Evaluation of Hemostatic Compression on Radial Artery Occlusion After Trans Radial Percutaneous Coronary Intervention
Article Information
Atikur Rahman1*, Tariq Ahmed Chowdhury2, A K S Zahid Mahmud Khan3, Fahdia Afroz4, Mohammad Faridul Hoque5, Mizanur Rahman Majumder6, Mahmudul Hasan Masum7, Ferdous Jahan8
1Assistant Registrar, Department of Cardiology, National Institute of Cardiovascular Diseases & Hospital (NICVD), Dhaka, Bangladesh.
2Assistant Professor, Department of Cardiology, National Institute of Cardiovascular Diseases & Hospital (NICVD), Dhaka, Bangladesh.
3Assistant Professor, Department of Cardiology, National Institute of Cardiovascular Diseases & Hospital (NICVD), Dhaka, Bangladesh.
4Associate Professor (C.C) & Resident Physician, National Institute of Cardiovascular Diseases & Hospital (NICVD), Dhaka, Bangladesh.
5Assistant Professor, Department of Cardiology, Colonel Maleque Medical College & Hospital, Manikganj, Bangladesh.
6Registrar, Department of Cardiology, National Institute of Cardiovascular Diseases & Hospital (NICVD), Dhaka, Bangladesh
7Registrar, Department of Cardiology, National Institute of Cardiovascular Diseases & Hospital (NICVD), Dhaka, Bangladesh.
8Resident, Department of Neonatology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh.
*Corresponding author: Atikur Rahman, Assistant Registrar, Department of Cardiology, National Institute of Cardiovascular Diseases & Hospital (NICVD), Dhaka, Bangladesh.
Received: 11 February 2024; Accepted: 20 February 2024; Published: 19 March 2024
Citation: Atikur Rahman, Tariq Ahmed Chowdhury, A K S Zahid Mahmud Khan, Fahdia Afroz, Mohammad Faridul Hoque, Mizanur Rahman Majumder, Mahmudul Hasan Masum, Ferdous Jahan. Evaluation of Hemostatic Compression on Radial Artery Occlusion After Trans Radial Percutaneous Coronary Intervention. Cardiology and Cardiovascular Medicine. 8 (2024): 96-101.
View / Download Pdf Share at FacebookAbstract
Background: Radial artery occlusion (RAO) is a significant concern in the trans-radial approach (TRA), limiting future use of the radial artery for procedures such as coronary artery bypass graft surgery (CABG), invasive hemodynamic monitoring, and arterio-venous fistula creation for hemodialysis in chronic kidney disease (CKD) patients through the same vascular approach. This study aimed to evaluate the hemostatic compression on radial artery occlusion after trans-radial percutaneous coronary intervention.
Methods: This prospective observational study was conducted in the Department of Cardiology, National Institute of Cardiovascular Diseases (NICVD), Dhaka, Bangladesh from September 2018 to August 2019. A total of 140 patients who underwent percutaneous coronary intervention (PCI) through TRA were randomly enrolled and divided into two groups, with 70 cases in each. Group I underwent 2-hour hemostatic compression after trans-radial PCI, while Group II received 6-hour hemostatic compression after the procedure. For data analysis, SPSS version 23.0 was applied.
Results: In this study, early radial artery occlusion was observed in 4.3% of patients in group I and 12.8% in group II (P=0.04). Similarly, late radial artery occlusion occurred in 2.8% of patients in group I and 11.4% in group II, with a statistically significant difference (P=0.04). Multivariate logistic regression analysis identified predictors of radial artery occlusion, including a hemostatic compression time of 6 hours (P=0.01), postprocedural nitroglycerine use (P=0.03), and procedure time (P=0.03).
Conclusion: A shorter duration of hemostatic compression is associated with a lower incidence of early and late radial artery occlusion after transradial intervention.
