Elements of a Successful Sports Medicine Fellowship Match: A Crosssectional Survey of Fellowship Applicant and Faculty Perspectives
Article Information
Louis M. Day M.D, Nicholas A. Ott M.D, Adam W. Anz M.D, Steve E. Jordan M.D, Jessi Truett Ed.D., BCBA*, Roger V. Ostrander III, M.D
Andrews Research & Education Foundation, 1020 Gulf Breeze Pkwy, Gulf Breeze, FL 32561, USA
*Corresponding Author: Jessi Truett, Andrews Research & Education Foundation, 1020 Gulf Breeze Pkwy, Gulf Breeze, FL 32561, USA
Received: 15 November 2024; Accepted: 22 November 2024; Published: 03 December 2024
Citation: Louis M. Day, Nicholas A. Ott, Adam W. Anz, Steve E. Jordan, Jessi Truett, Roger V. Ostrander. Elements of a Successful Sports Medicine Fellowship Match: A Cross-sectional Survey of Fellowship Applicant and Faculty Perspectives. Journal of Orthopedics and Sports Medicine. 6 (2024): 273-281.
View / Download Pdf Share at FacebookAbstract
Background: The majority of orthopaedic surgery residents complete a year of fellowship training after orthopaedic surgery residency as currentday practice is becoming increasingly subspecialized. In recent years, sports medicine fellowships have consistently had more applicants than positions available, which makes matching applicants to the appropriate program crucial.
Objective: This prospective, cross-sectional survey study aimed to identify the factors of a fellowship program that are important to prospective orthopaedic sports medicine fellows and to the faculty involved in the fellow selection process.
Methods: This study was administered to two groups: 42 prospective fellows (52% response rate) and 27 fellowship faculty (10% response rate). The study occurred from November 2022 to June 2023.
Results: Fifteen applicant factors were evaluated. The top three factors influencing an applicant’s decision were high case volume, high case complexity, and business/practice management training. The lowest three factors influencing an applicant’s decision were trauma call, research activity, and salary. Twelve factors were evaluated for faculty. The top three factors influencing a faculty member’s decision were interview quality, letters of recommendation, and residency reputation. The lowest three factors influencing a faculty member’s decision were sports coverage experience, leadership experience, and conference experience.
Conclusion: This cross-sectional survey study elucidated the top three factors influencing an applicant’s decision to select a sports medicine fellowship. These factors were high case volume, complex case exposure, and business/practice management training. Additionally, the study demonstrated the top three factors considered by faculty members were interview quality, letters of recommendation, and residency reputation.
Keywords
Orthopaedics; Fellowship; Medical education; Orthopaedic match
Article Details
1. Introduction
Most orthopaedic surgery residents (~90%) are choosing to complete a year of fellowship training after orthopaedic surgery residency due to practice becoming increasingly subspecialized [1,2]. The job market has seen a steady increase in positions targeted toward fellowship-trained orthopaedic surgeons. Fellowship training has been shown to improve marketability and positively influence clinical decision-making [3-5]. Sports medicine continues to be one of the most popular and competitive orthopaedic fellowships. In recent years, sports medicine has consistently had more applicants than positions available [6]. Applicants applying to accredited orthopaedic fellowship programs participate in the San Francisco Match (SF Match), a trusted United States-based residency and fellowship match service that weighs applicant preference against program preference to determine the placement of the fellow.7 Programs strive to remain competitive and attract quality applicants. It is beneficial for both applicants and sports medicine faculty to better understand the factors most important to a successful fellowship match [8-10].
The factors that orthopaedic surgery sports medicine applicants desire in a fellowship program have been previously investigated [11-13]. Additionally, the factors that orthopaedic sports medicine program directors deem important in fellowship applicants have been investigated [14,15]. However, more specific details on the exact factors of interest combined with how strongly these factors are favored is not well understood. Previous studies utilized ranking systems to elucidate the factors of interest to applicants and program directors, which do not clearly express the true strength of the participants’ views. Thus, this cross-sectional survey study aimed to identify the genuine factors of a fellowship program that are important to prospective orthopaedic sports medicine fellows. The study also aimed to demonstrate the factors that are important to the faculty members involved in the fellow selection process. Therefore, we hypothesized that the cross-sectional survey would elucidate the factors or qualities important to prospective orthopaedic fellows and the faculty involved in the fellow selection process.
