Etiology and Outcome of Tuberculosis among Paediatric Patients in a Specialized Paediatric Hospital
Article Information
Md. Atiqul Islam1*, Mohammed Jafor Iqbal2, Tanusree Sen3, Sonia Saif4, Mizanur Rahman5
1Professor, Department of Paediatric Infectious Diseases and Community Paediatrics, Bangladesh Shishu Hospital & Institute, Dhaka, Bangladesh
2Junior Consultant, Department of Paediatric Infectious Diseases and Community Paediatrics, Bangladesh Shishu Hospital & Institute, Dhaka, Bangladesh
3Registrar, Department of Paediatric Infectious Diseases and Community Paediatrics, Bangladesh Shishu Hospital & Institute, Dhaka, Bangladesh
4Department of Internal Medicine, Sheikh Fazilatunnesa Mujib Memorial KPJ Specialised Hospital and Nursing College, Gazipur, Bangladesh
5Senior Consultant, Department of Pediatrics, 250 Bed Sadar Hospital, Shariatpur, Bangladesh
*Corresponding Author: Dr. Md. Atiqul Islam, Professor, Department of Paediatric Infectious Diseases and Community Paediatrics, Bangladesh Shishu Hospital & Institute, Dhaka, Bangladesh.
Received: 27 November 2024; Accepted: 11 August 2025; Published: 05 September 2025
Citation: Md. Atiqul Islam, Mohammed Jafor Iqbal, Tanusree Sen. Etiology and Outcome of Tuberculosis among Paediatric Patients in a Specialized Paediatric Hospital. Journal of Paediatrics, Perinatology and Child Health. 9 (2025): 154-160.
View / Download Pdf Share at FacebookAbstract
Introduction: Tuberculosis (TB) remains a significant public health challenge, particularly in children, where its presentation can vary from pulmonary to extra-pulmonary forms. This study aims to explore the clinical spectrum of TB in children, including the distribution of types, diagnostic methods, and treatment outcomes.
Methods: This cross-sectional study was conducted at the Department of Paediatric Infectious Diseases and Community Paediatrics in Bangladesh Shishu (Children) Hospital and Institute during the period from January 2022 to January 2023. A total of 100 Paediatric patients diagnosed with tuberculosis were selected as study subjects. Data were entered into Microsoft Excel and analysed using SPSS software. Descriptive statistics were used to summarize the findings, with frequencies and percentages reported for categorical data. Chi-square tests were applied to determine the association between variables like type of tuberculosis, diagnostic findings, treatment regimen, and outcomes. Statistical significance was set at a p-value <0.05.
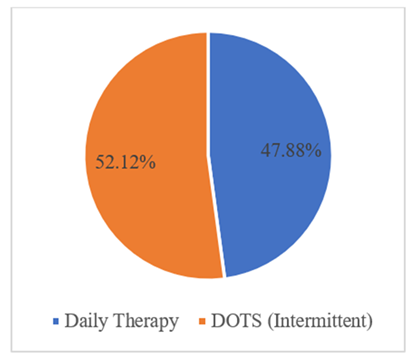
Result: The study included 100 children with tuberculosis, showing a slight male predominance (60%). Pulmonary tuberculosis was the most common form (40%), followed by CNS tuberculosis (20%). Extra-pulmonary tuberculosis accounted for 60% of cases, with a variety of presentations including abdominal and lymphadenitis forms. The tuberculin skin test was positive in 64% of cases, with pulmonary TB having the highest positivity rate (75%). DOTS (intermittent therapy) was used in 52.1% of patients, while 47.8% received daily therapy. Overall, 5.6% of patients left against medical advice, and 4.2% expired. CNS tuberculosis had the highest mortality rate.
Conclusion: This study highlights the diverse clinical presentations and diagnostic challenges of tuberculosis in children, particularly the significant burden of extra-pulmonary TB. Pulmonary TB was the most common form, but extra-pulmonary TB accounted for the majority of cases, often with normal chest X-rays and low AFB positivity. The tuberculin skin test proved useful, but comprehensive diagnosis requires clinical, radiological, and molecular methods. Treatment outcomes were generally favorable, though CNS TB had higher mortality.
