Enteric Fever with Concomitant Pancreatitis and Cholangitis. A Case Report-Based Review of the Literature
Article Information
Qutabuddin Khuhro3, Muhammad Sohaib Asghar1*, Atif Majeed3, Hafeezullah Shaikh3, Shobha Luxmi1, Abubakar Tauseef1, Maryam Zafar1, Uzma Rasheed2, Mariam Siddiqui1, Saad Aslam1
1Department of Internal Medicine, Dow University Hospital, Karachi, Pakistan
2Department of Internal Medicine, Liaquat National Hospital and Medical College, Karachi, Pakistan
3Department of Gastroenterology, Dow University Hospital, Karachi, Pakistan
*Corresponding author: Muhammad Sohaib Asghar, Department of Internal Medicine, Dow University Hospital, Karachi, Pakistan
Received: 14 December 2019; Accepted: 30 December 2019; Published: 31 December 2019
Citation:
Qutabuddin Khuhro, Muhammad Sohaib Asghar, Atif Majeed, Hafeezullah Shaikh, Shobha Luxmi, Abubakar Tauseef, 'Maryam Zafar and Uzma Rasheed', Mariam Siddiqui, Saad Aslam. Enteric Fever with Concomitant Pancreatitis and Cholangitis. A Case Report-Based Review of the Literature. Archives of Internal Medicine Research 2 (2019): 085-091.
View / Download Pdf Share at FacebookAbstract
Here we present a case of concomitant pancreatitis and cholangitis in a young female patient with culture-proven Salmonella Typhi in the blood which was sensitive to Meropenem and Azithromycin only. The multiple drug-resistant strain of Salmonella Typhi can lead to serious complications as was present in our case. The resistance is acquired by alteration in the genome sequence. Currently, control of such an unknown outbreak of Salmonella Typhi's multiple drug-resistant strains are important, since it is a serious healthcare issue in disease control and prevention of endemic countries.
Keywords
Typhoid, Pancreas, Cholangitis, Fever, Enteric, Outbreak
Typhoid articles Typhoid Research articles Typhoid review articles Typhoid PubMed articles Typhoid PubMed Central articles Typhoid 2023 articles Typhoid 2024 articles Typhoid Scopus articles Typhoid impact factor journals Typhoid Scopus journals Typhoid PubMed journals Typhoid medical journals Typhoid free journals Typhoid best journals Typhoid top journals Typhoid free medical journals Typhoid famous journals Typhoid Google Scholar indexed journals Pancreas articles Pancreas Research articles Pancreas review articles Pancreas PubMed articles Pancreas PubMed Central articles Pancreas 2023 articles Pancreas 2024 articles Pancreas Scopus articles Pancreas impact factor journals Pancreas Scopus journals Pancreas PubMed journals Pancreas medical journals Pancreas free journals Pancreas best journals Pancreas top journals Pancreas free medical journals Pancreas famous journals Pancreas Google Scholar indexed journals Cholangitis articles Cholangitis Research articles Cholangitis review articles Cholangitis PubMed articles Cholangitis PubMed Central articles Cholangitis 2023 articles Cholangitis 2024 articles Cholangitis Scopus articles Cholangitis impact factor journals Cholangitis Scopus journals Cholangitis PubMed journals Cholangitis medical journals Cholangitis free journals Cholangitis best journals Cholangitis top journals Cholangitis free medical journals Cholangitis famous journals Cholangitis Google Scholar indexed journals Fever articles Fever Research articles Fever review articles Fever PubMed articles Fever PubMed Central articles Fever 2023 articles Fever 2024 articles Fever Scopus articles Fever impact factor journals Fever Scopus journals Fever PubMed journals Fever medical journals Fever free journals Fever best journals Fever top journals Fever free medical journals Fever famous journals Fever Google Scholar indexed journals Enteric articles Enteric Research articles Enteric review articles Enteric PubMed articles Enteric PubMed Central articles Enteric 2023 articles Enteric 2024 articles Enteric Scopus articles Enteric impact factor journals Enteric Scopus journals Enteric PubMed journals Enteric medical journals Enteric free journals Enteric best journals Enteric top journals Enteric free medical journals Enteric famous journals