Keywords
Radial artery occlusion; RAO; Trans-radial approach; Percutaneous coronary intervention; PCI; CKD
Article Details
1. Introduction
Radial artery occlusion (RAO) is a significant complication following radial artery catheterization, often asymptomatic but with potentially serious consequences such as hand ischemia [1]. The incidence of RAO shortly after the procedure varies widely in the literature, ranging from 2% to 18% [2]. Assessment methods include the radial pulse method, Barbeau's test (Plethysmography evidence), and color Doppler study. In a study by Huang et al., immediate occlusion rates were 4.7% by the radial pulse method (absent pulse) and 10.7% by the Doppler study [3]. Another study evaluating RAO by plethysmography evidence reported rates of 12% with traditional hemostatic methods and 5% with patent hemostatic methods at a 24-hour follow-up [4]. The variability in the rate of radial artery occlusion (RAO) can be attributed to the persistent presence of the radial pulse even after occlusion, with the occluded radial artery distal stump maintaining a palpable pulse due to macro-collateral circulation from the palmar arches, reaching up to 70% of mean arterial pressure [5]. RAO is influenced by various demographic, clinical, and peri-procedural factors, including low body weight, female gender, anticoagulant use and dosage, radial artery diameter, sheath size, number of catheters, procedure duration, and type and duration of access site compression after the procedure [6,7]. A recent study in India by Garg et al. identified lower BMI, diabetes mellitus, pre-procedural radial artery diameter ≤ 2.5 mm, low pre-procedural peak systolic velocity, and radial artery to sheath ratio <1 as additional predictors of RAO [8]. Data on coronary procedures through the trans-radial approach (TRA) in the Bangladeshi population are limited. A study by Patwary et al. reported radial artery spasm in 7.5% of cases during coronary angiography (CAG) [9]. Another thesis study conducted at NICVD by Kabir et al. found a higher radial artery spasm rate of 17.1% [10]. In a thesis by Matin et al. at NICVD, radial artery occlusion (RAO) was reported to be 9.6% [11]. Additionally, a study by Samir B. Pancholy and Tejas M. Patel demonstrated that patients receiving hemostatic compression for 2 hours after the procedure had a significantly lower incidence of early (24 hrs.) and chronic (30 days) RAO, as defined by Doppler ultrasound, compared to those with 6 hours of compression after the procedure. The study found that demographic and procedural variables were similar between the two groups. Early (24 hrs.) radial artery occlusion occurred in 5.5% of patients in the 2-hour compression group and 12% in the 6-hour group, with a statistically significant difference (P=0.025). Chronic (30 days) radial artery occlusion occurred in 3.5% of patients in the 2-hour compression group and 8.5% in the 6-hour group, with a statistically significant difference (P=0.035). Occlusive compression was identified as the only independent predictor of radial artery occlusion (Odds ratio=13.1, P=0.001). The study concluded that 2-hour compression was superior to 6-hour compression in preventing radial artery occlusion after trans-radial percutaneous coronary intervention [12].
2. Methodology
From September 2018 to August 2019, a prospective observational study was carried out at the Department of Cardiology, National Institute of Cardiovascular Diseases (NICVD) in Dhaka, Bangladesh. A total of 140 patients who underwent percutaneous coronary intervention (PCI) via the trans-radial approach (TRA) were randomly assigned and categorized into two groups, each consisting of 70 cases. Group I received 2-hour hemostatic compression following trans-radial PCI, whereas Group II underwent 6-hour hemostatic compression post-procedure. RAO was defined as the absence of antegrade flow, monophasic flow, or inverted flow in the Duplex study. Radial arterial blood flow was assessed early (24 hours) and late (30 days) using a color duplex study after the procedure in both groups. The study received approval from the ethical committee of the mentioned hospital, and proper written consent was obtained from all participants before data collection. All patients routinely underwent pre-procedural and post-procedural 12-lead ECG at a paper speed of 25 mm/s and 10 mm/mV standardization. As baseline investigations, 12-lead ECG, RBS, serum creatinine, screening blood tests for CAG & PCI, and echocardiography were carried out and noted. Duplex assessment of the radial artery was done early (after 24 hours) and late (after 30 days). Demonstration of flow, flow direction, flow pattern (laminar, turbulent), flow profile (monophasic, biphasic, tri-phasic, inverted), and flow velocity were recorded. All demographic and clinical information of the participants were recorded. Data were analyzed using SPSS version 23.0. In statistical analysis, a P-value < 0.05 was considered as the indicator of significance.