Keywords
Tuberculosis; DOTS; AFB; Chest X-ray; Paediatric infectious diseases; Global health; Children
Tuberculosis articles; DOTS articles; AFB articles; Chest X-ray articles; Paediatric infectious diseases articles; Global health articles; Children articles
Article Details
1. Introduction
Tuberculosis (TB) remains a significant global health challenge, particularly in low- and middle-income countries, where both the prevalence and mortality rates are highest. Children are particularly vulnerable to TB due to their immature immune systems, the increased likelihood of rapid progression to severe disease, and the difficulty in diagnosing TB in this population. In 2021, an estimated 1.1 million children developed TB globally, with about 230,000 children succumbing to the disease, underscoring the urgent need for effective interventions and research in this field [1]. The etiology of tuberculosis in paediatric patients is multifactorial, with factors such as malnutrition, HIV co-infection, close contact with TB-infected adults, and poor socio-economic conditions playing a pivotal role [2]. Rural areas, in particular, face unique challenges that exacerbate the spread of TB among children. These challenges include limited access to healthcare services, inadequate TB awareness and education, poverty, and malnutrition [3]. TB in children is primarily a consequence of exposure to an infectious adult, often within the household. The risk of transmission is particularly high in close-contact environments, and children living in households with TB patients are at greater risk of infection [4]. However, due to the paucibacillary nature of TB in children, they are less likely to transmit the disease, making paediatric TB cases often underreported and neglected in TB control programs [5]. In rural settings, the burden of paediatric TB is often compounded by several risk factors. Studies have shown that malnourished children are more likely to progress from latent TB infection to active TB disease [6]. Diagnosing TB in children is notoriously difficult, particularly in resource-limited rural settings. Unlike adults, who often present with the classic symptoms of cough, fever, and weight loss, children with TB may have non-specific symptoms, such as failure to thrive, recurrent respiratory infections, or prolonged fever, which can easily be mistaken for other common paediatric illnesses [7]. Moreover, obtaining sputum samples from young children for microbiological confirmation is often challenging. As a result, paediatric TB is often diagnosed based on clinical symptoms, radiographic findings, and history of contact with an infectious adult, which may lead to underdiagnosis or misdiagnosis [8]. The treatment of paediatric TB follows the same principles as in adults, with a combination of first-line anti-tubercular drugs used for six months or longer, depending on the severity of the disease [9]. However, in rural settings, treatment adherence is a significant challenge. In rural settings, outcomes are generally worse due to delayed diagnosis, inadequate treatment adherence, and the presence of multiple co-morbidities. Studies have shown that children in rural areas are more likely to present with advanced disease and are at a higher risk of treatment failure or death compared to their urban counterparts [10]. Additionally, social factors such as stigma, lack of TB awareness, and reliance on traditional healers may delay healthcare-seeking behavior, further contributing to poor outcomes [3]. This study aims to explore the clinical spectrum of TB in children, including the distribution of types, diagnostic methods, and treatment outcomes.
