Epidemiological Profile of Stroke Cases at the Sylvanus Olympio University Hospital in Lomé, Togo, 2017 – 2018
Article Information
Abou-Bakari Tchala1, Agballa Mébiny-Essoh Tchalla Abalo2*, Kodjo Agbeko Djagadou1, Toyi Tchamdja3, Essona Matatom Akara4, Rébécca Kinde5, Komi Dzidzonu Nemi1, Edem Kossi Mossi6, Lihanimpo Djalogue3, Abago Balaka1, Mohaman Awalou Djibril1,6
1Service de Médecine Interne, Centre Hospitalier Universitaire Sylvanus Olympio, Lomé, Togo
2Direction Préfectorale de la Santé de Haho, Notsè, Togo
3Service de Médecine Interne, Centre Hospitalier Universitaire de Kara, Kara, Togo
4Service de Médecine Générale, Centre Hospitalier Préfectoral de Notsè, Togo
5Field Epidemiology Training Program, Togo
6Clinique Médico-Chirurgicale, Centre Hospitalier Universitaire Sylvanus Olympio, Lomé, Togo
*Corresponding Author: Agballa Mébiny-Essoh Tchalla Abalo, Ministère de la Santé et de l’Hygiène Publique, Direction Préfectorale de la Santé de Haho, Centre Hospitalier Préfectoral de Notsè, Togo
Received: 24 October 2020; Accepted: 04 November 2020; Published: 16 November 2020
Citation: Abou-Bakari Tchala, Agballa Mébiny-Essoh Tchalla Abalo, Kodjo Agbeko Djagadou, Toyi Tchamdja, Essona Matatom Akara, Rébécca Kinde, Komi Dzidzonu Nemi, Edem Kossi Mossi, Lihanimpo Djalogue, Abago Balaka, Mohaman Awalou Djibril. Epidemiological Profile of Stroke Cases at the Sylvanus Olympio University Hospital in Lomé, Togo, 2017 – 2018. Fortune Journal of Health Sciences 3 (2020): 148-159.
View / Download Pdf Share at FacebookAbstract
Introduction
Strokes are the first cause of non-traumatic disability and the second cause of death worldwide. Data analysis is useful to improve their care. Our purpose was to describe the epidemiological profile of stroke cases admitted at the Sylvanus Olympio University Hospital (CHU-SO) from 2017 to 2018.
Method
We conducted a descriptive study that included all stroke cases admitted at Internal Medicine Department of CHU-SO from January 2017 to December 2018. Socio-demographic and clinical data were collected by medical records reviewing and patients' interview and thereafter compiled and analyzed with Epi Info 7.2.1.0.
Results
The overall prevalence was 7.6% (173/2, 270) and 11.4% in patients aged 50 and over. Median age was 58.5 years, Interquartile interval (IQ) [48-65] and M/F sex ratio was 1.16. The median delay for admission to CHU-SO was one day, IQ [0-2]. Among patients' medical history, high blood pressure, strokes, alcoholism and diabetes accounted for 68.2% (118/173), 16.8% (29/173), 15.0% (26/173) and 12.1% (21/173) respectively. Hemorrhagic stroke cases accounted for 80.6% (29/36) in patients aged less than 50, while ischemia's accounted for 64.2% (61/95) among those aged 50 and over. Recovery occurred in 30.1% (52/173) with 80.8% (42/52) of sequelae. Deaths occurred in 62.4% (108/173) and were associated with the absence of the head CT scan (OR=2.71; 95% CI [1.14-6.73]).
Conclusion
Strokes affected mainly active people with high mortality exacerbated by the absence of the head CT scan. Early availability of the head CT scan and implementation of other specific strategies carried out of an action plan could contribute to reduce the burden of stroke at CHU-SO.