3. Results
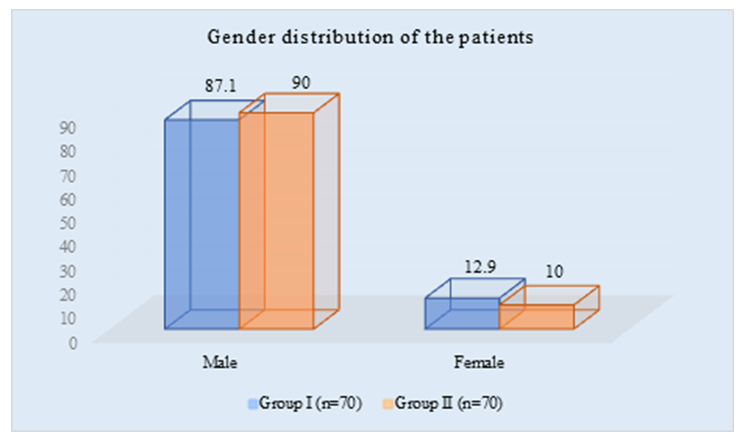
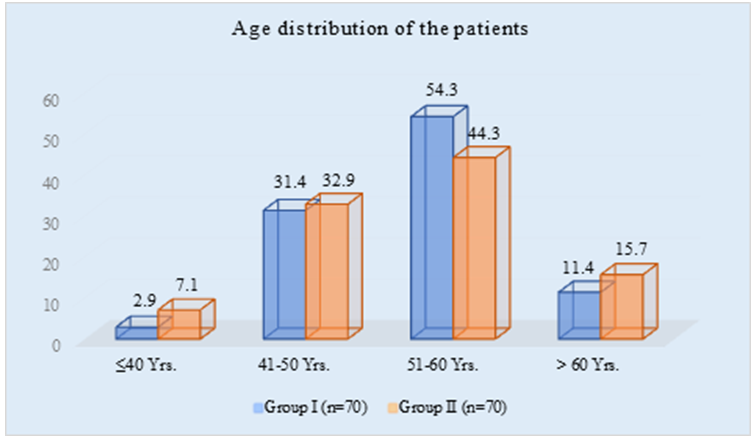
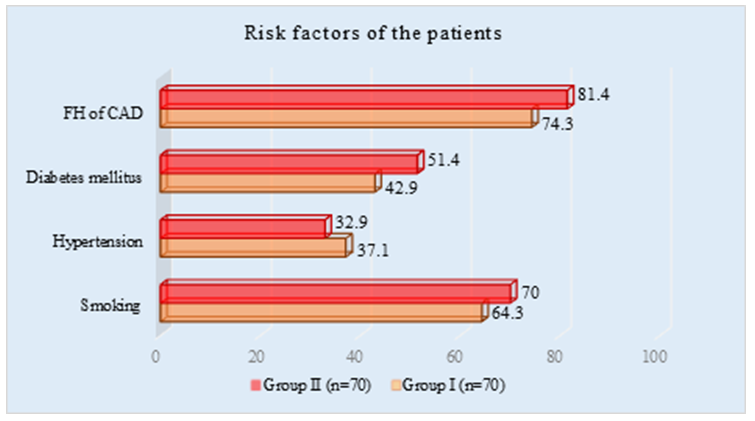
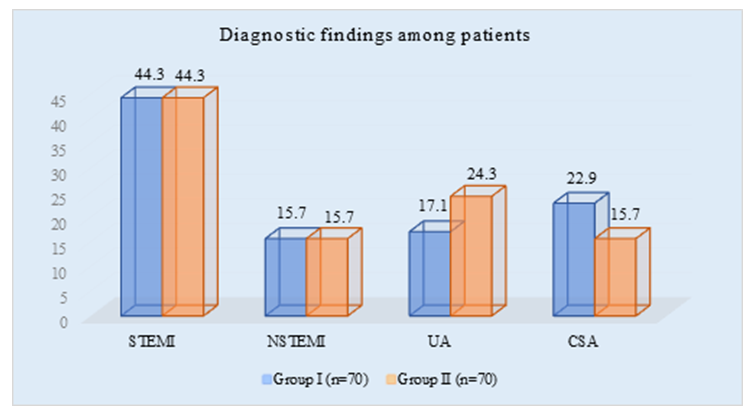
The mean age of the study population was 53.3 ± 6.6 and 53.5 ± 8.7 in groups I and II, respectively (P=0.85). There were no significant differences in the prevalence of smoking history, diagnosed diabetes mellitus, hypertension, and family history of CAD between the two groups (P>0.05). The mean BMI was nearly identical in group I and group II (26.4±1.3 vs. 26.7±1.5 Kg/m2) with a statistically insignificant difference (P=0.16). The mean BMI for the total patient population was 26.6±1.4 Kg/m2. The bar diagram illustrates the sex distribution among the study population, with 87.1% males and 12.9% females in group I, and 90% males and 10% females in group II. There was no statistically significant association in terms of sex between the study groups (P=0.59), and the male-to-female ratio was 8:1, indicating a male predominance in the study. There was no statistically significant association between the study groups by diagnosis. The incidence of UA was higher in group II than in group I (24.3% vs. 17.1%, P=0.30), but it did not reach the level of significance. Conversely, CSA was higher in group I than in group II (22.9% vs. 15.7%, P = 0.28), but it did not reach the level of significance. Procedural and post-procedural characteristics did not show any statistically significant association between the study groups (P>0.05), except for palpation findings. Absent pulse at early (24 hours) was observed more frequently in group II than in group I (11.4% vs. 2.9%, P=0.04)
with a significant association. The same characteristic was also observed more frequently in group II than in group I (8.6% vs. 1.4%, P=0.04) at late (30 days) with a significant association. Radial artery occlusion (RAO) at early (24 hours) was observed more frequently in group II than in group I (12.8% vs. 4.3%, P=0.04) with a significant association. The same characteristic was also observed more frequently in group II than in group I (11.4% vs. 2.8%, P=0.04) at late (30 days) with a significant association. Multivariate logistic regression analysis identified the duration of hemostasis compression time of 6 hours as a strong predictor of RAO (Odds ratio [OR] = 7.149, 95% Confidence Interval [CI] = 1.212-8.868; P=0.01).