2. Methods
This cross-sectional study was conducted at the Department of paediatric Infectious Diseases and Community paediatrics in Bangladesh Shishu (Children) Hospital and Institute during the period from January 2022 to January 2023. A total of 100 paediatric patients diagnosed with tuberculosis were selected based on clinical presentation, diagnostic confirmation, and fulfilment of inclusion criteria, which required a confirmed diagnosis of tuberculosis either through clinical, radiological, microbiological, or histopathological findings. Detailed demographic, clinical, and laboratory data were collected for each patient. Information such as age, sex, presenting symptoms, type of tuberculosis (pulmonary or extra-pulmonary), tuberculin skin test (TST) results, chest X-ray findings, sputum/gastric lavage acid-fast bacilli (AFB) results, and contact history were recorded. Nutritional status was assessed based on standard paediatric growth charts, and BCG vaccination status was documented through patient records or immunization cards. The main variables studied included the type of tuberculosis (pulmonary and extra-pulmonary), age and sex distribution, diagnostic findings (TST, AFB, chest X-ray), treatment regimens (daily or DOTS-based intermittent therapy), and treatment outcomes (cured, discharged against medical advice (DAMA), or deceased). The nutritional status and its association with TST outcomes were also analyzed. Tuberculin skin testing (TST) was performed on all children using the Mantoux method, and chest X-rays were taken to evaluate pulmonary involvement. Sputum or gastric lavage samples were subjected to AFB examination where possible. Additional diagnostic tools, such as imaging studies and histopathological examinations, were used for extra-pulmonary TB cases. Data were entered into Microsoft Excel and analyzed using SPSS software. Descriptive statistics were used to summarize the findings, with frequencies and percentages reported for categorical data. Chi-square tests were applied to determine the association between variables like type of tuberculosis, diagnostic findings, treatment regimen, and outcomes. Statistical significance was set at a p-value <0.05. Ethical approval was obtained from the Institutional Ethics Committee. Informed consent was taken from the guardians of all patients before data collection. Data confidentiality was maintained throughout the study.
2.1 Inclusion criteria
- • Children aged 0-18 years with a confirmed diagnosis of tuberculosis.
- • Patients are diagnosed based on clinical, radiological, microbiological, or histopathological evidence.
- • Patients with complete medical records and follow-up data.
2.3 Exclusion criteria
- • Children with a prior history of anti-tuberculosis treatment (ATT).
- • Incomplete or missing medical records.
- • Children with co-existing severe chronic illnesses that could interfere with the study outcome.
3. Results
|
Sex |
Frequency |
% |
|
Male |
60 |
60.0 |
|
Female |
40 |
40.0 |
|
Total |
100 |
100.0 |
Table 1: Distribution of children according to sex (N=100).
The study population consisted of 60 males (60%) and 40 females (40%), indicating a male predominance with a ratio of 1.5:1 (Table 1,2).
|
Age Group (years) |
Male n |
Male % |
Female n |
Female % |
Total |
Total % |
|
<6 |
20 |
33.3 |
15 |
37.5 |
35 |
35.0 |
|
6-10 |
25 |
41.7 |
10 |
25.0 |
35 |
35.0 |
|
>10 |
15 |
25.0 |
15 |
37.5 |
30 |
30.0 |
|
Total |
60 |
60.0 |
40 |
40.0 |
100 |
100.0 |
Table 2: Distribution of children according to age (N=100).
Most patients were under 6 years (35%), with a significant portion also in the 6–10-year age group (35%). There was male predominance in the older age categories (Table 3).
|
Final Diagnosis |
Frequency |
% |
|
Pulmonary Koch's |
40 |
40.0 |
|
CNS Tuberculosis |
20 |
20.0 |
|
Abdominal Koch’s |
15 |
15.0 |
|
TB Lymphadenitis |
10 |
10.0 |
|
Skin Tuberculosis |
5 |
5.0 |
|
Disseminated Koch's |
3 |
3.0 |
|
Miliary TB |
3 |
3.0 |
|
Psoas Abscess |
4 |
4.0 |
|
Total |
100 |
100.0 |
Table 3: Spectrum of type of tuberculosis (N=100).
Pulmonary tuberculosis was the most common diagnosis (40%), followed by CNS tuberculosis (20%). Extra-pulmonary forms accounted for 60% of cases (Table 4).
|
Final Diagnosis |
<6 years |
6-10 years |
>10 years |
Total |
|
Pulmonary Koch's |
15 |
10 |
15 |
40 |
|
CNS Tuberculosis |
5 |
8 |
7 |
20 |
|
Abdominal Koch's |
1 |
6 |
8 |
15 |
|
TB Lymphadenitis |
3 |
3 |
4 |
10 |
|
Skin Tuberculosis |
1 |
1 |
3 |
5 |
|
Disseminated Koch's |
0 |
1 |
2 |
3 |
|
Miliary TB |
0 |
1 |
2 |
3 |
|
Psoas Abscess |
0 |
0 |
4 |
4 |
|
Total |
25 |
30 |
45 |
100 |
Table 4: Spectrum of type of tuberculosis and age-wise distribution (N=100).
