Efficacy and Safety of Psychotherapeutic Interventions in Adults at Risk of Suicide: An Umbrella Review
Article Information
Erasmo Saucedo Uribe1,2,3,*, Leonel Estanislao Villalobos Gutiérrez1,Neri Alejandro Álvarez Villalobos3,Sandra Sabrina Rojo Garza3,Rodrigo Huereca Lucio2, Alessandro Javier Vite Castillo2,Alan Iván Macias Quintanilla2,Irma Guadalupe Rocha Rangel2,Eduardo Jahir López Sanchéz2
1Department of Psychiatry, University Hospital “Dr. José E. González”, Universidad Autónoma de Nuevo León, Monterrey, Nuevo León, México
2Centro de Neurociencias Avanzadas UANL, University Hospital “Dr. José E. González”, Universidad Autónoma de Nuevo León, Monterrey, Nuevo León, México
3Centro de Análisis Avanzado de Información Científica 360, Facultad de Medicina of Universidad Autónoma de Nuevo León
*Corresponding Author: Erasmo Saucedo, Department of Psychiatry, University Hospital “Dr. José E. González”, Universidad Autónoma de Nuevo León, Monterrey, Nuevo León, México, Mitras Centro, Monterrey
Received: 26 December 2023; Accepted: 03 January 2024; Published: 29 January 2024
Citation: Erasmo Saucedo Uribe, Leonel Estanislao Villalobos Gutiérrez,Neri Alejandro Álvarez Villalobos,Sandra Sabrina Rojo Garza,Rodrigo Huereca Lucio, Alessandro Javier Vite Castillo,Alan Iván Macias Quintanilla,Irma Guadalupe Rocha Rangel,Eduardo Jahir López Sanchéz. Efficacy and Safety of Psychotherapeutic Interventions in Adults at Risk of Suicide: An Umbrella Review. 8 (2024): 24-39.
View / Download Pdf Share at FacebookAbstract
Background: Psychological therapies are increasingly important in providing interventions to people at risk of suicide, but good quality evidence on their effectiveness remains low. The aim of this study is to determine the efficacy and safety of psychotherapies on suicidality in psychiatric adult patients.
Method: We conducted a systematic search in MEDLINE, Embase, Web of science, Scopus, PsycInfo and CDSR database from the first available year to August 2023. The methodological quality was evaluated by the AMSTAR-2 tool. We summarized the effects of psychotherapies on suicide-related outcomes.
Results: 7 systematic reviews (SR) and meta-analyses (MA) were included, 3 in patients with depression and 4 in borderline personality disorder (BPD). The studies´ quality of evidence ranges from critically low to high. The effect of psychotherapies on suicide-related outcomes were summarized, highlighting mindfulness-based interventions (MBIs) and problem-solving therapy (PST) for depression, and Schema therapy (SchT), mentalization-based therapy (MBT), psychodynamic therapy (PDT), and dialectical behavioral therapy (DBT) for BPD. Only one study reported safety results. Limitations: The number of studies excluded not meeting the inclusion criteria; a more inclusive search strategy; the quality of the evidence of the included studies.
Conclusion: In major depressive disorder (MDD), PST and MBIs show statistically significant improvements in reducing suicidal ideation. In BPD, SchT can be effective in reducing unspecified suicidality, MBT on “self-harm” and “suicidal ideation and behavior”, DBT and PDT in selfinjurious behaviors. Only 1 study reported data of the psychotherapies´ safety. More precise, specific and higher quality evidence is required to establish reliable conclusions.
Keywords
Umbrella Review, Psychotherapy, Suicide, Self-injurious Behavior, Suicidal Ideation, Major Depressive Disorder, Borderline Personality Disorder.
Umbrella Review articles; Psychotherapy articles; Suicide articles; Self-injurious Behavior articles; Suicidal Ideation articles; Major Depressive Disorder articles; Borderline Personality Disorder articles
Umbrella Review articles Umbrella Review Research articles Umbrella Review review articles Umbrella Review PubMed articles Umbrella Review PubMed Central articles Umbrella Review 2023 articles Umbrella Review 2024 articles Umbrella Review Scopus articles Umbrella Review impact factor journals Umbrella Review Scopus journals Umbrella Review PubMed journals Umbrella Review medical journals Umbrella Review free journals Umbrella Review best journals Umbrella Review top journals Umbrella Review free medical journals Umbrella Review famous journals Umbrella Review Google Scholar indexed journals Psychotherapy articles Psychotherapy Research articles Psychotherapy review articles Psychotherapy PubMed articles Psychotherapy PubMed Central articles Psychotherapy 2023 articles Psychotherapy 2024 articles Psychotherapy Scopus articles Psychotherapy impact factor journals Psychotherapy Scopus journals Psychotherapy PubMed journals Psychotherapy medical journals Psychotherapy free journals Psychotherapy best journals Psychotherapy top journals Psychotherapy free medical journals Psychotherapy famous journals Psychotherapy Google Scholar indexed journals Suicide articles Suicide Research articles Suicide review articles Suicide PubMed articles Suicide PubMed Central articles Suicide 2023 articles Suicide 2024 articles Suicide Scopus articles Suicide impact factor journals Suicide Scopus journals Suicide PubMed journals Suicide medical journals Suicide free journals Suicide best journals Suicide top journals Suicide free medical journals Suicide famous journals Suicide Google Scholar indexed journals Self-injurious Behavior articles Self-injurious Behavior Research articles Self-injurious Behavior review articles Self-injurious Behavior PubMed articles Self-injurious Behavior PubMed Central articles Self-injurious Behavior 2023 articles Self-injurious Behavior 2024 articles Self-injurious Behavior Scopus articles Self-injurious Behavior impact factor journals Self-injurious Behavior Scopus journals Self-injurious Behavior PubMed journals Self-injurious Behavior medical journals Self-injurious Behavior free journals Self-injurious Behavior best journals Self-injurious Behavior top journals Self-injurious Behavior free medical journals Self-injurious Behavior famous journals Self-injurious Behavior Google Scholar indexed journals Suicidal Ideation articles Suicidal Ideation Research articles Suicidal Ideation review articles Suicidal Ideation PubMed articles Suicidal Ideation PubMed Central articles Suicidal Ideation 2023 articles Suicidal Ideation 2024 articles Suicidal Ideation Scopus articles Suicidal Ideation impact factor journals Suicidal Ideation Scopus journals Suicidal Ideation PubMed journals Suicidal Ideation medical journals Suicidal Ideation free journals Suicidal Ideation best journals Suicidal Ideation top journals Suicidal Ideation free medical journals Suicidal Ideation famous journals Suicidal Ideation Google Scholar indexed journals Major Depressive Disorder articles Major Depressive Disorder Research articles Major Depressive Disorder review articles Major Depressive Disorder PubMed articles Major Depressive Disorder PubMed Central articles Major Depressive Disorder 2023 articles Major Depressive Disorder 2024 articles Major Depressive Disorder Scopus articles Major Depressive Disorder impact factor journals Major Depressive Disorder Scopus journals Major Depressive Disorder PubMed journals Major Depressive Disorder medical journals Major Depressive Disorder free journals Major Depressive Disorder best journals Major Depressive Disorder top journals Major Depressive Disorder free medical journals Major Depressive Disorder famous journals Major Depressive Disorder Google Scholar indexed journals Borderline Personality Disorder articles Borderline Personality Disorder Research articles Borderline Personality Disorder review articles Borderline Personality Disorder PubMed articles Borderline Personality Disorder PubMed Central articles Borderline Personality Disorder 2023 articles Borderline Personality Disorder 2024 articles Borderline Personality Disorder Scopus articles Borderline Personality Disorder impact factor journals Borderline Personality Disorder Scopus journals Borderline Personality Disorder PubMed