Evaluation of Functional and Radiological Outcome of Late Fixation of Femoral Neck Fracture in Young Adults by Cannulated Lag Screws
Article Information
Dr. Subrata Saha1*, Dr. Md Tayef Mahmud2, Dr. Md. Shadiqur Rahman3, Dr. Dibakar Sarkar4, Dr. Ifthear Irfan5, Dr. Sharmistha Roy6
1Junior Consultant, 100 Bed Upazila Health Complex, Kashiani, Gopalganj, Dhaka, Bangladesh
2Assistant Registrar, Department of Orthopedic Surgery, Chittagong Medical College Hospital, Dhaka, Bangladesh
3Medical Officer, National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, Bangladesh
4Junior Consultant, National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, Bangladesh
5Medical Officer, National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, Bangladesh
6Consultant, Clinical Pathology, Ibn Sina Diagnostic & Consultation Centre, Dhaka, Bangladesh
*Corresponding Author: Dr. Md. Shadiqur Rahman, Medical Officer, National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, Bangladesh.
Received: 24 July 2025; Accepted: 31 July 2025; Published: 07 August 2025
Citation: Subrata Saha, Md Tayef Mahmud, Md. Shadiqur Rahman, Dibakar Sarkar, Ifthear Irfan, Sharmistha Roy. Evaluation of Functional and Radiological Outcome of Late Fixation of Femoral Neck Fracture in Young Adults by Cannulated Lag Screws. Journal of Orthopedics and Sports Medicine. 7 (2025): 397-405
View / Download Pdf Share at FacebookAbstract
Background: Femoral neck fractures are common injuries that affect hip stability, leading to impaired weight-bearing and mobility. It most commonly affects older adults, where replacement arthroplasty is the recommended standard treatment. In contrast, these fractures are relatively rare in younger individuals, accounting for only 2-10% of cases. For this group, early internal fixation is the preferred method to preserve the femoral head and its blood supply. However, bearing all these factors in mind, the present study aims to evaluate the functional and radiological outcomes of delayed fixation for femoral neck fractures in our setting.
Material & Method: The quasi-experimental study was conducted at the National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, from September 2021 to September 2023. The study population included patients with femoral neck fractures who met the inclusion criteria. A total of 40 patients were enrolled. All cases were assessed using clinical features, X-ray, and Harris Hip Score (HHS). Follow-up continued for a minimum of 9 months with clinical, functional, and radiological outcomes recorded.
Results: The mean age was 32.7 ± 9.14 years with male predominance (66.7%). The main cause of injury was a road traffic accident (67%). The most common fracture was Garden type III (46.7%, n = 19). The mean duration of injury to operation was 10.5 ± 2.8 days, and follow-up was 43.3 ± 6.7 weeks. 76.7% of cases achieved radiological union. There were 4 (10%) avascular necrosis (AVN) of the femoral head and 1 (3.3%) wound infection. Non-unions and unsatisfactory functional outcomes were higher in the 3rd week fixation than 2nd week fixation. These were significantly associated (p <.05). Though not significantly associated, the nonunion rate was higher among displaced fractures and patients aged 31-40 years. Finally, 70% of cases had satisfactory (52.5% excellent and 17.5% good) and 30% satisfactory (10% fair and 20% poor) functional outcomes with a mean HHS of 85.25±12.09.
Conclusion: Although delayed fixation is not the preferred approach, it remains a clinically effective option for treating femoral neck fractures in young adults.
