Evaluation of Pandemic Influenza A (H1N1) Pneumonia Patients Followed up in Intensive Care Unit from the Perspective of COVID-19
Article Information
Pakize Özçiftci llmaz*, Barçln Öztürk, Ali Rlza Ka?nlcl, Mustafa Deniz, Ali Ihsan Sert, Öngün ?ahin, Can Karaman, Ibrahim Kurt
Intensive Care Unit, Aydln Adnan Menderes University, Aydln, Turkey
*Corresponding Author: Pakize Özçiftci llmaz, Intensive Care Unit, Aydln Adnan Menderes University, 09100, Aydln, Turkey
Received: 10 February 2021; Accepted: 02 March 2021; Published: 15 March 2021
Citation: Pakize Özçiftci Yılmaz, Barçın Öztürk, Ali Rıza Kağnıcı, Mustafa Deniz, Ali İhsan Sert, Öngün Şahin, Can Karaman, İbrahim Kurt. Evaluation of Pandemic Influenza A (H1N1) Pneumonia Patients Followed up in Intensive Care Unit from the Perspective of COVID-19. Archives of Clinical and Medical Case Reports 5 (2021): 314-324.
View / Download Pdf Share at FacebookAbstract
Introduction: Influenza A (H1N1) virus have been a serious problem in 2009, which was considered as a pandemic and caused the death of more than 12000 people. Pneumonia is the most common complication of influenza infection and can be seen as viral pneumonia and/or bacterial coinfection. However, since November 2019, the world has been exposed to a new pneumonia agent named SARS - CoV - 2 from the Coronavirus family. In this case series, we aimed to re-evaluate the cases we followed up in the intensive care unit due to severe pandemic Influenza A infection between November 2019 and March 2020 from the Covid-19 perspective.
Cases: There were five cases diagnosed with pandemic influenza A (H1N1) pneumonia in intensive care between November 2019 and March 2020, and the average age was 50. Given the risk factors two patients had immunosuppression and two patients had diabetes. Fever, respiratory distress and cough were the most prominent symptoms, and involvement in both lungs was detected in all patients on radiological imaging. Unfortunately, all patients had died despite antiviral therapy, antibiotic treatment against secondary bacterial infection, hemodynamic and respiratory support treatments.
Discussion: Considering the literature, covid-19 and influenza co-infections have been detected in 34 cases since November 2019. In general terms, covid-19 and influenza tables are similar, with slight differences. In this case we look back to our findings, similar cases are considered as covid-19 under current conditions.
Keywords
Covid-19; Pneumonia; Influenza A; Case series
Covid-19 articles; Pneumonia articles; Influenza A articles; Case series articles
Covid-19 articles Covid-19 Research articles Covid-19 review articles Covid-19 PubMed articles Covid-19 PubMed Central articles Covid-19 2023 articles Covid-19 2024 articles Covid-19 Scopus articles Covid-19 impact factor journals Covid-19 Scopus journals Covid-19 PubMed journals Covid-19 medical journals Covid-19 free journals Covid-19 best journals Covid-19 top journals Covid-19 free medical journals Covid-19 famous journals Covid-19 Google Scholar indexed journals Pneumonia articles Pneumonia Research articles Pneumonia review articles Pneumonia PubMed articles Pneumonia PubMed Central articles Pneumonia 2023 articles Pneumonia 2024 articles Pneumonia Scopus articles Pneumonia impact factor journals Pneumonia Scopus journals Pneumonia PubMed journals Pneumonia medical journals Pneumonia free journals Pneumonia best journals Pneumonia top journals Pneumonia free medical journals Pneumonia famous journals Pneumonia Google Scholar indexed journals Influenza A articles Influenza A Research articles Influenza A review articles Influenza A PubMed articles Influenza A PubMed Central articles Influenza A 2023 articles Influenza A 2024 articles Influenza A Scopus articles Influenza A impact factor journals Influenza A Scopus journals Influenza A PubMed journals Influenza A medical journals Influenza A free journals Influenza A best journals Influenza A top journals Influenza A free medical journals Influenza A famous journals Influenza A Google Scholar indexed journals pandemic influenza articles pandemic influenza Research articles pandemic influenza review articles pandemic influenza PubMed articles pandemic influenza PubMed Central articles pandemic influenza 2023 articles pandemic influenza 2024 articles pandemic influenza Scopus articles pandemic influenza impact factor journals pandemic influenza Scopus journals pandemic influenza PubMed journals pandemic influenza medical journals pandemic influenza free journals pandemic influenza best journals pandemic influenza top journals pandemic influenza free medical journals pandemic influenza famous journals pandemic influenza Google