Effectiveness of Virtual Reality Vs Standard Physical Therapy on Range of Motion, Pain and Enjoyment in Patients with Acute Burns: A Meta-Analysis and Evidence Based Review
Article Information
Nupur Hajela*, Mercedes Dobson-Brazier, Jenna Sawdon Bea
Department of Physical Therapy, California State University, Fresno, California, United States
*Corresponding author: Nupur Hajela, Assistant Professor, Department of Physical Therapy, California state University, Co-Director Gait Balance and Mobility Clinic, Director, Rehabilitation Technology and Outcomes Research, California Sports Science Institute, 5315 Campus Drive M/S PT29, Fresno, CA 93740-8031, USA
Received: 17 January 2022; Accepted: 25 January 2022; Published: 02 February 2022
Citation: Nupur Hajela, Mercedes Dobson-Brazier, Jenna Sawdon Bea. Effectiveness of Virtual Reality Vs Standard Physical Therapy on Range of Motion, Pain and Enjoyment in Patients with Acute Burns: A Meta-Analysis and Evidence Based Review. Archives of Clinical and Biomedical Research 6 (2022): 94-118.
View / Download Pdf Share at FacebookAbstract
Background: Each year 1.1 million people report having a burn injury, with 45,000 people requiring hospitalization. Patients suffering from a burn, experience one of the most excruciating types of pain, that is most commonly unsuccessfully treated though analgesics. Physical therapy increases a patient’s pain thus decreasing a patient’s compliance with treatment and willingness to move. Virtual reality has been proven to decrease burn pain, but there is limited information on the effects it has on range of motion and treatment enjoyment. The purpose of this study is to determine the effectiveness of VR as a treatment tool to increase ROM and enjoyment as part of cognitive distraction while decreasing reported pain when compared to standard physical therapy in patients with acute burns.
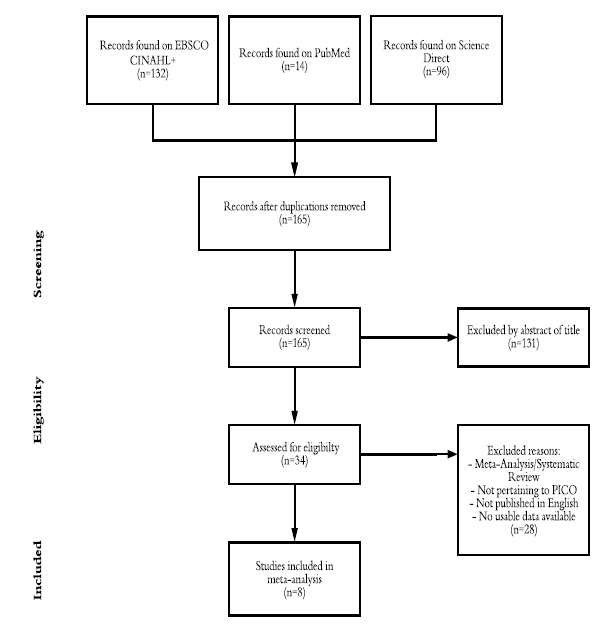
Methods: The search between Science Direct, Cinahl and PubMed yielded a total of 242 articles in total which were reviewed based on relevance of titles and abstracts. Prior to reviewing abstracts there were 77 duplicates removed, leaving 165 non-duplicate articles. There were 131 articles removed after reading the abstract and finding the articles did not fit within the meta-analysis leaving 34 articles left to review for inclusion/exclusion criteria. After reviewing the articles, 8 studies eligible for this metaanalysis based on the inclusion and exclusion criteria were analyzed though Microsoft Excel. The studies were used for the following three outcome measures: range of motion, pain and enjoyment.
Results: Range of motion presented with homogenous results with a grand effect size of 0.19. Pain was found to have homogeneity with grand effect size of -0.45. Enjoyment was the only outcome measure that presented with heterogeneity and a grand effect size of 1.30. Virtual reality was proven to be an effective way to decrease pain and improving enjoyment. Range of motion had a trend to favoring virtua
Keywords
Immersive VR, Physical Therapy, Pain, Virtual Reality, Cognitive Distraction Therapy, Burns
Immersive VR articles; Physical Therapy articles; Pain articles; Virtual Reality articles; Cognitive Distraction Therapy articles; Burns articles
Article Details
1. Introduction
Burns are a common occurrence, with reports of burns affecting more than 1.1 million people each year, with the potential of more incidences that go unreported [1]. Of the populations of reports of burns, only 45,000 people required hospitalization from their burn injury with the length of stay averaging 17.9 days [1, 2]. Patients with burns experience one of the most excruciating types of pain a person can experience. The pain is made worse with procedural movements during physical therapy, which in turn decreases compliance with physical therapy [3-5]. Having pain this extreme can have an effect on any person physically, emotionally, psychologically, and cognitively [3, 6]. When a person is in pain it can affect the amount of movement the patient is willing to complete to do in order to prevent an increase in pain. Having high levels of pain can affect a person emotionally by creating high levels of stress which in turn can cause fear, terror and caution. This response can activate the body’s stress response [1]. High levels of pain can affect a patient psychologically and cognitively through mediating improper responses to outside stimulus [6]. The patient has also gone through a traumatic event causing their pain, therefore having increased levels of pain can bring them back to the traumatic event. A Physical Therapist’s goal is to improve a client’s function through movement and prevent contractures; however, when a patient is in excruciating pain it can be nearly impossible to motivate patients to move [7]. With this population early movement is imperative for faster recovery time, prevention of decreased functional mobility, surgical releases of contractures, and overall better quality of life [4, 7, 8]. Therefore, a treatment tool that can help encourage movement, while decreasing pain, is crucial to make physical therapy treatment more effective and tolerable for the patient [5, 9]. Current standard physical therapy does not include treatment options that decrease pain other than analgesics. Virtual reality (VR) is a tool that is capable of encouraging movement and decreasing pain by providing a level of distraction for the patient, allowing them to spend less time thinking about their pain and more time gaining movement of the affected area.
1.1 Burn etiology and pathology
A burn is an injury to organic tissue caused by a noxious stimulus of heat, cold, radiation, radioacti- vity, electricity, friction or contact with chemicals. When a burn occurs, there is a cellular and systemic change throughout the body. As a result of a burn, cells within the skin layers will either become damaged or die. The different cellular elements housed in the skin layers are affected through the noxious heat stimulus. When there is a noxious heat stimulus the brain receives signals of the potential danger from the dorsal horn of the spinal cord through A-delta and C fiber neurons [7]. The effects of burns are dependent on the level of skin which the burn penetrates. The deeper the burn the more damage is caused to the cells, nerve endings and vessels [1]. The skin becomes more fibrous and less elastic with each layer of damage. Along with cellular changes, patients experience an increase in edema secondary to damaged blood vessels allowing for an increase in permeability [1]. Range of Motion (ROM) is severely affected with increased edema, vascularity, fibroblast, and collagen; which can lead to contractures [7, 10, 11]. Contractures are excessive scar formation due to the overabundance and disorganized collagen formation, leaving the skin of the affected area inelastic [11]. Another important factor limiting a patient’s ROM is severe pain caused by damaged or exposed nerve endings.