2. Methods
2.1 Participants
This was a prospective cross-sectional survey study with two groups: prospective fellows and fellowship faculty. Enrollment began in November 2022 and was completed in June 2023. The final data analysis was completed November 2023. No changes were made to methods, protocols, or outcome measures after study commencement. Prospective orthopaedic surgery residents who were eligible for selection via the match to begin training at an accredited orthopaedic sports medicine fellowship were included in the applicant survey. Attending physicians involved in the education and training of sports medicine fellows at an accredited orthopaedic sports medicine fellowship were included in the faculty survey.
2.2 Survey creation and distribution
Investigators developed two surveys, one for applicants and one for faculty. The surveys were based on the available literature. Both surveys were reviewed, edited, and approved by the orthopaedic sports medicine faculty at the home institution, as well as the IRB, before being distributed to participants. Both surveys were distributed to participants using Research Electronic Data Capture (REDCap, Nashville, TN). REDCap is a secure browser-based web application that can build and manage online surveys and databases. A 29-question survey, including a 5-point Likert scale and free-text response questions, was sent to all orthopaedic surgery residents applying to an Accreditation Council for Graduate Medical Education (ACGME) accredited orthopaedic sports medicine fellowship at the authors’ home institution in the 2022-2023 match cycle. A 16-question survey, including a 5-point Likert scale and free-text response questions, was sent to orthopaedic sports medicine attending faculty directly involved in sports medicine fellows' education and training. The list of potential participants for the faculty group was obtained from publicly available contact information. The complete list of questions included in the applicant survey can be found in Appendix file. The complete list of questions in the faculty survey can be found in Appendix file. After initial distribution, serial follow-up emails were sent to encourage participation. The survey results were not used to influence the fellowship match process at the home institution and remained anonymous throughout the study.
2.3 Survey Analysis
Descriptive statistical analyses were used to summarize the applicant demographics and all survey responses (ex: proportions, percentages). All Likert scale questions were scored based on the number of responses in each category (n=5) of the Likert scale for each survey. The scoring was assigned as follows: Strongly disagree = -2 points, Disagree = -1 point, Neither agree nor disagree = 0 points, Agree = 1 point, Strongly agree = 2 points. The total scores for each question (factor) within the surveys were calculated. The total scores were then used to sort the factors from most favorable to least favorable. Descending sorting was completed for the graphical figures to represent the most favorable factors on top and the least favorable factors at the bottom. All neutral responses (i.e., Neither agree nor disagree) were graphed separately to prevent skewing. Thematic analysis was employed to elucidate common trends captured within free-response questions.
Institutional review board (IRB) approval was obtained (Number 1988219, Baptist Hospital Institutional Review Board).
3. Results
3.1 Applicants
The applicant survey was distributed to 81 orthopaedic sports medicine fellowship applicants who applied to the authors’ home institution in the 2022-2023 application cycle. Of the 81 applicants, 42 complete responses were received (52% response rate). Out of the 42 applicants, 35 (83%) were male and 7 (17%) were female (Table 1). The vast majority of participants were first-time applicants (98%). When analyzing the geographic location of the applicants’ residency programs, the highest percentage of applicants were from the South region (36%). This was followed by the Midwest (26%), Northeast (24%), West (10%), and International (5%). Twenty-one applicants were former collegiate athletes (50%), and two were former professional athletes (5%). Most of the former collegiate athletes participated in baseball (19%, n=4), followed by football (14%, n=3), and lacrosse (14%, n=3). The two applicants who were former professional athletes played ice hockey and lacrosse, respectively.
|
Question |
N = 42 |
|
Gender, n / N (%) |
|
|
Female |
7 / 42 (17%) |
|
Male |
35 / 42 (83%) |
|
Transgender |
0 / 42 (0%) |
|
Other |
0 / 42 (0%) |
|
Prefer not to say |
0 / 42 (0%) |
|
Residency Location, n / N (%) |
|
|
International |
2 / 42 (5%) |
|
Midwest |
11 / 42 (26%) |
|
Northeast |
10 / 42 (24%) |
|
South |
15 / 42 (36%) |
|
West |
4 / 42 (10%) |
|
First Time Applicant, n / N (%) |
41 / 42 (98%) |
|
Collegiate Athlete, n / N (%) |
21 / 42 (50%) |
|
Professional Athlete, n / N (%) |
2 / 42 (5%) |
Table 1: Self-reported Demographics of Applicant Survey Participants.