Keywords
Stroke; Internal Medicine Department; Lomé; Togo
Stroke articles; Internal Medicine Department articles; Lome articles; Togo articles, Stroke articles Stroke Research articles Stroke review articles Stroke PubMed articles Stroke PubMed Central articles Stroke 2023 articles Stroke 2024 articles Stroke Scopus articles Stroke impact factor journals Stroke Scopus journals Stroke PubMed journals Stroke medical journals Stroke free journals Stroke best journals Stroke top journals Stroke free medical journals Stroke famous journals Stroke Google Scholar indexed journals Internal Medicine Department articles Internal Medicine Department Research articles Internal Medicine Department review articles Internal Medicine Department PubMed articles Internal Medicine Department PubMed Central articles Internal Medicine Department 2023 articles Internal Medicine Department 2024 articles Internal Medicine Department Scopus articles Internal Medicine Department impact factor journals Internal Medicine Department Scopus journals Internal Medicine Department PubMed journals Internal Medicine Department medical journals Internal Medicine Department free journals Internal Medicine Department best journals Internal Medicine Department top journals Internal Medicine Department free medical journals Internal Medicine Department famous journals Internal Medicine Department Google Scholar indexed journals Lomé articles Lomé Research articles Lomé review articles Lomé PubMed articles Lomé PubMed Central articles Lomé 2023 articles Lomé 2024 articles Lomé Scopus articles Lomé impact factor journals Lomé Scopus journals Lomé PubMed journals Lomé medical journals Lomé free journals Lomé best journals Lomé top journals Lomé free medical journals Lomé famous journals Lomé Google Scholar indexed journals Togo articles Togo Research articles Togo review articles Togo PubMed articles Togo PubMed Central articles Togo 2023 articles Togo 2024 articles Togo Scopus articles Togo impact factor journals Togo Scopus journals Togo PubMed journals Togo medical journals Togo free journals Togo best journals Togo top journals Togo free medical journals Togo famous journals Togo Google Scholar indexed journals CHU-SO articles CHU-SO Research articles CHU-SO review articles CHU-SO PubMed articles CHU-SO PubMed Central articles CHU-SO 2023 articles CHU-SO 2024 articles CHU-SO Scopus articles CHU-SO impact factor journals CHU-SO Scopus journals CHU-SO PubMed journals CHU-SO medical journals CHU-SO free journals CHU-SO best journals CHU-SO top journals CHU-SO free medical journals CHU-SO famous journals CHU-SO Google Scholar indexed journals Odd Ratio articles Odd Ratio Research articles Odd Ratio review articles Odd Ratio PubMed articles Odd Ratio PubMed Central articles Odd Ratio 2023 articles Odd Ratio 2024 articles Odd Ratio Scopus articles Odd Ratio impact factor journals Odd Ratio Scopus journals Odd Ratio PubMed journals Odd Ratio medical journals Odd Ratio free journals Odd Ratio best journals Odd Ratio top journals Odd Ratio free medical journals Odd Ratio famous journals Odd Ratio Google Scholar indexed journals interquartile interval articles interquartile interval Research articles interquartile interval review articles interquartile interval PubMed articles interquartile interval PubMed Central articles interquartile interval 2023 articles interquartile interval 2024 articles interquartile interval Scopus articles interquartile interval impact factor journals interquartile interval Scopus journals interquartile interval PubMed journals interquartile interval medical journals interquartile interval free journals interquartile interval best journals interquartile interval top journals interquartile interval free medical journals interquartile interval famous journals interquartile interval Google Scholar indexed journals
Article Details
Introduction
Stroke is defined by the World Health Organization as the rapid development of localized or global clinical signs of brain dysfunction with symptoms lasting more than 24 hours and resulting in death with no apparent cause other than vascular origin [1]. It is the second leading cause of death worldwide and the third leading cause of death in low-income countries [2]. It is also the leading cause of acquired disability in adults and a leading cause of dementia [2,3]. Through mortality, physical disabilities and the expenses they entail, they have a negative impact on the socio-economic situation of countries [2,4,5,6].
Stroke incidence and mortality in low-income countries continue to rise [7]. In Togo, data on stroke are from the medical records of patients admitted to hospitals. The Sylvanus Olympio University Hospital (CHU-SO) and Campus University Hospital (CHU Campus) in Lomé and the Kara University Hospital (CHU Kara) are the national referral centers for stroke case management. According to a 2015 study conducted by Balogou [8], the estimated inpatient prevalence of stroke in Togo is 49.4%.
Over the past five years, stroke research in Togo has included a systematic review of stroke studies conducted in Togo [8], epidemiologic aspects of stroke cases admitted to Kara University Hospital [9], and CT scan aspects [10] and factors predictive of mortality [11]. Although CHU-SO is a major stroke referral hospital, no studies have specifically addressed the epidemiologic profile of strokes admitted to the neurology and internal medicine departments at this hospital despite data availability. Yet such research could help medical teams reorient or implement interventions that have an impact on stroke morbidity and mortality. The results of this study could also serve for planning and budgeting resources to ensure their continued availability for more effective stroke control.