Keywords
Late fixation; Young adult; Harris hip score; Cannulated lag screws; Femoral neck fracture
Article Details
1. Introduction
One of the main components of the locomotor system is the hip joint, which functions as a ball-and-socket type of synovial joint. It bears significant stress during walking, running, and other daily activities. Any condition that disrupts the normal biomechanics of this joint can lead to serious complications, including morbidity and even death. Therefore, to maintain appropriate hip function, all of the components associated with this joint should work together. In orthopedic practice, femoral neck fractures (FNF), a subtype of hip fractures, are frequently seen. This type of fracture is challenging to manage because of its high complication rate and ongoing debate about the most effective treatment. As the elderly population grows rapidly worldwide, femoral neck fractures are common in the aging population and appear to be becoming more frequent every day. It is estimated that by 2050, there will be 8.2 million hip fracture cases worldwide, with the age-related incidence rising by 1% annually. More recent studies have shown that femoral neck fractures account for 50% of proximal femur fractures. But fortunately, it is rare among the young population-there are only 2-10% cases below the age of 50 years [1,2]. The frequency of femoral neck fractures varies by region as well. North America and Europe have higher rates than Asia [3]. Female sex, white race, advanced age, low estrogen, low body mass index (<18.5 kg/m2), poor exposure to sunshine, low recreational activity, smoking, and alcohol misuse are some of the many characteristics that enhance the risk of fracture [4,5]. This fracture primarily affects older adults following minimal trauma, such as a fall from a standing height. On the other hand, although rare, these fractures usually occur in young individuals due to high-energy trauma, such as motor vehicle injury, fall from height, sports injury, etc. [5-7]. There is still no clear consensus on the best surgical approach for femoral neck fractures, even recent advancements in both diagnosis and fracture management. The type of surgical intervention depends on the patient's age, fracture pattern, activity level, comorbidities, bone quality, and the surgeon's preferences and practice patterns. Total hip arthroplasty (THA), unipolar arthroplasty, bipolar hemiarthroplasty, and reduction and fixation are among the available options. There are two types of arthroplasties: cemented and uncemented. Only patients who are really sick and unfit for surgery are given consideration for non-operative treatment [8-10]. In individuals younger than 60, the primary aim of treating femoral neck fractures is to preserve the femoral head and restore the patient's normal function. For the internal repair of such fractures, a variety of implants have been used over time, including smooth pins, threaded screws, nails (such as Jewett nails), and sliding/dynamic hip screws (SHS/DHS) with or without a derotation screw. Multiple cancellous screws are a common fixation device because they provide stable fixation for the majority of fracture patterns, a shorter operating time, and involve a relatively minimally invasive approach [7,9,10]. The most crucial factor in preventing avascular necrosis and nonunion is maintaining the blood supply to the femoral head. Therefore, the objective of treatment is to restore blood flow by achieving early anatomical reduction and stable fixation. Stable internal fixation and early anatomical reduction are essential for the successful fixation of femur neck fractures. According to and [11,12], mal-reduction is a powerful predictor of fracture healing problems such as non-union, avascular necrosis (AVN), malunion, reduced functional recovery, and eventual re-operation. The purpose of the present study is to assess the functional and radiological outcomes of delayed fixation of femoral neck fractures using cannulated leg screws in young adults.
2. Material and Method
This research was carried out at the National Institute of Traumatology and Orthopaedic Rehabilitation (NITOR), Dhaka, Bangladesh. A quasi-experimental study was conducted on 40 patients who suffered fractures in the neck and femur in our institute from September 2021 to September 2023. The inclusion criteria included the age of the patient, between 18 and 50 years of age, and the timing of the fracture, between 7 and 21 days. Patients with open fractures, pathological fractures, and polytrauma injuries are excluded from the study. Purposive sampling (non-randomized) was done according to the availability of the patients and strictly considering the inclusion and exclusion criteria. Demographic variables included age (18-50) and gender (male and female). Clinical variables included the side involved, type of fracture, mechanism of injury, interval between injury and operation, and duration of follow-up. Outcome variables included complications like wound complications (superficial and deep wound infection) and fracture fixation complications (non-union and avascular necrosis). After selecting a case according to inclusion and exclusion criteria, patients were evaluated preoperatively. An elaborate history was taken. A general examination and a local examination followed this. After admission, patients were put on surface traction to the affected limb with 1/10th of the patient's body weight. Radiological evaluation was done by taking anteroposterior and lateral X-rays of the affected hip. After that, essential investigations were given to all patients to prepare them for anaesthesia. Any associated illness was controlled with appropriate measures. After optimization of patients, a pre-anesthesia check-up was done. All patients underwent preoperative counselling regarding the operative procedure, probable complications, outcome, and other treatment options, along with their merits and demerits. After being informed, written consent was obtained. Data were collected with a pre-tested structured questionnaire containing history, clinical examination, laboratory investigations, preoperative, perioperative, postoperative complications, and postoperative follow-up findings. A data sheet was formulated to evaluate the outcomes according to HHS. Data were processed using the computer software program Microsoft Excel 2010 and analyzed by SPSS 27.0.1. The data presented on a categorical scale was expressed as frequency and corresponding percentage, while the quantitative data was presented as mean and standard deviation (SD). No data or information was collected without the written consent of the patient. Participation in this research was fully voluntary. The respondents were entirely free to withdraw their participation at any stage or at any time during the study. Written informed consent was obtained from each patient. Before consent, they were informed of the aim and purpose of the research. Confidentiality was assured and maintained.