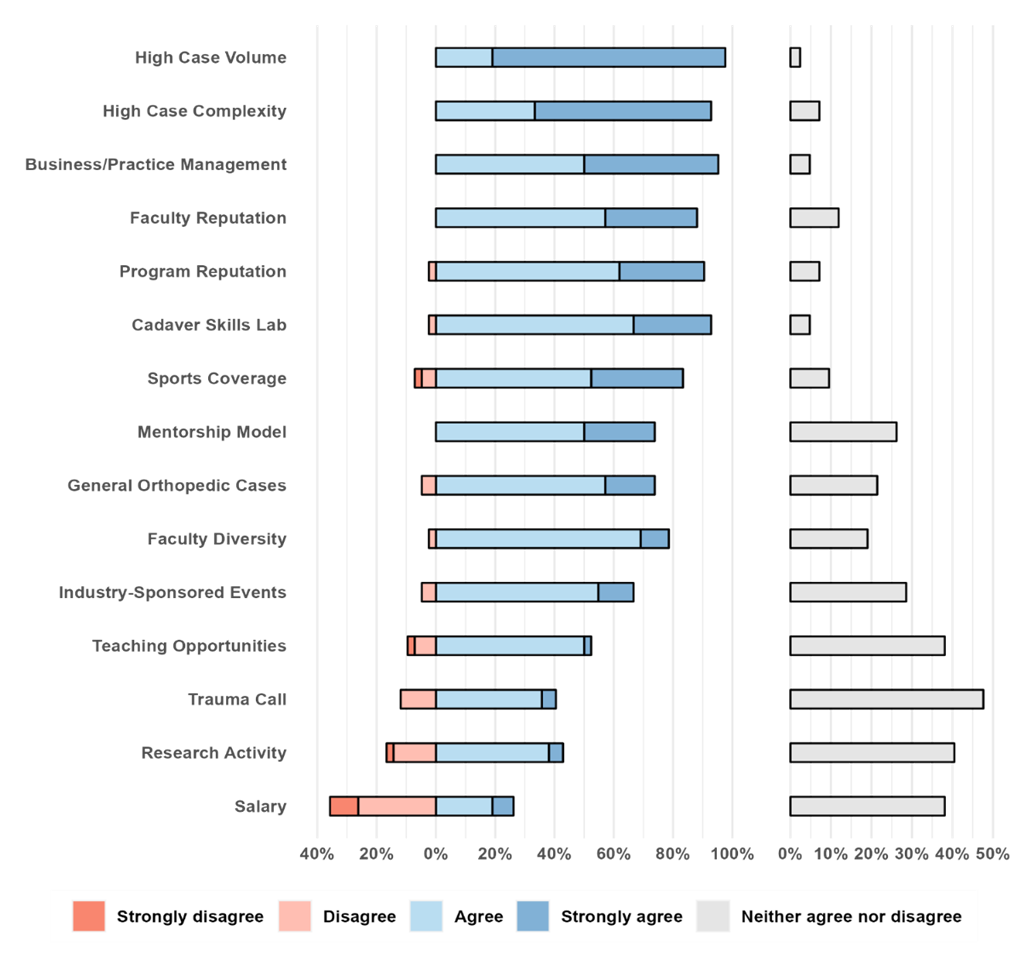
Overall, 15 factors were evaluated for applicants in this study (Figure 1). The top three factors (most favorable) influencing an applicant’s decision were high case volume, high case complexity, and business/practice management training. The lowest three factors (least favorable) influencing an applicant’s decision were trauma call, research activity, and salary.
