Endoscopic Thyroid Lobectomy: Our Early Experience at Lahore General Hospital, Lahore, Pakistan
Article Information
Muhammad Imran Khokhar*, Muhammad Abdulnasir Asghar, Danish Ali, Muhammad Qasim Farooq, Awais Amjad Malik, Suleman Asif, Muhammad Ahsan, Muhammad Farooq Afzal
Department of General Surgery, Surgical Unit 1, Lahore General Hospital, Lahore, Pakistan
*Corresponding author: Muhammad Imran Khokhar, Associate Professor of Surgery, Gujranwala Medical college, DHQ Teaching Hospital, Gujranwala, Pakistan.
Received: 01 November 2021; Accepted: 10 November 2021; Published: 25 November 2021
Citation: Muhammad Imran Khokhar, Muhammad Abdulnasir Asghar, Danish Ali, Muhammad Qasim Farooq, Awais Amjad Malik, Suleman Asif, Muhammad Ahsan, Muhammad Farooq Afzal. Endoscopic thyroid lobectomy: Our early experience at Lahore General Hospital, Lahore, Pakistan. Journal of Surgery and Research 4 (2021): 702-710.
View / Download Pdf Share at FacebookAbstract
Background
Conventional Thyroid Lobectomy leaves an unpleasant neck scar. Endoscopic thyroidectomy was first applied by Huschner in 1997. Amongst the best endoscopic techniques is the one we use, referred to as the endoscopic axillary-breast-shoulder approach (ABSA) innovated by Dr. Trans Ngoc Luong.
Objective
To examine the safety, feasibility and cosmetic outcome of endoscopic thyroid lobectomy.
Patients and Methods
We performed endoscopic lobectomy in 20 patients at Lahore General Hospital (LGH) from 9th September 2016 to 31st Dec 2019. We adopted axillary-breast-shoulder approach. Inclusion criteria were age 18-45 years, solitary nodule less than 5 cm and benign FNAC. Exclusion criteria were multiple nodules, solitary nodule more than 5 cm, age more than 45years, malignant FNAC, recurrent goiter and co-morbid like DM, HTN, IHD, COPD. The parameters studied were the conversion rate, operative time, hospital stay, complications, cosmetic outcome and patient satisfaction. The results were analyzed to draw rational conclusion.
Results
Successful endoscopic lobectomy was performed in almost all cases with conversion to open in two cases. The median operative time was 100 minutes. No preoperative injury was inflicted. One case sustained minor skin burns which healed without any residual scar. One patient developed full thickness skin burn and one patient had seroma. All patients were discharged on first postoperative day. Excellent cosmetic outcome achieved in all patients leading to their optimum satisfaction.
Conclusion
Endoscopic thyroid lobectomy is a safe and feasible procedure with satisfactory cosmetic outcome for benign solitary thyroid nodules in selected patients.
