Endoscopic Assisted Unilateral Transpedicular Microdiscectomy for a Patient of Thoracic Disc Herniation with Paraplegia
Article Information
Moshiur Rahman1*, Khairun Nabi Khan SIM2, Robert Ahmed Khan2, Mainul Haque Sarker1, Luis Rafael Moscote-Salazar3
1Department of Neurosurgery, Holy Family Red Crescent Medical College, Dhaka, Bangladesh
2Neurosurgery Department, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
3Center for Biomedical Research (CIB), Faculty of Medicine, University of Cartagena, Cartagena, Colombia
*Corresponding Author: Dr. Md Moshiur Rahman, Neurosurgery Department, Holy Family Red Crescent Medical College, 1 Eskaton Garden Rd, Dhaka 1000, Bangladesh
Received: 09 July 2020; Accepted: 18 September 2020; Published: 06 November 2020
Citation: Moshiur Rahman, Khairun Nabi Khan SIM, Robert Ahmed Khan, Mainul Haque Sarker, Luis Rafael Moscote-Salazar. Endoscopic Assisted Unilateral Transpedicular Microdiscectomy for a Patient of Thoracic Disc Herniation with Paraplegia. Archives of Clinical and Medical Case Reports 4 (2020): 1044-1051.
View / Download Pdf Share at FacebookAbstract
Background: Disc herniation of the thoracic spine is a rare lesion that is believed to occur in 1 in 1000 to 1 in 1,000,000 patients each year. Endoscopic-assisted thoracic disc microdiscectomy is a safe and effective surgical removal technique for intervertebral herniated thoracic discs.
Case Presentation: A 48-year-old female was presented with progressive weakness in both lower limbs for three months, incapacity to void urine for 2 weeks. She had back pain and neck pain for 5 years. Clinically, she was diagnosed with paraplegia at stage D6/7 as a case of dorsal disc prolapse. After doing unilateral transpedicular microscopic discectomy she recovered over 4 weeks and her muscle strength was 4/5 in the lower limbs, and she was able to walk.
Conclusion: Thoracic disc herniations are relatively uncommon compared with lumbar and cervical disc pathologies. Although it has posed significant problems for spinal surgeons, the adoption of minimally invasive thoracic disc resection procedures may result in decreased operating time, reduced blood loss, and faster patient recovery.
Keywords
Microdiscectomy; Disc Herniation; Paraplegia
Microdiscectomy articles, Disc Herniation articles, Paraplegia articles
Microdiscectomy articles Microdiscectomy Research articles Microdiscectomy review articles Microdiscectomy PubMed articles Microdiscectomy PubMed Central articles Microdiscectomy 2023 articles Microdiscectomy 2024 articles Microdiscectomy Scopus articles Microdiscectomy impact factor journals Microdiscectomy Scopus journals Microdiscectomy PubMed journals Microdiscectomy medical journals Microdiscectomy free journals Microdiscectomy best journals Microdiscectomy top journals Microdiscectomy free medical journals Microdiscectomy famous journals Microdiscectomy Google Scholar indexed journals Disc Herniation articles Disc Herniation Research articles Disc Herniation review articles Disc Herniation PubMed articles Disc Herniation PubMed Central articles Disc Herniation 2023 articles Disc Herniation 2024 articles Disc Herniation Scopus articles Disc Herniation impact factor journals Disc Herniation Scopus journals Disc Herniation PubMed journals Disc Herniation medical journals Disc Herniation free journals Disc Herniation best journals Disc Herniation top journals Disc Herniation free medical journals Disc Herniation famous journals Disc Herniation Google Scholar indexed journals Paraplegia articles Paraplegia Research articles Paraplegia review articles Paraplegia PubMed articles Paraplegia PubMed Central articles Paraplegia 2023 articles Paraplegia 2024 articles Paraplegia Scopus articles Paraplegia impact factor journals Paraplegia Scopus journals Paraplegia PubMed journals Paraplegia medical journals Paraplegia free journals Paraplegia best journals Paraplegia top journals Paraplegia free medical journals Paraplegia famous journals Paraplegia Google Scholar indexed journals pyrexia articles pyrexia Research articles pyrexia review articles pyrexia PubMed