Nerve endings sustain damage when the burn reaches the dermis and are completely obliterated when damage occurs in all the layers of the skin [5]. When the nerve fibers become damaged the body reacts to stimulus differently. For example, a patient may develop thermal allodynia, an abnormal response to a thermal stimulus. With exposed and damaged nerve fibers a person will have excruciating background and procedural pain. Background pain is present during rest caused by the inflammatory response [7]. Procedural pain is pain caused by movement whether active or passive [5, 7]. Physical therapy is a major contributor to procedural pain and is often excru- ciating, limiting the amount of motion to the effected joint. Burns are classified through mechanism of injury, size calculated through total body surface area (TBSA), and depth of burn [1]. Mechanism of injury is the type of stimulus that caused the burn such as chemical, thermal, and electrical [12]. The mechan- ism of injury plays a minimal role in the treatment of a burn. TBSA plays a significant role in burn treatment and is considered the gold standard. TBSA is a percentage of the body that is affected by all burns, with the exception of superficial burns. To calculate the TBSA, clinicians use the rule of nines, which is a simple formula that breaks down different segments of the body into either 4.5, 9, or 18% of the total body [13]. The rule of nine differs from the pediatric to adult population to account for the difference in segmental ratios [13].
There are four categories for depth of burn: superficial, partial-thickness, deep-thickness, and full thickness [1]. Superficial burns involve the first layer of skin, epidermis [13]. When the epidermis is burned most sensory receptors and all blood vessels remain intact thus causing pain but allowing the area to heal without extensive treatment [13]. The next level is partial-thickness burns which involve the epidermis and papillary level of the dermis. These burns will be characterized with extreme pain, and inflammation [5, 13]. As the burn injury extends deeper into the dermis reaching the reticular layer, it is categorized as a deep-thickness burn. Pain is reduced because the nerve endings are destroyed, but there is more inflammation [1, 13]. The last category of depth is a full thickness burn which includes all levels of the skin and any layer between the subcutaneous to the bone [1]. This is the most extreme level of burn and kills all tissue, vessels and nerve fibers in the area making this category pain free [1, 13]. When the burn patient arrives at the hospital there is a team of medical professionals that begin treatment immediately. This team can include nurses, occupational therapists (OTs), recreation therapists, social workers, dieticians, psychiatrists, and physici- ans. Each team member provides critical information to develop a plan of care to allow the patient the best possible outcome after a traumatic injury. While physical therapy is one aspect of care that a patient will receive, it is imperative to regain function [14]. Physical therapists work closely with other profe- ssions to allow for the most effective treatment plan, such as working with the nursing staff to ensure the patient has received the proper medication prior to treatment. Since physical therapy causes an increase in pain, all patients utilize analgesics to help decrease pain [15-21]. During treatment a patient will partake in activates that are specialized to their unique plan of care [11, 14, 22]. In general, a plan of care can consist of active, active-assisted and passive ROM, ambulation, functional re-training for ADLs and IDLs, strength training, aerobic exercise, splinting, positioning, scar management, and pressure therapy [6, 10, 11, 15, 18]. For each patient the treatments are specific to their injury, previous level of activity, stage of healing and if grafts were required; however, all treatment has one common goal: improve functional movement [14]. To encourage improved function, patients are given management tools outside of treatment sessions such as positioning, splitting, and pressure garments.
During physical therapy treatments, a patient will receive some form of ROM, ambulation/aerobic training, functional re-training and strength training. ROM is incorporated in all treatments regardless of the location of the burn because this allows for prevention of contractures. This can include passive, active-assistive, or active ROM, depending on the range presented by the patient [14]. Completing ROM helps maintain the tissue length through joint mobility and tissue elasticity [10]. Aerobic exercise and ambulation is included in treatment to improve strength and aerobic capacity. This also allows can help the patient mentally by giving them a sense of confidence, achievement, and normalcy [6]. Ambulation also encourages full body movement ensure there is a whole body treatment. It is important not to neglect the unaffected areas in treatment as physical therapist for whole body wellness [6, 14]. To encourage whole body wellness, functional re-training is important. This includes having the patient participate in activities of daily living (ADLs) and functional task as early as possible. Involving the patient in ADLs not only improves the patient’s functional abilities but it also allows for independence. That independence can lead to better compliance with treatment and improve the patient’s self-esteem [6, 11, 14, 22].
1.2 Standard physical therapy
Positioning and splinting are important for all burn patients to prevent contractures of the affected area [11, 22]. Typically, patients have a tendency to position themselves in a position of comfort which allows the skin to harden in a shortened state forming contractures. There is a positioning chart that is utilized for proper patient positioning for each affected joint 14 In conjunction with positioning, splints are utilized to ensure proper placement is maintained. Splinting is not only encourages proper positioning but also allows protection to the affected skin [11, 14]. Outside of proper positioning and splinting, patients are given pressure garments. These are designed to help with edema and improve scar formation. Compression garments are worn approximately 23 hours a day, only removed for bathing or moisturizing [11]. The physical therapist’s main goal is to promote function and prevent long term damage such as contracture formation [9, 22].
1.3 Virtual reality
With the amount of pain, a person with a burn experience, the medical profession is continually looking for ways to decrease pain with non- pharmacological options. Pharmacological treatments tend to have negative side-effects, place the patient at risk of addiction and have been shown to be ineffective with procedural pain [5, 9, 15-21]. Cognitive distraction therapy has been used throughout burn care to ease the pain caused by procedural treatments. This type of therapy is noninvasive and nonaddictive making it a valuable treatment tool [9, 23]. VR is now being used as cognitive distraction, with great success in decreasing pain. VR is defined as computer generated simulation of images or environments that can be interacted with through the use of connected equipment such as a googles, handheld sensor or a motion detected camera [9, 18, 21]. VR has been studied using a functional magnetic resonance imaging (fMRI) in healthy adults and in burn patients to determine if VR is decreasing pain [24]. According to Hoffman et al., the “pain matrix” of the brain during VR has been shown to reduce the amount of pain during activity and change the interpretation of a painful stimulus [4, 24]. VR is able to affect the pain matrix by providing distraction to the brain and sensory pain neurons; the interpretations of incoming pain signals [4] The body can only process a limited amount of stimulus at once; therefore, when a patient is using cognitive distraction treatment the dorsal horn of the corticospinal tract is overloaded making it difficult for the spinal cord to send pain signals to the brain [3, 4, 8, 19]. Due to the analgesic affect, VR allows patients to begin early movement needed for an effective recovery [9, 16, 19, 21].
VR with interactive tasks require patients to move their limbs through space to complete the task. The movements necessary to complete these tasks typically require the participant to have functional ROM with reaching or stepping [18]. Additionally, VR provides an enjoyable treatment tool that patients are motivated and compliant to use [23]. With patients compliance, the results of treatment can translate into long-lasting recovery in all aspects of life such as emotional, cognitive, psychosocial and physical [3]. Throughout the year’s VR has expanded into different levels thus allowing for more alternatives when choosing the proper treatment tool, not only for the patient but for the facility. A therapist can decide which level of VR to use based on the desired outcomes. There are two forms of VR, immersive VR and augmented reality systems such as interactive gaming consoles (IGC) can be utilized. Immersive VR uses a head mounted display (HMD) and a handheld device to control the environment and complete the tasks [15, 20]. With the HMD, the patient will be completely immersed within the environment and blocked from environmental distractions [8, 15, 20]. IGCs consist of gaming consoles that allow the participant to interact with the video game through force plates, handheld controls or infrared cameras. These systems include Nintendo Wii, Xbox Kinect, and PlayStation EyeToy [16-18, 21]. Immersive VR is more expensive but has the capacity to be programmed to accomplish the goals of the therapist. ICGs are more cost effective; however, are not as flexible with treatment options [8, 16, 21]. Both options provide a potential for an effective treatment to decrease pain and promote movement [8, 9, 20]. At the time this meta-analysis was performed there was no current literature that looked at the effectiveness of VR as a tool for early treatment to improve ROM while increasing patient enjoyment. There are systematic reviews and meta- analysis that look at the effects of VR on pain in the burn population, but that literature does not correlate pain, ROM, and enjoyment.