Keywords
Endoscopic, Lobectomy, Technique, Axillary-breast-shoulder, Thyroid surgery
Endoscopic articles; Lobectomy articles; Technique articles; Axillary-breast-shoulder articles; Thyroid surgery articles
Endoscopic articles Endoscopic Research articles Endoscopic review articles Endoscopic PubMed articles Endoscopic PubMed Central articles Endoscopic 2023 articles Endoscopic 2024 articles Endoscopic Scopus articles Endoscopic impact factor journals Endoscopic Scopus journals Endoscopic PubMed journals Endoscopic medical journals Endoscopic free journals Endoscopic best journals Endoscopic top journals Endoscopic free medical journals Endoscopic famous journals Endoscopic Google Scholar indexed journals Lobectomy articles Lobectomy Research articles Lobectomy review articles Lobectomy PubMed articles Lobectomy PubMed Central articles Lobectomy 2023 articles Lobectomy 2024 articles Lobectomy Scopus articles Lobectomy impact factor journals Lobectomy Scopus journals Lobectomy PubMed journals Lobectomy medical journals Lobectomy free journals Lobectomy best journals Lobectomy top journals Lobectomy free medical journals Lobectomy famous journals Lobectomy Google Scholar indexed journals Technique articles Technique Research articles Technique review articles Technique PubMed articles Technique PubMed Central articles Technique 2023 articles Technique 2024 articles Technique Scopus articles Technique impact factor journals Technique Scopus journals Technique PubMed journals Technique medical journals Technique free journals Technique best journals Technique top journals Technique free medical journals Technique famous journals Technique Google Scholar indexed journals Axillary-breast-shoulder articles Axillary-breast-shoulder Research articles Axillary-breast-shoulder review articles Axillary-breast-shoulder PubMed articles Axillary-breast-shoulder PubMed Central articles Axillary-breast-shoulder 2023 articles Axillary-breast-shoulder 2024 articles Axillary-breast-shoulder Scopus articles Axillary-breast-shoulder impact factor journals Axillary-breast-shoulder Scopus journals Axillary-breast-shoulder PubMed journals Axillary-breast-shoulder medical journals Axillary-breast-shoulder free journals Axillary-breast-shoulder best journals Axillary-breast-shoulder top journals Axillary-breast-shoulder free medical journals Axillary-breast-shoulder famous journals Axillary-breast-shoulder Google Scholar indexed journals Thyroid surgery articles Thyroid surgery Research articles Thyroid surgery review articles Thyroid surgery PubMed articles Thyroid surgery PubMed Central articles Thyroid surgery 2023 articles Thyroid surgery 2024 articles Thyroid surgery Scopus articles Thyroid surgery impact factor journals Thyroid surgery Scopus journals Thyroid surgery PubMed journals Thyroid surgery medical journals Thyroid surgery free journals Thyroid surgery best journals Thyroid surgery top journals Thyroid surgery free medical journals Thyroid surgery famous journals Thyroid surgery Google Scholar indexed journals Thyroid nodules articles Thyroid nodules Research articles Thyroid nodules review articles Thyroid nodules PubMed articles Thyroid nodules PubMed Central articles Thyroid nodules 2023 articles Thyroid nodules 2024 articles Thyroid nodules Scopus articles Thyroid nodules impact factor journals Thyroid nodules Scopus journals Thyroid nodules PubMed journals Thyroid nodules medical journals Thyroid nodules free journals Thyroid nodules best journals Thyroid nodules top journals Thyroid nodules free medical journals Thyroid nodules famous journals Thyroid nodules Google Scholar indexed journals Conventional Thyroid Lobectomy articles Conventional Thyroid Lobectomy Research articles Conventional Thyroid Lobectomy review articles Conventional Thyroid Lobectomy PubMed articles Conventional Thyroid Lobectomy PubMed Central articles Conventional Thyroid Lobectomy 2023 articles Conventional Thyroid Lobectomy 2024 articles Conventional Thyroid Lobectomy Scopus articles Conventional Thyroid Lobectomy impact factor journals Conventional Thyroid Lobectomy Scopus journals Conventional Thyroid Lobectomy PubMed journals Conventional Thyroid Lobectomy medical journals Conventional Thyroid Lobectomy free journals Conventional Thyroid Lobectomy best journals Conventional Thyroid Lobectomy top journals Conventional Thyroid Lobectomy free medical journals Conventional Thyroid Lobectomy famous journals Conventional Thyroid Lobectomy Google Scholar indexed journals axillary-breast-shoulder approach articles axillary-breast-shoulder approach Research articles axillary-breast-shoulder approach review articles axillary-breast-shoulder approach PubMed articles axillary-breast-shoulder approach PubMed Central articles axillary-breast-shoulder approach 2023 articles axillary-breast-shoulder approach 2024 articles axillary-breast-shoulder approach Scopus articles axillary-breast-shoulder approach impact factor journals axillary-breast-shoulder approach Scopus journals axillary-breast-shoulder approach PubMed journals axillary-breast-shoulder