Epileptogenic Temporal lobe Intrinsic Epidermoid Tumor: A Rare Case Report and Review of the Literature
Article Information
Mohammad Sujan Sharif1*, Tarikul Islam K M2, Abdur Rahman3, Abu Bakar Siddik4, Masum Rahman5*
1Department of Neurosurgery, Dhaka Medical College and Hospital, Dhaka, Bangladesh
2Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
3Department of Medicine, Life and Care Hospital Ltd, Dhaka, Bangladesh
4Department of Pain Medicine, Mayo Clinic, Florida, USA
5Department of Neurological Surgery, Mayo Clinic, MN, USA
*Corresponding Author: Mohammad Sujan Sharif, Department of Neurosurgery, Dhaka Medical College and Hospital, Dhaka, Bangladesh
Masum Rahman, Department of Neurological surgery, Mayo Clinic, Rochester, MN-55905, USA
Received: 19 July 2021; Accepted: 02 August 2021; Published: 14 August 2021
Citation: Mohammad Sujan Sharif, Tarikul Islam KM, Abdur Rahman, Abu Bakar Siddik, Masum Rahman. Epileptogenic Temporal lobe Intrinsic Epidermoid Tumor: A Rare Case Report and Review of the Literature. Journal of Cancer Science and Clinical Therapeutics 5 (2021): 382-388.
View / Download Pdf Share at FacebookAbstract
Intracerebral epidermoid cysts are uncommon, accounting for only around 1.5 percent of intracranial tumors. Among these, Temporal lobe intracerebral epidermoid tumors are exceedingly rare. The great majority of these slow-growing tumors are asymptomatic, whereas few exhibit overt symptomatologies. We report a case of epidermoid tumors in a unique location, presented as a secondary complex partial seizure. A forty-year-old female presented with multiple episodes of convulsions followed by loss of consciousness for nine months, increasing in frequency over the last two months. MRI of the brain without contrast showed a well-circumscribed right temporal lobe mass, appearing hypointense on the T1 and hyperintense on the T2 sequence. In addition to our experience and review of existing literature demonstrate gross total resection of these lesions confers control of localization-related epilepsy.
Keywords
Epidermoid cyst; Gross total resection; Aseptic meningitis; Seizure; Temporal lobe
Epidermoid cyst articles; Gross total resection articles; Aseptic meningitis articles; Seizure articles; Temporal lobe articles
Epidermoid cyst articles Epidermoid cyst Research articles Epidermoid cyst review articles Epidermoid cyst PubMed articles Epidermoid cyst PubMed Central articles Epidermoid cyst 2023 articles Epidermoid cyst 2024 articles Epidermoid cyst Scopus articles Epidermoid cyst impact factor journals Epidermoid cyst Scopus journals Epidermoid cyst PubMed journals Epidermoid cyst medical journals Epidermoid cyst free journals Epidermoid cyst best journals Epidermoid cyst top journals Epidermoid cyst free medical journals Epidermoid cyst famous journals Epidermoid cyst Google Scholar indexed journals Gross total resection articles Gross total resection Research articles Gross total resection review articles Gross total resection PubMed articles Gross total resection PubMed Central articles Gross total resection 2023 articles Gross total resection 2024 articles Gross total resection Scopus articles Gross total resection impact factor journals Gross total resection Scopus journals Gross total resection PubMed journals Gross total resection medical journals Gross total resection free journals Gross total resection best journals Gross total resection top journals Gross total resection free medical journals Gross total resection famous journals Gross total resection Google Scholar indexed journals Aseptic meningitis articles Aseptic meningitis Research articles Aseptic meningitis review articles Aseptic meningitis PubMed articles Aseptic meningitis PubMed Central articles Aseptic meningitis 2023 articles Aseptic meningitis 2024 articles Aseptic meningitis Scopus articles Aseptic meningitis impact factor journals Aseptic meningitis Scopus journals Aseptic meningitis PubMed journals Aseptic meningitis medical journals Aseptic meningitis free journals Aseptic meningitis best journals Aseptic meningitis top journals Aseptic meningitis free medical journals Aseptic meningitis famous journals Aseptic meningitis