The distribution of tuberculosis types varied by age, with pulmonary cases peaking in those over 10 years, while abdominal and CNS tuberculosis were more common in younger age groups (Table 5).
Table 5: Presenting symptoms of children diagnosed with tuberculosis (N=100).
Common presenting symptoms included cough (51%) and fever (67%), with altered sensorium prevalent in CNS cases. The swelling was noted in TB lymphadenitis (Table 6).
|
Final Diagnosis |
TST Positive |
TST Negative |
Total |
|
Pulmonary Koch's |
30 |
10 |
40 |
|
CNS Tuberculosis |
12 |
8 |
20 |
|
Abdominal Koch's |
11 |
4 |
15 |
|
TB Lymphadenitis |
8 |
2 |
10 |
|
Skin Tuberculosis |
2 |
0 |
5 |
|
Disseminated Koch's |
0 |
3 |
3 |
|
Miliary TB |
0 |
3 |
3 |
|
Psoas Abscess |
1 |
0 |
1 |
|
Total |
64 |
30 |
100 |
Table 6: Distribution of TB cases according to tuberculin skin test results (N=100).
The tuberculin skin test (TST) was positive in 64% of patients. Pulmonary tuberculosis had the highest positivity rate (75%) (Table 7).
|
Final Diagnosis |
X-ray Positive |
X-ray Normal |
Total |
|
Pulmonary Koch's |
40 |
0 |
40 |
|
CNS Tuberculosis |
2 |
18 |
20 |
|
Abdominal Koch's |
2 |
13 |
15 |
|
TB Lymphadenitis |
0 |
10 |
10 |
|
Skin Tuberculosis |
1 |
1 |
5 |
|
Disseminated Koch's |
0 |
3 |
3 |
|
Miliary TB |
1 |
2 |
3 |
|
Psoas Abscess |
0 |
1 |
1 |
|
Total |
46 |
47 |
100 |
Table 7: Association of type of tuberculosis against chest X-ray findings (N=100).
Chest X-ray was positive in 46% of patients, with all pulmonary cases showing abnormalities. Extra-pulmonary tuberculosis often presents normal X-rays (Table 8).
|
Final Diagnosis |
AFB Positive |
AFB Negative |
Total |
|
Pulmonary Koch's |
4 |
36 |
40 |
|
CNS Tuberculosis |
0 |
20 |
20 |
|
Abdominal Koch's |
0 |
15 |
15 |
|
TB Lymphadenitis |
0 |
10 |
10 |
|
Skin Tuberculosis |
0 |
5 |
5 |
|
Disseminated Koch's |
0 |
3 |
3 |
|
Miliary TB |
0 |
3 |
3 |
|
Psoas Abscess |
0 |
1 |
1 |
|
Total |
4 |
93 |
100 |
Table 8: Association of type of tuberculosis against sputum/gastric lavage AFB examination (N=100).
AFB examination confirmed pulmonary tuberculosis in only 4% of cases, illustrating the limitations of this test in extra-pulmonary forms (Table 9).
|
Final Diagnosis |
Contact History |
|
|
Present |
Absent |
|
|
Pulmonary Koch's |
8 (28.6%) |
20 (71.4%) |
|
CNS Tuberculosis |
4 (23.5%) |
13 (76.5%) |
|
Abdominal Koch's |
1 (9.1%) |
10 (90.9%) |
|
TB Lymphadenitis |
1 (10.0%) |
9 (90.0%) |
|
Skin Tuberculosis |
0 (0.0%) |
2 (100.0%) |
|
Disseminated Koch's |
1 (100.0%) |
0 (0.0%) |
|
Miliary TB |
0 (0.0%) |
1 (100.0%) |
|
Psoas Abscess |
0 (0.0%) |
1 (100.0%) |
|
Total |
15 (15.0%) |
56 (85.0%) |
Table 9: Association of type of tuberculosis with contact history (N=100).
