Encephalocraniocutaneous Lipomatosis (Haberland Syndrome) with Atrial Tachycardia in a Neonate: A Rare Case Report
Article Information
Kumari Naina1*, Aditi Baruah2, Bipul Kumar Das1
1Post Graduate trainee, Department of Paediatrics, Assam Medical College and Hospital, Assam, India
2Associate Professor, Department of Paediatrics, Assam Medical College and Hospital, Assam, India
*Corresponding Author: Kumari Naina, Post Graduate trainee, Department of Paediatrics, Assam Medical College and Hospital, Dibrugarh, Assam, India
Received: 22 June 2021; Accepted: 29 June 2021; Published: 05 July 2021
Citation:
Kumari Naina, Aditi Baruah, Bipul Kumar Das. Encephalocraniocutaneous Lipomatosis (Haberland Syndrome) with Atrial Tachycardia in a Neonate: A Rare Case Report. Journal of Pediatrics, Perinatology and Child Health 5 (2021): 136-141.
View / Download Pdf Share at FacebookKeywords
Encephalocraniocutaneous Lipomatosis, Neonate, Atrial Tachycardia
Encephalocraniocutaneous Lipomatosis articles; Neonate articles; Atrial Tachycardia articles
Article Details
1. Background
Encephalocraniocutaneous lipomatosis (ECCL), also known asHaberland syndrome, is a rare, non-hereditary neurocutaneous condition first described by Haberland and Perou in 1970. Dysgenesia of the cephalic neural crest and the anterior neural tube during embryo-pathogenesis is a most widely accepted theory. Most ECCL patients present with characteristic lipomatous hamartomas with overlying alopecia in a unilateral distribution on the scalp and ipsilateral scleral lipoepidermoid cysts. The subcutaneous fatty mass with nonscarring alopecia seen in patients with ECCL, better known as nevus psiloliparus is the dermatologic hallmark of the condition. Because of the nonprogressing nature of the lesions involved, most patients with ECCL live nearly normal lives with the exception of an increased chance of epileptic seizures, mild-to-moderate mental retardation, and motor impairment that all correlate with the presence of cerebral malformations, such as intracranial lipomas, spinal lipomas, arachnoid cysts, atrophy of a hemisphere, porencephalic cysts, dilated ventricles, hydrocephalus, and calcifications.
2. Case Report
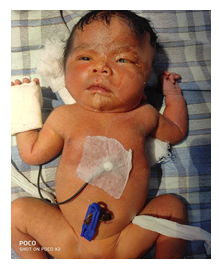
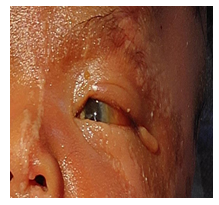
A 7 day old female baby born at full term with a birth weight of 3.2 kg , delivered by normal vaginal delivery with the history of Birth Asphyxia. She was born out of a non-consanguineous marriage, the mother being 28 years old and a second gravida. Antenatally, there was no history of any drug intake or maternal illness and it went uneventful. There was no history of any neonatal death in the family. She was admitted in the NICU (Outborn Unit). On physical examination (head to toe examination), revealed a large hairless lesion on the left frontotemporal scalp (nevus psiloliparus) and similar dermal presentations along the left side of the body (along the lines of Blaschko). Eye examination showed a dermolipoma (bulbar conjunctival hypertrophy) in the left temporal conjunctiva, left sided peripheral corneal opacity, skin tag at the outer canthus, coloboma of the medial left upper eyelid. Grade 2 (Roman) Limbal dermoid as per Visual Scoring System for Limbal Dermoid proposed in 2018.
On Cardiovascular examination, heart sounds were irregularly irregular with no murmur associated. All the other systems were within normal limits including the genitals. The baby went home against medical advice and was regularly followed up over phone. On day 21 of life, the parents informed that the baby expired at home following inconsolable cry since that evening. The cause of death is still unknown.
2.1 Investigations
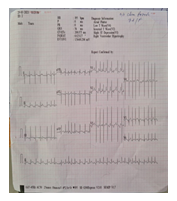
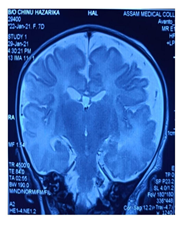
USG B SCAN revealed no obvious abnormality on day 9 and it was advised to repeat the same after the age of one month. Electrocardiogram revealed Multifocal Atrial Tachycardia with Right Axis Deviation. Echocardiogram revealed a patent foramen ovale (3 mm). Radiological investigations, Chest Roentgeno-gram done on Day 6 showed cardiomegaly (Cardiothoracic ratio: 0.67). NECT Brain showed Mild left cerebral hemi atrophy, Focal hyperdense lesion of blood density in right cerebellar hemisphere Contrast enhanced Magnetic Resonance Imaging done on Day 9, showed blooming foci noted in periventricular region adjacent to the occipital horn of bilateral lateral ventricles, suggestive of bleed.