Table 1: Age distribution (N=140)
|
Age (Years) |
Group I |
Group II |
P-value |
||
|
(n=70) |
(n=70) |
||||
|
n |
% |
n |
% |
||
|
≤40 Yrs. |
2 |
2.9 |
5 |
7.1 |
|
|
41-50 Yrs. |
22 |
31.4 |
23 |
32.9 |
|
|
51-60 Yrs. |
38 |
54.3 |
31 |
44.3 |
|
|
> 60 Yrs. |
8 |
11.4 |
11 |
15.7 |
|
|
Mean ±SD |
53.3±.6.6 |
53.5±8.7 |
0.85 |
||
Table 2:Cardiovascular risk factors (N=140)
|
Risk Factors |
Group I |
Group II |
P-value |
||
|
(n=70) |
(n=70) |
||||
|
n |
% |
n |
% |
||
|
Smoking |
45 |
64.3 |
49 |
70 |
0.47 |
|
Hypertension |
26 |
37.1 |
23 |
32.9 |
0.6 |
|
Diabetes mellitus |
30 |
42.9 |
36 |
51.4 |
0.31 |
|
FH of CAD |
52 |
74.3 |
57 |
81.4 |
0.31 |
|
BMI (Mean) |
26.4±1.3 |
26.7±1.5 |
0.16 |
||
Table 3: Diagnostic findings (N=140)
|
Diagnosis |
Group I |
Group II |
P-value |
||
|
(n=70) |
(n=70) |
||||
|
n |
% |
n |
% |
||
|
STEMI |
31 |
44.3 |
31 |
44.3 |
1 |
|
NSTEMI |
11 |
15.7 |
11 |
15.7 |
1 |
|
UA |
12 |
17.1 |
17 |
24.3 |
0.3 |
|
CSA |
16 |
22.9 |
11 |
15.7 |
0.28 |
Table 3 showed STEMI: ST-Elevation Myocardial Infarction, NSTEMI: Non-ST-Elevation Myocardial Infarction, UA: Unstable Angina, CSA: Coronary Artery Spasm
Table 4: Procedural and post-procedural characteristics (N=140)
|
Variables |
Group I |
Group II |
P-value |
||
|
(n=70) |
(n=70) |
||||
|
n |
% |
n |
% |
||
|
Sheath size used |
|||||
|
6F |
64 |
91.4 |
65 |
52.9 |
0.75 |
|
5F |
6 |
8.6 |
5 |
7.1 |
0.75 |
|
Types of sheaths used |
|||||
|
New |
26 |
37.1 |
29 |
41.4 |
0.61 |
|
Sterilized |
44 |
62.9 |
41 |
58.6 |
0.61 |
|
Nitroglycerin |
38 |
54.3 |
32 |
45.7 |
0.31 |
|
Number of vessels stented |
|||||
|
1 |
60 |
85.7 |
55 |
78.6 |
0.27 |
|
2 |
10 |
14.3 |
15 |
21.4 |
0.27 |
|
Procedure Time (min) |
|||||
|
Mean ±SD |
53.3±8.2 |
55.1±9.1 |
0.23 |
||
|
Palpation findings |
|||||
|
AP at 24 hrs. |
2 |
2.9 |
8 |
11.4 |
0.04 |
|
AP at 30 days |
1 |
1.4 |
6 |
8.6 |
0.04 |
|
Spasm |
9 |
12.8 |
11 |
15.7 |
0.62 |
|
Hematoma |
2 |
2.9 |
3 |
4.3 |
0.64 |
Table 5: Duplex assessment of RAO (N=140)
|
Assessment |
Group I |
Group II |
P-value |
||
|
(n=70) |
(n=70) |
||||
|
n |
% |
n |
% |
||
|
RAO at 24 hrs. |
3 |
4.3 |
9 |
12.8 |
0.04 |
|
RAO at 30 days |
2 |
2.8 |
8 |
11.4 |
0.04 |
Table 6: Multivariate logistic regression analysis of RAO with confounding factors
|
Variables of interest |
Odds Ratio |
P-value |
|
(OR) |
||
|
Age in years (>55) |
1.034 |
1.118 |
|
Male gender |
0.52 |
0.6 |
|
Smoking |
2.188 |
0.34 |
|
Hypertension |
1.573 |
0.5 |
|
Diabetes mellitus |
1.076 |
0.91 |
|
Increased BMI kg/m2 |
1.479 |
0.09 |
|
Sterilized sheath use |
1.497 |
0.56 |
|
Nitroglycerin use |
1.624 |
0.03 |
|
Procedure time |
1.186 |
0.03 |
|
HC time 6 hours |
7.149 |
0.01 |
4. Discussion