Several factors (n=5) included in the applicant survey targeted sports medicine practice, including high case volume, high case complexity, sports coverage availability, general orthopaedic case availability, and trauma call requirements. Regarding surgical experience during fellowship, applicants agreed that case volume was essential to a fellowship program (98%). Similar results were found for case complexity (93%). Applicants were asked about the importance of sports coverage during the fellowship year. Most applicants stated that it was important (83%). Collegiate sports were the most desired level of sports coverage (57%), followed by professional sports (33%). When asked which sports they would prefer to cover, applicants mentioned football the most (88%, n=37). This was followed by basketball (52%, n=22), baseball (38%, n=16), and soccer (24%, n=10). The majority of applicants agreed that having opportunities for general orthopaedic cases (i.e., arthroplasty, trauma) is an important aspect of a fellowship program (74%). The most common cases that applicants desired were arthroplasties, including knee and hip (57%, n=24). This was followed by general trauma, including long bone fractures and ankle fractures (29%, n=12). Applicants were asked to list the sports medicine procedures that are most important to gain exposure to during fellowship training in order of importance. Anterior cruciate ligament reconstruction was the most listed procedure (74%, n=31). This was followed by rotator cuff repair (40%, n=17), multi-ligament knee reconstruction (40%, n=17), meniscus repair (38%, n=16), and shoulder instability/labrum repair (24%, n=10). When asked about whether covering trauma call influences the decision to rank a program, many applicants took a neutral stance (48%), fewer agreed (41%), and only a small portion of applicants disagreed (12%). Those who agreed preferred it as an option, but not a requirement and not at the expense of their sports medicine experience (76%, n=13). Some common positive comments for taking trauma call include the opportunity for moonlighting or supplementing income, as well as the opportunity to maintain general trauma surgical skills.
Figure 1: Applicant questionnaire factors. All applicant questionnaire factors (n=15) were scored based on the number of responses in each category of the 5-point Likert scale. The graphic was sorted to list the highest-scoring (most favorable) factors on top and the lowest-scoring (least favorable) factors at the bottom. All neutral responses were graphed separately to prevent skewing.
Most survey factors (n=8) were targeted at the educational aspects of a fellowship, including business/practice management, faculty reputation, program reputation, cadaver skills lab availability, mentorship model, faculty diversity, industry-sponsored events, and teaching opportunities. The addition of business and practice management training to a fellowship program was considered highly important among applicants (95%). Also, applicants agreed that program reputation (91%) and faculty reputation (88%) were important factors when considering fellowship programs. Access to a cadaver surgical skills lab was considered valuable (93%). A fellowship program that follows a mentorship model (extended training period with a specific faculty member) was considered important among applicants (74%). When asked to describe the ideal relationship dynamic between a mentor and mentee, applicants agreed upon a collegial relationship involving trust, respect, and gradual autonomy (60%, n=25). When asked at which point during fellowship applicants expect surgical autonomy, most applicants answered at months three to four (48%). This was followed by months five to seven (41%). The ideal total number of fellows in a program varied. Two fellows was the most common answer (41%). This was followed by three (36%), four (19%), and five or more fellows (5%). In-person interviews were the most popular interview style (60%), compared to virtual interviews (12%). However, many applicants had no preference (29%). Applicants who favored in-person interviews felt that in-person experiences gave them a better feel for the program (80%, n=20). Applicants also believed in-person interviews allow for better interactions and stronger rapport with faculty (64%, n=16). Those in favor of virtual interviews reported that virtual interviews were less expensive (100%, n=5), timesaving (40%, n=2), and allowed for fewer missed interview opportunities (20%, n=1). When asked about faculty diversity, applicants agreed it was an important factor (79%). Industry-sponsored educational events during fellowship were considered important (67%). When asked about teaching opportunities for students or residents, applicants agreed it was important (52%). However, a large portion took a neutral stance (38%). Most applicants viewed the presence of residents as positive (81%). When asked why the presence of residents was positive, the most common response was that they provide teaching opportunities (71%, n=24). This was particularly important for those interested in pursuing academic positions in the future. Also, teaching residents was mentioned as an opportunity to help the fellows themselves learn (47%, n=16). Others noted that residents can help with workload, which includes activities such as rounding (6%, n=2). Those who viewed residents negatively (19%) mentioned they might take away case volume and focus during fellowship training (75%, n=6). Applicants stated this might ultimately affect autonomy or the mentor/mentee relationship (25%, n=2).
Additionally, only about half of applicants believed research activity is an important aspect of a fellowship program (43%), and many took a neutral stance (40%). Annual salary importance was split amongst applicants (26% agreed, 36% disagreed, and 38% took a neutral stance).