2.1 Surgical procedures
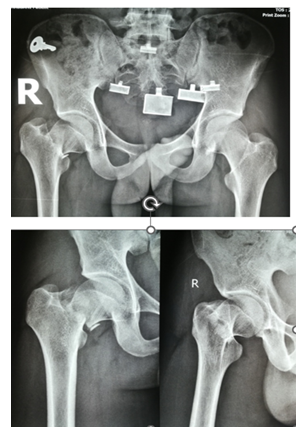
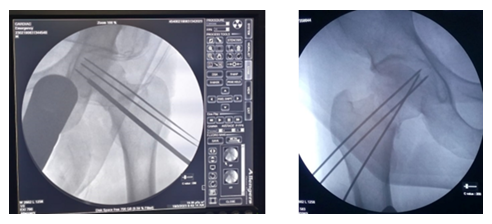
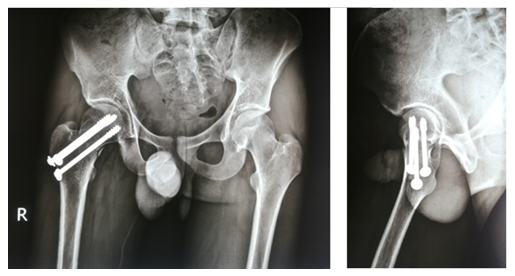
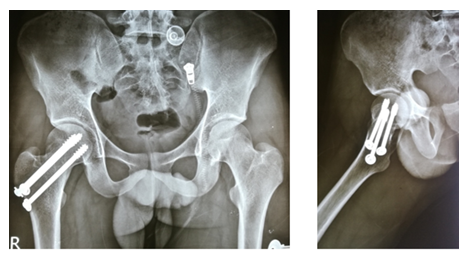
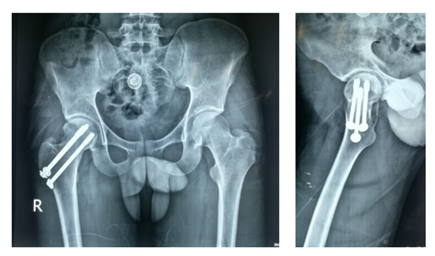
After selecting a case according to inclusion and exclusion criteria, patients were evaluated preoperatively. An elaborate history was taken. This was followed by a general examination and local examination. After admission, patients were put on surface traction to the affected limb with 1/10th of the patient's body weight. All patients underwent preoperative counselling regarding the operative procedure, probable complications, outcome, and other treatment options, along with their merits and demerits. After being informed, written consent was obtained. After preparing the patients for operation, Closed reduction is performed with the patient in the supine position on a fracture table (Figure 1). Reduction was confirmed by C-arm. After reduction, three guide wires are placed, usually in an inverted triangular fashion (Figure 2).
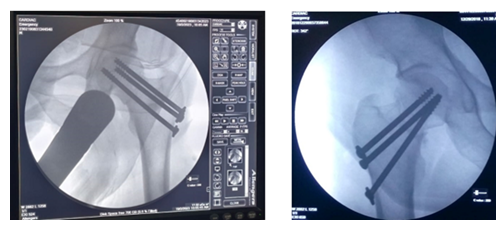
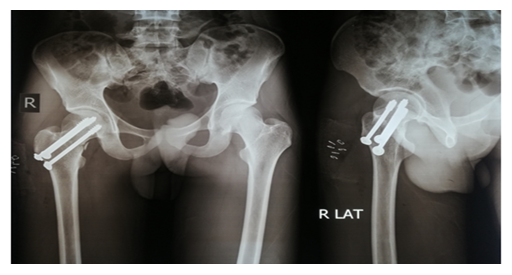
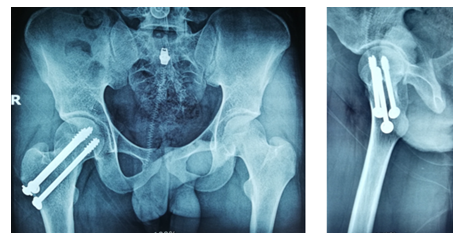
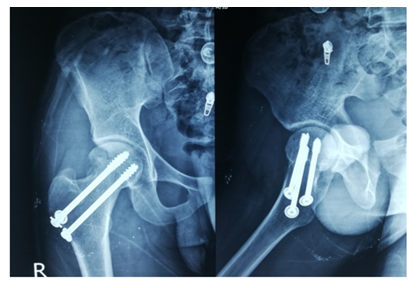
The screw lengths are measured, and drilling is performed using a 4.5 mm cannulated reamer. The screws are then inserted (for the BDSF technique, a specific sequence of middle, then superior, and lastly inferior screw insertion is to be followed). All three screws are inserted less than 5 mm subchondrally (Figure 3,4). In all cases, a prophylactic antibiotic was given. In the postoperative ward, proper fluid and hemodynamic balance were ensured. Change of posture was done twice an hour. The antibiotic was continued for 3 days. Analgesics were given to ensure a pain-free postoperative period. On the first postoperative day, patients were allowed to sit on the side of the bed. Patients were being educated about breathing exercises, isometric quadriceps exercises, gluteal exercises, and ankle pumping exercises. An immediate postoperative X-ray was done (Figure 5). After checking the dressing, on 4th POD, they were discharged from the hospital if their postoperative period was uneventful. Oral antibiotics were given for 10 days. Advice was given to continue isometric quadriceps exercise. Regarding ambulation, they were advised to do non-weight-bearing (of the affected side) crutch ambulation until directed by the physician. Use of elevated toilet seats onwards is also advised. The next follow-up would be given at the 14th POD. The first follow-up was given at 14th POD to check any signs of infection, pain status, and distal neurovascular status. The stitch was removed on the same day. Advice given about isometric quadriceps exercise, active abduction, extension exercise, and stretching exercise of the hip joint. The next follow-up was the 6th week after the operation. The range of motion was tested. An X-ray was done to check callus formation. Improvements were noted. Partial weight bearing was given at this follow-up. Subsequent follow-up was given at 12 weeks and every 4 weeks until union has been achieved or at least 9 months (Figures 6-10).