The objective of this study was to describe the epidemiological profile of stroke cases admitted to the Internal Medicine Department of Sylvanus Olympio University Hospital from January 2017 and December 2018 to characterize their magnitude, socio-demographic and clinical characteristics and trends.
Methods
Study area
The study was conducted at the Internal Medicine Department of the CHU-SO in Lomé.
Study Design and Period
This was a descriptive study conducted from February 1 to March 1, 2019.
Study Population
Study population was stroke cases admitted to the Internal Medicine Department at CHU-SO from January 1, 2017 and December 31, 2018.
Case Definition
A stroke case was any patient admitted to the Internal Medicine Department of CHU-SO between January 1, 2017 and December 31, 2018 who had a focal neurological deficit of abrupt onset lasting more than 24 hours and/or in whom the head CT scan revealed an ischemic or hemorrhagic stroke.
Data Collection and Tools
We collected data by reviewing patients’ medical records and completed by individual interviews during patients’ medical follow-up visits to the CHU-SO and also by telephone calls. Data collected was recorded on a form and a line-list in Excel designed for this study.
Study Variables
The study variables were:
- Socio-demographic variables: age, sex, socio- professional category, case origin;
- Clinical variables: motif for admission, type of stroke, personal history, duration of hospitalization, and outcomes.
Data Processing and Analysis
We used "Microsoft Word" for text entry and "Microsoft Excel" for data compilation. For the analysis we used Epi Info version 7.2.1.0. The results are presented in tables and graphs with values representing ratios, proportions, median and interquartile interval. For the statistical analysis we used the Chi-square test or the Fisher Exact test to assess the difference with a significance level of p < 0.05 and the 95% confidence interval to assess the significance of the Odd Ratio (OR) between deaths and the factors studied.
Definition of Concepts
Ischemic Stroke (IS): Type of stroke for which brain imaging (Head CT scan or Magnetic Resonance Imaging) excludes any other potential cause and in particular a cerebral hemorrhage.
Hemorrhagic Stroke (HS): Type of stroke for which brain imaging shows a recent hemorrhage congruent with clinical signs.
Stroke recovery: Stopping the process that caused the stroke (bleeding or ischemia) with partial or complete regression of signs. When the regression of signs is incomplete, it is referred to a recovery with sequelae.
Socio-professional Categories
The categorization described by the “Institut National de la Statistique, des Etudes Economiques et Démographiques (INSEED)” of Togo during the survey of Basic Welfare Indicators (QUIBB) conducted in Togo in 2015 [12] was used as the basis for defining socio- professional categories in relation to the period prior to the last stroke episode.
- Public employee: Any person having a permanent or fixed-term job in the public administration or in a Togolese state
- Private employee: Any person with a permanent or fixed-term job in a private company, a Non-Governmental Organization, an association, a group or a
- Self-employed farmer: Any person working for his or her own account in agriculture, animal husbandry or
- Other self-employed: Any person working for his or her own account in sectors other than agriculture, livestock and
- Other asset: A person who contributes to the production of a service or market good but whose consideration is generally not a salary (apprentice, trainee).
- Unemployed: Anyone between the ages of 15 and 64 who had not worked in the last seven days prior to the last stroke episode and who had looked for work during the same
- Inactive: Anyone who has not been employed in the seven days prior to the last stroke event, has not taken any steps to look for work, or was not ready to work in the four weeks prior to the last stroke event.
Ethical Considerations
Prior authorization was obtained from the CHU-SO administration and the Internal Medicine Department before conducting the study. The data collection, both during the analysis of the files and during the interview, was carried out confidentially and anonymously.
Results
Prevalence
During the study period, 2,270 patients were admitted to the Department, 173 of whom had a stroke, for an overall prevalence of 7.6%. Proportional morbidity ranged from 6.5% (75/1146) in 2017 to 8.7% (98/1122) in 2018 with p = 0.068. Table 1 presents prevalence by sex, age, and year.