3.2 Faculty
The faculty survey was distributed to 267 orthopaedic sports medicine attendings, with 27 participants completing the survey (10% response rate). Twelve factors were evaluated for faculty in this study (Figure 2). The top three factors (most favorable) influencing a faculty member's decision were interview quality, letters of recommendation, and residency reputation. The lowest three factors (least favorable) influencing a faculty member’s decision were sports coverage experience, leadership experience, and conference experience.
Figure 2: Faculty questionnaire factors. All faculty questionnaire factors (n=10) were scored based on the number of responses in each category of the 5-point Likert scale. The graphic was sorted to list the highest-scoring (most favorable) factors on top and the lowest-scoring (least favorable) factors at the bottom. All neutral responses are graphed separately to prevent skewing.
The United States Medical Licensing Examination (USMLE) board scores were included to assess the importance of objective measures in a faculty member's decision-making. Faculty agreed that USMLE scores were important (70%), but many took a neutral stance (30%). All other factors were subjective in nature including interview quality, letters of recommendation, residency reputation, research interest, sports coverage experience, leadership experience, and conference experience. Faculty agreed previous orthopaedic research experience was important (74%), but less so was the desire to pursue future research interests (63%). Like the applicants, most faculty preferred two as the ideal number of fellows in a fellowship program (52%). This was followed by five or more (22%), three (19%), and then four fellows (7%). Like applicants, many faculty mentioned a mentorship model when describing the ideal relationship dynamic between a fellow and attending physician (44%, n=12). Additionally, mutual respect was a factor mentioned amongst faculty as important (19%, n=5). Most faculty preferred in-person interviews (89%) over virtual interviews (7%). The faculty in favor of in-person interviews felt that it offered a more thorough interview experience to assess the applicants’ personalities (79%, n=19) and allowed the applicant to better evaluate the facilities and program (21%, n=5). Those favoring virtual interviews stated that it was more convenient for the applicants. Diversity of the applicant was considered an important aspect of the application to faculty (63%).
4. Discussion
The most important finding of this cross-sectional survey study was that the top three factors influencing an applicant’s decision to select a sports medicine fellowship were high case volume, complex case exposure, and business/practice management training. In comparison, the top three factors for faculty members were interview quality, letters of recommendation, and residency reputation. The 15 factors evaluated for applicants were assessed using a survey. They were subsequently ranked based on total score per factor, which revealed the most and least important factors considered by applicants. Similarly, 12 factors were evaluated for faculty using a separate survey and ranked similarly.
The importance placed on high case volume and complex case exposure by applicants is similar to previous reports in the literature [12,13]. Oser et al. [13] reported that the variety and complexity of surgical cases are the most important factors in choosing fellowship programs. Business and practice management training was the third most important factor for applicants in a sports medicine fellowship program. Lusco et al. [16] demonstrated that general surgery program directors feel that residents should be trained in business and practice management, but are inadequately trained in this area. Miller et al. [17] further concluded that graduating orthopaedic residents were inadequately prepared to manage business issues in their respective practices. The graduating orthopaedic residents tended to have deficiencies in functional knowledge regarding business and practice management, particularly those of hospital-based practices. Our study shows prospective fellows emphasize business and practice management as part of their education, especially in the rapidly changing healthcare environment. Business management curriculums have previously been incorporated into fellowships to meet this deficiency. The Reno Orthopaedic Center trauma fellowship developed and implemented a business curriculum into their fellowship to provide their fellows with practical knowledge, allowing cost-efficient improvements in healthcare delivery [18,19].
Orthopaedic sports medicine faculty considered the quality of the interview, letters of recommendation, and residency reputation as the most important factors of a fellowship applicant’s application. This is similar to a previous study that showed the interview, letters of recommendation, and applicant residency program as the most important factors to program directors in ranking sports medicine fellowship applicants [15]. This data has been further supported by a study from Haislup et al. [14] which demonstrated that program directors placed high importance on the quality of the interview. The interview was also an important factor in ranking prospective orthopaedic surgery residents, which correlated with the rank list [20]. An applicant’s residency reputation was ranked as the third most important aspect of an applicant’s application in this study. This is consistent with findings from a previous study showing that most top-ranked orthopaedic sports medicine fellowships have matched fellows from the same residency programs for multiple years (a process commonly known as “pipelining”) [21]. More emphasis may be placed on residency reputation when faculty cannot get a sense of an applicant’s personality or skills through a virtual interview instead of in person. Peebles et al. [8,9] cautioned that program directors may shift emphasis to “word-of-mouth references”, personal connections to the fellows or faculty, or residency programs following the changes after the COVID-19 pandemic [8,9]. An overwhelming majority (89%) of faculty in this study preferred in-person interviews, which may help ameliorate this issue.