approach medical journals axillary-breast-shoulder approach free journals axillary-breast-shoulder approach best journals axillary-breast-shoulder approach top journals axillary-breast-shoulder approach free medical journals axillary-breast-shoulder approach famous journals axillary-breast-shoulder approach Google Scholar indexed journals postoperative pain articles postoperative pain Research articles postoperative pain review articles postoperative pain PubMed articles postoperative pain PubMed Central articles postoperative pain 2023 articles postoperative pain 2024 articles postoperative pain Scopus articles postoperative pain impact factor journals postoperative pain Scopus journals postoperative pain PubMed journals postoperative pain medical journals postoperative pain free journals postoperative pain best journals postoperative pain top journals postoperative pain free medical journals postoperative pain famous journals postoperative pain Google Scholar indexed journals
Article Details
1. Introduction
Thyroid nodules are conventionally operated by open technique pioneered by Kocher (Nobel prize in 1909). Due to recent advances in minimal invasive surgery (MIS), scar less neck surgery has been contemplated in different parts of world quite successfully. Learning curve of endoscopic thyroid surgeons has markedly improved during the recent years. Ever since Gagner et al reported an endoscopic approach to parathyroid gland in 1996, several endoscopic techniques for thyroid surgery have been described with the primary aim of obtaining better cosmetic results [1]. New endoscopic approaches are being practiced quite safely and all procedures are concerned about cosmetic results [2-4]. Although the indications for endoscopic thyroidectomy have been expanded extensively, but these procedures are not accepted readily for large benign thyroid lesions (size more than 3-4 cm) and for thyroid cancer [5-8].
In the last decade, endoscopic thyroidectomy has expanded and is being considered as an alternative to conventional thyroidectomy simply because it reduces tissue trauma, postoperative pain, and provides excellent cosmetic results [3]. Endoscopic approach to the thyroid and parathyroid gland may be direct or indirect. The direct approach places the access ports within the cervical region and is considered the least invasive [9-12]. The indirect approach provides access to the neck through a remote site from the target area [13-18]. The lateral neck [19] axillary [20] anterior chest [21] and breast [22] approaches have all been described. The difference between these techniques is only by the site of placement of the access cannula. Postoperatively, there is no visible neck scar with excellent cosmetic results and the return to work is early.
It is worthwhile mentioning the name of Dr Trans Ngoc Luong from Ha Noi, Vietnam, who has innovated a new endoscopic axillary-breast-shoulder approach in 2004. He has operated about 3500 cases at National Endocrine Hospital, Ha Noi, using above mentioned technique [23]. We adopted Dr Luong’s endoscopic axillary-breast-shoulder technique for thyroid surgery at Lahore General Hospital, Lahore. We would like to share our experience of this new technique.
2. Patients and Methods
This prospective study was conducted in 20 patients at Lahore General Hospital (LGH) from 9th September 2016 to 31st December 2019. The patients included in our study were 18-45 years of age, having unilateral solitary thyroid nodule less than 5 cm, with benign FNAC. The patients more than 45 years, recurrent goiter, nodules more than 5 cm, malignant FNAC and co-morbid (HTN, IHD, COPD) were excluded from our study.
Operative technique
All of our patients were operated under general anesthesia. We adopted Dr Luong’s Lateral approach for endoscopic thyroid lobectomy. One 10 mm trocar was inserted through axilla, one 5mm trocar inserted through areola and another 5mm trocar inserted close to shoulder tip (2.5cm below the lateral end of clavicle) (Figure 2). CO2 insufflation maintaining pressure of 8-10 mm Hg was used during the procedure. Subcutaneous space over pectoralis major was created with the use of monopolar diathermy to reach suprasternal notch. From here onward space was created between strap muscles and platysma to reach thyroid cartilage. Sternocleidomastoid muscle dissected away from strap muscles up to superior belly of omohyoid. Sternothyroid muscle split along the fibers laterally and thyroid lobe was manipulated out with blunt dissection. With the help of harmonic scalpel inferior and superior poles dissected and lobectomy done making sure to preserve recurrent laryngeal nerve, external branch of superior laryngeal nerve, parathyroid glands and other adjacent structures (Figure 3). Haemostasias secured and specimen retrieved in Endo bag through the axillary port site making sure to avoid any spillage (Figures 4,5). Suction drain no. 14 placed in the neck through the axillary port site after thorough irrigation of area with saline. Port sites stitched and dressed.