Table 1: Prevalence of stroke by sex, age group, and year, Department of Internal Medicine, Sylvanus Olympio University Hospital, 2017-2018.
|
Variables |
Number of hospitalizations |
Number of stroke cases |
Proportion of Stroke Cases (%) |
p – value |
|
|
Sex |
Male |
1165 |
93 |
8.00 |
0.305 |
|
Female |
1178 |
80 |
6.80 |
||
|
Age groups |
Less than 50 years old |
1178 |
48 |
4.10 |
0.000 |
|
50 years old and over |
1092 |
125 |
11.40 |
||
|
Period |
2017 |
1146 |
75 |
6.50 |
0.068 |
|
2018 |
1122 |
98 |
8.70 |
||
Socio-demographic characteristics
Age and sex
The overall median age was 58.5 years with an interquartile interval (IQ) [48-65]. For the overall period, patients aged 50 years and older accounted for 72.3% (125/173) of cases while those aged less than 60 accounted for 52.0% (90/173). The M/F sex ratio were 1.16 for the overall period and ranged from 1.27 in 2017 to 1.09 in 2018 with p=0.604. Within age groups, this ratio was 1.67 for those under 50 years of age and 1.02 for those 50 years of age and older with p=0.152.
Socio-professional category and origin of cases
Data on the socio-professional category were available for 86.1% (149/173) and showed a proportion of self-employed workers of 48% (71/149). The place of origin variable was known for 89.6% (155/173) of patients, of whom 81.3% (126/155) were from the Lomé Commune region.
Clinical Features
Delay for recourse to the Sylvanus Olympio University Hospital
The median time to reach medical care at CHU-SO was one day IQ [0-2]. Between 2017 and 2018, the median time to reach CHU-SO varied between one day IQ [0-2] and less than one day IQ [0-1], respectively. In 53.8% of cases, the time to admission to CHU-SO was 24 hours or more. For both men and women, the median time to reach CHU-SO was one day.
Motif for admission
Over the two years, the three leading causes for admission were altered consciousness in 131 patients (75.7%), hemibody motor deficiency in 113 patients (65.3%) and central facial paralysis in 37 patients (21%). The distribution of patients by causes for admission is shown in Figure 1.
Patients’ history
In the history of patients admitted for stroke, high blood pressure was found in 118 patients (68.2%), stroke in 29 patients (16.8%), alcoholism in 26 patients (15%) and diabetes in 21 patients (12.1%). No previous history was found in 24 patients (13.9%).
Types of Stroke
Head computed tomography was performed on 131 patients (75.7%) and revealed ischemic stroke in 51.9% and hemorrhagic stroke in 48.1%. The proportion of stroke types varied by year, sex and age group (Table 2). Within age groups, HS accounted for 80.6% of cases in people younger than 50 years of age and 35.8% in people 50 years of age and older (Figure 2).
Table 2: Distribution of Stroke Type by Sex and Age Groups, Department of Internal Medicine, Sylvanus Olympio University Hospital, 2017–2018.
|
Variables |
Hemorrhagic Stroke |
Ischemic Stroke |
|||||
|
2017 n (%) |
2018 n (%) |
2017-2018 n (%) |
2017 n (%) |
2018 n (%) |
2017 – 2018 n (%) |
||
|
Sex |
Male |
11 (57.90) |
23 (52.30) |
34 (54.00) |
19 (54.30) |
15 (45.50) |
34 (50.00) |
|
Female |
8 (42.10) |
21 (47.70) |
29 (46.00) |
16 (45.70) |
18 (54.50) |
34 (50.00) |
|
|
Age Groups |
< 50 years old |
6 (31.60) |
23 (52.3) |
29 (46.00) |
6 (17.10) |
1 (03.00) |
7 (10.30) |
|
≥ 50 years |
13 (68.40) |
21 (47.70) |
34 (54.00) |
29 (82.90) |
32 (97.00) |
61 (89.70) |
|
Duration of Hospitalization
The overall median duration of stay was 9 days with IQ [3.5-18] and did not varied by year or sex.
Characteristics of Evolution
The evolution was marked by the recovery for 30.1% (52/173) patients including 80.8% (42/52) with sequelae. These sequelae were dominated by chronic headache: 69.0% (29/42), motor deficit: 61.9% (26/42), paresthesia: 35.7% (15/42), dementia: 33.3% (14/42) and epilepsy: 16.7% (7/42). Twenty-eight patients (66.7%) had at least two types of sequelae. Thirteen patients (7.5%) were discharged against medical advice. The overall case fatality rate was 62.4% (108/173). It ranged from 64.0% (48/75) in 2017 to 61.2% (60/98) in 2018 with p = 0.857. For both years, it was 67.7% (63/93) in men and 56.3% (45/80) in women with p = 0.452 (Table 3).