articles pyrexia PubMed Central articles pyrexia 2023 articles pyrexia 2024 articles pyrexia Scopus articles pyrexia impact factor journals pyrexia Scopus journals pyrexia PubMed journals pyrexia medical journals pyrexia free journals pyrexia best journals pyrexia top journals pyrexia free medical journals pyrexia famous journals pyrexia Google Scholar indexed journals Thoracic disc articles Thoracic disc Research articles Thoracic disc review articles Thoracic disc PubMed articles Thoracic disc PubMed Central articles Thoracic disc 2023 articles Thoracic disc 2024 articles Thoracic disc Scopus articles Thoracic disc impact factor journals Thoracic disc Scopus journals Thoracic disc PubMed journals Thoracic disc medical journals Thoracic disc free journals Thoracic disc best journals Thoracic disc top journals Thoracic disc free medical journals Thoracic disc famous journals Thoracic disc Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Retinal detachment articles Retinal detachment Research articles Retinal detachment review articles Retinal detachment PubMed articles Retinal detachment PubMed Central articles Retinal detachment 2023 articles Retinal detachment 2024 articles Retinal detachment Scopus articles Retinal detachment impact factor journals Retinal detachment Scopus journals Retinal detachment PubMed journals Retinal detachment medical journals Retinal detachment free journals Retinal detachment best journals Retinal detachment top journals Retinal detachment free medical journals Retinal detachment famous journals Retinal detachment Google Scholar indexed journals abdominal articles abdominal Research articles abdominal review articles abdominal PubMed articles abdominal PubMed Central articles abdominal 2023 articles abdominal 2024 articles abdominal Scopus articles abdominal impact factor journals abdominal Scopus journals abdominal PubMed journals abdominal medical journals abdominal free journals abdominal best journals abdominal top journals abdominal free medical journals abdominal famous journals abdominal Google Scholar indexed journals
Article Details
1. Introduction
Compared to lumbar and cervical disc pathologies, thoracic disc bulgings/herniations are fairly rare. It is estimated that only 0.25 to 1% of all disc herniations occur in the thoracic region [1]. Although rare, accurate diagnosis of thoracic disease, especially thoracic disc herniation, can be difficult because it can resemble many medical conditions and is often misdiagnosed as cardiac, abdominal, gastrointestinal, neoplastic, or demyelinatal [2]. Dorsalgia of progressive onset that follows any degree of myelopathy or sensory defects in thoracic disc herniation and can reach debilitating levels [3]. The surgical indication is determined when the patient has functional symptoms that do not lead to medical care and/or when neurological symptoms occur or worsen. The key clinical symptom is pain (intercostal neuralgia, back pain) that is present in 92% of cases. In the Quint report, 60% of 168 patients had neurological deficits [4]. It may be either sensory or motor disorders with a lesional syndrome (intercostal or abdominal radicular pain) or with a sub-lesional neurological condition in the form of sluggish medullary compression. A few rare cases of temporary or permanent paraplegia caused by central hernia occlusion of the anterior spinal artery have been reported [5]. Transpedicular approach can be an efficient and safe form of surgical decompression in patients carefully chosen. There are drawbacks to the unilateral transpedicular method for thoracic disc herniation. Disc at midline or midline crossing is an obstacle to this practice. Endoscopic-assisted microdiscectomy or pure endoscopic is also a choice for visualizing and extracting from the opposite side the disc/calcified material under direct vision. The goal is to determine the protection of endoscopic assisted thoracic disc microdiscectomy in a paraplegic patient. In January 2019, this retrospective analysis of one patient was carried out at a private hospital (Comfort Hospital), Dhaka, Bangladesh.