In this study, there was no significant difference in age distribution between the two groups. The mean age of patients in Group I and Group II was 53.3±6.6 and 53.5±8.7 years, respectively, with P=0.85. Similar results were reported by Karimul et al. [13]. Regarding sex distribution, there was no statistically significant difference between the study groups (P=0.59), and male patients predominated (81.6%). A study by Dharma et al. found no significant reduction in the risk of RAO in women patients (Odds ratio, 0.69; 95% confidence interval [CI], 0.38 to 1.26; P=0.147) [14]. History of smoking, diagnosed diabetes mellitus, hypertension, and family history of CAD were similar between the groups with no significant association (P>0.05). The mean BMI in Group I and Group II was nearly identical (26.4±1.3 vs. 26.7±1.5 Kg/m2), with no statistically significant difference (P=0.16). The overall patient BMI was 26.6±1.4 kg/m2, consistent with findings by Karimul et al. [13]. In Group I, 44.3% had STEMI, 15.7% had NSTEMI, 17.1% had UA, and 22.9% had CSA. Group II showed higher UA (24.3% vs. 17.1%, P=0.30) and lower CSA (15.7% vs. 22.9%, P=0.28). Matin et al. reported a similar disease profile [11]. Procedural and post-procedural characteristics showed no statistically significant association between the study groups (P>0.05), except for palpation findings. Absent pulse at early (24 hours) was higher in Group II than Group I (11.4% vs. 2.9%, P=0.04), with a significant association. The same was observed at late (30 days) (8.6% vs. 1.4%, P=0.04) with significant association. Studies using absent radial pulse as the sole criterion for RAO reported immediate rates ranging from 2% to 18% [2]. In certain studies, using Doppler, the reported incidence of RAO tends to be higher than when relying solely on the absence of pulse as a criterion. Huang et al. found that the rate of immediate occlusion was 4.7% using the radial pulse method and 10.7% using the Doppler study [3]. Lopes et al., in a Brazilian study, reported an incidence of early RAO (within 7 days) as 10.5% [15]. In this study, the primary outcome incidence of RAO early (24 hours) after trans-radial PCI, as defined by duplex ultrasound, was significantly lower in the 2-hour hemostatic compression group compared to the 6-hour group (4.3% vs. 12.8%, P=0.04). Late (30-day) RAO was also significantly lower in Group I than in Group II (2.8% vs. 11.4%, P=0.04). Similar findings were reported by Samir B. Pancholy et al., where early RAO occurred in 5.5% of patients with 2-hour compression and 12% with 6-hour compression, with statistically significant differences. Chronic RAO occurred in 3.5% with 2-hour compression and 8.5% with 6-hour compression [12]. The study also indicated that the use of post-procedural nitroglycerin reduced the incidence of RAO (OR=1.624; 95% CI=1.110-11.304; P=0.03). Longer procedure time was significantly associated with the development of RAO (OR=1.186, CI=1.097-1.289; P=0.03). This aligns with findings from Pancholy and Patel (2012) [12] and Rashid et al. (2016) [16], which identified hemostatic compression time as a significant predictor of RAO (P=0.025). In Matin et al.'s study, the incidence of RAO was 9.6% based on Duplex ultrasound [11]. Additionally, Karimul et al. [13] found predictors of RAO to include hemostatic compression time exceeding 2 hours, post-procedural nitroglycerine use, and prolonged procedure time.