Parameters measured
The parameters monitored in our operated patients were operative time, complications, hospital stay, cosmetic outcome and patient’s satisfaction. Cosmetic outcome was graded as poor, average or excellent. Patients were inquired whether they were fully satisfied, just satisfied or not satisfied at all. Results were analyzed and rational conclusion drawn.
3. Results
In our short series of 20 cases, all were females with age range from 18 to 45 years and median age 26 years. All were free from any chronic co-morbidity like HTN, DM, IHD etc. 13 patients underwent right thyroid lobectomy and in 7 cases left sided lobectomy was performed. Nodule size was less than 5 cm with mean size 3.4 cm. FNAC for all nodules was benign. All patients were successfully operated with conversion of two patients to open surgery. The operative time for initial two cases was about 160 minutes but in the last two cases it reduced to less than 90 minutes with the median operative time of about 110 minutes (Table 1). No patient had iatrogenic injury to recurrent laryngeal nerve, external branch of superior laryngeal nerve, parathyroid gland, trachea or esophagus. Per operative bleeding was encountered in one patient from dilated veins on the surface of thyroid and we had to covert to open surgery. One of our cases suffered minor skin burn that healed within two weeks of follow up without any residual scar (Table 2). Average postoperative drainage was 20 ml. Drain was removed on 1st post operative day and all patients discharged. One patient developed full thickness burn and it was excised with primary closure using 4/0 prolene. One patient developed post operative seroma during follow up which recovered spontaneously. No patient developed hoarseness, hematoma, hypocalcemia or port site infection during follow up. All patients were fully satisfied and cosmetic outcome was excellent (Table 3).
|
Parameters |
Values |
|
No. of patients |
20 |
|
M/F ratio |
0/20 |
|
Mean age(years) |
26 |
|
Side (Right/Left) |
13/6 |
|
Nodule size(cm) |
3.4 |
|
Conversion to open surgery |
2 |
|
Median operative time(minutes) |
110 |
|
Average hospital stays(hours) |
36 |
Table 1: Parameters relating to patients under study.
|
Injury to RLN |
0 |
|
Injury to superior laryngeal nerve (ext. branch) |
0 |
|
Injury to parathyroid gland |
0 |
|
Injury to Trachea/esophagus |
0 |
|
Mean perioperative bleeding(ml) |
20 |
|
Minor skin burns |
1 |
|
Full thickness skin burns |
1 |
Table 2: Per-operative complications.
|
Hoarseness |
0 |
|
Hematoma |
0 |
|
Post operative seroma |
1 |
|
Hypocalcemia |
0 |
|
Wound infection |
0 |
|
Hypothyroidism |
0 |
Table 3: Postoperative Complications.
