/dL, while the liberal strategy had a transfusional threshold of 9.5 g/dL with a target between 11 and 12 g/dL. This strategy was applied for twenty-eight days after randomization or until death [9]. The primary endpoint analyzed was the development of progressive multiple organ dysfunction syndrome, considered if the patient had one or more organ failure after the beginning of the study [9]. In a total of 5399 patients evaluated after a screening process, 648 were randomized into two groups. Of these, 511 were not included in the septic picture being withdrawn from the study, remaining 137 with sepsis or septic shock. The 137 patients were randomly divided into two groups for the application of the two types of strategies. In a group of 69 patients the restrictive strategy was applied and in the other with 68 the liberal strategy [9]. In the restrictive group, thirty-nine of the patients (56%) received at least one blood transfusion while in the liberal strategy group sixty-seven (99%) received at least one transfusion and this difference was statistically significant (p<0.01) [9].
In the restrictive strategy group, thirteen patients (18.8%) developed multiple organ dysfunction progressive syndrome, which is the same number as the liberal strategy group, which corresponds to 19.1% of the patients, and there was no statistically significant difference in the occurrence of this outcome (p=0.97) [9]. Regarding the number of deaths in 28 days, seven patients (10%) of the restrictive group died compared to two patients (3%) of the liberal group, but this difference was not statistically significant (p=0.08) [9]. The only difference statistically significant was related to the number of nosocomial infections that affected twelve patients (17%) of the restrictive group compared to twenty three (34%) of the liberal group. (p=0.02) [9].
Mokhtar et al., demonstrated in a retrospective study carried out at the Thalassemia Center of the Ain Shams University Children's Hospital in Egypt, in which 447 patients with transfusion dependent thalassemia B were recruited who were followed up in January 2000 and January 2010 for the morbidity and mortality parameters, standards and mortality rate of these patients, in addition to comparing with the age of onset, type, duration and adherence to iron chelation therapy and frequency of blood transfusion [10]. Patients were collected as demographic data: transfusion history, history of splenectomy and history of chelation and complications, complete physical examination and anthropometric measurements. Morbidity data were collected as signs and symptoms. The investigation included renal, hepatic, cardiac and endocrine morbidities [10]. Patients were divided into two groups: serum ferritin levels greater than 1500 ng/dL (group 1) and serum ferritin levels below 1500 ng/dL (group 2). The mean ferritin level was calculated with mean serum ferritin for the last two years prior to the study [10].
Of the 447 patients, 64.4% were men and 36.6% were women. Of these, 21.1% had transfusions every 2 weeks, 72.3% every month and 7.6% every 2 months. Concerning morbidity, 44.7% of the individuals presented endocrine dysfunction, 41.3% cardiovascular morbidities, 40.5% hepatic, 4.1% renal and 3.4% changes in bone mineral density [10]. In the comparison between groups considering demographics and clinical data, the only statistically significant difference was previous splenectomy that was performed in 53.1% of patients in group 1 versus 42.5% in group 2 [10]. Regarding the comparative morbidity between groups, cardiac complications related to decreased left ventricular contractility were 38.2% in group 1 versus 27.5% in group 2 (p=0.21), with a higher presence of osteoporosis in group 1 (5.3%) than in group 2 (1.3%) (p=0.31). Hypogonadism was observed in group 1 of 46.4% compared to 36.2% in group 2 (p=0.38) [10]. Regarding the other complications (arrhythmia, pulmonary hypertension, renal complications, elevation of liver enzymes, positive viral markers, diabetes mellitus, thyroid and parathyroid disorders), no statistically significant difference was found [10]. A mortality rate of 1.5% was found to be the most common cause of death in patients with thalassemia infections, with a survival rate of 80% at 5 years, 50% at 10 years, and 20% at 20 years [10].