Scholar indexed journals Dissemination articles Dissemination Research articles Dissemination review articles Dissemination PubMed articles Dissemination PubMed Central articles Dissemination 2023 articles Dissemination 2024 articles Dissemination Scopus articles Dissemination impact factor journals Dissemination Scopus journals Dissemination PubMed journals Dissemination medical journals Dissemination free journals Dissemination best journals Dissemination top journals Dissemination free medical journals Dissemination famous journals Dissemination Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Colon Cancer articles Colon Cancer Research articles Colon Cancer review articles Colon Cancer PubMed articles Colon Cancer PubMed Central articles Colon Cancer 2023 articles Colon Cancer 2024 articles Colon Cancer Scopus articles Colon Cancer impact factor journals Colon Cancer Scopus journals Colon Cancer PubMed journals Colon Cancer medical journals Colon Cancer free journals Colon Cancer best journals Colon Cancer top journals Colon Cancer free medical journals Colon Cancer famous journals Colon Cancer Google Scholar indexed journals Sporadic articles Sporadic Research articles Sporadic review articles Sporadic PubMed articles Sporadic PubMed Central articles Sporadic 2023 articles Sporadic 2024 articles Sporadic Scopus articles Sporadic impact factor journals Sporadic Scopus journals Sporadic PubMed journals Sporadic medical journals Sporadic free journals Sporadic best journals Sporadic top journals Sporadic free medical journals Sporadic famous journals Sporadic Google Scholar indexed journals
Article Details
1. Introduction
In 2009, World Health Organization declared the influenza A (H1N1) virus a pandemic that affected 190 countries starting from Mexico and caused a serious problem, resulting in the death of more than 12000 people. The effects of the pandemic continued until 2014 [1]. Report by CDC (USA Centers for Disease Control and Prevention), stated that 25% of patients who were hospitalized during this period were followed up in the intensive care unit with pneumonia picture, with 60% requiring mechanical ventilatory support [2]. Although pregnancy, asthma, chronic obstructive pulmonary disease, obesity, immunosuppression, chronic liver and kidney diseases are the major risk factors in terms of the severity of the disease, one-third of the patients followed up in the intensive care unit have been found to have no underlying comorbidity [3].
Pneumonia is the most common complication of influenza infection, which may present with viral pneumonia and/or bacterial coinfection. Patients with influenza pneumonia requiring mechanical ventilatory support are at high risk for rapid progression to acute respiratory distress syndrome (ARDS). During the H1N1 pandemic, 50-70% of patients followed up in the intensive care unit developed ARDS [4].
In November 2019, the world faced with the COVID-19 (SARS COV-2 infection) pandemic caused by a viral pathogen named SARS-CoV-2 from the coronavirus family. It may cause a range of diseases from the simple common cold to severe conditions such as pneumonia, severe ARDS, coagulopathy, multi-organ failure, and death [5].
The aim of this case series was to re-evaluate the patients we followed up in the intensive care unit for severe pandemic influenza A infection between November 2019 and March 2020 from the perspective of COVID-19.
2. Case Presentation
2.1 Case 1
During the follow-up of a 60-year-old female patient who received steroid treatment in the Rheumatology clinic with the diagnosis of Sjögren syndrome, he began to have fever and increasing dry cough. At that time, it was thought that the fever of the patient, who had no pathology on the chest computed tomography and had growth in the urine culture, might be due to urinary infection (Figure 1). Due to the addition of respiratory distress, sputum, hyponatremia, and impaired consciousness to the current picture of the patient who was given antibiotic therapy, she was intubated and transferred to the intensive care unit. Macrolide was added to the current treatment of the patient who had a reduction in the lower left lung ventilation on the chest radiograph with the pre-diagnosis of atypical pneumonia. A viral panel was requested for viral pneumonia due to low levels of C reactive protein (CRP) and leukopenia in the patient whose general condition continued to deteriorate despite antibiotic therapy and who developed hypotension. The condition of the patient, who was found to be positive for Pandemic Influenza A as a result of the viral panel, rapidly deteriorated, and she died due to multiorgan failure and diffuse intravascular coagulation.