journals Borderline Personality Disorder medical journals Borderline Personality Disorder free journals Borderline Personality Disorder best journals Borderline Personality Disorder top journals Borderline Personality Disorder free medical journals Borderline Personality Disorder famous journals Borderline Personality Disorder Google Scholar indexed journals psychotherapy articles psychotherapy Research articles psychotherapy review articles psychotherapy PubMed articles psychotherapy PubMed Central articles psychotherapy 2023 articles psychotherapy 2024 articles psychotherapy Scopus articles psychotherapy impact factor journals psychotherapy Scopus journals psychotherapy PubMed journals psychotherapy medical journals psychotherapy free journals psychotherapy best journals psychotherapy top journals psychotherapy free medical journals psychotherapy famous journals psychotherapy Google Scholar indexed journals mental disorder articles mental disorder Research articles mental disorder review articles mental disorder PubMed articles mental disorder PubMed Central articles mental disorder 2023 articles mental disorder 2024 articles mental disorder Scopus articles mental disorder impact factor journals mental disorder Scopus journals mental disorder PubMed journals mental disorder medical journals mental disorder free journals mental disorder best journals mental disorder top journals mental disorder free medical journals mental disorder famous journals mental disorder Google Scholar indexed journals psychiatric articles psychiatric Research articles psychiatric review articles psychiatric PubMed articles psychiatric PubMed Central articles psychiatric 2023 articles psychiatric 2024 articles psychiatric Scopus articles psychiatric impact factor journals psychiatric Scopus journals psychiatric PubMed journals psychiatric medical journals psychiatric free journals psychiatric best journals psychiatric top journals psychiatric free medical journals psychiatric famous journals psychiatric Google Scholar indexed journals
Article Details
1. Introduction
According to the World Health Organization (WHO) suicide is defined as the deliberate act of taking one's own life and more than 800,000 people die by suicide each year, so it represents an important global and public health problem [1,2]. In the general population, a previous suicide attempt is the most important risk factor for suicide [3]. Also, an episode of self-harm increases the chance of suicide by up to 100 times [4,5] making it a strong predictor of future suicide attempts [6, 7].
A problem in suicide research is the confusion resulting from the use of different terms to define suicidal behavior [8]. The North American literature distinguishes between suicide attempts and non-suicidal self-harm on the basis of intent to die [9], whereas, in the UK and Europe, the term 'self-harm'' is used to include any act of non-fatal harm against oneself, regardless of motivation or method, so the term ''suicide attempt'' is included within the term 'self-harm'' [10, 11, 12]. This lack of consensus could be explained by the high heterogeneity between studies due to the difference in suicidal phenotypes, methods of measurement, treatments, population characteristics and diagnosis. In clinical practice the risk of suicide is defined according to the best clinical judgment and criteria used by the person researching or through the support of multiple clinimetric scales.
Psychological therapies are increasingly important in providing interventions to people at risk of suicide or repeated self-harm, but good quality evidence on the effectiveness of interventions remains low [10, 11,12]. Because suicidal behavior also occurs in other mental disorders, there is not enough diagnostic specificity to link suicidal behavior exclusively to depression (Harned et al., 2014), so it is expected that they differ in their characteristics among the different diseases, such as characterological suicidality present in personality disorders, mainly in BPD, where suicidality is more unpredictable. Many psychotherapeutic approaches that target affective instability [13], as well as impulsivity [14] have been studied for this type of suicidality, such as dialectical behavior therapy [15, 16, 17] transference-focused psychotherapy [18] schema-focused therapy (SchT; Clarkin et al., 2007). Several recent SR and MA evaluating the effectiveness of psychoanalytic psychotherapy (Ougrin et al., 2015) (Abbass et al., 2014) conclude that effect sizes are largely similar to those of other therapies, although it may demonstrate superiority at follow-up in the longer term (de Maat et al., 2013) (Fonagy et al., 2015).
Despite the large number of studies on the effectiveness of psychotherapies in different disorders, it has been given less priority to the effect and safety of psychotherapy on suicidality, so there is still controversy about what type of psychotherapeutic interventions are of greater benefit to reduce the risk of suicide. To date, there is no umbrella review (UR) that describes the efficacy and safety of the different types of psychotherapy to reduce suicide risk among the different types of psychiatric disorders. We reviewed the published MA or SR to evaluate the available evidence for the influence of psychotherapies on suicide. The aim of this research is to summarize and evaluate the existing evidence to explore the impact of psychotherapies on suicide in adults with a specific psychiatric diagnosis.
2. Methods
The study protocol was registered in PROSPERO 2021: CRD42021237263.
2.1 Searching strategies and inclusion criteria
An UR was conducted. Two literature searchers were carried out by an expert external to the protocol in the databases MEDLINE, Embase, Web of science, Scopus, PsycInfo and CDSR to identify SR or MA that addressed observational, randomized and non randomized studies that examine the efficacy and safety of psychotherapeutic interventions for suicide risk in patients over 18 years of age with a psychiatric diagnosis. Following the guidelines of an umbrella type review, the first search and an update was carried out for articles published up to April 12, 2021 and August 15, 2023, respectively. The search strategy used the key words (¨psychiatric disorders¨ OR ¨psychiatric condition¨ OR ¨mental disorder¨) AND (¨psychotherapeutic counseling¨ OR ¨psychotherapy¨ OR ¨mental health programs¨) AND (¨suicide¨ OR ¨suicide risk¨ OR ¨self-destructive behavior¨ OR ¨attempt suicide¨ OR ¨suicidality¨) AND (¨systematic review¨ OR ¨meta analysis OR metaanalysis¨). To ensure inter-rater reliability during study selection, pilot tests were conducted, and Cohen's kappa coefficient was measured. Once a kappa greater than 0.7 was reached and agreement was found between the evaluators, the selection phase of titles and abstracts and full texts began. The review of the search results is carried out in three phases. In the first phase, six authors independently and in duplicate reviewed all titles and abstracts to select articles relevant to the topic. In the second phase, the full texts were searched for screening and included if they met the selection criteria, conflicts were resolved by a third reviewer; the articles that were not available in full text were excluded from the study. In the third phase, to avoid bias due to repetition of research subjects from the primary studies in the analysis, the primary studies and their inclusion criteria were reviewed in each SR and/or MA, using the information described in the tables of characteristics of the included studies, with the aim of identifying those primary studies that are repeated among secondary studies or that did not meet the inclusion criteria of the present UR. Once the repeated studies were identified, it was decided to eliminate those secondary studies in which all the primary studies were repeated or that did not meet the criteria. Language was not a limitation to the study.