Regarding specific case types, this study showed that ACL reconstruction is the procedure that prospective applicants want the most exposure to. This was followed by rotator cuff repair and multi-ligament knee reconstruction. This is likely due to the increasing occurrence of ACL injuries and subsequent reconstructions performed each year [22,23]. The rate of rotator cuff tears and subsequent repairs have also been steadily increasing. A study conducted by Yanik et al. [24] demonstrated that the rate of rotator cuff repair has been rising at about 1.6% per year, particularly in the 50-64 year age range. Multi-ligament knee reconstruction was the third most cited procedure applicants want exposure to during fellowship. One study previously reported that fellowship-trained sports medicine surgeons had significantly lower comfort levels with posterior cruciate ligament reconstruction and multi-ligamentous knee reconstruction [26]. This may be why fellowship applicants are placing importance on exposure to such procedures [3]. Meniscus repairs were also among the most highly sought-after procedures. This matches the increasing rate of isolated meniscus repair and increased interest in meniscus preservation in recent years [25]. Interestingly, hip arthroscopy was not ranked highly despite the increasing prevalence in fellowship [13]. These preferences should be considered by both applicants and faculty when assessing program fit.
Orthopaedic surgeons are choosing to pursue subspecialty fellowship training more frequently now than ever before. This shift is primarily due to increased marketability and the opportunity to improve surgical clinical decision-making skills associated with fellowship training. Sports medicine has continued to be among the most popular and, thus, the most competitive orthopaedic fellowships available. Due to the competitive nature of these programs, it is important that both applicants and faculty find an appropriate fit that offers the best learning experience. This ensures the quality of their subsequent work done during the fellowship year. What makes an appropriate “fit” has been evaluated in the literature for both applicants and faculty to varying degrees. This study has provided a standardized scoring of factors on a 5-point Likert scale. This methodology is frequently employed by cross-sectional survey studies [11-15,26]. Furthermore, Likert scales have been noted to have greater reliability than visual analog scales, which many studies in the current literature have used [26]. The factors elucidated in this study for applicants and faculty can thus reliably be considered to ensure a successful sports medicine fellowship match.
There are several limitations to cross-sectional survey studies, with the largest being the limitation of sample size for both applicants and faculty. The applicant sample size was limited to those applying to the authors’ home institution, which may not reflect the views of orthopaedic sports medicine applicants in other programs. The faculty sample size was limited to those who could be publicly identified online as orthopaedic sports medicine attending faculty. This was further limited to individuals directly involved in sports medicine fellows' education and training.
5. Conclusion
This cross-sectional survey study elucidated the top three factors influencing an applicant’s decision to select a sports medicine fellowship: high case volume, complex case exposure, and business/practice management training. The study also demonstrated the top three factors considered by faculty members were interview quality, letters of recommendation, and residency reputation.
Acknowledgements:
This work was financially supported in part by a grant from the State of Florida Department of Health (DoH).
- Andrews Institute Center for Regenerative Medicine, Department of Research, Andrews Research & Education Foundation (AREF), Gulf Breeze, FL 32561, USA.
- ICMJE criteria for authorship:
- • Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND
- • Drafting the work or revising it critically for important intellectual content; AND
- • Final approval of the version to be published; AND
- • Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Author List:
- Louis M. Day, M.D.1,2 - Co-investigator. Responsible for all ICMJE criteria for authorship (1-4). Specifically played a large role in concept design of work, patient recruitment, data interpretation, manuscript drafting, manuscript approval, and revision questions.
- Nicholas A. Ott, M.D.1,2 - Co-investigator. Responsible for all ICMJE criteria for authorship (1-4). Specifically played a large role in concept design of work, data analysis, data interpretation, manuscript drafting, manuscript approval, and revision questions.