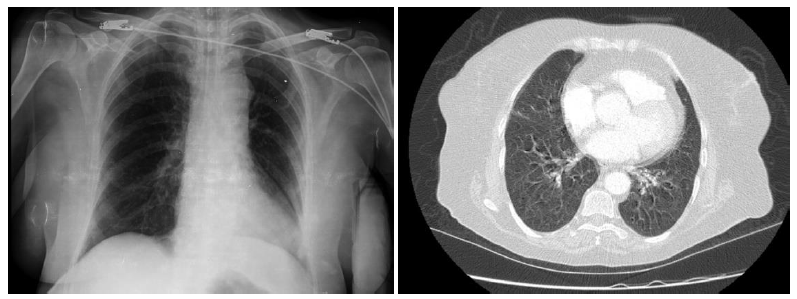
Figure 1: Case 1- Chest X-ray and thorax computed tomography section.
2.2 Case 2
Thoracic computed tomography of a 47-year-old male patient, who had no diseases other than diabetes mellitus in his medical history and presented to the emergency department with the complaints of respiratory distress and dry cough, revealed bilateral, predominantly peripheral-subpleural patchy areas of ground-glass opacities in the lungs (Figure 2). The patient who had hypoxemia in blood gas was transferred to the intensive care unit. Ceftriaxone, macrolide and oseltamivir treatments were initiated with pre-diagnoses of viral pneumonia and atypical pneumonia. Viral panel was requested. Pandemic influenza A was detected. The patient who initially received noninvasive mechanical ventilation was intubated, and it was switched to noninvasive mechanical ventilation from invasive mechanical ventilation due to the deepening of hypoxemia under treatment. His medical treatment was revised due to the addition of bacterial co-infections to his medical picture during the follow-up. However, the patient who did not respond to the treatment died.
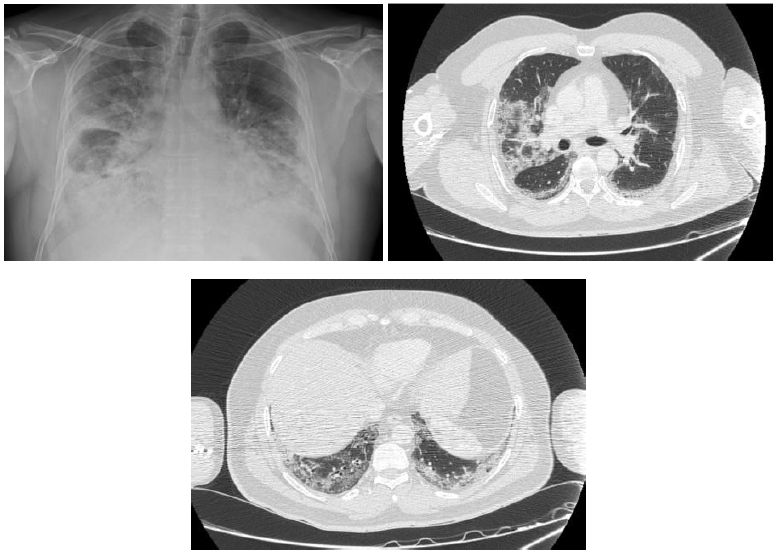
Figure 2: Case 2- Chest X-ray and thorax computed tomography sections.
2.3 Case 3
A 24-year-old male patient who presented to the emergency department of another center with the addition of respiratory distress to upper respiratory tract symptoms persisting for a week was admitted to the intensive care unit due to hypoxemia, and noninvasive mechanical ventilatory support and oseltamivir treatment were initiated. The patient, whose hypoxemia deepened despite noninvasive treatment and who was intubated on the second day of his hospitalization, was followed up to continue his treatment. In his chest computed tomography, patchy areas of ground-glass opacity, more prominent in the lower zones of both lungs, were detected (Figure 3). The viral panel requested was positive for pandemic influenza A. As the acute kidney injury progressed during the follow-up of the patient, the patient was included in the hemodialysis program. Lung-protective ventilation strategies were started for the patient who developed acute respiratory distress syndrome (ARDS) and had progression on chest radiograph under treatment. Extracorporeal membrane oxygenation (ECMO) was administered to the patient who did not respond to treatment. The patient, whose condition gradually worsened, died from severe hypoxia and sudden bleeding.