2.2 Eligibility criteria
The selection criteria were the characteristics of the studies along with the participant, intervention, comparison, outcome criteria (PICO). The target studies consisted of SR and/or MA that included patients ≥18 years of age with an established psychiatric diagnosis as defined by diagnostic criteria or clinical diagnosis confirmed by a clinimetric tool or a diagnostic classification: Mini International Neuropsychiatric Interview (MINI), Structured Clinical Interview for DSM-5 (SCID), any edition of the international Classification of Diseases (ICD) or Diagnostic and Statistical Manual of Mental Disorders in its fourth edition, fourth revised edition or fifth edition (DSM-IV, -TR, -V), and reporting sufficient data to perform the analyses, with or without psychiatric comorbidities. The intervention had to feature any type of psychotherapy approach either face-to-face, in its entirety, as part of the exposure of interest, or as part of the subgroup analysis and no comparator restrictions. The result had to contain any suicidality-related outcome and/or safety of the intervention as a primary or secondary outcome. Studies were excluded if: did not specify psychiatric diagnosis; did not evaluate the effectiveness of psychotherapy on suicidality; included interventions other than face-to-face psychotherapy (telepsychiatry, interventions via email or text message); evaluated treatments that were not intended to be complete (complementary modules to psychotherapies); included vulnerable populations, such as prisoners or cancer patients; the population was under 18 years of age, however, when there was no age restriction and the data were separated by age subgroups, only information from those under 18 years of age was excluded.
2.3 Data extraction
Data extraction was performed independently and in duplicate. Any discrepancies were resolved in consensus meetings with two of the authors and a third reviewer. If data of importance to our study were incomplete, the author of the corresponding article would be contacted to request additional information, however, this was not necessary.
Information extracted from the reviews includes general study information such as author, country and publication date; number of studies and participants included; interventions, outcome measures; effect size with 95% confidence interval (CI), P, I2 value; summary of results. The recommendation of the tool for conducting SR and MA “Preferred reporting items for Systematic reviews and Meta-analyses” (PRISMA) were followed.
2.4 Methodological and quality evaluation of the evidence
Two authors independently assessed the quality of evidence of the included reviews. The methodological quality was evaluated using the AMSTAR-2 tool (A Measurement Tool to Assess Systematic Reviews). The tool includes a checklist divided into sections with a total of 16 elements, of which 7 are considered critical domains to determine the confidence of the SR and/or MA. For the evaluation of the studies, the elements had to be answered with: “Yes'', “Partial Yes" or "No". The score given was divided into four degrees of study quality: high, moderate, low or critically low. All this is described in the Appendix [19].
2.5 Statistical Analysis
A descriptive analysis of the included MA and SR was carried out, along with the impact measures (OR, RR, SMD, with 95% CI) of interventions on suicide-related outcomes. The tables 1, 3 and 4 describe the main characteristics of each study included and in the results section a narrative description of the studies and its main findings related to the interventions that have shown effectiveness on suicidality was carried out. Due to the heterogeneity of the studies, the outcome measure evaluated (suicidality, parasuicidal behavior, suicidal ideation, self-harm, suicidal behavior), and the reporting of effect sizes, it was not possible to perform a MA, so a descriptive analysis was chosen. The measures of the effect size of psychotherapies on suicide risk were: incidence rate ratio (IRR), odds ratio (OR), risk ratio (RR) and standardized mean difference (Hedges' g) for continuous measurements. Mainly, the measure of effect size and its CI was used.
Table 1 : Characteristics of the studies included.
CBA, Controlled before and after; df, degrees of freedom; I2, heterogeneity statistic; MA, Meta-analysis; n, simple size; NA, Not available; Q, Q-statistic.; QES, Quasi-experimental studies; RCT, Randomized Controlled Trial; SR, Systematic Review Diagnosis: BPD, Borderline Personality Disorder.
Table 2 : Assessments of the AMSTAR-2.
N: No; N-MA-C: No meta-analysis conducted; O-RCT: Includes only RCTs; PY: Partial yes; Q: Question; Y: Yes.
Table 3: Characteristics of Depression Studies.
CI, Confidence interval; g, Hedges g; n, simple size; NA, Not Available; NRCT, Non-Randomized Controlled Trial; OR, Odds ratio; p, p value; RCT, Randomized Controlled Trial; RR, Risk Ratio; SMD, Standardized Mean Difference; t, t-statistic.
Assessments tools: LPC, Lifetime Parasuicide Count; OAS-M, Overt Aggression Scale-Modified; SASII, Suicide Attempt Self-Injury Interview.
Diagnosis: BPD, Borderline Personality Disorder.
Psychotherapy: CAT, Cognitive Analytic Therapy; CBT, Cognitive Behavioral Therapy; CCT, Client-Centered Therapy; CTBE, Community Therapy by Experts; CVT, Comprehensive Validation Therapy; DBT-C, Dialectical Behavioral Therapy; DBT, Dialectical Behavioral Therapy; DBTmin, Reduced Dialectical Behavioral Therapy; DDP, Dynamic Deconstructive Psychotherapy; GPM, General Psychiatric Management; IGP, Interpersonal Group Psychotherapy; IT, Interpersonal Therapy; IPT-BPD, Interpersonal Therapy adapted for Borderline Personality Disorder; MBT, Mentalization Based Therapy; PDT, Psychodynamic Therapy; PFPR, Psychotherapy Focused on Psychic Representation; SchT, Schema Therapy; SCM, Structural Clinical Management; ST, Supportive Therapy; TAU, Treatment-as-usual; TC, Therapeutic Community; TFP, Transference- focused Psychotherapy; TFP, Transference-focused Psychotherapy; WL, Wait list.
Table 5: Results by diagnosis and psychotherapeutic intervention.