Google Scholar indexed journals Seizure articles Seizure Research articles Seizure review articles Seizure PubMed articles Seizure PubMed Central articles Seizure 2023 articles Seizure 2024 articles Seizure Scopus articles Seizure impact factor journals Seizure Scopus journals Seizure PubMed journals Seizure medical journals Seizure free journals Seizure best journals Seizure top journals Seizure free medical journals Seizure famous journals Seizure Google Scholar indexed journals Temporal lobe articles Temporal lobe Research articles Temporal lobe review articles Temporal lobe PubMed articles Temporal lobe PubMed Central articles Temporal lobe 2023 articles Temporal lobe 2024 articles Temporal lobe Scopus articles Temporal lobe impact factor journals Temporal lobe Scopus journals Temporal lobe PubMed journals Temporal lobe medical journals Temporal lobe free journals Temporal lobe best journals Temporal lobe top journals Temporal lobe free medical journals Temporal lobe famous journals Temporal lobe Google Scholar indexed journals Sylvian fissure articles Sylvian fissure Research articles Sylvian fissure review articles Sylvian fissure PubMed articles Sylvian fissure PubMed Central articles Sylvian fissure 2023 articles Sylvian fissure 2024 articles Sylvian fissure Scopus articles Sylvian fissure impact factor journals Sylvian fissure Scopus journals Sylvian fissure PubMed journals Sylvian fissure medical journals Sylvian fissure free journals Sylvian fissure best journals Sylvian fissure top journals Sylvian fissure free medical journals Sylvian fissure famous journals Sylvian fissure Google Scholar indexed journals suprasellar-chiasmatic articles suprasellar-chiasmatic Research articles suprasellar-chiasmatic review articles suprasellar-chiasmatic PubMed articles suprasellar-chiasmatic PubMed Central articles suprasellar-chiasmatic 2023 articles suprasellar-chiasmatic 2024 articles suprasellar-chiasmatic Scopus articles suprasellar-chiasmatic impact factor journals suprasellar-chiasmatic Scopus journals suprasellar-chiasmatic PubMed journals suprasellar-chiasmatic medical journals suprasellar-chiasmatic free journals suprasellar-chiasmatic best journals suprasellar-chiasmatic top journals suprasellar-chiasmatic free medical journals suprasellar-chiasmatic famous journals suprasellar-chiasmatic Google Scholar indexed journals basilar-posterior foss articles basilar-posterior foss Research articles basilar-posterior foss review articles basilar-posterior foss PubMed articles basilar-posterior foss PubMed Central articles basilar-posterior foss 2023 articles basilar-posterior foss 2024 articles basilar-posterior foss Scopus articles basilar-posterior foss impact factor journals basilar-posterior foss Scopus journals basilar-posterior foss PubMed journals basilar-posterior foss medical journals basilar-posterior foss free journals basilar-posterior foss best journals basilar-posterior foss top journals basilar-posterior foss free medical journals basilar-posterior foss famous journals basilar-posterior foss Google Scholar indexed journals retro-sellar-cerebellopontine articles retro-sellar-cerebellopontine Research articles retro-sellar-cerebellopontine review articles retro-sellar-cerebellopontine PubMed articles retro-sellar-cerebellopontine PubMed Central articles retro-sellar-cerebellopontine 2023 articles retro-sellar-cerebellopontine 2024 articles retro-sellar-cerebellopontine Scopus articles retro-sellar-cerebellopontine impact factor journals retro-sellar-cerebellopontine Scopus journals retro-sellar-cerebellopontine PubMed journals retro-sellar-cerebellopontine medical journals retro-sellar-cerebellopontine free journals retro-sellar-cerebellopontine best journals retro-sellar-cerebellopontine top journals retro-sellar-cerebellopontine free medical journals retro-sellar-cerebellopontine famous journals retro-sellar-cerebellopontine Google Scholar indexed journals Epidermoid cysts articles Epidermoid cysts Research articles Epidermoid cysts review articles Epidermoid cysts PubMed articles Epidermoid cysts PubMed Central articles Epidermoid cysts 2023 articles Epidermoid cysts 2024 articles Epidermoid cysts Scopus articles Epidermoid cysts impact factor journals Epidermoid cysts Scopus journals Epidermoid cysts PubMed journals Epidermoid cysts medical journals Epidermoid cysts free journals Epidermoid cysts best journals Epidermoid cysts top journals Epidermoid cysts free medical journals Epidermoid cysts famous journals Epidermoid cysts Google Scholar indexed journals