The purpose of this study is to determine the effectiveness of VR as a treatment tool to increase ROM and enjoyment while decreasing reported pain when compared to standard physical therapy in patients with acute burns. These outcomes will be measured through goniometry for ROM and either Graphic Rating Scale (GRS) scale, the Visual Analog Scale (VAS), or Wong-Baker Face Scale as a subjective response for pain and enjoyment. The null hypothesis is that there will be no difference in joint ROM, reported enjoyment and pain in participants with acute burns using VR therapy versus individuals using standard physical therapy with analgesics. The alternative hypothesis, there will be a difference in joint ROM reported enjoyment and pain in participants with burns using VR therapy versus individuals using standard physical therapy with analgesics.
2. Methods
Databases utilized for this study included: EBSCO: CINAHL Plus with Full Text, PubMed, and Science Direct. Search terms used were: “burns”, “burn injury”, “burns trauma”, “major burns”, “virtual reality”, “VR”, “augmented reality”, “interactive multimedia”, “physiotherapy”, “physical therapy”, “rehabilitation”, “rom”, “range of motion”, “range of movement”. The search was limited to peer-reviewed articles from 2005 to 2020.
2.1 Selection criteria
Studies were included if they were a randomized control trial or within group design, participants were 5 years of age to 90 years of age within a hospital burn unit, required ROM during physical therapy, and at least one joint was affected from the burn. The study must include the use of a goniometer and an outcome measure for pain or enjoyment. The study must also include a form of virtual reality treatment. Exclusion criteria included studies that were not published in English, had participants with cognitive impairments or burns affecting the head. A single assessor was used to determine the overall quality of articles used in this meta-analysis by utilizing the PEDro scale. The PEDro scale is an 11-item assessment that methodologically determines the quality of each randomized control study. One point is awarded for each item of the PEDro scale except the first item, making the final score out of ten [9]. The PEDro scale assists to identify articles validity strengths and any threats present to the validity of each research study. The total score resulted in a good, fair and poor rating based on total points. A good score was six or higher, a fair score was four or five points, and a low score was anything less than 4.25 See Table 1 for a comparison of the PEDro scores for all articles included in this meta-analysis.
2.2 Outcome measure
In order to evaluate improvements of joint ROM, a basic goniometer was exclusively used across all the studies. Goniometers demonstrates reliability and validity in measuring joint ROM in the burn population using the Norkin and White standardized protocols of goniometry measurements [21, 26, 27]. Since the articles were not all joint specific when considering the change of ROM, an average minimum detectable change (MDC) of nine degrees or more for all joints was used, except for the ankle. The ankle has a MDC of five degrees of more. There was no reported minimum clinically important difference (MCID) for ROM [26]. The articles used for this research assessed pain using either the GRS 0-100 scale or the VAS 0-10. The GRS and the VAS have been proven to be a reliable and valid tool in measuring patients with burns level of pain [28]. Both outcomes have been shown to correlate with one another with high reliability and validity [5, 9, 20, 29]. For the pain outcome measure MDC was not reported however MCID was reported by Lee et al. The MCID for pain has been proven to be 30 or 3 based on the GRS or VAS [30]. The last outcome measure utilized for this study was fun or enjoyment, which was measured using the GRS, VRS or Wong- Baker Face Scale. These outcome measures are not commonly used for enjoyment therefore there is no reliability or validity for these measures.
However, they have been proven tools to be reliable and valid for measurement of nominal responses such as “no fun at all” to “most fun possible” [31]. The three different outcome measures have been proven to correlate with one another [29, 32, 33]. Since enjoyment was measured using a nominal scale there is minimal statistical data reported. There were no reports of MDC or MCID found for enjoyment. Acute burns will be used throughout this review and an inclusion criterion for this meta-analysis. For the purpose of this review, acute hospitalized burns are classified as a burn injury that requires professional treatment in a burn center of a hospital from initial injury until the formation of scarring. This time frame is most critical for functional impairments and requires daily treatments. It is important to use acute burn population for this review as this is the time patients will receive initial movement therapy [10]. All therapy done after this period is no longer considered the acute stage of a burn and requires a different level of treatment.
2.3 Data extraction and statistical analysis
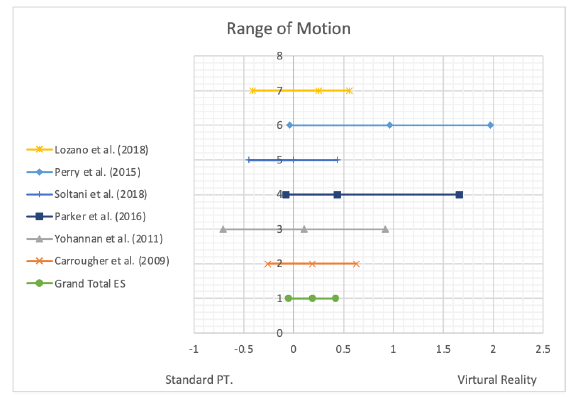
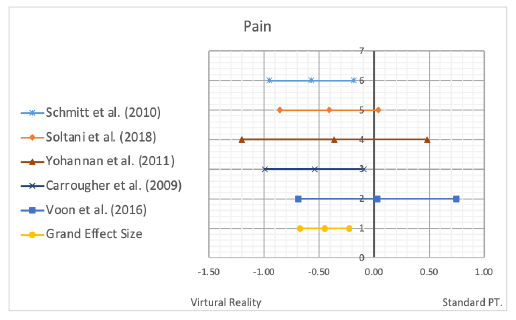
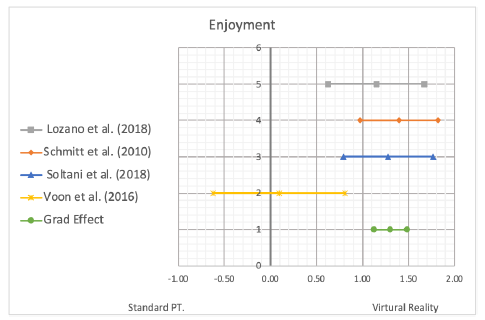
Data utilized in this meta-analysis was retrieved in the results and tables from the included articles. Post- test and standard deviation of ROM and pain scores were observed from those provided in each article. Some articles did not provide standard deviation so a software system, Open Meta, was used to calculate those numbers using the given information for the articles. In order to pair each data point and find statistical similarity, analyzation of the mean change, mean standard deviation and sample size was extracted from each article and entered into the spread sheet. This process allowed for direct comparison of the two groups, virtual reality and standard physical therapy treatment. Effect size with 95% confidence intervals were computed using Microsoft Excel, for post-intervention of range of motion, pain and enjoyment using standard mean differences. A random effect size for two groups was used to create the statistical representation of all data used to generate the forest plots. Heterogeneity was assessed with the Q statistic and I2, with a statistic alpha=0.05. The effect size was determined to be small, medium of large based on the cutoff scores of 0.2-0.5, 0.5-0.8, >0.8, respectively [34]. Forest plots were created to demonstrate the grand effect size between studies for each outcome measure. See Figures 2 through 4.