Enteric Google Scholar indexed journals Outbreak articles Outbreak Research articles Outbreak review articles Outbreak PubMed articles Outbreak PubMed Central articles Outbreak 2023 articles Outbreak 2024 articles Outbreak Scopus articles Outbreak impact factor journals Outbreak Scopus journals Outbreak PubMed journals Outbreak medical journals Outbreak free journals Outbreak best journals Outbreak top journals Outbreak free medical journals Outbreak famous journals Outbreak Google Scholar indexed journals paratyphoid articles paratyphoid Research articles paratyphoid review articles paratyphoid PubMed articles paratyphoid PubMed Central articles paratyphoid 2023 articles paratyphoid 2024 articles paratyphoid Scopus articles paratyphoid impact factor journals paratyphoid Scopus journals paratyphoid PubMed journals paratyphoid medical journals paratyphoid free journals paratyphoid best journals paratyphoid top journals paratyphoid free medical journals paratyphoid famous journals paratyphoid Google Scholar indexed journals lower immunity articles lower immunity Research articles lower immunity review articles lower immunity PubMed articles lower immunity PubMed Central articles lower immunity 2023 articles lower immunity 2024 articles lower immunity Scopus articles lower immunity impact factor journals lower immunity Scopus journals lower immunity PubMed journals lower immunity medical journals lower immunity free journals lower immunity best journals lower immunity top journals lower immunity free medical journals lower immunity famous journals lower immunity Google Scholar indexed journals nausea articles nausea Research articles nausea review articles nausea PubMed articles nausea PubMed Central articles nausea 2023 articles nausea 2024 articles nausea Scopus articles nausea impact factor journals nausea Scopus journals nausea PubMed journals nausea medical journals nausea free journals nausea best journals nausea top journals nausea free medical journals nausea famous journals nausea Google Scholar indexed journals anti-pyretic articles anti-pyretic Research articles anti-pyretic review articles anti-pyretic PubMed articles anti-pyretic PubMed Central articles anti-pyretic 2023 articles anti-pyretic 2024 articles anti-pyretic Scopus articles anti-pyretic impact factor journals anti-pyretic Scopus journals anti-pyretic PubMed journals anti-pyretic medical journals anti-pyretic free journals anti-pyretic best journals anti-pyretic top journals anti-pyretic free medical journals anti-pyretic famous journals anti-pyretic Google Scholar indexed journals
Article Details
1. Introduction
Enteric fever consists of typhoid and paratyphoid fever, caused by Salmonella enterica serotype Typhi and Paratyphi A, B, and C. The clinical manifestations of both are similar but the intensity of paratyphoid fever is less severe. Salmonella typhi organisms are gram-negative, anaerobic, non-encapsulated, flagellated bacilli [1]. Mostly, infections by Salmonella typhi occur in developing countries and are the highest in incidence in areas with poor sanitation. The incidence of the disease increases during the hot, dry season or after heavy rains in which drinking water is contaminated by the sewer system. Over the past century, there has been a dramatic fall in the incidence of Typhoid fever in the United States due to improved sanitary conditions, water treatment and food handling practices and mostly are now acquired by contact with asymptomatic carriers. In endemic areas, children aged 1-5 years are at the highest risk of developing an infection due to lower immunity and the disappearance of their maternal antibodies. Susceptibility to Typhoid fever is increased in people with co-existing illnesses such as HIV-infection or people taking antibiotics or proton pump inhibitors, the latter reducing gastric acid, which is a primary host defense mechanism against Salmonella typhi. Infection is spread via a fecal-oral route by food or water that is contaminated by an infected person with active disease or an asymptomatic chronic carrier [1].