NA, Not Available; SR, Systematic Review; MA, Meta-analyses.
Diagnosis: BPD; Borderline Personality Disorder.
Psychotherapy: CAU, Care-as-usual; CBT, Cognitive Behavioral Therapy; DBT, Dialectical Behavioral Therapy; EHC, Existential Humanistic Cognitive Therapy; MBI, Mindfulness-based Interventions; MBT, Mentalization-based-Therapy; PATH, Problem Adaptation Therapy; PDT, Psychodynamic Therapy; PST, Problem Solving Therapy; SchT, Schema Therapy; ST-CI, Supportive Therapy for Cognitively Impaired Older Adults; ST, Supportive Therapy.
3. Results
3.1 Selection of studies
A total of 1590 studies were found, 1174 in the first search and 416 in the update. After eliminating duplicates and after screening of titles and abstracts, 53 were retrieved for further review. After full-text review, 38 studies were excluded due to noncompliance with the selection criteria, resulting in a total of 15 secondary studies. These were subsequently subjected to a detailed review in which the primary studies they included were also evaluated. After this exhaustive review, 8 studies were excluded due to repetition of research subjects and, finally, a total of 7 studies were selected for the extraction and qualitative analysis of the UR. The flow chart of the selection process and reasons for exclusion is shown in Figure 1.
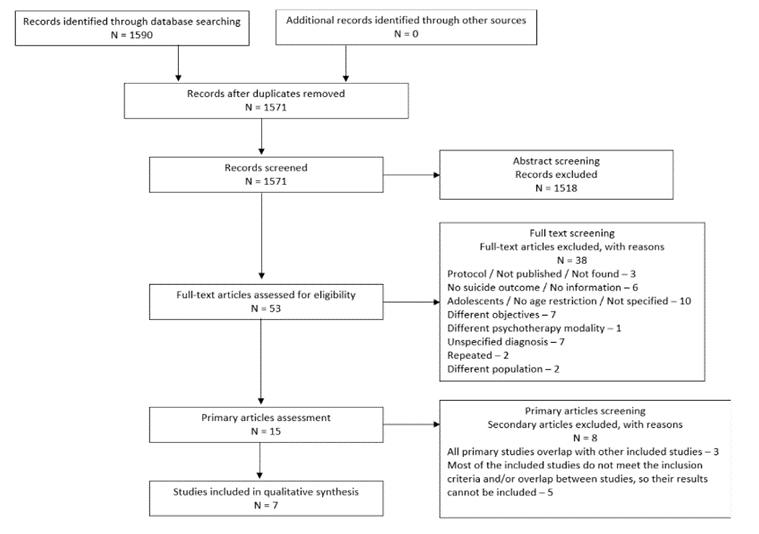
Figure 1: Flow chart of document retrieval
3.2 Characteristics of systematic reviews
The 7 selected studies were published between 2010 and 2022. Of the 7 selected studies, 5 are from the first search (Kroger et al 2010;) [20, 21, 22,23] and 2 from the update [24, 25]. Only the study by Cristea et al. 2017 also evaluates safety. Three studies [20, 22, 23] were conducted in patients with depression and 4 studies in patients with BPD (Kroger et al 2010) [21, 22,24]. The characteristics of the SR are shown in Table 1.
3.3 Evaluation of the quality of evidence
The quality of the evidence was assessed by two reviewers independently using the AMSTAR-2 tool. Two SR [21,24], were rated as low quality of evidence, mainly by failing to comply with the critical domains of explicitly stating the methods of the review prior to conducting the study and comprehensive literature review, respectively. One study [22] was rated critically low quality of evidence, failing to report the analysis of heterogeneity within the MA of the primary studies and the impact of their risk of bias on the interpretation of the results. The MA by Kroger et al. 2010 has moderate quality of evidence, indicating that, although it has some weaknesses, there are no flaws in the critical domains. The remaining studies [21, 22,25] were rated as high quality of evidence or low risk of bias. The results are shown in Table 2.
3.3 Efficacy of psychotherapies on suicide risk
The main characteristics of the studies on depression and BPD are listed in Table 3 and 4, respectively, including the clinimetric tools used to measure suicide related outcomes, summary results, and effect sizes. The total number of primary studies and included patients shown in the tables does not reflect the number of studies analyzed in this UR because not all of them focus on investigating the effect on suicidality. For the qualitative analysis, only the results on suicidality were considered, which are described below.
3.4 Depression
The SR by Okolie et al. 2017, evaluated the effectiveness of interventions to prevent suicide defined as “suicidal behavior (suicide, suicide attempt, self-injury)” and reduce “suicidal ideation” in older adults (>60) with depression and/or other disabilities. Only 3 of the 21 studies included evaluated psychotherapies, two randomized controlled trials [26, 27] and one quasi-experimental study [28]. Gustavson et al. results showed significantly greater reductions in suicidal ideation in older people with MDD and executive dysfunction who received 12 weekly sessions of PST or Supportive Therapy (ST) at 12 weeks (OR: 0.50, Z=-2.16, p=0.031) and 36 weeks (OR: 0.50, Z=-1.96, p=0.05) post-treatment. Single people were less likely to show improvement in suicidal ideation (OR: 2.5, Z=2.10, p=0.036) and disabled participants were more likely to show improvement (OR: 1.05 per unit increase in WHODAS, Z=2.03, p=0.042). At 36 weeks, there was a significant effect for age (OR: 0.57 per decade, Z=-2.59, p=0.01), and those who were younger were less likely to be suicidal. Kiosses et al. examined the effects of Problem-Adaptation Therapy (PATH) and Supportive Therapy for Adults with Cognitive Impairment (ST-CI) in older adults with MDD and dementia. Both treatments were found to have comparable reductions in suicidal ideation in participants after 12 weeks (time: F[1, 95.8]=10.06, p=0.0020). However, there was no significant difference in the course of suicidal ideation between PATH and ST-CI (time by treatment interaction: F[1, 95,8]=0.75, p=0.3897). Konradt et al. investigated the efficacy of humor group therapy (HGT) in older patients with MDD and reported improvements in suicidality in both intervention participants and untreated controls (main effect: F=21.65, p<0.001).
The SR and MA by Cuijpers, et al. 2013, studied the effect of psychotherapy on suicidality on adults with depressive disorder. Only 3 of 13 randomized trials included evaluated the effect of psychotherapy vs. a control condition on “suicidal ideation or suicide risk”. Two evaluated CBT, one against waiting list (WL) and Existential Humanistic Cognitive Therapy [29] and one against usual treatment [30] the last compared mindfulness-based CBT against usual treatment [31]. Four comparisons between a psychotherapy condition and a control condition resulted in a mean effect size g=0.12 (95%CI -0.20-0.44), not significantly different from zero. Heterogeneity was low (I2=30.81) and not significant. According to a post hoc power calculation these studies had sufficient statistical power to find an effect size of g=0.47. The combined results indicated very small and nonsignificant effects on suicidality, but there was too little statistical power to consider this as the true effect. The quality of the included studies and the low levels of suicidality of patients included in these studies possibly influenced the effect size, besides, the studies did not specifically target suicidal patients with depression. They conclude that there is insufficient research to establish whether or not psychotherapy for adult depression has an effect on suicidality.