3. Results
A total of forty patients with femoral neck fractures who met the study's inclusion requirements were chosen. Patients received follow-up care and surgical treatment between September 2021 and September 2023. Every patient received at least 36 weeks of follow-up. The following outcomes were attained in this series. In this study, (Table 1) the highest number of patients, 16 (40%), were in the 21-30 year age group, followed by 11 (26.7%) cases in the 41-50 year age group, 09 (23.3%) in the 31-40 year age group, and the lowest 4 (10%) cases in the < 20-year age group. The mean age was 32.7 ± 9.14 years, with a range from 18 to 50 years. In this study, road traffic accidents accounted for 27 (67%) cases, which was the most common cause of injury. This was followed by falling on the ground and falling from height, which accounted for 9 (23%) and 4 (10%) cases, respectively. The most occurring fracture was Garden type III (46.7%, n = 19), followed by Garden type IV in 9 (23.3%) and Garden type II in 8 (20%) cases. The lowest number of cases (n = 4, 10%) were Garden type I fractures. Undisplaced (i.e., Garden type I and Garden type II) femoral neck fractures constituted 12 (30%) cases, whereas displaced (i.e., Garden type III and Garden type IV) femoral neck fractures constituted 28 (70%) cases. Cases are categorized into 2 groups according to the duration of injury to operation. Out of 40 cases, 33 (83.3%) were operated on in the 2nd week (8-14 days), and 7 (16.7%) were operated on in the 3rd week (15-21 days) of injury. The mean duration of injury to operation was 10.5 ± 2.8 days, ranging from 8 days to 18 days. Table 2 categorizes the total duration of follow-up of the patients into 4 groups. The mean duration of follow-up was 43.3 ± 6.7 weeks, ranging from 36 weeks to 56 weeks. Among the 40 cases, most of them were followed up for 36 to 42 weeks (60%, n = 24). 5 (13.3%) cases were followed up for 43 to 48 weeks, 9 (23.3%) cases were followed up for 49 to 53 weeks, and the rest 1 (3.3%) cases were followed up for 55 to 60 weeks. Radiological outcome is categorized into 2 groups: union and non-union. Among the 40 cases, Table 3 shows 31 cases (76.7%) achieved union radiologically, whereas 9 cases (23.3%) failed to achieve radiological union. (Table 4) shows the complications observed among the study group during their follow-up period. A total of 5 cases (13.3%) developed complications. Among them, 4 (10%) cases developed AVN, and 1 (3.3%) case developed wound infection. Patients are grouped into satisfactory and unsatisfactory outcomes according to the Harris Hip Score at last follow-up. After the last follow-up, the final outcome was assessed with the HHS tool. Out of 40 cases, (Table 5) shows 21 (52.5%) had excellent (90 to 100), 7(17.5%) had good (80 to 89), 8 (20%) had poor (less than 70) and the rest 4 (10%) had fair (70 to 79) score. The cumulative satisfactory outcome (excellent and good) was 70% and the unsatisfactory outcome (fair and poor) was 30%. The mean HHS was 82.5±12.09 at last follow up ranging from 53 to 100.
|
Age (In years) |
Frequency |
Percent |
|
<20 |
4 |
0.1 |
|
21-30 |
16 |
0.4 |
|
31-40 |
9 |
0.233 |
|
41-50 |
11 |
0.267 |
|
Total |
40 |
1 |
|
Mean ± SD |
32.7 ± 9.14 |
Table 1: Distribution of cases according to age (N=40).