Among the 71 cases of tuberculosis, contact history was present in 15% of patients. Pulmonary Koch’s had the highest prevalence of contact history (28.6%) (Table 10).
|
Final Diagnosis |
BCG Vaccination |
|
|
Absent |
Present |
|
|
Pulmonary Koch's |
6 (21.4%) |
22 (78.6%) |
|
CNS Tuberculosis |
12 (70.6%) |
5 (29.4%) |
|
Abdominal Koch's |
5 (45.5%) |
6 (54.5%) |
|
TB Lymphadenitis |
2 (20.0%) |
8 (80.0%) |
|
Skin Tuberculosis |
1 (50.0%) |
1 (50.0%) |
|
Disseminated Koch's |
1 (100.0%) |
0 (0.0%) |
|
Miliary TB |
1 (100.0%) |
0 (0.0%) |
|
Psoas Abscess |
0 (0.0%) |
1 (100.0%) |
|
Total |
28 (39.4%) |
43 (60.6%) |
Table 10: BCG vaccination status in TB patients (N=100).
Of the 71 tuberculosis patients, 39.4% were not vaccinated with BCG. Pulmonary Koch’s had the highest vaccination rate (78.6%) (Table 11).
|
Nutritional Status |
TST Outcome |
|
|
Positive |
Negative |
|
|
Malnourished |
34 (65.4%) |
18 (34.6%) |
|
Normal |
15 (78.9%) |
4 (21.1%) |
|
Total |
49 (69.0%) |
22 (31.0%) |
Table 11: Association of TST outcome with nutritional status (N=100).
Among the 71 patients, 69.0% tested positive for TST. Malnourished individuals showed a higher positivity rate (65.4%) compared to those with normal nutrition (Figure 1).
Of the 71 patients, 47.8% received daily therapy, while 52.1% were treated with DOTS (intermittent) (Table 12).
|
Final Diagnosis |
Treatment Type |
|
|
Daily |
Intermittent (DOTS) |
|
|
Pulmonary Koch's |
11 (39.3%) |
17 (60.7%) |
|
CNS Tuberculosis |
13 (76.5%) |
4 (23.5%) |
|
Abdominal Koch's |
4 (36.4%) |
7 (63.6%) |
|
TB Lymphadenitis |
5 (50.0%) |
5 (50.0%) |
|
Skin Tuberculosis |
0 (0.0%) |
2 (100.0%) |
|
Disseminated Koch's |
1 (100.0%) |
0 (0.0%) |
|
Miliary TB |
0 (0.0%) |
1 (100.0%) |
|
Psoas Abscess |
0 (0.0%) |
1 (100.0%) |
|
Total |
34 (47.9%) |
37 (52.1%) |
Table 12: Distribution of different types of tuberculosis and their treatment (N=100).
The majority of patients received treatment through DOTS (52.1%), with CNS tuberculosis patients having the highest percentage on daily therapy (76.5%) (Table 13).
|
Treatment |
Outcome |
|
|
DAMA* |
EXPIRED |
|
|
Daily |
3 (8.8%) |
2 (5.9%) |
|
Intermittent |
1 (2.7%) |
1 (2.7%) |
|
Total |
4 (5.6%) |
3 (4.2%) |
*DAMA: Discharge Against Medical Advice.
Table 13: Association of treatment outcome with the type of treatment (N=100).