2. Case Report
A 48 years female presented with gradual weakness in both lower limbs for three months with unable to void urine for 2 weeks, the patient had back pain and neck pain for 5 years. She was treated by a physician and initially diagnosed with transverse myelitis. Her CSF study revealed normal findings. As there was no improvement of symptoms they wanted a consultation from neurological aspects. Then she was examined carefully and found a sensory level of D8 and joint position sense was absent on both lower limbs. Motor power was grade 3 in lower limbs. There were increased knee and ankle jerks with patellar clonus and bilateral extensor plantar response. She was catheterized and there was perianal numbness (symmetrical). Her upper limb examination revealed no abnormality. She had no history of trauma, infection, or tumor surgery. MRI Dorsal Spine revealed dorsal 6/7 level disc herniation with spinal cord compression. (Figure 1A and 1C) CT dorsal spine revealed no abnormalities/calcification. (Figure 1B). Clinically, she was diagnosed as a case of dorsal disc prolapse at D6/7 level with paraplegia.
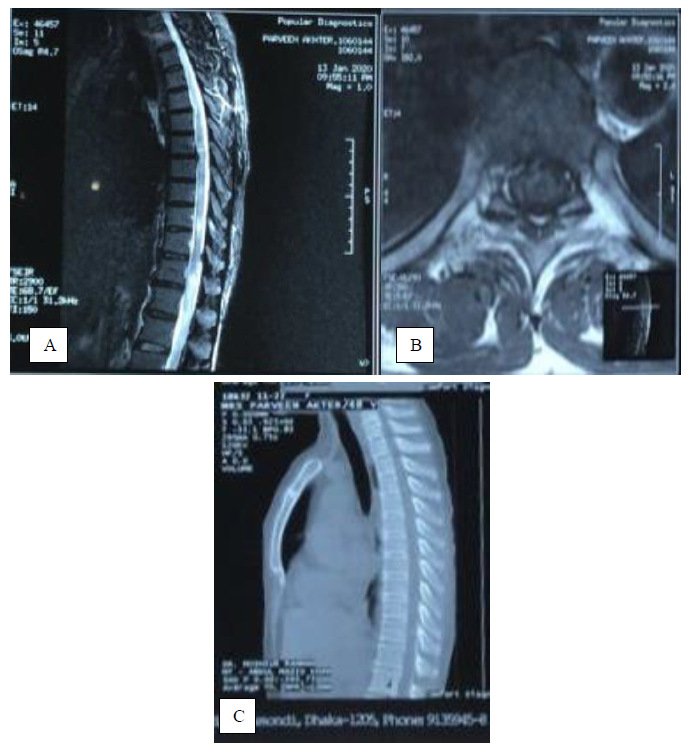
Figure 1: (A, B) MRI dorsal spine showing dosal 6/7 disc herniation with spinal cord compression; (C) CT dorsal spine showing no abnormalities.
2.1 Operative procedure
A 3 cm paramedian linear incision was made about 3 cm lateral to the midline on left D6/7 level under C-arm. Skin, subcutaneous tissue, deep fascia, were cut, paraspinal muscles were detached and retracted by Caspar retractor. The high-speed drill was used to make a hole inside the pedicle of the dorsal 7 vertebral body. It was then enlarged and with the help of micro curette and micro rontgers and endplate were palpated and breached under operating neuro microscope and further enlargement of the hole was made; through the 5 mm hole disc was then removed and posterior longitudinal ligament was cut through karrison punch. Under the direct microscopic vision, the disc was then removed gradually and the dura mater was seen along with spinal cord pulsation. The 30-degree endoscope was used to check for disc under the thecal sac. The posterior longitudinal ligament was cut and discectomy crossing the midline which was confirmed by C-arm in antero-posterior view. CSF leak was checked by doing the Valsalva maneuver. A subcutaneous free fat graft was then taken to fill up the hole. Wound closed in layers keeping a closed drain in situ. The postoperative period was uneventful and the patient was static. Over 4 weeks she recovered and her muscle power was 4/5 in lower limbs and was able to walk. She was able to void urine without any difficulty and PVR (post-void residual) on Ultrasonography on 4 weeks follow up was 35 ml.