3. Results
3.1 Selection of studies
A comprehensive search of three databases for articles relating to acute burn physical therapy was performed December 2019 to September 2020. The search between Science Direct, Cinahl and PubMed yielded a total of 242 articles in total which were reviewed based on relevance of titles and abstracts. Prior to reviewing abstracts there were 77 duplicates removed, leaving 165 non-duplicate articles. There were 131 articles removed after reading the abstract and finding the articles did not fit within the meta- analysis leaving 34 articles left to review for inclusion/exclusion criteria. After reviewing the articles for inclusion/exclusion criteria, there were 8 studies left for data collection. Articles were excluded for being a meta-analysis or systematic review, not pertinent to PICO, original article not published in English and there was no usable data throughout the study. All of the included studies quantified at least one of the outcome measures to be analyzed but mentioned at least two of the outcome measures within the study. See Figure 1 for a graphical representation.
A PEDro scale for critically appraising the strengths and limitations of each article was utilized by a single reviewer. The 8 studies had a score ranging from 5-7 on a scale of 10, giving the articles a fair to good rating. Therapist and subject blinding were not meet in any of the studies due to a within-subject crossover study design being utilized for a majority of the articles. Refer to Table 1 for a complete PEDro score breakdown of each articles. The 8 studies evaluated in this meta-analysis utilized various types of virtual reality to complete range of motion exercises during physical therapy treatment. Virtual reality was utilized by both augmented and immersive reality for the studies. Range of motion was measured using a goniometer in the standardized positions. Pain and enjoyment were measured using the GRS, VAS and Wong-Baker. The average age of participants within the studies was 7 to 37.8 years of age [15-21, 35]. Three studies included the pediatric population only, two incorporated both pediatric and adults, and three studies studied only adults. Individual study characteristics definitions are listed in Table 2.
All studies examined the effects VR had a patient through the three different outcome measure utilizing pre- and post-data for an average change in participants. The subjects of each article were patients within the burn unit of a hospital partaking in physical therapy. The studies sample sizes ranged from nine to 54. Lozano et al. examined the effect of VR physical therapy on joint ROM and Wong-Baker enjoyment response in 66 patients through a randomized control trail. Both upper and lower extremity joints were utilized for data collection. The study took place a minimum of twice a week for 15-30 minutes sessions with the Xbox Kinect, but the patients received 1-2 sessions of physical therapy per day five days a week. The total treatments ranged from 8-11 treatments per patient. The study was broken into two separate stages with the intervention group completing their portion of the study prior to collecting data on the control group. Range of motion was measured for both passive and active ROM at the beginning of the study, at time of discharge and a one week follow up. According to Lozano et al. results, there was statistical significance between groups at the time of discharge for active ROM and enjoyment. Data collected for passive ROM and at the follow-up were not included in this study in order to remain consistent with other articles [16]. Parry et al. studied 9 patients to determine the effect VR had on ROM of the upper extremity, subjective pain and enjoyment responses through a randomized control trial. Linear ROM was the only data presented within the study. The motion measured included shoulder flexion, external rotation and abduction, along with elbow flexion. The study consisted of patients completing 25–35-minute sessions twice a day, five days a week for a total of three weeks. The VR system utilized was the PlayStation EyeToy and was used for all treatments in the intervention group. The total treatment sessions were 30 per participant in each group. The study continued to follow the patients after discharge at 3-weeks and did a check-in at 3- months and then 6- months. For the purpose of this meta-analysis only the three-week check-in was used to remain within the acute time frame. The results from this study concluded that the changes in active ROM were not significant at the 6-month mark. However, the largest gain of ROM in the VR group was made at the 3-week mark and these patients continued to make linear progress at the two follow ups [18].
Schmitt et al. was one of three studies that utilized immersive VR through the use of SnowWorld, a computer game designed for the burn population. This study had 54 patients complete 6-20 minute sessions once a day for five days, with a total treatment of 5 sessions per group. Over the course of the study subjective GRS response of pain and enjoyment were collected. Active assisted ROM was measured but no data was presented within the article. Both pain and enjoyment were shown to have statistically significant changes in the VR group compared to the control group [19]. Parker et al. utilized the Nintendo Wii to determine the effects VR had on VAS pain scale and active ROM. Both upper and lower extremity joints were measured including the shoulder, elbow, wrist, hand, knee and ankle. The study included 23 patients divided between the intervention and control group. All sessions lasted 20-30 mins twice a day for a total of 7 days with a total treatment of 14 sessions per patient. In terms of the VR pain scale, the data did show a statistically significant improvement in the Wii group compared to the control. Active ROM was presented with raw data and therefore required Excel to calculate the average change. According to the study there was not statistically significant difference in active ROM at any joint [17].
Voon et al. accessed the feasibility of using the Xbox Kinect to improve subjective VAS of pain and enjoyment. This was a with-in group study of 15 participants that were treated for a total of 14 sessions. When the patient was in the intervention group the sessions lasted 30 minutes with 15 of those minutes being utilized for the Xbox Kinect and the other 15 minutes for standard physical therapy. Both the control and the VR group were seen twice a day for a total of 7 days. This study required participants to fulfill the requirement of each group independent of regular physical therapy sessions. The intervention group showed statistically significant compliance with the exercise program. VAS for enjoyment was statistically significant for the VR group compared to the control group, while VAS for pain was not statistically significant between groups [35]. Carrougher et al. was the second study use immersive VR system, SnowWorld. This study consisted of a with-in group comparison of 54 patients to determine the effects of VR on GRS pain and ROM. This study included both upper and lower extremity joints when measuring ROM, with higher rate of upper extremity joints effected. The joints included hand, wrist forearm, elbow, shoulder, hip knee and ankle. Each session lasted on average 10 minutes once a day for two days, leading to one treatment per condition. This study concluded that VR was statistically significant for reducing subjective pain response compared to the control. In terms of ROM, there was no significant gain in ROM between the groups however, the change in ROM was slightly greater with the VR group [15].
Solatni et al. was the third study to use the immersive VR system, SnowWorld in its with-in group study. There were 54 participants that was measured for ROM and subjective GRS of pain and enjoyment. Joints measured for ROM included only the upper extremity: hand, wrist, forearm, elbow and shoulder. Each participant took part in a three-minute session once per treatment condition. The results of this study concluded there was statistical significance in GRS pain and enjoyment response during the VR treatment compared to the control. ROM did not present with statistically significant changes for VR compared to the control, but there was a significant practice effect. No matter the order in which the patient received treatment the second treatment was significantly great in ROM improvements than the first treatment [20]. Yohannan et al. utilized the Nintendo Wii to determine the effect VR had on ROM and the VAS pain and enjoyment responses. ROM and VAS pain scale were included in this study, VAS enjoyment scale was not included due to lack of data. All data was presented in terms of a slope there for the mean had to be calculated using the baseline numbers and the slope. SEM was provided and transferred into SD to fit data previously collected. This study was a randomized control trail that included 23 patients divided equally into two groups. For the Wii group the patients received 30-minute sessions with 15 minutes of the session incorporating the Wii and the other 15 minutes spent doing joint specific exercise. The control group received just 30 minutes of joint specific exercise. Both groups had a total of three sessions. ROM and VAS for pain and enjoyment were not statistically significant in this study however the data did trend towards the Wii group. The Wii group experienced less pain over the course of the study while improving function instead of increasing ROM [21].
3.2 Synthesis of results
Results from the studies were converted into effect size to facilitate comparisons between the studies and are represented on Tables 3-6. The effect size was calculated based off of pre- and post-data reported for each outcome measures assessed. Each outcome measure, ROM, pain, and enjoyment have an individual statistical data with a forest plot. The results favoring VR fall to the right of the vertical axis for the effects of VR on ROM and enjoyment. Results favoring VR fall to the left of the vertical axis. For ROM, six studies were included in the data.