Article Details
1. Introduction
Epidermoid cysts (EC) are slowly growing; benign tumors account for 0.3 to 1.8 percent of all brain tumors. They can be divided into four categories describing their anatomic sites: retro-sellar-cerebellopontine angle, parasellar-Sylvian fissure, suprasellar-chiasmatic, and basilar-posterior fossa. Among these, the retro-sellar-cerebellopontine angle is the most frequent location found in about 40 percent of cases [1]. They occur from the third to fifth weeks of gestation when the ectoderm and neuroectoderm fail to separate properly, resulting in ectodermal inclusions during gastrulation [2, 3]. Epidermoid cysts are usually benign and consist of a thin capsule of stratified keratinized squamous epithelium. Symptoms depend on tumor location, including dizziness, hearing loss, tinnitus, gait disruption, trigeminal neuralgia, diplopia, vision impairment, lethargy, and headache [3]. Rupture of an epidermoid cyst is a rare but severe complication that may lead to chemical meningitis and hydrocephalus. Epilepsy secondary to epidermoid cysts fairly uncommon manifestation. Here we report a case of the right temporal lobe epidermoid cyst, presented with seizure.
2. Case Presentation
A 40 years old female presented with a history of multiple
episodes of convulsion for the last nine months; however, the first episode occurred while she was doing her household chores. First, she felt unwell, which was in the form of restlessness and eventually leading to a seizure followed by loss of consciousness for about 20-30 minutes. After she regained her consciousness, she remained confused for about 10-15 minutes. On query, she noticed a headache that was intermittent, global in distribution, mild in intensity, not associated with nausea or vomiting, no specific aggravating or relieving factor. However, headache preceded seizure during the last one and half months. There were no cognitive, motor, sensitivity, or coordination issues discovered during the neurological evaluation. MRI reveals an intra-axial mass located in the right anterior temporal region extending to the temporal pole and middle fossa dura downward, measuring about AP- 3.8 cm x CC- 4.1 cm x TD- 3.2 cm. The lesion is hypointense on T1WI, predominantly hyperintense on T2WI, diffusion restricted in DWI, medially the tumor is related with insular arteries, thin rim of grey matter surrounded laterally, medially and superiorly. There was slight ring enhancement, pre-operative radiological yields to some degree of a dilemma between epidermoid tumor and astrocytoma grade-II or III.
Surgery was performed through a right temporal craniotomy. Extradurally we reach the temporal pole. Then durotomy was done in a curvilinear fashion with reflected towards inferiorly. A thin cortical mantle was found over the cyst. An avascular intra-axial mass was exposed which was a pearly mass characteristic of an epidermoid cyst was encountered. The tumor was resected from the parenchyma without hampering the white matter, although in the medial aspect, some bits of tumor attached with M3 branches were left behind. The tumor contained cystic and solid portions, and the cystic content was viscid. The cystic lesion was filled with keratinized debris. No hair or obvious calcification or ossification was observed in the cyst. Post-operative recovery was uneventful. On the 3rd POD patient developed chemical meningitis and status epilepticus which was managed conservatively. At six months follow-up of the patient there were no neurological complaints and no signs of recurrence noticed. Histologically, the cyst wall was lined by stratified squamous epithelium and the cyst contained laminated layers of keratinized debris. No appendages of skin were present. The histopathological findings confirm the diagnosis of the epidermoid cyst.