3. Discussion
Several surgical procedures and various methods have been developed for treating thoracic disc herniation. It has been surgically treated with thoracotomy, posterolateral extracavitary, costotransversectomy, and transpedicular approaches [6-11]. These surgical approaches have produced similar surgical results, preventing severe damage to the spinal cord that has typically occurred with a laminectomy approach [12]. Unilateral transpedicular microscopic discectomy provides access to a minimally invasive posterolateral muscle-splitting procedure that does not damage the contents of the thoracic cavity. This procedure is effective in the thoracic spine, with shorter hospital stay, less postoperative discomfort, reduced blood loss, and shorter recovery times. The thoracic spine with appropriate patient range and correct surgical procedure should predict these same advantages.
Symptomatic herniation of thoracic discs is a rare occurrence. Although the recorded incidence of symptomatic thoracic disc herniations is relatively low, it is estimated that asymptomatic thoracic disc protrusions are as high as 37% [13]. Asymptomatic herniations of thoracic discs are mistakenly diagnosed with MRI. Although thoracic disc herniations have been thought to be relatively uncommon until recently, more cases are being identified with enhanced imaging techniques, including MRI [14]. Degenerative changes in the disc are an important cause of thoracic disc prolapse.
Microendoscopic thoracic discectomy was reported by Perez-Cruet and colleagues in 2004 [15]. Their study presented findings in 7 patients with 9 thoracic discs extracted using a 30 microendoscope. An incision was made from the midline 3 to 4 cm, and the tubular dilators were centered at the level of the herniated disc on the superior aspect of the caudal transverse process. Passed via the microendoscope and attached to the final tubular retractor. In their 2006 study, Eichholz and colleagues found this technique to have fewer incisions and less tissue disturbance than the conventional lateral extracavitary method for thoracic disc herniation [16]. Khoo and colleagues identified 13 patients with minimally invasive lateral extracavitary microscopically assisted approaches [17].
Thoracic discectomy usually has a complication rate of 20% to 30%. Some authors found that because of the lower complication rate for thoracic discectomy, where there is a choice to choose between an anterior or posterior approach, the posterior approach is preferred. A meta-analysis of 545 patients undergoing thoracic discectomy found a complication rate of 24%, including lung complications of 6% and intercostal neuralgia of 6% [18]. Some complications were recorded by McAfee et al. in video-assisted thoracic surgery [19]. Such was intercostal neuralgia (8%) and atelectasis (6%). Mayer has described the thoracic disc herniation approach to mini-thoracotomy. These techniques were then improved by using a mini-thoracotomy supported microscope, which was recorded in the surgical microscope [20]. A report observed thoracotomy-related risks with 30-day mortality range from 3 to 30% in patients with metastases and this has contributed to the development of alternative posterolateral techniques [21-28]. Several authors have identified strategies for spinal metastasis resection not involving a transcavitary approach [29-35].
Costotransversectomy was first identified in 1894 by Menard for the drainage of tuberculous abscesses in patients with Pott paraplegia [36]. Various modifications of this procedure for removing anterior thoracic have been created. While patients diagnosed with costotransversectomy had a substantially higher rate of comorbidities, its perioperative complications were very similar to those in which thoracolumbar approaches were performed.
In the late 1960s, the Transthoracic method improved [10]. Thoracotomy morbidities contributed to the development of thoracoscopic techniques [37]. Surgeons have resisted anterior and/or lateral thoracotomic approaches due to a need for a multidisciplinary approach. Subsequent treatments were more widely used for symptomatic disc herniations of the spine thoracic segment [38].
The benefit of the surgical microscope was a direct visualization of thoracic disc herniation, and a high-speed burr was used for decompression of the spinal canal to visualize the spinal cord 5-6 mm long. The natural history of thoracic disc herniations remains uncertain. The minimally invasive thoracic microdiscectomy technique is a viable option that avoids substantial muscle and ligament dissection, minimizes unnecessary retraction of critical anatomical structures, decreases bone resection, minimizes blood loss, avoids iatrogenic instability and removes the use of fusion or instrumentation. To order to better grasp the reasons behind the creation and use of this technique, one needs to have an understanding of the history of thoracic disc herniation surgical treatment. We used this secure technique to enhance three-dimensional surgical visualization, promote clinical teaching for assistant surgeons, and reduce the learning curve. For the operator who is not familiar with endoscopic spinal surgery, the experience is important to obtain the requisite hand-to-eye coordination.