4. Discussion
Halogen blood transfusion is associated with potential complications such as acute transfusion reaction, infections, and immunosuppression. To reduce such risks, halogen transfusion should be minimized [1]. The use of blood components should be sufficient for clinical maximization of results without, however, representing an increase in the risk of side effects whether they are infectious or not [1]. There is limited evidence of high quality of the risks and benefits of red blood cell transfusion [1]. In the study by Kirpalani et al., with four hundred and fifty-one premature infants, with gestational age of less than thirty-one weeks, low-weight hemoglobin was used for transfusion (90 to 135 g/L with respiratory support (77 g/L up to 115 g/L with respiratory support and 68 g/L up to 100 g/L without respiratory support) as a parameter for transfusion has no advantages because it did not present statistically significant changes on the evaluated outcomes and mortality [8].
In the study by Karam et al., when assessing the transfusion of red blood cells in pediatric patients with severe sepsis or septic shock, no difference was found regarding the development of progressive multiple organ dysfunction syndrome when compared to a strategy of restrictive behavior of hemoglobin for transfusional indication of 7 g/dL aiming to reach hemoglobin values between 8.5 and 9.5 g/dL) with a liberal strategy (transfusion threshold of 9.5 g/dL with target between 11 and 12 g/dL). The restrictive group received a significantly lower number of transfusions, with no significant difference in mortality [9]. Thus, this study also points to the non-inferiority of restrictive behaviors in relation to more liberal behaviors, and can be adopted as alternatives in order to avoid the complications of multiple transfusions [1, 8, 9].
In the retrospective cohort of Cholette et al., when analyzing one hundred and twenty-eight transfusions of children under eighteen years submitted to palliative or reparative surgeries with cardiopulmonary bypass, there was no association between the storage time of red blood cells and survival of patients. However, it has indicated that there is an influence on the rate of postoperative infections, which increase as the storage time increases [7]. In the retrospective study by Mokhtar et al., transfusions were evaluated in pediatric patients with transfusion dependent thalassemia B. The chronic deleterious effect of iron accumulation on target organs resulting from multiple red blood cell transfusions was an important cause of morbidity (endocrine, cardiovascular, hepatic, renal, and bone mineral density changes). However, the main cause of death identified in this study were infections, with patients presenting an average survival of 20% in 20 years [10].
5. Conclusion
The red blood cell transfusion in pediatric populations is a subject that needs further studies to measure the real impact on mortality, especially considering that certain groups require periodic transfusions, such as those with some types of congenital anemia. All this must be taken into account for establishments of correct transfusion thresholds in order to minimize possible deleterious effects, such as the acute transfusion hemolytic reaction.
References
- Fung MK, Grossman BJ, Hilyer CD, et al. Technical Manual of American Association of Blood Banks (AABB). (18th) Bethesda: AABB (2014).
- Lena M Napolitano, Stanley Kurek, Fred A Luchette, et al. Clinical practice guideline: red blood cell transfusion in adult trauma and critical care. Crit Care Med 37 (2009): 3124-3157.
- Klein HG, Spahn DR, Carson JL. Red blood cell transfusion in clinical practice. Lancet 370 (2007): 415-426.
- Bachowski G, Borge D, Brunker PAR, et al. A Compendium of Transfusion Practice Guidelines. (3rd) American Red Cross (2013).
- New FV, Berryman J, Bolton-Maggs PHB, et al. Guideline on transfusion for fetuses, neonates and older children. British Journal of Haematology 175 (2016): 784-828.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine 6 (2009): e1000097.
- Cholette JM, Pietropaoli AP, Henrichs KF, et al. Longer RBC storage duration is associated with increased postoperative infections in pediatric cardiac surgery. Pediatr Crit Care Med 16 (2015): 227-235.
- Kirpalani H, Whyte RK, Andersen C, et al. The Premature Infants in Need of Transfusion (PINT) study: a randomized, controlled trial of a restrictive (low) versus liberal (high) transfusion threshold for extremely low birth weight infants. J Pediatr 149 (2006): 301-307.
- Karam O, Tucci M, Ducruet T, et al. Canadian Critical Care Trials Group and the PALISI Network. Red blood cell transfusion thresholds in pediatric patients with sepsis. Pediatr Crit Care Med 12 (2011): 512-518.
- Mokhtar GM, Gadallah M, El Sherif NH, et al. Morbidities and mortality in transfusion-dependent Beta-thalassemia patients (single-center experience). Pediatr Hematol Oncol 30 (2013): 93-103.