In this study, Table 1 shows the highest number of patients, 16 (40%), were 21 to 30-year age group, followed by 11 (26.7%) cases in the 41–to 50-year age group, 09 (23.3%) in the 31 to 40-year age group, and the lowest 4 (10%) cases in < 20-year age group. The mean age was 32.7 ± 9.14 years, with a range from 18 to 50 years.
|
Duration of follow-up (in weeks) |
Frequency |
Percentage |
|
36-42 |
24 |
0.6 |
|
43-48 |
5 |
0.133 |
|
49-54 |
9 |
0.233 |
|
55-60 |
1 |
0.033 |
|
Total |
40 |
1 |
|
Mean ± SD |
43.3 ± 6.7 |
Table 2: Distribution of patients according to duration of follow-up (N=40).
Table 2 categorized the total duration of follow-up of the patients into 4 groups. The mean duration of follow-up was 43.3 ± 6.7 weeks, ranging from 36 weeks to 56 weeks. Among the 40 cases, most of them were followed up for 36 to 42 weeks (60%, n = 24). 5 (13.3%) cases were followed up for 43 to 48 weeks, 9 (23.3%) cases were followed up for 49 to 53 weeks, and the rest 1 (3.3%) cases were followed up for 55 to 60 weeks.
|
Radiology |
Frequency |
Percent |
|
Union |
31 |
76.7 |
|
Non-union |
7 |
23.3 |
|
Total |
30 |
100 |
Table 3: Distribution of cases according to radiological outcome (N=40).
Radiological outcome is categorized into 2 groups: union and non-union. Among the 40 cases, (Table 3) shows 31 cases (76.7%) achieved union radiologically, whereas 9 cases (23.3%) failed to achieve radiological union.
|
Complication |
Frequency |
Percentage |
|
Wound infection |
1 |
0.033 |
|
AVN |
4 |
0.1 |
|
Total |
5 |
0.133 |
Table 4: Distribution of cases according to complications (N=40).
Table 4 shows the complications observed among the study group during their follow-up period. A total of 5 cases (13.3%) developed complications. Among them, 4 (10%) cases developed AVN, and 1 (3.3%) case developed wound infection.
|
Haris Hip Score |
Frequency |
Percent |
|
Satisfactory |
||
|
Excellent (90-100) |
21 |
0.525 |
|
Good (80-89) |
7 |
0.175 |
|
Un-satisfactory |
||
|
Fair (70-79) |
4 |
0.1 |
|
Poor (<70) |
8 |
0.2 |
|
Total |
40 |
1 |
|
Mean ± SD |
85.25±12.09 |
|
Table 5: Distribution of cases according to HHS at last follow-up (N=40).
Patients are grouped into satisfactory and unsatisfactory outcomes according to Harris hip score at last follow-up. After last follow-up, the outcome was assessed with the HHS tool. Out of 40 cases, Table 5 shows 21 (52.5%) had excellent (90 to 100), 7 (17.5%) had good (80 to 89), 8 (20%) had poor (less than 70), and the rest 4 (10%) had fair (70 to 79) score. The cumulative satisfactory outcome (excellent and good) was 70% and unsatisfactory outcome (fair and poor) was 30%. The mean HHS was 85.25±12.09 at last follow up ranging from 53 to 100.
|
Duration of injury to surgery (in days) |
Radiological outcome |
p value |
|
|
Non-union |
Union |
||
|
2nd week (8-14) |
5 (15.2%) |
28 (84.8%) |
0.034 |
|
3rd week (15-21) |
4 (57.1%) |
3 (42.9%) |
|
|
Total |
9 |
31 |
|
Table 6: Association between duration of injury to surgery and radiological outcome of the cases (N=40).
Table 6 shows rates of non-union were higher (57.1%) when fixation was done in the 3rd week in comparison to 2nd week fixation (non-union rate was 15.2%), and this was statistically significant (p value <.05).
|
Duration of injury to surgery (in days) |
Functional outcome |
p value |
|
|
Satisfactory |
Unsatisfactory |
||
|
2nd week (8-14) |
26 (78.8%) |
7 (21.2%) |
0.003 |
|
3rd week (15-21) |
1 (14.3%) |
6 (85.7%) |
|
|
Total |
27 |
13 |
|
Table 7: Association between duration of injury to surgery and Functional outcome of the cases (N=40).