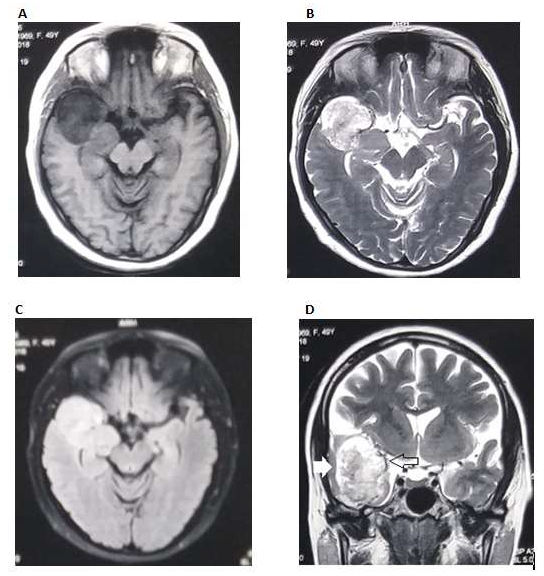
Figure 1: MRI shows (A) Hypointense mass in right temporal pole in T1WI; (B) Mixed intensity with predominantly hyperintense on T2WI; (C) Lesion was hyperintense in FLAIR sequence; (D) Measuring about 3.8 x 4.1 x 3.2 cc. medially related to insular arteries. Arrows denotes thin rim of cortex surrounding the lesion.
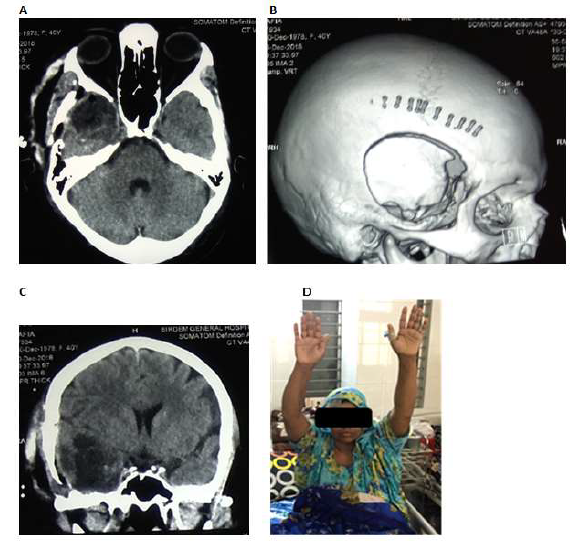
Figure 2: Post-operative image shows complete removal of tumor (A-C). No paresis observed at 9th POD (D).
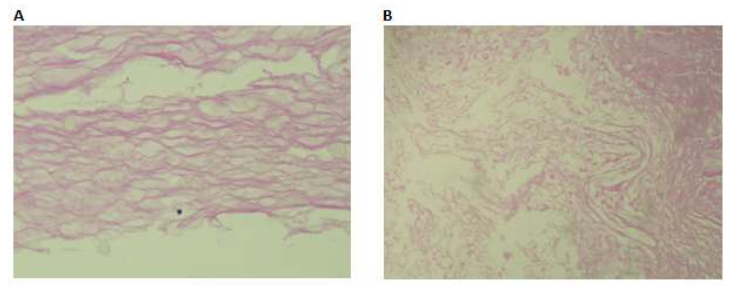
Figure 3: Section shows laminated layers and flakes of keratin material and squamous epithelium (A-B).
3. Discussion
Epilepsy caused by EC is uncommon, and the epileptogenesis process is still unknown. It might results from cyst infiltration into the brain parenchyma, chemical meningitis, or a structural alteration in epileptogenic areas. Intracerebral epidermoid tumors are uncommon, accounting for around 1.5 percent of all epidermoid tumors [4]. The pathogenesis of intracerebral epidermoid tumors is still controversial, and many theories have been suggested [5, 6]. A subpopulation of cells derived from mesectoderm lines that give rise to the skin may move and become entangled within the primitive cerebral hemisphere as the neural tube closes. These trapped cells may develop and differentiate, resulting in an epidermoid tumor, or they may have less cell differentiation, leading to the formation of a dermoid tumor [7]. Epidermoid cysts are composed of an outer cystic capsule, a keratinized stratified squamous epithelial layer, and inner cystic contents that include tissue debris, keratin, water, and solid cholesterol [3, 8]. Clinical manifestations of the IECs depend on the size and locations of the tumors [9]. For example, IECs affecting the brainstem exhibit rapidly progressive clinical course [10, 11]. Common signs of IECs include convulsion, hemiparesis, cranial nerve palsy, abnormal gait, and also symptoms of raised intracranial pressure [9, 12]. In addition, patients can also demonstrate signs of meningitis due to rupture of cyst or leakage of cyst contents spontaneously [11]. In our case, we found only several episodes of complex partial seizure.