Limitation of the Study
This single-center study had a limited sample size and was conducted over a short duration. Consequently, the findings may not accurately represent the overall scenario in the entire country.
5. Conclusion & Recommendation
The critical correlation between hemostatic compression duration and radial artery occlusion following trans-radial intervention underscores the significance of timely and strategic post-procedural care. The findings strongly advocate for a shorter compression duration, as it emerges as a pivotal factor in reducing both early and late occurrences of radial artery occlusion. This not only enhances the overall efficacy of trans-radial interventions but also addresses the imperative need for minimizing associated complications. Healthcare practitioners should consider these results when formulating post-procedural protocols, emphasizing the potential benefits of a nuanced approach to compression duration. As medical practices continue to evolve, optimizing procedural techniques and post-interventional care protocols becomes paramount in ensuring the safety and success of trans-radial interventions.
References
- Rademakers LM & Laarman GJ. Critical hand ischemia after transradial cardiac catheterisation. An uncommon complication of a common procedure. Neth Heart J 20 (2012): 372–375.
- Pancholy SB. Transradial access in an occluded radial artery. New technique. J Invasive Cardiol 19 (2007): 541–544.
- Huang CH, Chen CY, Chen IC. Impact of the transradial approach to coronary angiography or angioplasty on radial artery in Taiwanese population. Acta Cardiol Sin 20 (2004): 212–218.
- Pancholy S, Coppola J, Patel T, et al. Prevention of radial artery occlusion-patent hemostasis evaluation trial (PROPHET study). A randomized comparison of traditional versus patency documented hemostasis after transradial catheterization. Catheter Cardiovasc Interv 72 (2008): 335–340.
- Kerawala CJ & Martin IC. Palmar arch backflow following radial forearm free flap harvest. British J Oral & Maxillofacial Surgery 41 (2003): 157–160.
- Plante S, Cantor W J, Goldman L, et al. Comparison of bivalirudin versus heparin on radial artery occlusion after transradial catheterization. Catheter Cardiovasc Interv 76 (2010): 654–658.
- Tuncez A, Kaya Z, Aras D, et al. Incidence and predictors of radial artery occlusion associated transradial catheterization. Int J Med Sci 10 (2013): 1715–1719.
- Garg N, Madan BK, Khanna R, et al. Incidence and predictors of radial artery occlusion after transradial coronary angioplasty. Doppler-guided follow-up study. J Invasive Cardiol 27 (2015): 106–112.
- Patwary MS, Uddin MJ, Rahman MM, et al. Advantage of Trans Radial Coronary Angiography. A Study of 40 Patients. University Heart J 5 (2010).
- Kabir MS. In-hospital outcome of Transradial PCI compared to Transfemoral PCI in coronary artery disease patient (2013).
- Matin MA. Incidence & predictors of radial artery occlusion of coronary procedure through transrarial approach. A-doppler guided study (2016).
- Pancholy SB and Patel TM. Effect of duration of hemostatic compression on radial artery occlusion after transradial access. Catheter Cardiovasc Interv 79 (2012): 78–81.
- Islam MK, Uddin MJ, A Momen, et al. Role of Intra-arterial Nitroglycerin (Postprocedural, Prehemostasis) to Reduce Radial Artery Occlusion After Transradial Catheterisation: A Doppler-guided Study. Mymensingh Med J 32 (2023): 412-420.
- Dharma S, Kedev S, Patel T, et al. A novel approach to reduce radial artery occlusion after transradial catheterization. Postprocedural/prehemostasis intra-arterial nitroglycerin. Catheter Cardiovasc Interv 85 (2015): 818–825.
- Sá BJLd, Barros LdFT, Brandão SCS, et al. Interferência de introdutores reprocessados na oclusão da artéria radial após cateterismo cardíaco. Revista Brasileira de Cardiologia Invasiva 21 (2013): 270–275.
- Rashid M, Kwok CS, Pancholy S, et al. Radial Artery Occlusion After Transradial Interventions. A Systematic Review and Meta-Analysis. J Am Heart Assoc 5 (2016).