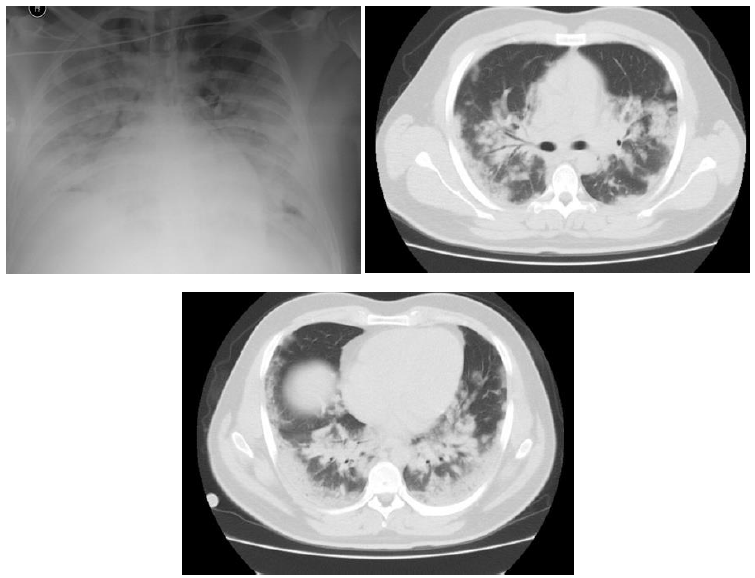
Figure 3: Case 3- Chest X-ray and thorax computed tomography sections.
2.4 Case 4
A 55-year-old female patient with a medical history of breast cancer operation presented to her family doctor with complaints of headache, fatigue, and diffuse body pain persisting for a week. The patient who presented to emergency department due to the addition of cough, sputum, and dyspnea to her complaints under oral antibiotherapy was admitted to the Thoracic Diseases Clinic since bilateral infiltration were noted in the middle and lower lung zones on chest radiograph (Figure 4). The patient with increasing dyspnea and worsened hypoxemia during the follow-up while receiving antibiotic and antiviral therapy was transferred to the intensive care and intubated. Lung-protective ventilation was administered to the patient who was evaluated to have ARDS. The viral panel result was positive for pandemic influenza A. The patient, who developed bacterial coinfections during the follow-up and whose clinical condition deteriorated under treatment, died.

Figure 4: Case 4- Chest X-ray.
2.5 Case 5
A 64-year-old male patient with a history of hypertension, coronary artery disease, and diabetes mellitus presented to another center with fever, cough, and dyspnea on exertion, and the thoracic computed tomography revealed areas of significant consolidation in each lung's upper lobe, and bilateral pleural effusion (Figure 5). The patient was referred to our hospital and transferred to the intensive care unit. His antibiotic and antiviral treatment was arranged. The viral panel result was positive for pandemic influenza A. The patient was switched to invasive mechanical ventilation due to the failure of improving oxygenation with noninvasive mechanical ventilation and the progression of the ARDS. The patient developed pneumomediastinum and subcutaneous emphysema during the follow-up. The ventilator settings of the patient who did not need tube thoracostomy were revised. The patient whose creatinine values increased and who developed oliguria received hemodialysis. Despite the treatment, the patient with deteriorated clinical condition died.
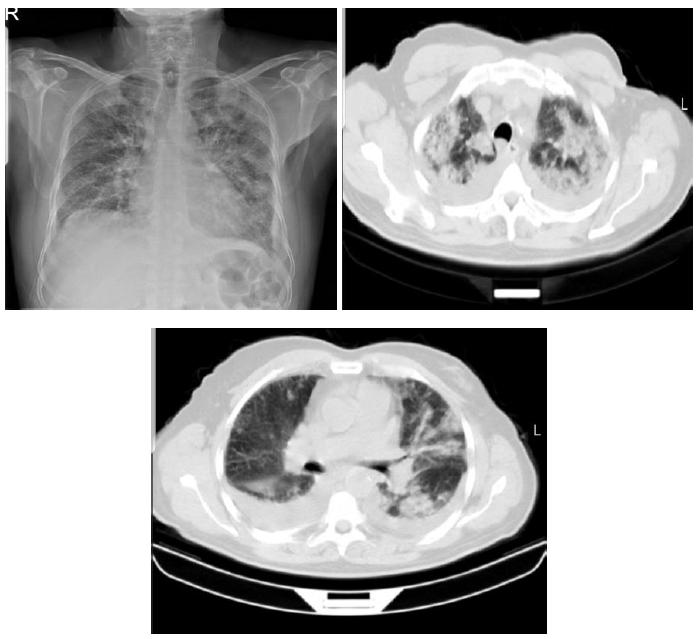
Figure 5: Case 5- Chest X-ray and thorax computed tomography sections.