There was a range of effect sizes from -0.002 to 0.964. The mean effect size was small, 0.19, with confidence intervals crossing the vertical axis representing not clinically significant results. The articles used for this data set were homogeneous based on a relatively identical Q-value to degrees of freedom and high p-value. Due to having a Q-value and degrees of freedom so close, I2 was calculated, and it was determined there was negligible variance between studies making the results homogeneous. Having homogeneous data is significant because it means the treatment of VR is more likely to have caused the change in ROM than a random sampling error. All individual data can be seen in Table 4.
The effect of VR on pain included five studies that had homogeneity throughout. There was a small Q- value, and a large p-value leading to low variance among the outcome measure and homogeneity between the studies. Due to those significant results of the Q-value and p-value, I2 was not calculated to determine amount of variance. The effect sizes ranged from -0.57 to 0.03 with a moderate grand effect size of -0.45. The grand effect did not cross the vertical axis making these results clinically significant. All individual data can be seen in Table 5
The outcome measure of enjoyment had four studies to quantify the data. These four articles had high variance as evident in the high Q-value, and very low p-value resulting in heterogeneity. Based on this information I2 was calculated to be 69.7%. The effect size ranged from 0.09 to 1.39 all favoring VR, with a large grand effect size of 1.30. The grand effect size was clinically significant as it did not cross the vertical axis. The forest plots individual data can be seen in Table 6.
|
Pedro |
Lozano et al., 2018 |
Parry et al., 2015 |
Schmitt et al., 2010 |
Parker et al., 2016 |
Voon, et al., 2016 |
Carrougher et al., 2009 |
Soltani et al., 2018 |
Yohannan et al., 2011 |
|
Category |
||||||||
|
Random Subject Allocation |
— |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
— |
|
Concealed Allocation |
— |
Yes |
Yes |
— |
— |
— |
— |
— |
|
Baseline Comparability |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
— |
Yes |
|
Blind Subjects |
— |
— |
— |
— |
— |
— |
— |
— |
|
Blind Therapists |
— |
— |
— |
— |
— |
— |
— |
— |
|
Blind Assessors |
Yes |
Yes |
Yes |
— |
Yes |
— |
— |
— |
|
Adequate Follow-up |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Intention-to-treat Analysis |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Between-group Comparisons |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Point Estimates and Variability |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Score: #/10 |
6 |
7 |
6 |
6 |
7 |
6 |
5 |
5 |
Table 1: PEDro Scores for Each Study.
|
Author |
Age |
Frequency |
Intervention |
N |
Control |
N |
Outcome |
|
Lozano et al., 2018 |
5-12 y.o M=7 |
15-30 min, 2x/week Total Treatments= 8-11 |
Xbox Kinect AROM |
31 |
AAROM standard physical therapy |
35 |
AROM w/goni Wong Baker ”Enjoyment” |
|
Parry et al., 2015 |
5-12 y.o M=11.4 |
25-35 min 2x/day 5days/week, 3 weeks Total Treatments= 30 |
PlayStation EyeToy AROM and AAROM |
9 |
PROM & AROM standard physical therapy |
8 |
AROM w/goni |
|
Schmitt, 2010 |
6-19 y.o M= 12 |
6-20 min sessions 1x/day, 5 days Total Treatment= 5 |
SnowWorld AAROM |
54 |
AAROM and joint specific exercise |
54 |
GRS Pain GRS Enjoyment |
|
Parker et al., 2016 |
16-59 y.o M=30 |
20-30 min 2x/day; 7 days total Total Treatments= 14 |
Nintendo Wii AROM |
11 |
Passive ROM and joint specific exercise, PT intervention |
12 |
VAS pain AROM w/goni |
|
Voon et al., 2016 |
23-40 y.o M= 30 |
15 min Xbox per 30 min session, 2x/day, 7 days Total Treatments= 14 |
Xbox Kinect AROM |
15 |
Standard therapy |
15 |
VAS Pain VAS Enjoyment |
|
Carrougher et al., 2009 |
21-57 y.o M=35 |
10 min per treatment, 2 days Total Treatments= 2 |
SnowWorld AAROM |
AAROM exercise with standard physical therapy |
39 |
GRS for pain ROM w/goni |
|
|
Soltani et al., 2018 |
15-66 y.o M=36 |
3 mins per treatment, Single day Total Treatments=1 |
SnowWorld AROM |
54 |
Standard therapy |
54 |
GRS for pain ROM w/goni GRS Enjoyment |
|
Yohannan et al., 2011 |
20-78 y.o M= 37.8 |
15 min Wii per 30 min session Total Treatments= 3 |
Nintendo Wii AROM |
11 |
Passive ROM and joint specific exercise |
12 |
VAS for pain AROM w/goni |
Table 2: Summary of Study Characteristics.
|
Outcome Measure |
Q-value |
Degrees of Freedom |
p-value |
I2 |
|
Range of Motion |
5.08 |
5 |
0.41 |
1.63% |
|
Pain |
2.33 |
4 |
.67 |
|
|
Enjoyment |
9.91 |
3 |
0.019 |
69.70% |
Table 3: Summary of Q- values, p-values and I2 for outcome measures.
|
Study |
Description |
X |
Y |
|
Lozano et al. (2018) |
ES |
0.25 |
7 |
|
CI Lower |
-0.41 |
7 |
|
|
CI Upper |
0.56 |
7 |
|
|
Perry et al. (2015) |
ES |
0.964 |
6 |
|
CI Lower |
-0.04 |
6 |
|
|
CI Upper |
1.97 |
6 |
|
|
Soltani et al. (2018) |
ES |
-0.002 |
5 |
|
CI Lower |
-0.45 |
5 |
|
|
CI Upper |
0.44 |
5 |
|
|
Parker et al. (2016) |
ES |
0.44 |
4 |
|
CI Lower |
-0.08 |
4 |
|
|
CI Upper |
1.66 |
4 |
|
|
Yohannan et al. (2011) |
ES |
0.105 |
3 |
|
CI Lower |
-0.71 |
3 |
|
|
CI Upper |
0.92 |
3 |
|
|
Carrougher et al. (2009) |
ES |
0.189 |
2 |
|
CI Lower |
-0.26 |
2 |
|
|
CI Upper |
0.63 |
2 |
|
|
Grand Total ES |
ES |
0.19 |
1 |
|
CI Lower |
-0.05 |
1 |
|
|
CI Upper |
0.42 |
1 |
Table 4: Grand effect sizes and confidence intervals for outcome measure: ROM.
|
Study |
Description |
X |
Y |
|
Schmitt et al. (2010) |
ES |
-0.57 |
6 |
|
CI Lower |
-0.95 |
6 |
|
|
CI Upper |
-0.18 |
6 |
|
|
Soltani et al. (2018) |
ES |
-0.41 |
5 |
|
CI Lower |
-0.86 |
5 |
|
|
CI Upper |
0.04 |
5 |
|
|
Yohannan et al. (2011) |
ES |
-0.36 |
4 |
|
CI Lower |
-1.2 |
4 |
|
|
CI Upper |
0.48 |
4 |
|
|
Carrougher et al. (2009) |
ES |
-0.54 |
3 |
|
CI Lower |
-1 |
3 |
|
|
CI Upper |
-0.09 |
3 |
|
|
Voon et al. (2016) |
ES |
0.03 |
2 |
|
CI Lower |
-0.69 |
2 |
|
|
CI Upper |
0.75 |
2 |
|
|
Grand Effect Size |
ES |
-0.45008 |
1 |
|
CI Lower |
-0.67378 |
1 |
|
|
CI Upper |
-0.22637 |
1 |
Table 5: Grand effect sizes and confidence intervals for outcome measure: Pain.
|
Study |
Description |
X |
Y |
|
Lozano et al. (2018) |
ES |
1.15 |
4 |
|
CI Lower |
0.63 |
4 |
|
|
CI Upper |
1.67 |
4 |
|
|
Schmitt et al. (2010) |
ES |
1.39471 |
3 |
|
CI Lower |
0.974141 |
3 |
|
|
CI Upper |
1.815278 |
3 |
|
|
Soltani et al. (2018) |
ES |
1.28 |
2 |
|
CI Lower |
0.79 |
2 |
|
|
CI Upper |
1.76 |
2 |
|
|
Grand Effect |
ES |
1.291366 |
1 |
|
CI Lower |
1.019657 |
1 |
|
|
CI Upper |
1.563075 |
1 |
Table 6: Grand effect sizes and confidence intervals for outcome measure: Enjoyment.