Performing the head CT scan was associated with stroke patients’ survival with OR = 2.71, 95% CI [1.14 - 6.73] and p = 0.013. Case fatality was 50% in patients with no known history and ranged from 62.7% to 100% in patients with a history depending on the nature of the history.
Table 3: Distribution of Stroke Cases and Deaths by Sex, Age Group, Type of Stroke, Year of Admission, and Head computer tomography scan completion, Department of Internal Medicine, Sylvanus Olympio University Hospital, 2017-2018.
|
Variables |
Case (n) |
Death (n) |
Case Fatality (%) |
p – value |
|
|
Sex |
Female |
80 |
45 |
56.25 |
0.452 |
|
Male |
93 |
63 |
67.74 |
||
|
Age Groups (years) |
0- 50 |
48 |
30 |
62.50 |
0.995 |
|
51 – 98 |
125 |
78 |
62.40 |
||
|
Year of Admission |
2017 |
75 |
48 |
64.00 |
0.857 |
|
2018 |
98 |
60 |
61.22 |
||
|
Type of Stroke |
Ischemic |
68 |
38 |
55.88 |
0.863 |
|
Hemorrhagic |
63 |
37 |
58.73 |
||
|
Head Computer Tomography |
Performed |
131 |
75 |
57.25 |
0.013 |
|
Not performed |
42 |
33 |
78.57 |
||
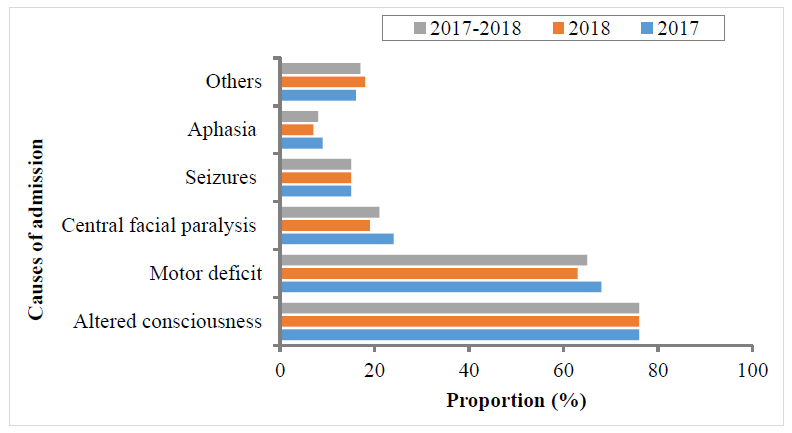
Figure 1: Distribution of Causes of Admission in Stroke Patients, Department of Internal Medicine, Sylvanus Olympio University Hospital, Togo, 2017 - 2018.
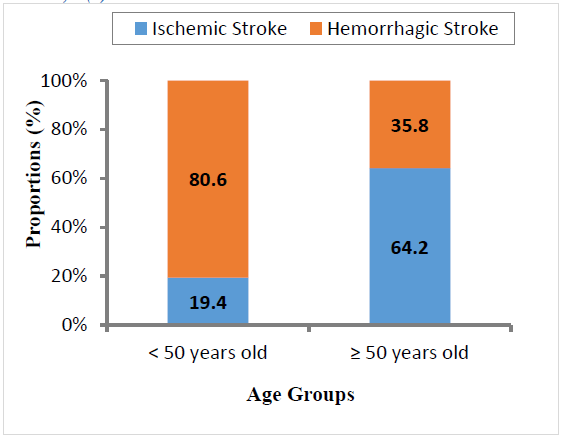
Figure 2: Distribution of Stroke Types by Age Group, Department of Internal Medicine, Sylvanus Olympio University Hospital, Togo, 2017 – 2018.
Discussion
This study determined the proportional morbidity of stroke in the Department of Internal Medicine of CHU-SO. It has also revealed the link between age and the type of stroke as well as the high mortality of patients admitted. The study also showed a relationship between performing Head CT scan and the survival of patients admitted for stroke at CHU-SO. The results of this secondary data analysis may be compromised by data quality, including a significant proportion of missing and inconsistent data. Most of the necessary data was available for this study. Indeed, for the variables with incomplete information, the proportion of available data was at least 86%.