CRP: C - Reactive Protein; WBC: White Blood Cell; AST: Aspartate Aminotransferase; LDH: Lactate Dehydrogenase
Table 1: Laboratory values for intensive care admission.
|
Case S.no |
APACHE II |
SOFA |
PSI |
The duration of mechanical ventilation (day) |
Length of stay in the ICU (day) |
Length of stay in hospital (day) |
|
Case 1 |
23 |
9 |
120 |
13 |
13 |
13 |
|
Case 2 |
16 |
7 |
107 |
17 |
21 |
23 |
|
Case 3 |
24 |
9 |
96 |
7 |
7 |
7 |
|
Case 4 |
13 |
2 |
85 |
23 |
26 |
26 |
|
Case 5 |
25 |
9 |
194 |
24 |
30 |
31 |
APACHE II: Acute Physiology and Chronic Health Evaluation; SOFA: Sequential Organ Failure Assessment Score; PSI: Pneumonia Severity Index
Table 2: Intensive care admission scores, mechanical ventilator and length of stay.
3. Discussion
Throughout the history, the world has witnessed many viral pandemics that killed millions of people. While the medical world was expecting a new Influenza A pandemic after 2009, it faced the coronavirus pandemic. After the first coronavirus case was reported in November 2019, it spread faster than anyone could have predicted, and the epidemic turned into a pandemic. The first case in our country was identified in March 2020. Our study aimed to evaluate our Pandemic Influenza A (H1N1) patients, who were followed up in our intensive care clinic between November 2019 and March 2020 and unfortunately died, from the perspective of COVID-19. Meta-analyses have shown that 22% of community-acquired pneumonias are due to viral agents, and most of them are associated with influenza [6]. In 11-35% of influenza cases, bacterial co-infections accompany the medical picture [6]. Therefore, the diagnosis of influenza may remain in the background or not be considered. There was growth in the admission cultures of three of our patients.
The mortality rate of severe influenza patients followed up in the intensive care unit ranges from 7% to 58%, although it varies in studies [7-9]. Age, higher APACHE II score, requirement for mechanical ventilation and dialysis were associated with mortality in a study including patients between 2009 and 2015 [8, 10]. Mortality was found to be higher in the 50-65 age group compared to other age groups [8]. The mortality rate of patients who are followed up in the intensive care unit for COVID-19 ranges from 0.7% to 52.4% [11].
While most of our patients presented with fever, cough and dyspnea, one patient presented with headache and generalized body pain. In their study comparing the clinical features of COVID-19 with influenza, Zayet et al. found similar frequency of fever, cough, fatigue, headache and myalgia symptoms, with no significant difference [12]. A study comparing COVID-19 and influenza-related ARDS patients found no difference in terms of neutrophil-to-lymphocyte ratio, hemoglobin, thrombocyte and creatinine values, but found significantly higher aspartate transaminase (AST), lactate dehydrogenase (LDH) and D-Dimer values in the influenza group. In the same study, C-reactive protein (CRP) levels were found to be significantly higher in the COVID-19 group [9]. While AST was normal in two patients in our case series, LDH and CRP were higher in all patients (Table 1, 2).
In Influenza (H1N1) pneumonia, radiological abnormality is more prominent in basal and central lung areas, and bilateral alveolar involvement is observed [13]. The most common radiographic findings are ground-glass opacities and consolidation, followed by a reticular pattern [1]. Similar to influenza, ground-glass opacities and consolidations are the most common findings of COVID-19 pneumonia. However, it is believed that lower lobe involvement is more pronounced in COVID-19 compared to diffuse involvement of all lobes in influenza [14]. Some studies have stated that ground-glass opacities are unilateral, multifocal and peripheral in the early stage of the disease, and with the progression of the disease, they turn into bilateral, diffuse consolidation areas [15]. Examining the radiological imaging results of our patients at the time of admission, it was seen that one patient had no radiological finding, then an infiltration appeared in the lower left lung, while other patients had bilateral ground-glass opacity, especially more pronounced in the basal segments. One patient had bilateral pleural effusion accompanied by ground-glass opacity.