4. Discussion
In review, the purpose of this study was to investigate the difference of virtual reality compared to standard physical therapy for improving range of motion and enjoyment all while decreasing pain for individuals suffering from an acute burn injury. All studies included were screened by one assessor to determine if it met the eligibility criteria of being in the acute setting and quantified at least one of the three outcome measures. The results of this meta-analysis demonstrated that VR is favored for improving ROM, increasing treatment enjoyment and decree- sing pain during treatment. With varying results for each outcome measure, the null hypothesis: there will be no difference in joint ROM, reported enjoyment and pain in patients with acute burns using VR therapy versus individuals using standard physical therapy with analgesics, is rejected with caution. The null hypothesis is rejected with caution due to heterogeneity with large amounts of variance for the studies used for enjoyment, and ROM not clinically significant as the confidence interval crossed the vertical axis. The other two outcome measures, pain and enjoyment, were clinically significant and moderately to strongly favored VR.
VR may be favored against standard physical therapy for many reasons. One reason is that VR causes changes within the brain’s “pain matrix”. According to Hoffman et al. when a person is using VR and a painful stimulus is active, the areas of the brain that normally respond to pain have decreased activity [9, 24]. Pain is no longer being perceived by the brain due to the fact the brain is occupied with another stimulus. VR is utilizing the Gate Control theory to decrease the “pain matrix” activity. The Gate Control theory states that faster and larger nerve fibers are going to send signals to the brain diminishing the available processing of slower pain nerve fibers within the brain [36, 37]. With decreased pain recognition, a patient could be more willing to move the affected area leading to lifelong effects [8]. The use of VR to decrease pain has been studied and analyzed for many years with the same results; VR will present with an analgesic effect without diminished results over time [38, 39]. For this reason, patients that utilize VR have better treatment compliance allowing for an increase in ROM. If a patient is more willing to move, then the effects of the natural healing process of the skin hardening and becoming inelastic can be diminished [10, 38]. A moving patient is less likely to spend their time in the positions of comfort for long periods of time decreasing the possibility of contracture formation thus decreasing the number of surgeries [10]. This early movement can have long-lasting effects both physically and psychologically [6, 22].
Patients with poor treatment compliance leads to not only skin contractures but can lead to post traumatic stress disorder (PTSD), depression and drug abuse [3, 5, 40]. When a treatment is necessary but is excruciating for the patient, it can lead to increased stress levels which in turn can develop into PTSD or drug abuse. Patients will begin to correlate physical therapy with a traumatic experience leading the patient to no longer wanting to move [5]. The patient could also develop a dependence for analgesics to decrease the pain, but over time, the patient will require an increased dosage of medications to have the same effects. This can lead to the patient having a drug abuse problem as the patient attempts to medically reduce the pain with stronger more dangerous medication. Both of these side effects can cause the patient to stop moving which can led to skin contractures. This can cause some people to develop depression for they are no longer moving the way they were prior to the injury. Skin contractures are going to limit the functional use of the affected area which can take away independence with activities of daily living [6, 10, 22]. All of that can lead to an increase in hospitalization which can cause more stress. The more stress the patient is under the longer it takes for the tissue to heal. Stress can lead to a decreased healing rate as a stressed-out body release too many glucocorticoids which decreases cytokines from being released [41]. Since cytokines are decreased, the cells needed for tissue regeneration and capillary regrowth, phagocytes, are not recruited to assist with the healing process. With limited cytokines in the affected tissue, not only is the recruitment of phagocytes reduced but there is also a decreased barrier to infection [34]. This cellular response to stress prolongs the healing rate which can increase hospitalization. This increased time in the hospital can also play a role in patients developing PTSD or depression [41, 42].
Since ROM was only treading towards VR, it is important to remember that these studies looked at patients in the acute phase of healing. Changes in ROM can be improved on for months to even years after a burn [22]. This is a long process therefore some changes in ROM are not seen until after the studies were over. Two studies, Parry et al and Lozano et al. completed follow-up visits in their studies and concluded that ROM continued to improve [16, 18]. This continuing growth of ROM in follow-ups months later reveals that time is needed to truly have an impact on ROM and that some of the studies included within this meta-analysis did not have enough time to have true changes in ROM. VR treatments did present with some trends in the data such as age is irrelevant, and repetition of treatment does not diminish the effect. This goes in line with findings from other studies that looked at the importance of age [38]. This meta-analysis included pediatric, mixed age groups and adult populations within the study and the results were similar across the board. Shockingly, the studies that included both pediatric and adults tended to favor VR slightly more than those with just pediatric patients. For example, in the fun forest plot Soltani et al., a mixed age group with a mean age of 36, had a large effect size compared to Lozano et al. who was strictly pediatrics [16, 20]. This result was seen throughout all the outcome measures, leading to the fact that age is not a barrier to having effects on ROM or pain. With this information, burn units could incorporate some form of VR with their patients without having to consider the patient’s age.
While age appears to be irrelevant, another clinical issue is the effectiveness of the treatment after repeated use. From this meta-analysis it appears longer treatment durations did not change the effectiveness VR had on the treatment. These results are in agreeance with other research that the analgesic effects did not diminish over multiple sessions [43]. The studies with the largest total treatment time did not differ significantly than those with shorter treatment times. In some instances, the longer treatments durations lead to a larger increase in ROM and decrease pain. The only study that significantly differed in results was Voon et al. which can be attributed to the study design [35]. This study was the only study within the pain and enjoyment forest plots that consisted of patients completing independent exercise without the supervision of a skilled physical therapist. While the results of this study did trend towards VR and the results were homogeneous for ROM and pain, there was some variance that needs to be considered between all outcome measures. With all the studies, the main variance between them was treatment duration. For ROM, Parry et al. and Parker et al. had the largest amounts of total treatments and treatment times which allowed these two studies to strongly favor VR [17, 18]. This trend was apparent throughout all the outcome measures. Those studies that had the largest treatment durations in days of treatment and time spent per day had the strongest effect towards VR. According to Bricknell et al., tissue elongation takes a minimum of one hour a day of stretching to have a change of the tissues length [11]. This supports the larger effect sizes with Parry et al and Parker et al as they were the only two studies that treated patients within the study for at least an hour a day [17, 18]. Another area that caused variance was the amount of supervision per study. Voon et al had their participants doing the study treatments independently from a skilled therapist [35]. Those independent sessions were outliers for both pain and enjoyment forest plots as seen in Figures 2 and 3. Having supervision in the early stages of recovery is important to not only ensure the patient is completing the treatments properly, but to also provide encouragement and ensure the patient they are not alone in this process [6]. The lack of that social component may have led Voon et al to be the only study with a small effect size in all outcome measures presented [35]. The other studies that had a skilled therapist working with the individual during the treatment session had larger effect sizes favoring VR in all outcomes. All results collected for this meta-analysis are consistent with other systematic reviews and meta-analysis performed on this population. Luo et al and Scapin et al. reported that VR does decrease the patient’s perception of pain and trends towards improving ROM [3, 23]. Enjoyment is something newly studied but does follow the trend of Luo et al. that enjoyment increased during VR treatment than in standard physical therapy [3]. There was also no difference in age between the results. Furthermore, this meta-analysis is the first to quantify the changes of ROM in this population but due to the small sample size, this study may have reduced statistical power.