Table 7 shows functional outcome (measured by Harris hip score) at final follow-up showed higher unsatisfactory rate (85.7%) when fixed at 3rd week compared to when fixed at 2nd week (21.2%). Contrary to that higher satisfactory rate was found when fixed at 2nd week (78.8%) compared to when fixed at 3rd week (14.3%). This association was statistically significant (p <.05).
|
Garden class |
Radiological union |
p value |
|
|
Non-union |
Union |
||
|
Undisplaced |
1 (8.3%) |
11 (91.7%) |
0.32 |
|
Displaced |
8 (28.6%) |
15 (71.4%) |
|
|
Total |
9 |
31 |
|
Table 8: Association between fracture type (Garden class) and radiological outcome of the cases (N=40).
Table 8 shows that of the total 40 cases in the study highest percentage of union was achieved among undisplaced fractures (91.7%, 11 out of 12 cases) and among displaced fracture, it was 71.4% (15 out of 23 cases). This association was not statistically significant (p value >.05), but nonunion rate was higher among displaced fractures (28.6%) compared to undisplaced fractures (8.3%).
4. Discussion
Given their high functional demands, maintaining the native hip architecture and mechanics following a femoral neck fracture is a top goal in the treatment of physiologically young patients [8]. Because of its natural route, the femoral head's blood supply is intrinsically susceptible. Despite having several arterial supplies, the femoral head's blood supply is inherently unstable, making it vulnerable to vascular compromise in the event of trauma [13]. There is a considerable range in the reported rates of AVN and nonunion following internal fixation [14]. Some studies claim that the best outcomes come from reducing and fixing femoral neck fractures in young adults as soon as possible. However, some investigations were unable to establish a connection between AVN, nonunion, and the time interval between surgeries [15]. Sixteen (40%) of the patients in this study were in the age range of 21 to 30 years, followed by eleven (26.7%) in the 41-50 year age group, nine (23.3%) in the 31-40 year age group, and the fewest four (10%) in theunder-20 year age group. With a range of 18 to 50 years, the mean age was 32.7 ± 9.14 years. The results were lower than those of Butt et al. [16] (42 years, with a range of 20-55 years) [16], but they were comparable to those of Elmi et al. [15] (34.3 ± 12.5 years). The average age at which neck femur fractures occur is declining, most likely as a result of a rise in high velocity injuries that cause these fractures to occur in younger individuals. In this study, the male-female ratio was 2.1:1, with 27 (67.5%) males and 13 (32.5%) females. This observation is nearly identical to Butt et al.'s [16] finding that the male-to-female ratio was 1.7: 1. The male-to-female ratio ranged from as low as 1.25:1 by Jo et al. [17] and 1.5:1 by Gani et al. [18] to as high as 4:1 by Elmi, et al. [18] and 4.8:1 by Upadhyaya et al. [14], according to the majority of research conducted on younger populations [14,15]. Because they are more prone to osteoporotic fractures, women experience a higher overall incidence of femoral neck fractures. However, the percentage of male cases in the current study was higher than that of female cases because the study cases were younger and motor vehicle accidents were the primary cause of injury. The most frequent cause of injury in this study was traffic accidents, which accounted for 27 (67%) of the cases. Falls from height and falls on the ground were next, accounting for four (10%) and nine (23%) instances, respectively. Therefore, only 23% of cases are caused by trivial or low velocity trauma, while 77% are caused by high velocity trauma. [19] A study found that more RTAs (43%) than falls on the ground (26%). Similarly, [18] discovered more RTAs (55.08%) than minor trauma (19.49%). In their study, [16] discovered that falls from height were more common (74%) than RTA (20%). This data supports the current study because the study patients were younger. The increased incidence of RTA was also amenable for the lower mean age of this study. The current study indicated that the most frequently occurring fracture was Garden type III, accounting for 46.7% (n = 19) of cases, followed by Garden type IV in 23.3% (n = 9) and Garden type II in 20% (n = 8) of cases. The lowest number of cases (n = 4, 10%) were Garden type I fractures. Undisplaced (i.e., Garden type I and Garden type II) femoral neck fractures constituted 12 (30%) cases, whereas displaced (i.e., Garden type III and Garden type IV) femoral neck fractures constituted 28 (70%) cases. Likewise, a result was shown by [17]. In their study, Garden type III fractures were most prevalent (48.9%). Other types were type II (35.6%), type IV (11.1%), and the lowest type I (4.4%). A study by Nizami et al. [20] in Pakistan identified similarities, reporting Garden II, III, and IV fractures at rates of 24%, 48%, and 28%, respectively. They didn’t take any Garden I fracture. Displaced fractures were 74% and undisplaced fractures were 26% in the study by Razik et al. [13], which was similar to this study. But slightly