MRI imaging with DWI is beneficial in the preoperative diagnosis of the IECs. All the IECs in children are located in the brainstem [13]. The common differential diagnosis includes dermoid cysts, arachnoid cysts. The most common location of intracranial ECs is extra-axial, whereas some intra-axial epidermoid cysts were also reported in some literature. They named those “Intracerebral epidermoid cysts,” “Intraparenchymal epidermoid cysts,” or “Intra-axial epidermoid cysts” [8, 9, 13, 14]. MRI remains the primary imaging modality for the diagnosis of IECs. The signal intensity depends on the relative amount of lipid, cholesterol, and keratin within the lesion [10]. On MRI, IECs usually appear hypointense on T1WI and hyperintense on T2WI [14]. They typically do not have peritumoral edema on T2WI and post-contrast enhancement [10, 12]. While in some cases, contrast enhancement was observed peripherally [10, 14-16]. In our case, we observed T1 hypointense, T2 mixed intense, FLAIR hyperintense, diffusion restricted in DWI, mild contrast rim enhancement. Fluid-attenuated inversion-recovery sequence (FLAIR) was more sensitive than conventional sequences in differentiation epidermoid cysts from arachnoid cysts as the epidermoid cases display hyperintense signal CSF as detected in 8 cases and intermediate signal intensity in 2 cases [15, 17, 18]. In our case, we found hyperintense in the FLAIR sequence.
Although the malignant transformation of these lesions is extremely rare malignant melanoma within the temporal lobe epidermoid cyst has been reported [19, 20, 21]. The transformation could be explained by the presence of different cellular elements within the tumors, which arise from the same embryological origin of the neural crest. Some articles stated about the malignant transformation of epidermoid tumors into carcinoma. They recommended immediate post-operative MRI to evaluate the amount of resection and close clinical and image follow-up twice per year after surgery [22]. Subtle growth without clinical deterioration may be followed on a routine basis. In case of clinical deterioration, urgent new MRI should be performed to exclude malignant transformation and changes in size, followed by changes in signal, edema, and gadolinium enhancement must point toward a new surgical approach [22]. The patient were discharged with an antiepileptic drug. Upon our radiological and clinical follow-up over six months, the patient remained seizure-free. The optimal management of intraparenchymal epidermoid cysts removes cyst content with complete resection of the capsule [11, 23]. However, radical removal of the tumor capsule is challenging because of the strong adherence of the tumor capsule with surrounding brain parenchyma, especially in eloquent areas such as the brainstem [2, 23]. The primary concern following conservative resection is tumor recurrence. Zheng et al. found a recurrence rate of 44.4% in patients who underwent subtotal resection [13]. The pathogenesis of this tumor is closely associated with the embryological territory [24]. A better understanding of the pathophysiology will lead to more effective preventative interventions.
4. Conclusion
This case should alert clinicians to the differential diagnosis of intraparenchymal brain tumors. Gross total excision of the lesion may result in a better seizure-free life. Regular postoperative follow-up is recommended to detect any malignant changes at an early stage.
References
- Trindade V, Gomes M, Santo M, et al. Giant Epidermoid Cyst: A Rare Cause of Temporal Lobe Epilepsy. J Neurol Surg Reports 78 (2017): e101-e105.
- Iaconetta G, Carvalho GA, Vorkapic P, et al. Intracerebral epidermoid tumor: a case report and review of the literature. Surg Neurol 55 (2001): 218-222.