4. Conclusion
Symptomatic thoracic disc herniation is rare and can present very differently, with the most feared neurological deficits. Through expanded usage and advancement of minimally invasive procedures, spine surgeons can easily remove offending thoracic disc herniations with less morbidity than conventional procedures. Surgery is complicated and full of risks for that. Adoption of minimally invasive thoracic disc resection procedures will lead to decreased operating time, lower blood loss, and faster recovery of patients. We believe that further advances in instruments and developments in endoscopically controlled techniques are likely to increase this procedure's effectiveness, safety, and popularity.
Conflict of Interest
There is no potential conflict of interest relevant to this case report.
Financial Disclosure
No funding was provided for this case report.
Patient Consent
This study obtained patient consent directly from the patient.
Author’s Contributions
The author's contributions include manuscript preparation and editing. The manuscript has been prepared and approved by all the authors to be submitted and published.
Acknowledgement
The principal author is grateful to Dr. Paulo Pereira for his kind help to prepare the case report and also like to express his gratitude to Dr. Luis Rafael for his inspiration and motivation.
References
- McInerney J, Ball PA. The pathophysiology of thoracic disc disease. Neurosurg Focus 9 (2000): 1.
- Linscott MS, Heyborne R. Thoracic intervertebral disk herniation: a commonly missed diagnosis. J Emerg Med 32 (2007): 235-238.
- Cornips EM, Janssen ML, Beuls EA. Thoracic disc herniation and acute myelopathy: clinical presentation, neuroimaging findings, surgical considerations, and outcome. J Neurosurg Spine 14 (2011): 520-528.
- Quint U, Bordon G, Preissl I, et al. Thoracoscopic treatment for single level symptomatic thoracic disc herniation: a prospective followed cohort study in a group of 167 consecutive cases. Eur Spine J 21 (2012): 637-645.
- Guest JD, Griesdale DE, Marotta T. Thoracic disc herniation presenting with transient anterior spinal artery syndrome. A case report. Interv Neuroradiol [Internet] 6 (2000): 327-331.
- Hulme A. The surgical approach to thoracic intervertebral disc protrusions. J Neurol Neurosurg Psychiatry 23 (1960): 133-137.
- Larson SJ, Holst RA, Hemmy DC, et al. Lateral extracavitary approach to traumatic lesions of the thoracic and lumbar spine. J Neurosurg 45 (1976): 628-637.
- Le Roux PD, Haglund MM, Harris AB, et al. Thoracic disc disease: experience with the transpedicular approach in twenty consecutive patients. Neurosurgery 33 (1993): 58-66.
- Patterson RH Jr, Arbit E. A surgical approach through the pedicle to protruded thoracic discs. J Neurosurg 48 (1978): 768-772.
- Perot PL Jr, Munro DD. Transthoracic removal of midline thoracic disc protrusions causing spinal cord compression. J Neurosurg 31 (1969): 452-458.
- Rosenthal D, Rosenthal R, de Simone A. Removal of a protruded thoracic disc using microsurgical endoscopy. A new technique. Spine 19 (1994): 1087-1091.
- Arseni C, Nash F. Thoracic intervertebral disc protrusion. A clinical study. J Neurosurg 17 (1960): 418-430.
- Wood KB, Garvey TA, Goundry C, et al. Thoracic MRI evaluation of asymtomatic individuals. J Bone Joint Surg Am 77 (1995): 1634-1638.
- Rosenbloom SA. Thoracic disc disease and stenosis. Radiol Clin North Am 29 (1991): 765-775.
- Perez-Cruet MJ, Kim BS, Sandhu F, et al. Thoracic microendoscopic discectomy. J Neurosurg Spine 1 (2004): 58-63.
- Eichholz KM, O’Toole JE, Fessler RG. Thoracic microendoscopic discectomy. Neurosurg Clin N Am 17 (2006): 441-446.