4. Discussion
Keeping in view the deep cosmetic concern of large majority of thyroid patients especially females, we conducted this study in our hospital to assess the feasibility and safety of endoscopic approach. We operated all of our patients with Dr Tran Ngoc Luong’s endoscopic technique using axillary-breast-shoulder approach. We found this approach to be very practical, feasible and safe. Our study has been quite encouraging as the results of our study are very much comparable with the international literature. Our learning curve of endoscopic procedure improved enormously during the study. Our operative time was quite prolonged in initial two cases (approx. 160 minutes each) due to poor logistics and untrained staff. Now operative time is reduced to less than 90minutes due to better logistics and improved learning curve of the surgeons and staff. No injury was inflicted to the adjacent structures (recurrent laryngeal nerve, external branch of superior laryngeal nerve, parathyroid glands, esophagus, trachea and any major vessels) during surgery except minor skin burns in one patient. Avoidance of injury to these structures has been possible because of improved endoscopic visualization of above-mentioned structures. This patient had minor burn due to strong camera light in early cases of our study. We have been able to avoid this complication in the later part of our study by lowering the intensity of camera light, using 30-degree scope to avoid continuous exposure of skin by changing the direction of scope and continuously putting saline socked gauze over the skin. This burn healed without any residual scar within two weeks’ time. One patient developed full thickness diathermy burn that was excised and subcuticular stitches were applied using 4/0 prolene. Only one patient developed postoperative seroma which was managed conservatively on OPD basis. No patient developed hematoma in our study possibly because of immaculate hemostasis during dissection. We used three doses of I.V second generation cephalosporin, prophylactically. By using the lateral approach, Palazzo et al. [24] have removed nodules of mean size 22 mm (range 2-47 mm), while our mean nodule size is 34 mm. The conversion rate in our early study has been 13% that is comparable to 0-13% mentioned in international literature where conversion was mostly due to malignant histological result, bleeding, difficult dissection and large nodule size [25]. Miccoliet al. [26] have reported recurrent nerve palsy in eight cases (2.1%) and eleven patients exhibited hypoparathyroidism, of which only two had permanent hypocalcemia (1.8%). In our study, all cases, the recurrent laryngeal nerve was identified and preserved intact. The superior and inferior parathyroid were identified and preserved. Cosmetic outcome was excellent in all of our patients and all were fully satisfied regarding the surgery (Figure 1). We as surgeons found this procedure safe and feasible but has a learning curve.

Figure 1: Preop nodule and postop scarless neck

Figure 2: Port sites
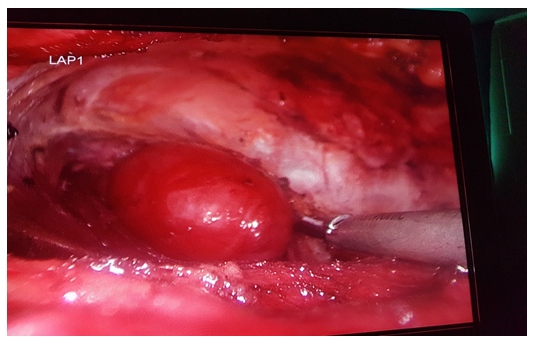
Figure 3: Perop dissection

Figure 4: Retrieval of specimen
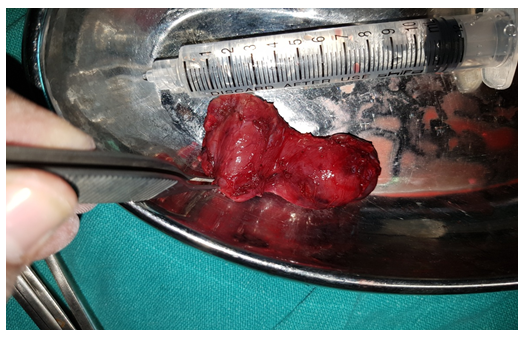
Figure 5: Retrieved specimen
5. Conclusion
Our early experience at Lahore General Hospital, Lahore proved that endoscopic thyroid lobectomy is a reasonably safe and feasible procedure with satisfactory cosmetic outcome. This technique can be practiced safely in carefully selected patients.
Acknowlwdgements
The authors gratefully acknowledge Dr Tran Ngoc Luong for his valuable contributions.
References
- Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg. 12 (1996): 83:875.
- Koh YW, Park JH, Kim JW, Lee SW, Choi EC. Endoscopic hemithyroidectomy with prophylactic ipsilateral central neck dissection via an unilateral axillo-breast approach without gas insufflation for unilateral micropapillary thyroid carcinoma: preliminary report. Surg Endosc 24 (2010): 188-197.
- Ikeda Y, Takami H, Sasaki Y, Takayama J, Kurihara H. Are there significant benefits of minimally invasive endoscopic thyroidectomy? World J Surg 28 (2004): 1075-1078.