In conclusion, the manifestations of COVID-19 and influenza are similar, with slight differences. Patients admitted with a clinical picture similar to the cases mentioned above are evaluated as potential COVID-19 patients under current conditions. This brings to mind a number of possibilities; 1) Although the first case in Turkey was reported in March 2020, cases before this date could have been caused by coronavirus. 2) Strict rules for the COVID-19 pandemic may have prevented the influenza A pandemic. 3) Reviewing the literature, COVID-19 and influenza coinfections have been detected in 34 cases since November 2019 [16, 17]. However, the coexistence of influenza and COVID-19 may be more common than we think. Independent of COVID-19, pandemic influenza A should be kept in mind, especially in patients who present with viral pneumonia during the winter months.
References
- Rohani P, Jude CM, Chan K, et al. Chest Radiological Findings of Patients With Severe H1N1 Pneumonia Requiring Intensive Care. J Intensive Care Med 31 (2016): 51-60.
- Jain S, Kamimoto L, Bramley AM, et al. 2009 Pandemic Influenza A (H1N1) Virus Hospitalizations Investigation Team. Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med 361 (2009): 1935-1944.
- World Health Organization. Clinical management of human infection with pandemic (H1N1) (2009).
- Li SH, Hsieh MJ, Lin SW, et al. Outcomes of severe H1N1 pneumoniae: A retrospective study at intensive care units. J Formos Med Assoc 119 (2020): 26-33.
- Gürlevik SL, Koronavirüsler ve Yeni Koronavirüs SARS-CoV-2. J Pediatr Inf 14 (2020): 46-48.
- Cantan B, Luyt CE, Martin-Loeches I. Influenza Infections and Emergent Viral Infections in Intensive Care Unit. Semin Respir Crit Care Med 40 (2019): 488-497.
- Duggal A, Pinto R, Rubenfeld G, et al. Global variability in reported mortality for critical illness during the 2009-10 influenza A(H1N1) pandemic: a systematic review and meta-regression to guide reporting of outcomes during disease outbreaks. PLoS One 11 (2016): e0155044.
- Chao CM, Lai CC, Chan KS, et al. Outcomes of patients with severe influenza infection admitted to intensive care units: a retrospective study in a medical centre. J Med Microbiol 66 (2017): 1421-1428.
- Tang X, Du RH, Wang R, et al. Comparison of Hospitalized Patients With ARDS Caused by COVID-19 and H1N1. Chest 158 (2020): 195-205.
- Marin-Corral J, Climent C, Muñoz R, et al. Patients with influenza A (H1N1)pdm09 admitted to the ICU. Impact of the recommendations of the SEMICYUC. Med Intensiva 42 (2018): 473-481.
- Serafim RB, Póvoa P, Souza-Dantas V, et al. Clinical course and outcomes of critically ill patients with COVID-19 infection: a systematic review. Clin Microbiol Infect 23 (2020): S1198-743X(20)30648-0.
- Zayet S, Kadiane-Oussou NJ, Lepiller Q, et al. Clinical features of COVID-19 and influenza: a comparative study on Nord Franche-Comte cluster. Microbes Infect 22 (2020): 481-488.
- Adlgüzel N, Karakurt Z, Balcl MK, et al. Influenza A (H1N1) virus pneumonia in intensive care unit. Tuberk Toraks 58 (2010): 278-285.
- Onigbinde SO, Ojo AS, Fleary L, et al. Chest Computed Tomography Findings in COVID-19 and Influenza: A Narrative Review. BioMed Research International (2020).
- Shi H, Han X, Jiang N, et al. “Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study,” The Lancet Infectious Diseases 20 (2020): 425-434.
- Ozaras R, Cirpin R, Duran A, et al. Influenza and COVID-19 coinfection: Report of six cases and review of the literature. J Med Virol 92 (2020): 2657-2665.
- Antony SJ, Almaghlouth NK, Heydemann EL. Are coinfections with COVID-19 and influenza low or underreported? An observational study examining current published literature including three new unpublished cases. J Med Virol 92 (2020): 2489-2497.