- Khoo LT, Smith ZA, Asgarzadie F, et al. Minimally invasive extracavitary approach for thoracic discectomy and interbody fusion: 1-year clinical and radiographic outcomes in 13 patients compared with a cohort of traditional anterior transthoracic approaches. J Neurosurg Spine 14 (2011): 250-260.
- Elhadi AM, Zehri AH, Zaidi HA, et al. Surgical efficacy of minimally invasive thoracic discectomy. J Clin Neurosci 22 (2015): 1708-1713.
- McAfee PC, Regan JR, Zdeblick T, et al. The incidence of complications in endoscopic anterior thoracolumbar spinal reconstructive surgery: a prospective multicenter study comprising the first 100 consecutive cases. Spine 20 (1995): 1624-1632.
- Mayer HM. Microsurgical anterior approach to T5-T10 (Mini-TTA). In Ed.: Mayer HM. Minimally Invasive Spine Surgery. Springer (2006): 129-137.
- Gokaslan ZL, York JE, Walsh GL, et al. Transthoracic vertebrectomy for metastatic spinal tumors. J Neurosurg 89 (1998): 599-609.
- Hall DJ, Webb JK. Anterior plate fixation in spine tumor surgery. Indications, technique, and results. Spine 16 (1991): 80-83.
- Hosono N, Yonenobu K, Fuji T, et al. Vertebral body replacement with a ceramic prosthesis for metastatic spinal tumors. Spine 20 (1995): 2454-2462.
- Moore AJ, Uttley D. Anterior decompression and stabilization of the spine in malignant disease. Neurosurgery 24 (1989): 713-717.
- Obbens EA, Kim JH, Thaler H, et al. Metronidazole as a radiation enhancer in the treatment of metastatic epidural spinal cord compression. J Neurooncol 2 (1984): 99-104.
- Siegal T, Siegal T. Surgical decompression of anterior and posterior malignant epidural tumors compressing the spinal cord: a prospective study. Neurosurgery 17 (1985): 424-432.
- Sundaresan N, Digiacinto GV, Hughes JE, et al. Treatment of neoplastic spinal cord compression: results of a prospective study. Neurosurgery 29 (1991): 645-650.
- Sundaresan N, Galicich JH, Lane JM, et al. Treatment of neoplastic epidural cord compression by vertebral body resection and stabilization. J Neurosurg 63 (1985): 676-684.
- Bridwell KH, Jenny AB, Saul T, et al. Posterior segmental spinal instrumentation (PSSI) with posterolateral decompression and debulking for metastatic thoracic and lumbar spine disease. Limitations of the technique. Spine 13 (1988): 1383-1394.
- Cybulski GR, Stone JL, Opesanmi O. Spinal cord decompression via a modified costotransversectomy approach combined with posterior instrumentation for management of metastatic neoplasms of the thoracic spine. Surg Neurol 35 (1991): 280-285.
- Faccioli F, Lima J, Bricolo A. One-stage decompression and stabilization in the treatment of spinal tumors. J Neurosurg Sci 29 (1985): 199-205.
- Jelsma RK, Kirsch PT. The treatment of malignancy of a vertebral body. Surg Neurol 13 (1980): 189-195.
- Johnston FG, Uttley D, Marsh HT. Synchronous vertebral decompression and posterior stabilization in the treatment of spinal malignancy. Neurosurgery 25 (1989): 872-876.
- Magerl F, Coscia MF. Total posterior vertebrectomy of the thoracic or lumbar spine. Clin Orthop (1988): 62-69.
- Perrin RG, McBroom RJ. Anterior versus posterior decompression for symptomatic spinal metastasis. Can J Neurol Sci 14 (1987): 75-80.
- Menard V. Causes de la paraplégie dans le mal de Pott, son traitement chirurgical par l'ouverture directe du foyer tuberculeux des vertebres. Rev Orthop 5 (1894): 47-64.
- Oskouian Jr RJ, Johnson JP, Regan JJ. Thoracoscopic microdiscectomy. Neurosurgery 50 (2002): 103-109.
- Yoshihara H, Yoneoka D. Comparison of in-hospital morbidity and mortality rates between anterior and nonanterior approach procedures for thoracic disc herniation. Spine 39 (2014): 728-733.