2. Case Presentation
A 25 years old female of Asian ethnicity, with no known co-morbidities, presented to us with complaints of fever, nausea, vomiting, and jaundice. Four days after the primary complaint, she started complaining of generalized abdominal pain with increasing the spikes of fever. She denied any hematemesis, shortness of breath, melena and palmer erythema. Empirically, the patient was started on intravenous ceftriaxone, intravenous proton pump inhibitor, anti-emetic and anti-pyretic for her fever, nausea, vomiting and loose stools. The physical examination was unremarkable except for soft abdomen and mild tenderness present on the right upper quadrant and bowel sounds were increased. Laboratory findings were Hemoglobin: 7.7 g/dl, white cell count: 24.5x109 cells per microliter with differential counts of Neutrophils of 51% and Lymphocytes were 35%, Platelet count: 258x109 per microliter of blood, Urea: 27.4 mg/dl, Creatinine: 0.76 mg/dl, Sodium 131 mEq/Litre, Potassium: 2.7 mEq/Litre , Chloride: 100 mEq/Litre, International Normalization Ratio (INR): 1.6, Total Bilirubin: 36.72 umol/L with Direct bilirubin of 21.87 umol/L and indirect bilirubin of 14.85 umol/L, Alanine amino-transaminase (ALT): 196 U/L, Alkaline Phosphatase (ALP): 242 IU/L. Blood Culture and sensitivity were sent, and the patient was started on potassium supplements and vitamin K injections. The differential considerations included Enteric fever, Malaria, Fulminant Hepatitis, Drug-induced liver toxicity, and viral hepatitis. Ultrasound Abdomen showed mild Hepato-splenomegaly, and swelling of the pancreas with common bile duct dilated without a calculator. Further workup showed raised serum Amylase and Lipase with quantitative values of 642 U/L and 446 U/L respectively, C-Reactive Protein (CRP): 193 mg/L, serum Lactate dehydrogenase 1470 units per liter, serum albumin 3.26 gm/dl, retic count 8.02%, Peripheral smear: microcytic, hypochromic anemia and right-sided neutrophil shift with no malarial parasite seen, Viral markers and Autoimmune profile was negative. Computerized tomography scan of the abdomen showed common bile duct dilatation along with focal enlargement of distal body and tail of pancreas with loss of normal pancreatic clefts with no peripancreatic fat stranding, necrosis or fluid collection (Figure 1, 2). Possibility of pancreatitis concomitant cholangitis was suggested. Meanwhile, Blood culture and sensitivity report confirmed the growth of Salmonella Typhi, hence the final impression of acute pancreatitis with concomitant cholangitis was made as a complication of enteric fever.

Figure 1: Computerized tomography scan of the abdomen showing common bile duct dilatation without calculus.
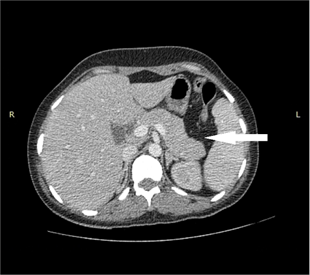
Figure 2: Computerized tomography scan of the abdomen showing focal enlargement of the distal body and tail of the pancreas.
During hospital course, the patient’s antibiotics were shifted to intravenous Meropenem with aggressive intravenous hydration while her deranged liver function enzymes along with serum amylase and lipase were gradually on a decreasing pattern, potassium levels returned to normal after intravenous replacement.
The fever also settled after 7 days of starting antibiotics, and the patient was managed conservatively without opting for Magnetic retrograde cholangiopancreatography (MRCP) or Endoscopic retrograde cholangiopancreatography (ERCP). After completion of antibiotics coarse, the patient was discharged on oral medication with a follow-up in one week in an ambulatory clinic setting. On the follow-up, the patient was Afebrile with no abdominal pain and jaundice clinically improved, along with normal Liver Function Tests, serum Lipase and Amylase.
3. Discussion
Enteric fever is defined as an acute systemic disease is a manifestation of organism Salmonella enterica serotype Typhi which is globally disseminated with an estimated prevalence of 17 million cases and 600,000 casualties [1]. Enteric fever is endemic in areas of the world that are known for poor sanitation, food malpractices and consumption of contaminated water that are Africa, Latin America and Asia (Pakistan and Indian subcontinent) [2]. Typhoid fever presents as sustained fever, headache, and malaise. The severity of the illness has been associated with the virulence of the particular Salmonella typhi strain as well as the immunocompetence, age, and nutritional status of the patient [1]. After the ingestion of Salmonella typhi, approximately 10-20% develop acute diarrhea which lasts for 7-14 days, followed by fever, increasing in a stepwise manner over a 3-5 days period, which is usually higher during the late afternoon. Adults and older children may present with constipation instead of diarrhea. Enteric fever manifests itself with symptomatology divided into intervals of weeks. First-week clinical outcomes are headache, fever, anorexia, nausea, vomiting, abdominal pain and constipation. The second week comprises of rose spots, bradycardia, hepatosplenomegaly, and abdominal tenderness. Complications of enteric fever are prevalent in the third and fourth week, including intestinal perforation [3], pneumonia, ataxia, psychosis, altered consciousness, pancreatitis, cholangitis, cholecystitis and nephritis [4]. On physical examination, findings include the brown coated tongue, hepatosplenomegaly, decreased auditory acuity, nuchal rigidity, confusion, bradycardia, rose spots which are blanching maculopapular lesions 2-4mm usually appearing on the chest and abdomen.