The systematic MA by Schmelefske et al. 2020, evaluated the effectiveness of MBIs in the treatment of suicide defined as “suicidal ideation and/or behaviors”. Although there was no age restriction and diagnosis was not an inclusion criterion, a subgroup analysis was performed where the effect size on suicidality was calculated in a subgroup of 5 studies of adult patients with depression. None of the 13 studies included provided outcomes on suicidal behaviors, whereas all reported data on suicidal ideation. In the 5 studies using samples of individuals with depressive disorders [31, 32, 33, 34, 35] MBIs were found to have a significant moderate effect, Hedges' g=0.45 (95%CI [0.28, 0.62], p<0.001). In controlled studies, MBIs were found to have significant moderate effects in studies with depressive samples (k=4), Hedges' g=0.44 (95% CI [0.20, 0.68], p<0.001) without heterogeneity (I2=0.00%, Q=0.61). They concluded that MBIs have significant effects on suicidal ideation as well as on psychological outcomes associated with suicide (e.g., depression). Although MBIs appear to elicit significant increases in mindfulness, more research is needed to understand the mechanisms through which MBIs lead to a decrease in suicidal ideation and other related clinical outcomes.
3.5 Borderline personality disorder
The study by Rameckers et al. 2021, evaluated the efficacy of psychotherapies in adults (≥18) with a primary diagnosis of BPD through a multilevel MA. The outcomes assessed included the BPD symptom domain, where "suicidality/self-harm" was considered. A total of 87 studies were included. Of the outcomes related to suicidality, with large effect sizes, SchT (g=1.161, 95%CI [0.669, 1.653], p=0.013) and Mentalization-based Therapy (MBT; g=0.872, [0.612, 1.132], p=0.042) were strongly associated with greater reductions in suicidality compared to the average treatment effect. No improvement in suicidality was reported with any other type of psychotherapy.
The SR and MA of Stoffers-Winterling et al. 2022 evaluated the effect of standalone and adjunctive psychotherapeutic treatments on adults with BPD in comparison with active treatments and nonspecific control conditions. “Self-injury” and “suicide related outcomes (suicidal ideation and behavior)” were included as part of the primary outcomes. Twenty of the 32 RCTs included investigated standalone treatments and were considered for this UR: DBT (n=10), MBT (n=4), Interpersonal Therapy Adapted for BPD (IPT-BPD; n=2), CBT (n=2) and DDP (n=2), however, only 3 DBT RCTs and 4 MBT RCTs reported statistically significant results on suicidality. For DBT, statistically significant moderate to large effects were observed for self-harm (SMD -0.54, p=0.006, 95%CI -0.92 to -0.16, n=3 studies, n=110 participants, I2=0%). Statistical heterogeneity was marginal for all these effect estimates (0-5%). MBT was evaluated in 4 studies. The risk of self-harm (Risk ratio [RR] 0.51, p<0.0007, 95%CI 0.34-0.75, n=2 studies, n=172 participants) or suicide-related outcomes (RR 0.10, p<0.0001, 95%CI 0.03-0.32, n=2 studies, n=172 participants) was significantly lower in MBT-treated groups (statistical heterogeneity 0% for both estimates). In conclusion, statistically significant effect estimates supported by low quality of evidence, were only found for DBT (self-harm) and MBT (self-harm, suicide-related outcomes).
The SR and MA of RCTs by Cristea et al. 2017 evaluated the efficacy of psychotherapies in the adult BPD population randomized to psychotherapy exclusively or to a control intervention. Study selection differentiated stand-alone psychotherapies (22 of 33 studies included) compared with control interventions from add-on designs (experimental intervention added to treatment as usual [TAU]) compared with TAU alone. Suicidality was assessed in the outcomes described as BPD symptoms, self-injury and suicidality. The most represented approaches were DBT (N=12), PDT (N=8) and CBT (N=5). The subgroup analyses were conducted on “all borderline-relevant outcome” category (BPD symptoms, self-harm and parasuicidal behavior, and suicide) combining stand-alone and add-on designs because no differences were found between them. DBT (g=0.34; 95%CI, 0.15-0.53 [9 trials]) and PDT (g=0.41; 95%CI, 0.12-0.69 [7 trials]) were more effective than control interventions, whereas CBT (g=0.24; 95%CI, -0.01 to 0.49 [5 trials]) and other interventions (g=0.38; 95%CI, -0.15 to 0.92 [6 trials]) were not. The difference between effect sizes in the subgroups were not significant (p=0.87). No differences were found between the types of psychotherapies. Most trials focused on DBT followed by PDT, and both types generated significant and small effect sizes between groups, with low heterogeneity for DBT. CBT was not superior to control conditions, although this result was based on only five trials, heterogeneity was low. Nonetheless, effects are small, inflated by risk of bias and publication bias, and particularly unstable at follow-up.
The MA by Kröger et al. 2010 examined the long-term efficacy and effectiveness of DBT in adults (≥18) with BPD through a hierarchical mixed-effects modeling approach. Effect sizes for “suicidal and self-injurious behaviors” were calculated. Calculations of post-intervention were based on 16 studies (8 RCTs and 8 neither randomized nor controlled trials [nRCTs]). Suicide behaviors and suicide attempts were included. After discarding studies that did not report rates for calculating odds ratios or reported no effects on self injurious behaviors, 11 of 16 studies were included for analysis. Suicidal and self-injurious behaviors were not inclusion criteria for the remaining studies, so a dichotomous moderator that characterizes studies examining samples with high rates of self-injurious behaviors (k=6) was used. A total of 643 patients in treatment were included, 377 of these treated with DBT, with a dropout rate of 28.5% and 27.3%, respectively between preintervention and postintervention. Analysis of only RCTs (k=6) resulted in an effect size estimate of 0.23, 95%CI [-0.00, 0.46], t(5)=1.93, p= 0.110 (two-tailed) in suicidal and self-injury behaviour outcome. While including the moderator considering the impact of controlled RCTs of specific BPD treatments [36, 37] yields an effect size estimate of 0.60, 95%CI [0.49, 0.71], t(4)=10.61, p>0.001 (two-tailed). Addition of nRCT (k=5; number of patients treated=142, after dropout=99) resulted in an effect size estimate of 0.37, 95%CI [0.17, 0.57], t(10)=3.59, p=0.006 (two-tailed), with no evidence of bias trends for nRCTs, x2(1)<0.28, p=0.597. Including the moderator considering the impact of controlled RCTs of BPD-specific treatments [36, 37] yields an effect size estimate of 0.56, 95% CI [0.52, 0.60], t(9)=27.04, p>0.001 (two-tailed). There was no significant unexplained between-study variation (H=3.3, df=9, p=0.951). In conclusion, they found a moderate overall effect and a moderate effect size for suicidal and self-injurious behaviors when including a moderator for RCTs with specific treatments for BPD. It is important to mention that the results report self-injurious and suicidal behaviors together which, from the characteristics of the included studies, it can be assumed that the results encompass suicide attempts and self-injury without suicidal intent together within the same effect size, whereas suicidal ideation is not measured. This is the only study on BPD in which the outcome measure for the effect on suicide risk are described.