- Kang SW, Jeong JJ, Yun JS, et al. Robot-assisted endoscopic surgery for thyroid cancer: experience with the first 100 patients. Surg Endosc 23 (2009): 2399-2406.
- Hüscher CS, Chiodini S, Napolitano C, et al. Endoscopic right thyroid lobectomy. Surg Endosc 11 (1997): 877.
- Shimizu K, Akira S, Jasmi AY, et al. Video-assisted neck surgery: endoscopic resection of thyroid tumors with a very minimal neck wound. J Am Coll Surg 188 (1999): 697-703.
- Jeong JJ, Kang SW, Yun JS, Sung TY, Lee SC, Lee YS, et al. Comparative study of endoscopic thyroidectomy versus conventional open thyroidectomy in papillary thyroid microcarcinoma (PTMC) patients. J Surg Oncol 100 (2009): 477-480.
- Gagner M, Inabnet WB. 3rd Endoscopic thyroidectomy for solitary thyroid nodules. Thyroid 11 (2001): 161-163.
- Inabnet WB, Chu CA. Transcervical endoscopic-assisted mediastinal parathyroidectomy with intraoperative parathyroid hormone monitoring. Surg Endosc 17 (2003): 16-78.
- Miccoli P, Bendinelli C, Conte M, et al. Endoscopic parathyroidectomy by a gasless approach. J Laparoendosc Adv Surg Tech A 8 (1998): 189-194.
- Miccoli P, Bendinelli C, Vignali E, et al. Endoscopic parathyroidectomy: report of an initial experience. Surgery 124 (1998): 1077-1079.
- Naitoh T, Gagner M, Garcia-Ruiz A, et al. Endoscopic endocrine surgery in the neck. An initial report of endoscopic subtotal parathyroidectomy. SurgEndosc 12 (1998): 202-205.
- Ng WT. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 10 (2008): 339-340.
- Ohgami M, Ishii S, Arisawa Y, et al. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 10 (2000): 1- 4.
- Ikeda Y, Takami H, Niimi M, et al. Endoscopic thyroidectomy by the axillary approach. SurgEndosc 15 (2001): 1362-1364.
- Ikeda Y, Takami H, Niimi M, et al. Endoscopic thyroidectomy and parathyroidectomy by the axillary approach. A preliminary report. SurgEndosc 16 (2002): 92-95.
- Ikeda Y, Takami H, Niimi M, et al. Endoscopic total parathyroidectomy by the anterior chest approach for renal hyper-parathyroidism. Surg Endosc 16 (2002): 320-322.
- Chantawibul S, Lokechareonlarp S, Pokawatana C. Total video endoscopic thyroidectomy by an axillary approach. J Laparoendosc Adv Surg Tech A 13 (2003): 295-299.
- Inabnet WB III, Gagner M. Endoscopic thyroidectomy. J Otolaryngol 30 (2001): 41-42.
- Ikeda Y, Takami H, Sasaki Y, et al. Endoscopic neck surgery by the axillary approach. J Am Coll Surg 191 (2000): 336-340.
- Takami H, Ikeda Y. Minimally invasive thyroidectomy. Aust NZ J Surg 72 (2002): 841-842.
- Ohgami M, Ishii S, Arisawa Y. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 10 (2000): 1-4.
- Ngoc Luong T. Open and Endoscopic Thyroidectomy (2009).
- Palazzo FF, Sebag F, Henry JF. Endocrine surgical technique: Endoscopic thyroidectomy via the lateral approach. Surg Endosc 20 (2006): 339-342
- EunLeeK, RAo J, KyuYoun Y, et al.Endoscopic Thyroidectomy with the da-Vinci Robot System using the BABA technique-our Initial Experience. Surg Laprosc. Endosc & Percutan Tech 19 (2009): e71-75
- Miccoli P, Bellantone R, Mourad M, et al. Minimally invasive video-assisted thyroidectomy: multi-institutional experience. World J Surg 26 (2002): 972- 978.