Fever usually persists during the second week of infection and the patient appears significantly ill. Significant gastrointestinal complications related to lymphoid hyperplasia and necrosis especially in the ileocecal area are seen in the third week of the illness, such as bleeding and perforation, the latter being a surgical emergency requiring resection of the affected bowel, supportive care, and broad-spectrum antibiotics, as it can further cause Gram-negative sepsis. Rare complications are cholecystitis, cholangitis, and pancreatitis. Diagnosis of enteric fever is certified by blood culture, urine culture, and stool culture with the most accurate test of bone marrow culture [1]. Enteric fever is to be immediately cured with empiric antibiotics, preferred agents are fluoroquinolones, ciprofloxacin 500 mg twice daily for 7-10 days. Other fluoroquinolones chosen are norfloxacin, ofloxacin, and levofloxacin. An alternative regimen is intravenous ceftriaxone for 14 days rendered safe in children and pregnant women due to cartilage erosion effects of fluoroquinolones [1]. Acute pancreatitis and cholangitis are rare and uncommon complications of enteric fever. Acute pancreatitis and cholangitis complicate enteric fever through the transmission of bacteria by hematogenous and lymphatic spread, by targeted descent of bacteria migrating into pancreatic and common bile duct from the duodenum and biliary tree [5, 6]. Signs and symptoms of acute pancreatitis caused by salmonella typhi are minimal than isolated acute pancreatitis, patients usually are asymptomatic, or complaints of abdominal pain, nausea, vomiting [6, 7]. However, the diagnosis of enteric fever mediated pancreatitis is established on elevated levels of amylase and lipase and computerized tomography scan outcomes [5, 6, 7]. Cholangitis complicating enteric fever manifest itself with high spiking fever, chills, jaundice, purulent bile under high pressure, mental confusion, and hepatic abscess [8]. Diagnosis is verified by leucocytosis, slightly raised alkaline phosphatase and transaminases [9]. Salmonella typhi along with its antimicrobial immune strains has raised alarming concerns worldwide especially in India and Asia [10, 11]. USA based study of resistant strains calculated about 25% strains was resistant to one of the antibiotics while 17% to five or more drugs [1]. R-factor plasmid encrypts for immunization to chloramphenicol, amoxicillin, and trimethoprim sulfamethazine complex. Treatment modalities utilized for acute pancreatitis complicating enteric fever is coverage by broad-spectrum antibiotics that are gentamicin, ampicillin, and metronidazole [11, 12, 13]. Non-pharmacological interventions are rehydration and NG tube placement with intermediate suction [14, 15, 16]. Cholangitis can be cured by the antimicrobial regimen of amikacin, an aminoglycoside [7, 17] while surgical intervention to eradicate microbes is cholecystectomy in carrier patients [18, 19].
4. Conclusion
Our case presents a 25-year-old female, with fever, nausea, vomiting, and jaundice. On examination, there was right upper quadrant tenderness with mild hepato-splenomegaly on ultrasound, the pancreas was swollen
and dilated common bile duct. Laboratory findings were severe hyperbilirubinemia and sepsis, with raised serum Amylase and Lipase, and the patient's blood culture report also turned out to be positive for Salmonella Typhi. The diagnosis of concomitant pancreatitis and cholangitis was made on a background of Salmonella Typhi infection, with sensitivity to Azithromycin and Meropenem only. The outbreak of resistant Salmonella Typhi strains is associated with higher rates of complications. This resistance is acquired through a change in the sequence of the genome [20]. Currently, it is important to control such an unidentified outbreak of multiple drug-resistant Salmonella Typhi strains because it is a serious healthcare issue in disease control and prevention of developing countries.
Disclosure statement
The authors declare no conflicts of interest with this article's content.
Funding statement
This work is not supported by any sponsors. No funding required in this study.
Ethical approval statement
Ethical consent to participate has been taken from the patient in the form of written informed consent.