Inconsistencies were corrected by a second review of medical records and by interviewing patients at their follow-up visit. Inconsistencies that could not be corrected were removed.
Prevalence
The overall prevalence was 7.6%. For a pathology with high fatality and disability, this prevalence is high. It is significantly higher in subjects aged 50 years and over, where it is 11.4%, than in subjects under 50 years of age, where it is 4.1% (p=0.000). This difference suggests that the prevalence of stroke may increase with age, as shown in other studies in Africa and around the world [1,13,14,15]. The incidence of stroke in our study is similar to the 6.5% prevalence (p=0.338) reported by Coulibaly [6] in a study conducted in three Medicine Departments in Mali. Pio [16] in Togo and Basse [13] in Senegal reported higher frequencies of 45% (p=0.000) and 19.6% (p=0.000), respectively. The differences can be explained by the study sites: our study was conducted in an Internal Medicine Department where are admitted all types of patients, while those of Basse [13] and Pio [16] were conducted in a Neurology Departments where are only admitted patients with neurologic conditions, primarily stroke.
Socio-demographic Characteristics
The patients’ mean age was 58.5 years and 52% were under 60 years of age. These results showed that the majority of stroke cases admitted to CHU-SO are adult who correspond to the active category of society. The occurrence of stroke could have an impact on family income through death and disability.
In Togo, Pio [16], Apetse [17] and Kumako [9] reported a mean age of 58.2 years, 58.22 years and 59.66 years respectively, while N'goran [18] in Côte d'Ivoire reported a mean age of 60 years. A higher mean age of 72.8 years was reported in France by Peretti [19] and 67 years in India by Sridharan [14]. The differences observed between these different types of average age can be explained by the difference in life expectancy between countries: relatively low in sub-Saharan African countries (60 years in Togo and 54 years in Côte d'Ivoire) compared to 69 years in India and 83 years in France [20]. In our study, we noted a male predominance with M/F sex ratio of 1.16 with a non-significant variation between 1.27 in 2017 and 1.08 in 2018 (p=0.604). On the other hand, a sex ratio with a female predominance (F/M = 1.23) was reported by Pio [16] in Togo. Male predominance seems to be more pronounced in patients under 50 with a sex ratio of 1.67 compared to 1.02 in patients aged 50 and over.
Clinical Features
In our study, the median time to seek medical care at the CHU-SO was 1 day IQ [0-2] (mean 2.1±4.3 days) with 53.8% of patients seeking care at least 24 hours after the onset of symptoms. This relatively long delay in relation to the severity of the disease can be explained by the low socioeconomic level of the populations leading to prior recourse to self- medication and a long delay in patient referral. Kumako [9] reported a longer average delay (5.15±8.97 days) in Kara, Togo.
The most frequent reasons for hospital admission were altered consciousness (75.7%) and hemibody motor deficit (65.3%). The high proportion of cases with altered consciousness can be explained by the nature of the Department, which has an intensive care unit and thus receives most severe cases. In African populations, due to a lack of knowledge about stroke and poverty, it is often the apparent severity of symptoms that motivates consultations or referrals, resulting in a low proportion of signs such as headache, facial paralysis, or paresthesia. Keita [21] in Mali reported a predominance of coma and hemiplegia, with a frequency of 47.8% and 54.7% respectively.
The patients’ history was dominated by high blood pressure (68.2%), alcoholism (15%) and diabetes (12.1%). This may indicate that a history of these conditions increases the risk of stroke. Most stroke studies [1,4,16,22] have reported high blood pressure as the most common risk factor for stroke.
The proportion of the two types of stroke was roughly the same (51.9% IS and 48.1% HS). However, there was an increase in the number and proportion of HS between 2017 and 2018 from 19 cases (35.2%) to 44 cases (57%), particularly among those younger than 50 years of age, where the proportion increased from 31.6% to 52.3%. HS was predominant in younger patients (80.6% of patients under 50 years of age had a HS). Other studies in Togo [9,16,17] found similar proportions for both types of stroke. Sun [23] reported ischemic stroke ranging from 43% to 78% in China versus 87% in Europe and hemorrhagic stroke ranging from 18% to 47% in China versus 10% in Europe.