4.1 Clinical implications
Based on these findings, physical therapists can use VR as a treatment tool to help their patients recover quicker with less pain compared to traditional physical therapy. VR has been proven as a good analgesic for procedural pain, which is one of the main complaints with physical therapy [4, 6, 7, 15, 23, 24, 43]. Since the patient is having less pain, enjoyment of the treatment may be increased. Through increased enjoyment and decreased pain, patients have another positive side effect of treatment such as decreased anxiety, increased compliance with treatment and increased ROM [3, 23]. These patients are dealing with a traumatic event that has changed their life forever. During the acute stage of healing there are a lot of new changes a person has to adjust to, all while being in a stressful environment of a hospital. While a hospital is there to save a person’s life it does add stress to the situation by having to go through different procedures, dressing changes, daily medication, occupational therapy, and physical therapy [3, 5, 6]. The patient’s stress levels can be decreased through the use of VR by adding an element of fun that also safely deceases pain levels without major negative side effects.
Having less pain and more enjoyment with physical therapy treatments using VR can lead to an increase in exercise compliance [3, 23, 39]. This increase in exercise compliance can lead to a greater increase in ROM early on in treatments. While ROM was not clinically significant, it does trend towards VR. Since there is no harm caused with VR, this could be a more superior treatment option than just standard physical therapy alone based on the analgesic effect. By having increased compliance and increased ROM this can lead to more positive benefits to the patient such as contracture prevention and decreased surgeries required [39]. One of the most common complications of a burn injury is contracture formation [6, 10]. This is typically due to decreased movement from the patient during the healing stage, but VR can help improve movement as mentioned above. Having a decrease in pain and an increase in enjoyment can lead to a decrease in anxiety to physical therapy and movement in general. The more willing the patient is to move during treatments the more compliant they are to participate in treatments and to move outside of physical therapy [6].
4.2 Limitations
While every attempt was made to limit validity threats, this meta-analysis did present with threats to internal, external and construct validity throughout the studies and within the creation of this meta- analysis. There were two major internal validity threats presented throughout the search and studies themselves. Since this meta-analysis was completed by a single appraiser there could have been selection bias when conducting a search for studies to include. Some studies could have been omitted based on the search criteria utilized. Another internal validity threat was all articles included were lacking blinding of the subjects and the assessors. While the articles were carefully screened, there was a limited number of studies that fit within the inclusion of this meta- analysis. The lack of blinding can lead to inaccurate data due to the fact the assessor could have influenced the participants to perform in a manner that favored the intervention. Threats to external validity were contributed to the limited number of studies and the varying sample sizes within the studies. Due to VR recently becoming more popular with this population, there are limited studies available. The limited studies made it impossible to complete a sub analysis on the different confounding variables such as age, specific joint and augment versus immersive reality. The studies themselves had varying sample sizes but overall there were small samples compared to the number of patients suffering from burns. Having such a small sample size makes it challenging to generalize these results, but all the studies had varying VR treatment guidelines, age groups and joints affected allowing this data to reach a large portion of this population. With the varying construct of the studies this led to threats against construct validity. The main threat was the lack of an intervention protocol for burn physical therapy. All studies treated patients for different durations such as Soltani et al. treating the patient for three minutes one time20 compared to Parry et al who treated up to an hour a day, five-days a week for three-weeks18. The definition of standard physical therapy was different per study as well. Some studies incorporated active- assisted ROM while other used passive ROM or a combination of both. Along with not having standardized treatment protocols, the VR used throughout the studies were different. There were four different types of VR systems used throughout the studies, including immersive and augmented reality. The immersive VR studies had to exclude all head burns due to the headpiece that has to be worn to use the VR system [15, 19, 20]. The augmented VR systems do not have to screen for all head burns and could include minor head burns as there is no equipment that required to sit on the head. Between the augmented VR systems, they utilized a different style of play where the Nintendo Wii and PlayStation EyeToy require a handheld device to control the game while the Xbox Kinect did not require any equipment that needed to be physically touched by the patient.
4.3 Future research
After completing this meta-analysis, there is some preliminary research conducted on the effects of VR on ROM, pain and enjoyment; however, there are some areas in which future research should be considered. First there need to be longitudinal studies that look at the effects of VR on ROM and pain over years to determine if early treatment has an impact on contracture formation rate. There also need to be more studies that break down results by specific joints to determine if VR is a joint specific treatment. Currently the studies presented in this meta-analysis did not break down the results per joint leading to question if all joints are benefited in increasing ROM using VR. With these new studies there should be a treatment protocol for utilizing VR that consist of having physical therapy for at least an hour a day. A standard physical therapy treatment for a patient with a burn injury consists of one to two sessions a day, therefore the studies need to incorporate treatment plans that are similar to what is being practiced already. Lastly, the type of VR needs to be further studied to determine if a hospital can be cost effective with purchasing the required equipment. There is limited information on the different effects augmented VR compared to immersive VR has on the improvement of ROM and the analgesic effect.
5. Conclusion
In conclusion, this meta-analysis is in line with other systematic reviews and meta-analysis about the effect’s VR has on patients with acute burn injuries. VR during the acute stage of healing can benefit the patient in many ways. It can decrease a patient’s pain with treatment, can improve ROM, and improve
overall enjoyment of treatment. The effect size was moderate with homogeneity, representing a clinically significant change in reported pain. VR can increase the enjoyment of a treatment, but this is said with caution as the data had large amounts of variability. The effect size was a large effect size that was clinically meaningful but is unable to be generalized for the entire population. The last outcome of range of motion was not clinically significant but did have a strong trend towards utilizing VR as a treatment option. The effect size was small, but the data did present with homogeneity. VR, whether augmented or immersive, should be incorporated within the treatment to allow for the best results possible with the early stages of healing in a burn injury.
References
- Nowak TJ. Burn pathophysiology. Perioper Nurs Clin 7 (2012): 9-17.
- Tzy-Chyi Yu, Xian Zhang, Janice Smiell, Huanxue Zhou, Ruixin Tan, Elaine Böing, et Healthcare resource utilization, treatment patterns, and cost of care among patients with thermal burns and inpatient autografting in two large privately insured populations in the united states. Burns 46 (2020): 825-835.
- Luo H, Cao C, Zhong J, Chen J, Cen Adjunctive virtual reality for procedural pain management of burn patients during dressing change or physical therapy: A systematic review and meta?analysis of randomized controlled trials. Wound Repair Regen 27 (2019): 90-101.
- Hoffman HG, Patterson DR, Carrougher GJ, Dana Nakamura, Merilyn Moore, Azucena Garcia-Palacios, et al. The effectiveness of virtual reality pain control with multiple treatments of longer durations: A case Int J Hum Comput Interact 13 (2001): 1-12.
- Esselman PC, Thombs BD, Magyar-Russell G, Fauerbach JA. Burn rehabilitation: State of the science. Am J Phys Med Rehabil 85 (2006): 383-413.
