Effectiveness of Providing Cognitive-behavioral Group Therapy for Both Children and their Parents Separately in the Treatment of Childhood Major Depressive Disorder: A Pilot Study
Article Information
Nermeen Nabil Fawzy*
Child psychiatry unit, Abbassia Psychiatric Hospital, General Secretariat of Mental Health, Ministry of Health and Population, Cairo, Egypt
*Corresponding Author: Nermeen Nabil Fawzy, Child psychiatry unit, Abbassia Psychiatric Hospital, General Secretariat of Mental Health, Ministry of Health and Population, Cairo, Egypt
Received: 14 November 2019; Accepted: 21 November 2019; Published: 27 November 2019
Citation: Nermeen Nabil Fawzy. Effectiveness of Providing Cognitive-behavioral Group Therapy for Both Children and their Parents Separately in the Treatment of Childhood Major Depressive Disorder: A Pilot Study. Journal of Psychiatry and Psychiatric Disorders 3 (2019): 274-285.
View / Download Pdf Share at FacebookAbstract
Background: Three social learning mechanisms were hypothesized to influence the development of depressogenic cognitive styles: modeling of parents’ negative cognitive styles; direct learning from negative parental inferential feedback regarding the stressful events in the child’s life; and indirect learning from negative parenting practices. In this study, I proposed an approach addressing psychopathology in parents as well as their children through providing cognitive behavioral therapy for both, separately, in treatment of childhood Major depressive disorder. This study’s objective is to evaluate the effectiveness of this approach.
Method: Cognitive behavioral group therapy was provided separately to seven children diagnosed with Major depressive disorder, and their parents in 12 weekly 1-hour sessions. Parents’ sessions were parallel to children sessions, focused on learning the same skills and techniques taught in the children’s groups, targeting modifying negative cognitive styles of parents as well as children. Psychiatric clinical interview by specialized child psychiatrists and Parent-rated Mood and Feelings Questionnaire (PMFQ) were used pre- and post-treatment to evaluate depressive symptoms.
Results: At the end of the treatment, all children no longer met criteria for major depressive disorder. There were statistically significant reductions in scores of parent-rated Mood and Feelings Questionnaire, which also demonstrated that none of the children no longer had a score indicative of depressive disorder.
Conclusion: This study suggested that providing cognitive behavioral group therapy for both children and their parents, separately, is an effective approach for childhood major depressive disorder treatment.
Keywords
Childhood major depressive disorder; Parental psychopathology; CBT for children; CBT for parents
Childhood major depressive disorder articles, Parental psychopathology articles, CBT for children articles, CBT for parents articles
Childhood major depressive disorder articles Childhood major depressive disorder Research articles Childhood major depressive disorder review articles Childhood major depressive disorder PubMed articles Childhood major depressive disorder PubMed Central articles Childhood major depressive disorder 2023 articles Childhood major depressive disorder 2024 articles Childhood major depressive disorder Scopus articles Childhood major depressive disorder impact factor journals Childhood major depressive disorder Scopus journals Childhood major depressive disorder PubMed journals Childhood major depressive disorder medical journals Childhood major depressive disorder free journals Childhood major depressive disorder best journals Childhood major depressive disorder top journals Childhood major depressive disorder free medical journals Childhood major depressive disorder famous journals Childhood major depressive disorder Google Scholar indexed journals Parental psychopathology articles Parental psychopathology Research articles Parental psychopathology review articles Parental psychopathology PubMed articles Parental psychopathology PubMed Central articles Parental psychopathology 2023 articles Parental psychopathology 2024 articles Parental psychopathology Scopus articles Parental psychopathology impact factor journals Parental psychopathology Scopus journals Parental psychopathology PubMed journals Parental psychopathology medical journals Parental psychopathology free journals Parental psychopathology best journals Parental psychopathology top journals Parental psychopathology free medical journals Parental psychopathology famous journals Parental psychopathology Google Scholar indexed journals CBT for children articles CBT for children Research articles CBT for children review articles CBT for children PubMed articles CBT for children PubMed Central articles CBT for children 2023 articles CBT for children 2024 articles CBT for children Scopus articles CBT for children impact factor journals CBT for children Scopus journals CBT for children PubMed journals CBT for children medical journals CBT for children free journals CBT for children best journals CBT for children top journals CBT for children free medical journals CBT for children famous journals CBT for children Google Scholar indexed journals CBT for parents articles CBT for parents Research articles CBT for parents review articles CBT for parents PubMed articles CBT for parents PubMed Central articles CBT for parents 2023 articles CBT for parents 2024 articles CBT for parents Scopus articles CBT for parents impact factor journals CBT for parents Scopus journals CBT for parents PubMed journals CBT for parents