In patients receiving daily therapy, 8.8% left against medical advice (DAMA) and 5.9% expired, while for those on intermittent therapy, 2.7% experienced both outcomes. Overall, 5.6% of all patients left against medical advice, and 4.2% expired, with slightly higher DAMA rates in the daily therapy group (Table 14).
|
Final Diagnosis |
Outcome |
|
|
DAMA |
EXPIRED |
|
|
Pulmonary Koch's |
0 (0.0%) |
0 (0.0%) |
|
CNS Tuberculosis |
2 (11.8%) |
3 (17.6%) |
|
Abdominal Koch's |
2 (18.2%) |
0 (0.0%) |
|
TB Lymphadenitis |
0 (0.0%) |
0 (0.0%) |
|
Skin Tuberculosis |
0 (0.0%) |
0 (0.0%) |
|
Disseminated Koch's |
0 (0.0%) |
0 (0.0%) |
|
Miliary TB |
0 (0.0%) |
0 (0.0%) |
|
Psoas Abscess |
0 (0.0%) |
0 (0.0%) |
|
Total |
4 (5.6%) |
3 (4.2%) |
Table 14: Association of treatment outcome with the type of tuberculosis (N=100).
The overall cure rate was 61.9% among patients. Pulmonary Koch’s had the highest cure rate (75.0%), while CNS tuberculosis had a significant proportion of treatment failures (23.5%).
4. Discussion
The study revealed a male predominance in tuberculosis cases, with a male-to-female ratio of 1.5:1 (60% males vs. 40% females). This finding aligns with previous studies which have shown a higher prevalence of tuberculosis in males compared to females, possibly due to biological and environmental factors that make males more susceptible to infection and disease progression [7]. Most children in this study were under the age of 6 years (35%), with an equal percentage (35%) in the 6-10 year age group. This reflects the vulnerability of younger children to tuberculosis, which is in line with prior research showing that tuberculosis tends to affect younger populations due to their immature immune systems [4]. Pulmonary tuberculosis was the most common type of TB diagnosed, accounting for 40% of cases. CNS tuberculosis was the next most prevalent (20%), followed by abdominal TB (15%). This pattern is consistent with global data, where pulmonary tuberculosis remains the most frequently diagnosed form in children. However, extra-pulmonary tuberculosis was found in 60% of cases in this study, reflecting the high burden of non-pulmonary TB in paediatric populations [11]. Fever (67%) and cough (51%) were the most common presenting symptoms. Altered sensorium was prevalent in CNS tuberculosis cases (20%). Similar findings were reported by Marais et al. [2], who observed that fever and cough are typically the earliest and most common symptoms in paediatric tuberculosis, particularly in pulmonary cases. The tuberculin skin test was positive in 64% of the cases, with pulmonary TB having the highest positivity rate (75%). This is consistent with studies that indicate higher TST positivity in pulmonary TB compared to extra-pulmonary forms, where TST sensitivity can be lower [12]. Despite its limitations, TST remains a useful diagnostic tool in paediatric populations, particularly when supported by other diagnostic methods. AFB smear positivity was low, with only 4% of cases testing positive, all of which were pulmonary TB cases. This reinforces the well-known limitation of AFB examination in diagnosing TB, particularly in extra-pulmonary forms, as seen in several other studies [3]. Only 15% of cases had a history of contact with TB patients, and 39.4% were not vaccinated with BCG. The low rate of contact history is consistent with the difficulty in tracing transmission in children, who are often infected through casual household contact [13]. The protective role of the BCG vaccine remains a topic of debate; however, this study found that 60.6% of the cases had been vaccinated, and pulmonary TB cases had the highest vaccination rates (78.6%). This suggests that while BCG vaccination may reduce the risk of severe TB forms, it does not completely prevent infection [14]. In terms of treatment, 52.1% of patients received DOTS (Directly Observed Treatment, Short-course), while 47.8% were on daily therapy. DOTS remains the preferred treatment for managing paediatric TB, especially in resource-limited settings, as it ensures treatment adherence and minimizes the risk of drug resistance [15]. Regarding outcomes, the overall cure rate was 61.9%, with pulmonary TB cases showing the highest cure rates (75%). CNS tuberculosis had the highest mortality (17.6%) and a significant number of patients leaving against medical advice (DAMA). This mirrors findings from other studies that indicate CNS TB has a poorer prognosis due to its invasive nature and delayed diagnosis [16].