References
- Crum NF. Current trends in typhoid fever. Current Gastroenterology Reports 5 (2003): 279-286.
- Arif N, Khan AA, Iqbal Z. Hepatic involvement with typhoid fever: a report of nine patients. J Pak Med Assoc 40 (1990): 4-9.
- Pandey A, Gangopadhay AN, Upadhyaya VD. Typhoid Sigmoid Colon Perforation in an 18 month old boy. World J Pediatr 4 (2008): 305-307.
- Meena VK, Kumar N, Nawal R. An unusual presentation of typhoid fever causing aseptic meningitis, acute pancreatitis, acute glomerulonephritis, acute hepatitis. Chin Med J (Engl) 126 (2013): 397-398.
- Pezzilli R, Morselli-Labate AM, Barakat B, Romboli E, Ceciliato R, Piscitelli L, et al. Pancreatic Involvement in Salmonella Infection. J Pancreas (Online) 4 (2003): 200-206.
- Hearne SE, Whigham TE, Brady CE. Pancreatitis and typhoid fever. The American Journal of Medicine 86 (1989): 471-473.
- Cho JH. Successful endoscopic hemoclipping and conservative management for typhoid fever complicated by massive intestinal bleeding and acute pancreatitis: Case report. Medicine (Baltimore) 98 (2019): e16521.
- Wilson OH. PRIMARY TYPHOID CHOLECYSTITIS AND CHOLANGITIS. Journal of the American Medical Association L (1908): 1607-1608.
- Harris AI, Korsten MA. Acute Suppurative Cholangitis Secondary to Calcific Pancreatitis; Gastroenterology 71 (1976): 847-850.
- Elizabeth J Klemm, Sadia Shakoor, Andrew J Page, Farah Naz Qamar, Kim Judge, Dania K Saeed, et al. Emergence of an Extensively Drug-Resistant Salmonella enterica Serovar Typhi Clone Harboring a Promiscuous Plasmid Encoding Resistance to Fluoroquinolones and Third-Generation Cephalosporins. mBio 9 (2018):e00105-e00118.
- Thompson CN, Karkey A, Dongol S, Arjyal A, Wolbers M, Darton T, et al. Treatment Response in Enteric Fever in an Era of Increasing Antimicrobial Resistance: An Individual Patient Data Analysis of 2092 Participants Enrolled into 4 Randomized, Controlled Trials in Nepal. Clin Infect Dis 64 (2017): 1522-1531.
- Hermans P, Gerard M, Laethem YV, De Wit S, Clumeck N. Pancreatic disturbances and typhoid fever. Scandinavian Journal of Infectious Diseases 23 (1991): 201-205.
- Russell IJ, Forgacs P, Geraci JE. Pancreatitis Complicating Typhoid Fever. JAMA 235 (1976): 753-754.
- Andrén-Sandberg A, Höjer H. Necrotizing acute pancreatitis induced by salmonella infection. Int J Pancreatol 15 (1994): 229.
- Sevastos N, Kolokotronis K, Papatheodoridis GV. Acute pancreatitis associated with Salmonella enteritidis. The American Journal of Gastroenterology 96 (2001): 3450-3451.
- Murphy S, Beeching NJ, Rogerson SJ, Harries AD. Pancreatitis associated with Salmonella enteritis. The Lancet 338 (1991): 571.
- Garg P, Parashar S. Pancreatic abscess due to Salmonella typhi. Postgrad Med J 68 (1992): 294-295.
- Hamaguchi H, Okabayashi Y, Yoneda R, Ueno H, Yoon S, Sakaue M, et al. A case of acute pancreatitis complicating salmonella enteritis. International Journal of Pancreatology 26 (1999): 189-192.
- Strand CL, Sanders SL. Salmonella typhimurium pancreatic abscess: report of a case. The American Surgeon 44 (1978): 174-176.
- Elizabeth J Klemm, Sadia Shakoor, Andrew J Page, Farah Naz Qamar, Kim Judge, Dania K Saeed, et al. Emergence of an Extensively Drug-Resistant Salmonella enterica Serovar Typhi Clone Harboring a Promiscuous Plasmid Encoding Resistance to Fluoroquinolones and Third-Generation Cephalosporins. mBio 9 (2018): e00105-e00118.