3.6 Safety of psychotherapy in patients at risk of suicide
Only the SR by Cristea et al. 2017 described safety data on psychotherapeutic interventions. Adverse effects were defined as participant death by suicide and death from any cause after randomization. They report that adverse effects were rare in both the experimental treatment and control groups. Likewise, 2 and 5 deaths by suicide were reported in the treatment and control group, respectively. Six deaths from all causes were reported in each group. However, it is not stated whether the suicide deaths in the treatment group were due to adverse effects of the intervention, and it is not specified in which psychotherapeutic interventions they occurred.
4. Discussion
Table 5 shows a summary of the findings of this UR, which describes the measures of suicidality evaluated by the included SR and MA, the psychotherapies evaluated, the outcomes and the number of primary studies on which those are based.
4.1 Major depressive disorder
Of the psychotherapies studied in patients with a diagnosis of depression, only PST and MBI showed statistically significant improvement on suicidal ideation. The SR by Okolie et al. 2017 was the only study carried out in the elderly population where only the included study by Gustavson et al. 2016 showed a significantly greater reduction in suicidal ideation with PST compared to ST in MDD and executive dysfunction. Only 1 primary study [31] is repeated in 2 of the 3 depression studies selected for this UR [20, 23], where the intervention studied is mindfulness-based CBT; Cuijpers et al. included it within CBT interventions while Schmelefske et al. within the MBI. In the case of CBT vs control conditions, the effect size was small and non-significant on “suicidal ideation and suicide risk” although heterogeneity was low, while MBI vs control interventions obtained a statistically significant moderate effect on suicidal ideation. Therefore, effect on suicidal ideation by CBT, PST, and MBT are based on 3, 1, and 5 primary studies, respectively. More trials are needed to support these outcomes, since statistical power may be influenced by the small number of studies included, few studies addressing the elderly population, most of the studies included in the SR by Okolie et al. were of low quality of evidence, not all studies included in the MA by Cuijpers et al. focused on suicidal patients, and Cuijpers et al. and Schmelefske et al. both were rated as low quality of evidence, so the results of these studies may not represent an accurate and complete summary of the results in the included primary studies.
4.2 Borderline personality disorder
The results of the MA by Rameckers et al. 2021 revealed that SchT and MBT were strongly related to greater reductions in suicidality compared to TAU, based on 8 primary studies for each psychotherapeutic approach, although it is worth mentioning that it encompasses “suicidality/self-harm” in general, without specifying what exactly is evaluated (self-harm, ideation or suicide attempts), likewise, it is not specified how many of these 16 studies evaluate suicidality in their results. It is important to remark that of the studies of BPD included in this UR, this is the one that covers the most primary studies and evaluates the effectiveness of multiple psychotherapeutic interventions on BPD more broadly so, many of the primary studies included here overlap in the rest of the secondary studies included in this UR, also it analyzes the most DBT studies, a total of 41, although it did not specify how many of these assessed suicidality. Likewise, the critically low quality of evidence of this MA, which translates into low reliability of the study, compromises the confidence in the results. Although, it was decided to include it because it is the only one that analyzes the effectiveness of SchT, this approach being one of which showed improvement in suicidal tendencies, in addition to the fact that despite repeating a large part of the studies on DBT within the rest of the SR and MA included, the results obtained were different from the other studies, so it is important to describe the possible causes of this, as detailed below. There was no significant improvement in suicidality in the analysis of studies evaluating DBT. In contrast, when evaluating DBT, Stoffers-Winterling et al. observed statistically significant moderate to large effects on self-harm based on 3 primary studies with 0% heterogeneity, as did Kroger et al. with moderate effect size for suicidal and self-injurious behaviors based on 11 primary studies. This could be because in the last two suicidality was assessed more specifically as self-harm or suicidal and self-injurious behaviors, while Rameckers et al. measured unspecified “suicidality”. Or perhaps this difference is due to the effect sizes of the studies that do not overlap between secondary studies, however, it is difficult to know as it is not mentioned which of the primary studies by Rameckers et al. measure suicide risk. MBT also showed large effect sizes with larger reductions in suicidality, findings consistent with those described by Stoffers-Winterling et al., this is to be expected because the 4 primary studies considered in the latter are also included by Rameckers et al. 2021, although Stoffers-Winterling et al. do make a distinction between the suicidality characteristics evaluated, demonstrating improvement in “self-harm” and “suicide-related outcomes (suicidal ideation and suicide behavior” with 2 primary studies for each of these suicidality sub classifications and 0% heterogeneity for both estimates. Although both secondary studies agreed in their results, the findings of the study by Rameckers et al. could also shed clarity on the importance of specifying which aspects of suicide risk are measured when evaluating efficacy on suicidality. Although the study by Cristea et al. showed significant and small effect sizes between groups for DBT and PDT, with low heterogeneity for DBT, it's important to note that it was decided to extract the result that most closely matches the objective of the UR and it was "relevant outcomes in BPD" where not only measures of suicidality are included, but also symptomatology, this because the analysis of suicidality separately does not show specific results by type of psychotherapy, and the aim of the UR is to see the psychotherapies with greater evidence of decreased suicidality. In summary, the four studies provide evidence for the effectiveness of certain psychotherapies, such as SchT, MBT, PDT, and DBT, in reducing suicidal behaviors and self-harm in adults with BPD. These results are promising, but it is critical to consider the limitations of each study and the need for future research to fully understand the factors that influence the effectiveness of these therapies in this specific population.