higher undisplaced fractures (41%) were reported by [21]. In this study, out of 40 cases, 33 (83.3%) underwent surgery in the second week (8-14 days) post-injury, while 7 (16.7%) were operated on in the third week (15-21 days) post-injury. The mean duration of injury to operation was 10.5 ± 2.8 days, ranging from 8 days to 18 days. This finding was almost similar to that of mean 8.8 days (range 5-21 days) by Zahid, et al. [6] and mean 8.5 days by Pal et al. [22] and Choubey, but higher than that of Butt et al. [22] (mean 6 days with range 2-9 days) and lower to Wongwai et al. [23], (mean 13 days with range 2-30 days) [6,16,21,22]. Delay of fixation can be due to many reasons, notably delayed presentation of the patients, delayed referral to the competent trauma care center for such fracture management, etc. The average follow-up duration was 43.3 weeks with a standard deviation of 6.7 weeks, spanning from 36 to 56 weeks. Among the 40 cases, most of them were followed up for 36 to 42 weeks (60%, n = 24). 5 (13.3%) cases were followed up for 43 to 48 weeks, 9 (23.3%) cases were followed up for 49 to 53 weeks, and the rest 1 (3.3%) cases were followed up for 55 to 60 weeks. Long-term follow-up was not done. So, the most common complication, like AVN, could not be assessed. Of the 40 cases, 31 (77.5%) demonstrated radiological union, while 9 cases (22.5%) did not achieve radiological union. For delayed fracture fixation after 1 week with acceptable reduction, the rate of non- union was 25% in study by Gumustas et al. [21] This was similar to current study. However, lower incidences of non-union were reported by others, being 16%, 11.5%, and 9%, respectively, by Wongwai et al. [23], Elmi et al. [15], and Butt et al. [16]. Contrary to this study, no nonunion was reported by Pal eta l. [22]. Rates of non-union were higher (57.1%) when fixation was done in the 3rd week in comparison to 2nd week fixation (non-union rate was 15.2%). This was statistically significant (p value <.05). A total of four cases (13.3%) experienced complications. Among them, 3 (10%) cases developed AVN, and 1 (3.3%) case developed wound infection. This finding is more or less similar to the rate of AVN (8.7%) reported by Wongawi, et al. [23] and the 3.8% wound infection reported by Elmi et al. [15] and Pal eta l. [22]. AVN rate was 0% by Razik et al. [13] in patients fixed later than 48 hours by Agar et al. [24]. Long-term follow-up is needed to assess the actual rate of AVN following fixation of the femoral neck, which might be higher than the present follow-up period. The HHS tool was used to evaluate the study's final results following the last follow-up. Eight cases (20%) had bad scores (less than 70), seven cases (16.7%) had good scores (80 to 89), four cases (10%) had fair scores (70 to 79), and twenty-one cases (52.5%) had excellent scores (90 to 100). At the last follow-up, the mean HHS was 85.25±12.09. 30% of results were unsatisfactory, and 70% of results were cumulatively satisfactory. Agar, et al. [24] reported 73.1% satisfactory and 26.9% unsatisfactory results, which was comparable to this [24]. Similarly, Nizami, et al. [20] classified 36% of results as unsatisfactory and 64% as satisfactory [20]. However, Butt et al. [16] found a greater satisfied outcome of 86.6%, while Zahid, et al. [6] reported a higher unsatisfactory outcome of 39.4%. The highest percentage of union was obtained among undisplaced fractures (91.7%, 11 out of 12 cases) and among displaced fractures (71.4%, 15 out of 21 cases) out of the 40 total cases in the research. Although the nonunion rate was higher in the group with displaced fractures (28.6%) than in the group without displacement fractures (8.3%), this link was not statistically significant (p value >.05). Jo, Lee, and Lee found lower rates of non-union in both displaced and undisplaced fractures (18.5% and 0%, respectively), but Karaeminogullari, et al. [11] reported greater rates of non-union in both displaced and undisplaced groups (38% and 18%, respectively) [17]. There are a few limitations to this study. The follow-up period was only 36 weeks. Lack of supervised physiotherapy after discharge from the hospital is, in some cases, another problem affecting the final outcome of the patient. The actual number of AVNs in the femoral head could not be assessed due to the short duration of follow-up.
5. Conclusions
For young adults with femoral neck fractures, early fixation is the preferred course of treatment. However, due to various factors, early intervention is not always possible, which may lead to complications such as nonunion or avascular necrosis. Despite experiencing delayed fixation, it is clear from this study that most patients achieved union at their last follow-up examination. Therefore, while delayed fixation is not ideal, it can still result in successful outcomes and remains a viable treatment option.
Acknowledgements
The authors are grateful to the entire staff of the National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, during the study period.
Conflict of Interest
Authors declare no conflict of Interest.