- Adam W. Anz, M.D.1,2 - Co-investigator. Responsible for all ICMJE criteria for authorship (1-4). Specifically played a large role in concept design of work, patient recruitment, data interpretation, manuscript drafting, manuscript approval, and revision questions.
- Steve E. Jordan, M.D.1,2 - Co-investigator. Responsible for all ICMJE criteria for authorship (1-4). Specifically played a large role in concept design of work, data analysis, data interpretation, manuscript drafting, manuscript approval, and revision questions.
- Jessi Truett, Ed.D., BCBA.1,2*, - Corresponding author and Co-investigator. Responsible for all ICMJE criteria for authorship (1-4). Specifically played a large role in concept design of work, data analysis, data interpretation, manuscript drafting, manuscript approval, and revision questions.
- Roger V. Ostrander III, M.D.1,2 - Primary investigator and Fellowship Program Director. Responsible for all ICMJE criteria for authorship (1-4).
Primary Institution:
Andrews Research & Education Foundation (AREF).
Funding:
This project was funded by a grant from the State of Florida Department of Health.
IRB:
Baptist Hospital IRB Number 1988219.
Confirmation Statement:
This article is neither published nor under consideration by another journal.
References
- Horst PK, Choo K, Bharucha N, et al. Graduates of Orthopaedic Residency Training are Increasingly Subspecialized: A Review of the American Board of Orthopaedic Surgery Part II Database. J Bone Joint Surg Am 97 (2015): 869-75.
- Harner CD, Ranawat AS, Niederle M, et al. AOA symposium. Current state of fellowship hiring: is a universal match necessary? Is it possible? J Bone Joint Surg Am 90 (2008): 1375-84.
- Yin B, Gandhi J, Limpisvasti O, et al. Impact of fellowship training on clinical practice of orthopaedic sports medicine. J Bone Joint Surg Am 97 (2015): e27.
- Mannava S, Jinnah AH, Cinque ME, et al. An Analysis of Orthopaedic Job Trends in the United States Over the Past 30 years. J Am Acad Orthop Surg Glob Res Rev 2 (2018): e056.
- Morrell NT, Mercer DM, Moneim MS. Trends in the orthopedic job market and the importance of fellowship subspecialty training. Orthopedics 35 (2012): e555-60.
- Mulcahey MK, Hayes MK, Smith CM, et al. Outcomes in the Orthopaedic Sports Medicine Fellowship Match, 2010-2017. Orthop J Sports Med 6 (2018): 2325967118771845.
- SF Match - Residency and Fellowship Match Services (2023). https://sfmatch.org/
- Peebles LA, Aman ZS, Kraeutler MJ, et al. The COVID-19 Pandemic Increased the Use of Virtual Fellowship Interviews, Reduced Case Volume, and Limited Sideline Coverage Opportunities During Sports Medicine Surgeon Training. Arthrosc Sports Med Rehabil 5 (2023): e891-e895.
- Peebles LA, Kraeutler MJ, Waterman BR, et al. The Impact of COVID-19 on the Orthopaedic Sports Medicine Fellowship Application Process. Arthrosc Sports Med Rehabil 3 (2021): e1237-e1241.
- Clark SC, Kraeutler MJ, McCarty EC, et al. Virtual Interviews for Sports Medicine Fellowship Positions Save Time and Money but Don't Replace In-Person Meetings. Arthrosc Sports Med Rehabil 4 (2022): e607-e615.
- Geraghty EH, Kraeutler MJ, Clark SC, et al. Program and Faculty Reputation Are Valued Most by Applicants to Orthopaedic Sports Medicine Fellowships. Arthrosc Sports Med Rehabil 5 (2023): e129-e135.
- Niesen MC, Wong J, Ebramzadeh E, et al. Orthopedic surgery fellowships: the effects of interviewing and how residents establish a rank list. Orthopedics 38 (2015): 175-9.
- Oser FJ, Grimsley BM, Swinford AJ, et al. Variety and Complexity of Surgical Exposure, Operative Autonomy, and Program Reputation Are Important Factors for Orthopaedic Sports Medicine Fellowship Applicants. Arthrosc Sports Med Rehabil 3 (2021): e855-e859.
- Haislup BD, Kraeutler MJ, Baweja R, et al. Orthopaedic Sports Medicine Fellowship Interviews: Structure and Organization of the Interview Day. Orthop J Sports Med 5 (2017): 2325967117741276.