4.3 Strengths and limitations
This is, to our knowledge, the first UR that synthesizes the existing evidence that has been reported in MA and SR on the efficacy and safety of psychotherapeutic interventions on suicide risk in psychiatric patients. Having considered the overlap of primary studies and their inclusion criteria in the selection process made it possible to exclude secondary studies in which all primary studies were repeated, which avoids inflating results or presenting redundant information, also giving rise to the interpretation of the information extracted as part of the discussion and general conclusions of this UR based on a broad set of empirical evidence. This study has some limitations. First, the large number of studies excluded because they do not meet inclusion criteria; second, it would have been relevant to include “hopelessness” in our search strategy and consider it as another form of suicide risk since it has been considered an important risk factor; third, the quality of the evidence of the studies included, where 2 of the studies on depression have low quality of evidence, while the largest study on BPD has critically low evidence, thus compromising the reliability of these studies and the results they describe. Finally, only the 3 studies of depression focused on measuring the effect of interventions on suicidality, yet within the analysis studies of patients with suicidal tendencies were not always exclusively included, but the global improvement was measured including results related to suicide, so this may have an impact on the results obtained and consequently on the conclusions of the secondary studies.
4.4 Implications
The heterogeneity between secondary studies were different definitions of age groups, diagnostic classifications, intervention modalities, and definitions and measurements of suicidality, were considered as the main challenge of the present UR, which reinforces the need to carry it out. Only MBT, DBT, PDT and SchT stand out as promising treatments to reduce the risk of suicide in those over 18 years of age with BPD, in addition to MBI and PST (based on a single study) in depression, this was mainly true when suicidality was sub classified into suicidal ideation, suicidal behavior and self-harm, as described in the case of DBT. The findings of the UR reflect the existence of a large amount of evidence that has been synthesized and analyzed in secondary studies that, although they provide very valuable information about the effect of psychotherapies in the psychiatric population, when evaluating “suicidality” the results can be inconsistent, even taking into account that to a large extent these results come from the analysis of the same primary studies that are repeated. This is precisely what justifies carrying out an UR, in order to offer a more global overview of the existing evidence and thus facilitate decision making by better translating the evidence into practice and/or providing valuable information about what is known and what remains unknown. The findings of this review make it possible to clarify that despite there being so many psychiatric diagnoses, types of psychotherapy and research that studies them, there are few psychotherapeutic approaches whose effectiveness can be assured with greater certainty in this risk population with an established diagnosis. However, this also gives us information that allows us to consider the possibility that this is due more to methodological issues than an apparent lack of effectiveness, understanding that these inconsistencies of the results are secondary to the challenge of defining and quantifying concepts as complex as “suicidality”. It is expected to assume that as more conditions or more specific subtypes of the already existing ones continue to be described, new tools or modifications to already existing scales will continue to be developed, this is a sign of the progress in research and understanding of psychiatry. Therefore, trying to establish a single scale as a standard measure for research purposes and to maintain it over time would be unlikely. A viable proposal is that when measuring “suicidality” they are subclassified into self-harm, suicidal ideation and suicidal behavior taking into account that there are scales that contemplate each of these. Considering “self-injury” separately from suicidal behavior since it is not always done for the purpose of suicide, in addition to the fact that it occurs more in certain psychiatric diagnoses (e.g. personality disorders) and taking as “suicidal behavior” everything that encompasses the different types of suicide attempts (e.g. interrupted or aborted attempts). Since when considered as a whole, “suicidality”, “parasuicidal behavior” or “suicidal tendency” is possible that it could yield unfavorable results, but when subclassified it could imply a decrease in the frequency of self-harm, suicidal attempts or ideation, which can also translate into an improvement in the patients' expectancy and quality of life, thus avoiding the risk of wrongly discarding the intervention studied due to an apparent lack of effectiveness, in addition to the fact that it could shed light on what type of intervention to offer depending on the predominance of the type of suicide risk present. The same applies to safety, where it is possible that the results are favorable if they are measured together when perhaps this is not the case for all forms of suicide risk, which would make it more complicated to choose an appropriate and more individualized intervention. It is also important to describe the age group, diagnosis and comorbidities present, since this can impact decision-making regarding the most appropriate prognosis and intervention for patients at risk. It is necessary to consider, as part of the variables to be evaluated when investigating psychotherapies, the safety of the intervention. The lack of evidence on this aspect is clear. The most important aspects to report would be worsening of symptoms, completed suicides, increase in frequency and intensity of suicidal ideation, self-harm and/or suicidal behavior, based on clinical judgment or with the support of scales.
5. Conclusion
Analysis of psychotherapies in patients with MDD reveals that PST and MBI show statistically significant improvements in reducing suicidal ideation, although these results are based on a limited number of primary studies. In the analysis of BPD, it is observed that SchT can be especially effective in reducing unspecified suicidality, while MBT can be effective on “self-harm” and “suicidal ideation and behavior”. Although DBT is the most studied approach, the lack of specificity in the assessment of suicidality in some studies raises the need for a more detailed approach to fully understand the therapeutic effects by showing no significant effects in one of the studies, although, it was rated as critically low quality of evidence, while the other studies highlight its possible effectiveness in reducing suicidal and self-injurious behaviors, as well as PDT. These findings are promising but underline the importance of future research to further clarify the factors that influence the effectiveness of these therapies in specific populations, considering the need for more detailed evaluation of suicidality in studies [38-47]. There is no information regarding the safety of psychotherapeutic interventions, which raises the importance of more research on this.
Funding Statement:
None
Acknowledgements
None
References
- Kuyken W. Cognitive therapy outcome: the effects of hopelessness in a naturalistic outcome study. Behaviour Res Therapy 42 (2018): 631-646.
- National Action Alliance for Suicide Prevention: Research Prioritization Task Force. A prioritized research agenda for suicide prevention: An action plan to save lives. Rockville, MD: NIMH Research Prioritization Task Force (2014).
- Hawton K, Saunders K A, C O'Connor R. Self-harm and suicide in adolescents. Lancet 379 (2012): 2373-2382.
- Brunner RK, Kaess M, Parzer P, et al. Life-time prevalence and psychosocial correlates of adolescent direct self-injurious behavior: a comparative study of findings in 11 European countries. J Child Psychol Psychiatry 55 (2014): 337-348.
- Kendall T, Taylor C, Bhatti H, et al. Longer term management of self-harm: summary of NICE guidance. BMJ 343 (2011).
- Hawton K, Bergen H, Cooper J, et al. Suicide following self-harm: findings from the Multicentre Study of self-harm in England, 2000-2012. J Affect Dis 175 (2015): 147-151.
- Lara J, Cox M. A Longitudinal Study of Nonsuicidal Self-Injury in Offspring at High Risk for Mood Disorder. J Clin Psychiatry 73 (2012): 821-828.
- De Leo D, Burgis S, Bertolote JM, et al. Definitions of suicidal behavior: lessons learned from the WHo/EURO multicentre Study. Crisis 27 (2006): 4-15.