Characteristics of Evolution
In our series, we noted a high case fatality of 62.4% among hospitalized stroke patients. This is significantly higher than the case-fatality reported in various studies in Togo [9] and Africa [6,22,24], which ranged from 20.3% to 44.6%. This high case fatality could be due to a conjunction of several factors. For patients, first of all, the severe and critical condition of patients at admission, sometimes associated with comorbidities that were initially unknown or insufficiently managed. This critical state may be aggravated by the delay in medical consultation, often with initial recourse to self-medication, traditional practitioners or religious worship centers, a situation most often favored by the low socio-economic level. Secondly, it could be the low capacity of the CHU-SO due to the non-availability of diagnostic means as well as limited therapeutic means. Patients were transported even in the acute phase to other health structures for the CT scan. The sequelae were found in 80.8% of the recovered patients, some of which were a source of significant disability such as epilepsy (16.7%), dementia (33.3%) or motor deficit (61.9%). This shows the heavy burden of morbidity associated with this condition responsible for a more or less important and most often definitive dependence.
Conclusion
Strokes are common in the Internal Medicine Department and affect active people. They are responsible for a high case fatality and disabling sequelae that have a significant social and economic impact. Despite this threat, the current health situation does not appear to be favorable in the short and midterm to controlling this disease, due to an insufficient technical platform and often the late recourse to health facilities. There is a need to develop and implement a stroke control action plan with strategies including communication and outreach interventions among people living with defects at risk of stroke. It is also critical to equip CHU-SO with stroke diagnostics, equipment, materials, and medications for stroke management. Capacity building of human resources at the CHU-SO supported by a supervision and monitoring/evaluation mechanism is also essential for stroke control.
Acknowledgements
The authors would like to express their gratitude to the Ministry of Health and Public Hygiene, the Direction of the Sylvanus Olympio University Hospital and the Head of the Internal Medicine Department of the CHU-SO.
Conflicts of interest:
The authors have declared that they have no conflicts of interest.
Contributions of the authors:
- Design and definition of the work plan: Abou-Bakari Tchala, Agballa Mébiny-Essoh Tchalla Abalo, A. Balaka
- Data Collection: Abou-Bakari Tchala
- Analysis and interpretation: Abou-Bakari Tchala, Agballa Mébiny-Essoh Tchalla Abalo, Essona Matatom Akara
- Writing of the manuscript: Abou-Bakari Tchala, Agballa Mébiny-Essoh Tchalla Abalo, Essona Matatom Akara
- Reviewed by: K.A. Djagadou, A. Balaka, T. Tchamdja, R. Kinde, K. D. Nemi, L. Djalogue, E. K. Mossi, M. A. Djibril
- Reading and validation of the final manuscript: All
What do we already know on this subject?
Data on inpatient stroke prevalence in Africa, risk factors associated with stroke, CT scan aspects, outcomes (mortality, sequelae).
What else does this study bring?
This study focuses on the epidemiology of stroke in a level 3 national referral service in Lomé with prevalence in a non-neurological service. It reveals the critical importance of early availability of CT images to guide therapeutic management and the association between their availability and stroke-related mortality.
References
- Béjot Y, Touzé E, Jacquin A, et al. Épidémiologie des accidents vasculaires cérébraux. Médecine/Sciences 25 (2009): 727-732.
- World Health Organization. Global Health Estimates 2016: Estimated deaths by age, sex, and cause. [Cited 2019, Feb 20]. Available at: https://www.who.int/healthinfo/global_burden_disease/estimates/en/ (2016).
- Adoukonou TA, Vallat JM, Joubert J, et al. Prise en charge des accidents vasculaires cérébraux en Afrique subsaharienne. Revue Neurologique 166 (2010): 882-893.
- Belo M, Balogou AA, Goeh-Akue E, et al. Particularites des accidents vasculaires cerebraux au Togo et en Afrique noire. Journal de la Recherche Scientifique de l’Universite de Lome 9 (2007).
- Balogou AA, Tossa KR, Kowu A, et al. Prix de revient d’une hospitalisation dans le service de neurologie du CHU de Lomé (Togo). Cahiers d'études et de Recherches Francophones/Santé 14 (2004): 109-114.