- Baweja R, Kraeutler MJ, Mulcahey MK, et al. Determining the Most Important Factors Involved in Ranking Orthopaedic Sports Medicine Fellowship Applicants. Orthop J Sports Med 5 (2017): 2325967117736726.
- Lusco VC, Martinez SA, Polk HC. Jr. Program directors in surgery agree that residents should be formally trained in business and practice management. Am J Surg 189 (2005): 11-3.
- Miller DJ, Throckmorton TW, Azar FM, et al. Business and Practice Management Knowledge Deficiencies in Graduating Orthopedic Residents. Am J Orthop (Belle Mead NJ) 44 (2015): E373-8.
- Althausen PL, Lybrand KE. The Role of Business Education in the Orthopedic Curriculum. Orthop Clin North Am 49 (2018): 445-453.
- Althausen PL, Bray TJ, Hill AD. Reno Orthopaedic Trauma Fellowship business curriculum. J Orthop Trauma 28 (2014): S3-11.
- Schenker ML, Baldwin KD, Israelite CL, et al. Selecting the Best and Brightest: A Structured Approach to Orthopedic Resident Selection. J Surg Educ 73 (2016): 879-85.
- Tanguilig G, Kraeutler MJ, Mulcahey MK. The Top 10 Orthopaedic Sports Medicine Fellowship Programs in the United States Frequently Select Fellowship Applicants From the Same Residency Programs. Arthrosc Sports Med Rehabil 5 (2023): e411-e414.
- Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 42 (2014): 2363-70.
- Herzog MM, Marshall SW, Lund JL, et al. Trends in Incidence of ACL Reconstruction and Concomitant Procedures Among Commercially Insured Individuals in the United States, 2002-2014. Sports Health 10 (2018): 523-531.
- Yanik EL, Chamberlain AM, Keener JD. Trends in rotator cuff repair rates and comorbidity burden among commercially insured patients younger than the age of 65 years, United States 2007-2016. JSES Rev Rep Tech 1 (2021): 309-316.
- Abrams GD, Frank RM, Gupta AK, et al. Trends in meniscus repair and meniscectomy in the United States, 2005-2011. Am J Sports Med 41 (2013): 2333-9.
- Bishop PA, Herron RL. Use and Misuse of the Likert Item Responses and Other Ordinal Measures. Int J Exerc Sci 8 (2015): 297-302.
Appendix File:
Complete List of Faculty Survey Questions
Q1: For applicants researching fellowship programs online, the information available is comprehensive, updated, and accurate.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q2: An applicant’s desire to pursue future research interests is an important aspect of a fellow’s application.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q3: An applicant’s previous experience in orthopaedic research is an important aspect of a fellow’s application.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q4: The quality of the applicant’s interview is an important aspect of a fellow’s application.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q5: An applicant’s experience attending or presenting at orthopaedic and/or sports medicine-related conferences is an important aspect of a fellow’s application.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q6: Letters of recommendation from sports medicine or orthopaedic faculty is an important aspect of a fellow’s application.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q7: An applicant’s previous experience and level of sports coverage is an important aspect of a fellow’s application.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q8: An applicant’s relevant leadership experience on committees at the medical school or residency level is an important aspect of a fellows application.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q9: An applicant’s USMLE board scores are an important aspect of a fellow’s application.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q10: The reputation of an applicant’s residency program is an important aspect of a fellow’s application.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q11: An applicant’s diversity is an important aspect of a fellow’s application.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q12: What effect did the transition to telemedicine services have on your ability to teach clinical skills?
Responses: “Negative”, “Somewhat negative”, “No effect”, “Somewhat positive”, “Positive”
Q13: There continue to be residual impacts from the COVID-19 pandemic on the fellowship selection process and fellow education.
Responses: “Strongly agree”, “Agree”, “Neither agree nor disagree”, “Disagree”, “Strongly disagree”
Q14: How many total fellows per program would you prefer?
Responses: “1”, “2”, “3”, “4”, “5+”
Q15: What is your preferred interview style?
Responses: “In-person interview”, “Virtual interview”, “No preference”
Why did you choose your answer for the previous question?
Responses: Free-text response
Q16: Please describe the ideal relationship dynamic between a fellow and attending physician.
Responses: Free-text response