- Crosby A E, Ortega L, Stevens M R, et al. Suicides - United States, 2005-2009. MMWR suppl 62 (2013): 179-183.
- NICE N I. Self-harm: assessment, management and preventing recurrence. NICE guideline (2022).
- Hawton K, Arensman E, Gunnell D, et al. Interventions for self-harm in children and adolescents. Cochrane Database Syst Rev 2015 (2015).
- Hawton K, Arensman E, Gunnell D, et al. Psychosocial interventions for self-harm in adults (Review). Cochrane Database Syst Rev 2016 (2016).
- Koenigsberg H, Mitropoulou V, Schmeidler J, et al. Characterizing affective instability in borderline personality disorder. Am J Psychiatry 159 (2002): 784-788.
- Crowell SE, Beauchaine TP, Linehan M M. A biosocial developmental model of borderline personality: Elaborating and extending Linehan's theory. Psychol Bull 135 (2009): 495-510.
- Driessen E C, Lisa L M Hegelmaier Abbass A A, et al. The efficacy of short-term psychodynamic psychotherapy for depression: a meta-analysis. Clin Psychol Rev 30 (2015): 25-36.
- Linehan M, Comtois K A, Murray A M et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch General Psychiatry 63 (2006): 757-766.
- Bateman A. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. Am J Psychiatry 156 (1999): 1563-1569.
- Bateman A. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry 166 (2009): 1355-1364.
- Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358 (2017): j4008.
- Cuijpers P, de Beurs DP, Van Spijker BA, et al. The effects of psychotherapy for adult depression on suicidality and hopelessness: A systematic review and meta-analysis. J Affective Dis 144 (2013): 183-190.
- Cristea IA, Gentili C, Cotet C D, et al. Efficacy of Psychotherapies for Borderline Personality Disorder. JAMA Psychiatry 74 (2017): 319.
- Okolie C, Dennis M, Simon Thomas E, et al. A systematic review of interventions to prevent suicidal behaviors and reduce suicidal ideation in older people. Int Psychogeriatrics 29 (2017): 1801-1824.
- Schmelefske E, Per M, Khoury B, et al. The Effects of Mindfulness-Based Interventions on Suicide Outcomes: A Meta-Analysis. Arch Suicide Res 26 (2020): 447-464.
- Rameckers SA, Verhoef REJ, Grasman RPPP, et al. Effectiveness of Psychological Treatments for Borderline Personality Disorder and Predictors of Treatment Outcomes: A Multivariate Multilevel Meta-Analysis of Data from All Design Types. J. Clin. Med 10 (2021): 5622.
- Stoffers-Winterling J M, Storebø O J, Kongerslev M T, et al. Psychotherapies for borderline personality disorder: a focused systematic review and meta-analysis. British J Psychiatry 221 (2022): 538-552.
- Kiosses D N, Rosenberg P B, Mcgovern A, et al. Depression and suicidal ideation during two psychosocial treatments in older adults with major depression and dementia. J Alzheimer’s Disease 48 (2015): 453-462.
- Gustavson K A, Alexopoulos GS, Niu GC, et al. Problem-solving therapy reduces suicidal ideation in depressed older adults with executive dysfunction. Am J Geriatric Psychiatry 24 (2016): 11-17.
- Konradt B, Hirsch R D, Jonitz M F, et al. Evaluation of a standardized humor group in a clinical setting: a feasibility study for older patients with depression. Int J Geriatric Psychiatry 28 (2013): 850-857.
- Collins RW. The Treatment of Depression: An Integrative Psychotherapy Model. Doctoral Dissertation. Saybrook Institute, San Fransisco (1996).
- Duarte PS, Miyazaki MC, Blay SL, et al. Cognitive-behavioral group therapy is an effective treatment for major depression in hemodialysis patients. Kidney International 76 (2009): 414-421.
- Barnhofer T, Crane C, Hargus E, et al. Mindfulness-based cognitive therapy as a treatment for chronic depression: a preliminary study. Behaviour Res Therapy 47 (2009): 366-373.
- Barnhofer T, Crane C, Brennan K, et al. Mindfulness-based cognitive therapy (MBCT) reduces the association between depressive symptoms and suicidal cognitions in patients with a history of suicidal depression. J Consult Clin Psychol 83 (2015): 1013-1020.
- Crane C, Barnhofer T, Duggan DS, et al. Mindfulness-based cognitive therapy and self-discrepancy in recovered depressed patients with a history of depression and suicidality. Cognitive Therapy Res 32 (2008): 775-787.
- Forkmann T, Brakemeier E L, Teismann T, et al. The Effects of mindfulness-based cognitive therapy and cognitive behavioral analysis system of psychotherapy added to treatment as usual on suicidal ideation in chronic depression: Results of a randomized-clinical trial. J Affective Dis 200 (2016): 51-57.
- Forkmann T, Wichers M, Geschwind N, et al. Effects of mindfulness-based cognitive therapy on self-reported suicidal ideation: Results from a randomised controlled trial in patients with residual depressive symptoms. Comprehensive Psychiatry 55 (2014): 1883-1890.
- Clarkin J F, Levy K N, Lenzenweger M F, et al. Evaluating three treatments for borderline personality disorder: A multiwave study. Am J Psychiatry 164 (2011): 922-928.
- McMain S F, Links P S, Gnam W H, et al. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. Am J Psychiatry 166 (2009): 1365-1374.
- APA A P. Conditions for Further Study: Suicidal Behavior Disorder. American Psychiatric Publishing.(2013): 801-803.
- Binks CA. Pharmacological interventions for people with borderline personality disorder. The Cochrane database of systematic reviews (2006).
- Black D W. Comparison of low and moderate dosages of extended-release quetiapine in borderline personality disorder: a randomized, double-blind, placebo-controlled trial. Am J Psychiatry 171 (2014): 1174-1182.
- Giesen-Bloo J V, Dyck R V, Spinhoven P, et al. Outpatient psychotherapy for borderline personality disorder: randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry 63 (2006): 649-658.
- Kliem S, Kröger C, Kosfelder J. Dialectical behavior therapy for borderline personality disorder: A meta-analysis using mixed-effects modeling. J Consult Clin Psychol 78 (2010): 936-951.
- Linehan M C, Guilford: New York NU. Cognitive Behavioral Therapy of Borderline Personality Disorder; Guilford: (1993).
- Linehan M, Suarez A, Allmon D, et al. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry 48 (1991): 1060-1064.
- Paris J. The Treatment of Borderline Personality Disorder, New York, USA: The Guildford Press (2012).
- Stoffers-Winterling J, Völlm B, Rücker G, et al. Psychological interventions for borderline personality disorder. Cochrane Library (2012).
- Preventing suicide. A global imperative (2014).