5. Limitations of the Study
The study was conducted in a single hospital with a small sample size. So, the results may not represent the whole community.
6. Conclusion
This study highlights the diverse clinical presentations and diagnostic challenges of tuberculosis in children, particularly the significant burden of extra-pulmonary TB. Pulmonary TB was the most common form, but extra-pulmonary TB accounted for the majority of cases, often with normal chest X-rays and low AFB positivity. The tuberculin skin test proved useful, but comprehensive diagnosis requires clinical, radiological, and molecular methods. Treatment outcomes were generally favorable, though CNS TB had higher mortality.
7. Recommendation
It is recommended that healthcare providers maintain a high index of suspicion for extra-pulmonary tuberculosis in children, especially when typical pulmonary symptoms or chest X-ray findings are absent. Early use of diagnostic tools such as the tuberculin skin test, combined with imaging and molecular diagnostics, can enhance detection. Strengthening BCG vaccination coverage, ensuring adherence to treatment protocols like DOTS, and providing additional support for patients with CNS tuberculosis can help improve outcomes and reduce mortality rates.
Funding: No funding sources
Conflict of interest: None declared.
References
- World Health Organization. Global tuberculosis report 2021: supplementary material. World Health Organization (2022).
- Marais BJ, Gie RP, Schaaf HS, et al. The natural history of childhood intra-thoracic tuberculosis: a critical review of literature from the pre-chemotherapy era. The International Journal of Tuberculosis and Lung Disease 8 (2004): 392-402.
- Seddon JA, Shingadia D. Epidemiology and disease burden of tuberculosis in children: a global perspective. Infection and drug resistance 18 (2014): 153-65.
- Newton SM, Brent AJ, Anderson S, et al. Paediatric tuberculosis. The Lancet infectious diseases 8 (2008): 498-510.
- Jenkins HE, Yuen CM. The burden of multidrug-resistant tuberculosis in children. The International Journal of Tuberculosis and Lung Disease 22 (2018): S3-6.
- Laghari M, Sulaiman SA, Khan AH, et al. A prospective study of sociodemographic, clinical characteristics and treatment outcomes of children with tuberculosis in Sindh, Pakistan. BMC Infectious Diseases 19 (2019): 1-1.
- Swaminathan S, Rekha B. Pediatric tuberculosis: global overview and challenges. Clinical Infectious Diseases 50 (2010): S184-94.
- Zar HJ, Workman LJ, Prins M, et al. Tuberculosis diagnosis in children using Xpert Ultra on different respiratory specimens. American journal of respiratory and critical care medicine 200 (2019): 1531-8.
- World Health Organization. Guidance for national tuberculosis programs on the management of tuberculosis in children. World Health Organization (2014).
- Harries AD, Hargreaves NJ, Graham SM, et al. Childhood tuberculosis in Malawi: nationwide case-finding and treatment outcomes. The International Journal of Tuberculosis and Lung Disease 6 (2002): 424-31.
- Golden MP, Vikram HR. Extrapulmonary tuberculosis: an overview. American family physician 72 (2005): 1761-8.
- Shingadia D, Novelli V. Diagnosis and treatment of tuberculosis in children. The Lancet Infectious Diseases 3 (2003): 624-32.
- Sharma SK, Mohan A, Kohli M. Extrapulmonary tuberculosis. Expert Review of Respiratory Medicine 15 (2021): 931-48.
- Zwerling A, Behr MA, Verma A, et al. The BCG World Atlas: a database of global BCG vaccination policies and practices. PLoS Medicine 8 (2011): e1001012.
- Nahid P, Dorman SE, Alipanah N, et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America clinical practice guidelines: treatment of drug-susceptible tuberculosis. Clinical Infectious Diseases 63 (2016): e147-95.
- Rock RB, Olin M, Baker CA, et al. Central nervous system tuberculosis: pathogenesis and clinical aspects. Clinical Microbiology Reviews 21 (2008): 243-61.
Journals List
© 2016-2026, Copyrights Fortune Journals. All Rights Reserved