Atrophic changes of bilateral cerebral hemispheres noted as evidenced by prominent extra cerebral CSF spaces, sylvian fissure, temporal and occipital horns of lateral ventricles and benign enlargement of the Subarachnoid spaces. On MR Angiography, A1 segment of left ACA appears hypoplastic, left vertebral artery appears hypoplastic, Left PCOM appears hypoplastic. Skin Biopsy was planned to be done at the age of 6 weeks but could not be done owing to the sudden demise or sudden death.
3. Discussion
ECCL is an uncommon ectomesodermal congenital disorder involving ophthalmological, dermatological and neurological systems. It occurs due to sporadic mutations in the FGFR1 gene involved in making a protein called fibroblast Growth Factor Receptors that triggers signalling within cells important for normal development of several parts of the body , including the brain [1]. Putative focal vascular defects (partial atrophy of one hemisphere/thin cerebral mantle), congenital abnormalities of the meninges, arachnoid cysts are frequently seen [2]. Clinical spectrum varied from totally normal to severe mental retardation with seizures. The extent of central nervous system abnormalities seen with neuroimaging cannot serve as an accurate predictor of future neurologic manifestations (2016) [3]. Proteus Syndrome (progressive and bilateral), Sebacceous nevus syndrome (cutaneous lesions are on the midline of the face) and Oculocerebrocutaneous syndrome (almond shaped hypoplastic skin defect) [4], Congenital lipomatous overgrowth, vascular malformations, epidermal nevi, and spinal/skeletal anomalies (CLOVES), epibulbar dermoids and aplasia cutis are closely comparable to this condition (2016) [3].
|
System |
Major Criteria |
Minor Criteria |
|
Skin |
1. Proven naevus psiloliparus (NP) 2. Possible NP and >1 of the minor criteria 2–5. 3. >2 Minor criteria 2–5 |
1. Possible NP 2. Patchy or streaky non-scarring alopecia without fatty naevus 3. Subcutaneous lipoma(s) in fronto-temporal region 4. Focal skin aplasia/Hypoplasia on scalp 5. Small nodular skin tags on eyelids or between outer canthus and tragus |
|
Eye |
1. Choristoma with or without associated anomalies |
1. Corneal and other anterior chamber anomalies 2. Ocular and eyelid coloboma 3. Calcification of globe. |
|
Central Nervous System |
1. Intracranial lipoma 2. Intraspinal lipoma 3. Two of the minor criteria |
1. Abnormal intracranial vessels, e.g. angioma, excessive vessels 2. Arachnoid cyst or other abnormalities of meninges 3. Complete or partial atrophy of hemisphere 4. Porencephalic cysts(s) 5. Asymmetrically dilated ventricles or hydrocephalous 6. Calcification (not basal ganglia) |
|
Other System |
1. Jaw tumour (osteoma, odontoma, ossifying fibroma. 2. Multiple bone cyst 3. Coarctation of aorta |
Table 1: ECCL diagnostic criteria proposed by Hunter and modified by Moog4.
|
Definite Case |
Probable Case |
|
Three systems involved, major criteria in ≥2, or |
Two systems involved, major criteria in both |
|
Three systems involved, proven NP or possible NP + ≥1 of the minor skin criteria 2-5, or |
Two systems involved, proven or possible NP. |
|
Two systems involved with major criteria, one of which is proven NP or possible NP + ≥1 of the minor skin criteria 2-5. |
Table 2: ECCL Application of criteria to the diagnosis.
4. Conclusion
There is no specific treatment for ECCL; management includes symptomatic treatment and surgical correction of cutaneous lesions for cosmetic improvements. If the diagnosis could be made earlier, the care of symptoms and the quality of life of the patient would be improved.
References
- Richters RJH, Seyger MMB, Meeuwis KAP, et al. Oculoectodermal syndrome – Encepha-locraniocutaneous lipomatosis associated with NRAS mutation. Acta Derm Venereol 100 (2020): 1-2.
- Moog U, Jones MC, Viskochil DH, et al. Brain anomalies in encephalocraniocutaneous lipomatosis. In: American Journal of Medical Genetics, Part A. Am J Med Genet A (2007): 2963-2972.
- Banta J, Beasley K, Kobayashi T, et al. Encephalocraniocutaneous lipomatosis (Haberland syndrome): A mild case with bilateral cutaneous and ocular involvement. JAAD Case Reports 2 (2016): 150-152.
- Özdogan S, Sayman C, Yaltirik CK, et al. Encephalocraniocutaneous lipomatosis: Haber-land syndrome. Am J Case Rep 18 (2017): 1271-1275.