- Coulibaly M, Toure MK, Traore AO, et al. Les Accidents Vasculaires Cérébraux au CHU «Le Luxembourg» de Bamako: Aspects Cliniques, Thérapeutiques et Pronostiques. Health Sciences and Disease 20 (2019).
- Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. The Lancet 383 (2014): 245-255.
- Balogou AA, Belo M. Epidémiologie récente des accidents vasculaires cérébraux au Togo. Revue Neurologique 171 (2015): A235-A236.
- Kumako VK, N’Timon B, Apetse K, et al. Accidents Vasculaires Cerebraux (AVC) au Centre Hospitalier Universitaire de Kara en zone semi rurale au Togo: aspects epidemiologiques et evolutifs. Journal de la Recherche Scientifique de l’Université de Lomé 19 (2017): 291-298.
- Sonhaye L, Tchaou M, Adjenou K, et al. Aspects scanographiques des accidents vasculaires cerebraux au Chu campus de Lome, Togo (A propos de 314 cas). Journal de la Recherche Scientifique de l’Université de Lomé 13 (2011): 25-30.
- Anayo KN, Agba L, Guinhouya KM, et al. Facteurs predictifs de mortalite des hematomes cerebraux aux CHU de lome. African Journal of Neurological Sciences 36 (2017): 17-22.
- Institut National de la Statistique et des Etudes Economiques et Démographiques (INSEED), Togo. Enquête sur les Indicateurs de Base du Bien Etre (QUIBB), Togo. [Cited 2018 sep 21]. Available at: http://www.stat-togo.org/contenu/pdf/pb/pb-rap-final-QUIBB-tg-2015.pdf (2015).
- Basse AM, Diagne NS, Boubacar S, et al. Epidemiology of Stroke: A Senegalese Study. Ann Clin Pathol 5 (2017): 1122.
- Sridharan SE, Unnikrishnan JP, Sukumaran S, et al. Incidence, types, risk factors, and outcome of stroke in a developing country: the Trivandrum Stroke Registry. Stroke 40 (2009): 1212-1218.
- de Peretti C, Chin F, Tuppin P, et al. Personnes hospitalisées pour accident vasculaire cérébral en France: tendances 2002–2008. Bull Epidemiol Hebd 10 (2012): 125.
- Pio M, Afassinou YM, Goeh-Akue E, et al. Autres Facteurs concourant aux accidents vasculaires cérébraux chez l’hypertendu traité au CHU sylvanus Olympio de Lomé. Revue Africaine et Malgache de Recherche Scientifique/Sciences de la Santé 3 (2015).
- Apetse K, Matelbe MC, Assogba K, et al. Prevalence de la syslipidemie, de l'hyperglycemie et de l'hyperrurucemi chez les patients victimes d'accidents vasculaires cerebraux au Togo. African Journal of Neurological Sciences 30 (2011).
- N’goran YN, Traore F, Tano M, et al. Aspects épidémiologiques des accidents vasculaires cérébraux (AVC) aux urgences de l’institut de cardiologie d’Abidjan (ICA). Pan African Medical Journal 21 (2015).
- de Peretti C, Nicolau J, Tuppin P, et al. Évolutions de la prise en charge hospitalière des accidents vasculaires cérébraux en court séjour et en soins de suite et de réadaptation entre 2007 et 2009 en France. La Presse Médicale 41 (2012): 491-503.
- Banque Mondiale. Indicateurs de développement dans le monde [Internet] [Cited 2019, May 18]. Available at: https://databank.banquemondiale.org/indicator/SP.DYN.LE00.IN/1ff4a498/Popular-Indicators
- Keita AD, Toure M, Diawara A, et al. Aspects epidemiologiques des accidents vasculaires cerebraux dans le service de tomodensitometrie a l'Hopital du Point G. Médecine Tropicale 65 (2005): 453-457.
- Sagui E. Les accidents vasculaires cerebraux en Afrique subsaharienne. Médecine tropicale 67 (2007): 596-600.
- Sun H, Zou X, Liu L. Epidemiological factors of stroke: a survey of the current status in China. Journal of Stroke 15 (2013): 109.
- Garbusinski JM, van der Sande MA, Bartholome EJ, et al. Stroke presentation and outcome in developing countries: a prospective study in the Gambia. Stroke 36 (2005): 1388-1393.