- Recinos PF, Roonprapunt C, Jallo GI. Intrinsic brainstem epidermoid cyst. J Neurosurg Pediatr 104 (2006): 285-289.
- Chandler WF, Farhat SM, Pauli FJ. Intrathalamic epidermoid tumor. J Neurosurg 43 (1975): 614-617.
- Tytus JS, Pennybacker J. Pearly Tumours in Relation to the Central Nervous System. J Neurol Neurosurg Psychiatry 19 (1956): 241-259.
- Hila H, Bouhaouala MH, Darmoul M, et al. Kyste épidermoïde vermien révélé par un traumatisme crânien. Neurochirurgie 52 (2006): 63-66.
- Tatagiba G, Iaconetta M, Samii M. Epidermoid cyst of the cavernous sinus: clinical features, pathogenesis and treatment. Br J Neurosurg 14 (2000): 571-575.
- Shtaya A, Dabbous B, Fanou E, et al. Unusual Intraparenchymal Pontomedullary Epidermoid Cyst in a 2-Year-Old Child: A Case Report and Review of the Literature. World Neurosurg 104 (2017): 1046.e15-1046.e20.
- Yan PX, Yu CJ. Minicraniotomy Treatment of an Intracerebral Epidermoid Cyst. min - Minim Invasive Neurosurg 47 (2004): 245-248.
- Gopalakrishnan C V, Dhakoji A, Nair S. Epidermoid Cyst of the Brainstem in Children. J Child Neurol 27 (2012): 105-112.
- Patibandla M, Yerramneni V, Mudumba V, et al. Brainstem epidermoid cyst: An update. Asian J Neurosurg 11 (2016): 194.
- Hanft SJ, Komotar RJ, Raper DMS, et al. Epidermoid tumors of the temporal lobe as epileptogenic foci. J Clin Neurosci 18 (2011): 1396-1399.
- Zheng J, Wang C, Liu F. Intraparenchymal epidermoid cyst: proper surgical management may lead to satisfactory outcome. J Neurooncol 138 (2018): 591-599.
- Aribandi M, Wilson NJ. CT and MR imaging features of intracerebral epidermoid – a rare lesion. Br J Radiol 81 (2008): e97-e99.
- Hu X-y, Hu C-h, Fang X-m, et al. Intraparenchymal epidermoid cysts in the brain: diagnostic value of MR diffusion-weighted imaging. Clin Radiol 63 (2008): 813-818.
- Takahashi M, Paz Paredes A, Scavarda D, et al. Brainstem Epidermoid Cyst in a Child-Case Report-. Neurol Med Chir (Tokyo) 47 (2007): 140-144.
- Mohammad FF, Ayman, Ahmed F, et al. Usual and Unusual Locations of Intra-Cranial Epidermoid Inclusion Cyst. Cairo Univ 80 (2012): 229-238.
- Ikushima I, Korogi Y, Hirai T, et al. MR of epidermoids with a variety of pulse sequences. AJNR Am J Neuroradiol 18 (1997): 1359-1363.
- Uchino A, Hasuo K, Matsumoto S, et al. Intracranial epidermoid carcinoma: CT and MRI. Neuroradiology 37 (1995): 155-158.
- Michenet P, Vital C, Rivel J, et al. Malignant transformation of an intracranial epidermoid cyst. Ann Pathol 9 (1989): 360-362.
- Vajtai I, Tassi D, Varga Z, et al. Malignant melanoma evolving inside a cerebral epidermoid cyst. Orv Hetil 136 (1995): 1171-1174.
- Vellutini EAS, de Oliveira MF, Ribeiro APC, et al. Malignant transformation of intracranial epidermoid cyst. Br J Neurosurg 28 (2014): 507-509.
- Ahmed I, Auguste KI, Vachhrajani S, et al. Neurosurgical management of intracranial epidermoid tumors in children. J Neurosurg Pediatr 4 (2009): 91-96.
- Kaido T, Okazaki A, Kurokawa S-I, et al. Pathogenesis of intraparenchymal epidermoid cyst in the brain. Surg Neurol 59 (2003): 211-216.