- Procter F. Rehabilitation of the burn patient. Indian J Plast Surg 43 (2010): S101-S113.
- Michael Morgan 1, Jennifer R Deuis 1, Majbrit Frøsig-Jørgensen 1, Richard J Lewis 1, Peter J Cabot 2, Paul D Gray, et al. Burn pain: A systematic and critical review of epidemiology, pathophysiology, and treatment. Pain Med 19 (2018): 708-734.
- Ford CG, Manegold EM, Randall CL, Aballay AM, Duncan CL. Assessing the feasibility of implementing low-cost virtual reality therapy during routine burn care. Burns 44 (2018): 886-895.
- Morris LD, Louw QA, Crous LC. Feasibility and potential effect of a low-cost virtual reality system on reducing pain and anxiety in adult burn injury patients during physiotherapy in a developing Burns (03054179) 36 (2010): 659-664.
- Thakrar GN, Patel DA, Sejpal JJ. Effect of physiotherapy rehabilitation in acute burn injury around shoulder joint. Indian J Physiother Occup Ther 9 (2015):
- Bricknell JC W, Darton A, Edmondson R, Iddamalgoda T, Katsu A, Lawrence E, et al. Burn physiotherapy and occupational therapy guidelines. In: Innovation AfC, ed (2017).
- Hettiaratchy S, Dziewulski P. Abc of burns: Pathophysiology and types of burns. BMJ (Clinical research ed) 328 (2004): 1427-1429.
- DeSanti L. Pathophysiology and current management of burn injury. Adv Skin Wound Care 18 (2005): 323-334.
- Wright Fundamentals of acute burn care and physical therapy management. Phys Ther 64 (1984): 1217-1231.
- Gretchen J Carrougher, Hunter G Hoffman, Dana Nakamura, Dennis Lezotte, Maryam Soltani, Laura Leahy, et al. The effect of virtual reality on pain and range of motion in adults with burn J Burn Care Res 30 (2009): 785-791.
- Lozano EI, Potterton The use of xbox kinect™ in a paediatric burns unit. S Afr J Physiother 74 (2018).
- Matthew Parker, Brett Delahunty, Nicolas Heberlein, Neale Devenish, Fiona M Wood, Teresa Jackson, et al. Interactive gaming consoles reduced pain during acute minor burn rehabilitation: A randomized, pilot trial. Burns 42 (2016): 91-96.
- Ingrid Parry, Lynda Painting, Anita Bagley, Jason Kawada, Fred Molitor, Soman Sen, et al. A pilot prospective randomized control trial comparing exercises using videogame therapy to standard physical therapy: 6 months follow-up. J Burn Care Res 36 (2015): 534-544.
- Yuko S Schmitt, Hunter G Hoffman, David K Blough, David R Patterson, Mark P Jensen, Maryam Soltani, et al. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns (03054179) 37 (2011): 61-68.
- Maryam Soltani, Sydney A Drever, Hunter G Hoffman, Sam R Sharar, Shelley A Wiechman, Mark P Jensen, et al. Virtual reality analgesia for burn joint flexibility: A randomized controlled trial. Rehabil Psychol 63 (2018): 487-494.
- Sam K Yohannan, Patricia A Tufaro, Hope Hunter, Lauren Orleman, Sara Palmatier, Ca- nace Sang, et al. The utilization of nintendo® wii™ during burn rehabilitation: A pilot study. J Burn Care Res 33 (2012): 36-45.
- Spires MC, Kelly BM, Pangilinan PH Jr. Rehabilitation methods for the burn injured individual. Phys Med Rehabil Clin N Am 18 (2007):
- Scapin S, Echevarría-Guanilo ME, Boeira Fuculo Junior PR, Gonçalves N, Rocha PK, Coimbra Virtual reality in the treatment of burn patients: A systematic review. Burns 44 (2018): 1403-1416.
- Hunter G Hoffman, Todd L Richards, Aric R Bills, Trevor Van Oostrom, Jeff Magula, Eric J Seibel, et al. Using fmri to study the neural correlates of virtual reality analgesia. CNS Spectrums: CNS Spectrums: The International Journal of Neuropsychiatric Medicine 11 (2006): 45-65.
- Cashin AG, McAuley JH. Clinimetrics: Physiotherapy evidence database (pedro) scale. J Physiother 66 (2020):
- Edgar D, Finlay V, Wu A, Wood F. Goniometry and linear assessments to monitor movement outcomes: Are they reliable tools in burn survivors?. Burns 35 (2009): 58-62.
- Scalzitti DA, White DJ. Validity and reliability of goniometric measurement. In: Norkin CC, White DJ, eds. Measurement of joint motion: A guide to goniometry, 5e. New York, NY: McGraw-Hill Education (2016).
- Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med 8 (2001): 1153- 1157.
- Gracely RH, McGrath F, Dubner R. Ratio scales of sensory and affective verbal pain descriptors. Pain 5 (1978): 5-18.
- Lee JS, Hobden E, Stiell IG, Wells GA. Clinically important change in the visual analog scale after adequate pain control. Acad Emerg Med 10 (2003): 1128-1130.
- Vautier S. Measuring change with multiple visual analogue scales: Application to tense arousal. Eur J Psychol Assess 27 (2013): 111- 120.
- Garra G, Singer AJ, Domingo A, Thode The wong-baker pain faces scale measures pain, not fear. Pediatr Emerg Care 29 (2013): 17-20.
- Gregory Garra, Adam J Singer, Breena R Taira, Jasmin Chohan, Hiran Cardoz, Ernest Chisena, et al. Validation of the wong-baker faces pain rating scale in pediatric emergency department patients. Acad Emerg Med 17 (2010): 50-54.
- Fetters L, Tilson J. Evidence based physical therapy. 2 ed. Philadelphia, PA: A. Davis Company (2018).
- Voon K, Silberstein I, Eranki A, Phillips M, Wood FM, Edgar DW. Xbox kinect based rehabilitation as a feasible adjunct for minor upper limb burns rehabilitation: A pilot rct. Burns 42 (2016): 1797-1804.
- Gold JI, Belmont KA, Thomas DA. The neurobiology of virtual reality pain attenu- ation. Cyberpsychol Behav 10 (2007): 536-544.
- Melzack R, Wall PD. Pain mechanisms: A new theory. Science 150 (1965): 971-979.
- Sharar SR, Carrougher GJ, Nakamura D, Hoffman HG, Blough DK, Patterson Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: Preliminary results from 3 ongoing studies. Arch Phys Med Rehabil 88 (2007): S43-S49.
- Sam R Sharar, William Miller, Aubriana Teeley, Maryam Soltani, Hunter G Hoffman, Mark P Jensen, et al. Applications of virtual reality for pain management in burn-injured patients. Expert Rev Neurother 8 (2008): 1667-1674.
- Dalal PK, Saha R, Agarwal M. Psychiatric aspects of burn. Indian J Plast Surg 43 (2010): S136-S142.
- Brown NJ, Kimble RM, Rodger S, Ware RS, Cuttle L. Play and heal: Randomized controlled trial of ditto intervention efficacy on improving re-epithelialization in pediatric burns. Burns 40 (2014): 204-213.
- Gouin JP, Kiecolt-Glaser JK. The impact of psychological stress on wound healing: Methods and mechanisms. Immunol Allergy Clin North Am 31 (2011): 81-93.
- Hunter G Hoffman, Gloria T Chambers, Walter J Meyer, Lisa L Arceneaux, William J Russell, Eric J Seibel, et al. Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical proce- dures. Ann Behav Med 41 (2011): 183-191.