References
- Filipov O. Epidemiology and Social Burden of the Femoral Neck Fractures. Journal of IMAB -Annual Proceeding (Scientific Papers) 20 (2014): 516-8.
- Bäcker HC, Wu CH, Maniglio M, et al. Epidemiology of proximal femoral fractures . J Clin Orthop Trauma 12 (2021): 161-5.
- Kannus P, Parkkari J, Sievänen H, et al. Epidemiology of hip fractures. Bone 18 (1996): 57-63.
- Melton LJ. Epidemiology of hip fractures: Implications of the exponential increase with age. Bone 18 (1996): 121-5.
- Szymski D, Walter N, Lang S, et al. Incidence and treatment of intracapsular femoral neck fractures in Germany. Arch Orthop Trauma Surg 23 (2022): 2529-37.
- Zahid M, Sabir A Bin, Asif N, et al. Fixation Using Cannulated Screws and Fibular Strut Grafts for Fresh Femoral Neck Fractures with Posterior Comminution. Journal of Orthopaedic Surgery 1 (2012): 191-5.
- Florschutz AV, Langford JR, Haidukewych GJ, et al. Femoral Neck Fractures. J Orthop Trauma 29 (2015): 121-9.
- Pauyo T. Management of femoral neck fractures in the young patient: A critical analysis review. World J Orthop 5 (2014): 204.
- Gupta A, Choudhari P, Nagla A. Management Of Femoral Neck Fractures In Young / Middle Aged Adults. Orthopaedic Journal of M P 24 (2018): 48-60.
- Lowe JA, Crist BD, Bhandari M, et al. Optimal Treatment of Femoral Neck Fractures According to Patient’s Physiologic Age: An Evidence-Based Review. Orthopedic Clinics of North America 41 (2010): 157- 66.
- Karaeminogullari O, Demirors H, Atabek M, et al. Avascular necrosis and nonunion after osteosynthesis of femoral neck fractures: Effect of fracture displacement and time to surgery. Adv Ther 21 (2004): 335-42.
- Papakostidis C, Panagiotopoulos A, Piccioli A, et al. Timing of internal fixation of femoral neck fractures. A systematic review and meta-analysis of the final outcome. Injury 46 (2015): 459-66.
- Razik F, Alexopoulos AS, El-Osta B, et al. Time to internal fixation of femoral neck fractures in patients under sixty years—does this matter in the development of osteonecrosis of femoral head?. Int Orthop 25 (2012): 2127-32.
- Upadhyay A, Jain P, Mishra P, et al. Delayed internal fixation of fractures of the neck of the femur in young adults. J Bone Joint Surg Br 86 (2004): 1035-40.
- Elmi A, Tabrizi A, Rouhani A, et al. Long-Term Follow-Up Results of Delayed Fixation of Femoral Neck Fractures in Adults. Trauma Mon 26 (2013): 8-11.
- Butt MF, Dhar SA, Gani N ul, et al. Delayed fixation of displaced femoral neck fractures in younger adults. Injury 39 (2008): 238-43.
- Jo S, Lee SH, Lee HJ. The Correlation between the Fracture Types and the Complications after Internal Fixation of the Femoral Neck Fractures. Hip Pelvis 28 (2016): 35.
- Gani N, Ganai MA, Baba BA, et al. Observations on AVN Development in Patients of Fracture Neck of Femur Treated with Delayed Fixation. International Journal of Contemporary Medical Research IJCMR 6 (2019).
- Pei F, Zhao R, Li F, et al. Osteonecrosis of femoral head in young patients with femoral neck fracture: a retrospective study of 250 patients followed for average of 7.5 years. J Orthop Surg Res 29 (2020): 238.
- Nizami MA, Ahmed F, Shah MA, et al. Fracture neck of femur treated with cannulated screws in middle aged patients. Journal of Pakistan Orthopaedic Association 21 (2009): 45-51.
- Gumustas S, Tosun HB, Isyar M, et al. Femur neck fracture in young adults, is it really an urgent surgery indication: retrospective clinical study. Pan African Medical Journal (2018).
- Pal U, Choubey R. Results of Delayed Fixation of Displaced Femoral Neck Fractures In Adults: A Retrospective Clinical Study. J Evol Med Dent Sci 4 (2015): 9883-8.
- Wongwai T, Wajanavisit W, Woratanarat P. Non-union and avascular necrosis of delayed reduction and screw fixation in displaced femoral neck fracture in young adults. Journal of the Medical Association of Thailand 95 (2012): 120-7.
- Agar A, Utkan A. The Effect of Anatomical Reduction on Functional Outcomes in Femoral Neck Fracture: A Novel Modified Garden Index. Cureus 24 (2021).