medical journals CBT for parents free journals CBT for parents best journals CBT for parents top journals CBT for parents free medical journals CBT for parents famous journals CBT for parents Google Scholar indexed journals Major depressive disorder articles Major depressive disorder Research articles Major depressive disorder review articles Major depressive disorder PubMed articles Major depressive disorder PubMed Central articles Major depressive disorder 2023 articles Major depressive disorder 2024 articles Major depressive disorder Scopus articles Major depressive disorder impact factor journals Major depressive disorder Scopus journals Major depressive disorder PubMed journals Major depressive disorder medical journals Major depressive disorder free journals Major depressive disorder best journals Major depressive disorder top journals Major depressive disorder free medical journals Major depressive disorder famous journals Major depressive disorder Google Scholar indexed journals Diagnostic and statistical manual of mental disorders articles Diagnostic and statistical manual of mental disorders Research articles Diagnostic and statistical manual of mental disorders review articles Diagnostic and statistical manual of mental disorders PubMed articles Diagnostic and statistical manual of mental disorders PubMed Central articles Diagnostic and statistical manual of mental disorders 2023 articles Diagnostic and statistical manual of mental disorders 2024 articles Diagnostic and statistical manual of mental disorders Scopus articles Diagnostic and statistical manual of mental disorders impact factor journals Diagnostic and statistical manual of mental disorders Scopus journals Diagnostic and statistical manual of mental disorders PubMed journals Diagnostic and statistical manual of mental disorders medical journals Diagnostic and statistical manual of mental disorders free journals Diagnostic and statistical manual of mental disorders best journals Diagnostic and statistical manual of mental disorders top journals Diagnostic and statistical manual of mental disorders free medical journals Diagnostic and statistical manual of mental disorders famous journals Diagnostic and statistical manual of mental disorders Google Scholar indexed journals 5th edition articles 5th edition Research articles 5th edition review articles 5th edition PubMed articles 5th edition PubMed Central articles 5th edition 2023 articles 5th edition 2024 articles 5th edition Scopus articles 5th edition impact factor journals 5th edition Scopus journals 5th edition PubMed journals 5th edition medical journals 5th edition free journals 5th edition best journals 5th edition top journals 5th edition free medical journals 5th edition famous journals 5th edition Google Scholar indexed journals Parent-rated Mood and Feelings Questionnaire articles Parent-rated Mood and Feelings Questionnaire Research articles Parent-rated Mood and Feelings Questionnaire review articles Parent-rated Mood and Feelings Questionnaire PubMed articles Parent-rated Mood and Feelings Questionnaire PubMed Central articles Parent-rated Mood and Feelings Questionnaire 2023 articles Parent-rated Mood and Feelings Questionnaire 2024 articles Parent-rated Mood and Feelings Questionnaire Scopus articles Parent-rated Mood and Feelings Questionnaire impact factor journals Parent-rated Mood and Feelings Questionnaire Scopus journals Parent-rated Mood and Feelings Questionnaire PubMed journals Parent-rated Mood and Feelings Questionnaire medical journals Parent-rated Mood and Feelings Questionnaire free journals Parent-rated Mood and Feelings Questionnaire best journals Parent-rated Mood and Feelings Questionnaire top journals Parent-rated Mood and Feelings Questionnaire free medical journals Parent-rated Mood and Feelings Questionnaire famous journals Parent-rated Mood and Feelings Questionnaire Google Scholar indexed journals depressogenic cognitive styles articles depressogenic cognitive styles Research articles depressogenic cognitive styles review articles depressogenic cognitive styles PubMed articles depressogenic cognitive styles PubMed Central articles depressogenic cognitive styles 2023 articles depressogenic cognitive styles 2024 articles depressogenic cognitive styles Scopus articles depressogenic cognitive styles impact factor journals depressogenic cognitive styles Scopus journals depressogenic cognitive styles PubMed journals depressogenic cognitive styles medical journals depressogenic cognitive styles free journals depressogenic cognitive styles best journals depressogenic cognitive styles top journals depressogenic cognitive styles free medical journals depressogenic cognitive styles famous journals depressogenic cognitive styles Google Scholar indexed journals depressive disorder articles depressive disorder Research articles depressive disorder review articles depressive disorder PubMed articles depressive disorder PubMed Central articles depressive disorder 2023 articles depressive disorder 2024 articles depressive disorder Scopus articles depressive disorder impact factor journals depressive disorder Scopus journals depressive disorder PubMed journals depressive disorder medical journals depressive disorder free journals depressive disorder best journals depressive disorder top journals depressive disorder free medical journals depressive disorder famous journals depressive disorder Google Scholar indexed journals
Article Details
Abbreviations:
CBT - Cognitive-behavioral therapy; MDD - Major depressive disorder; DSM-5 - Diagnostic and statistical manual of mental disorders; 5th edition; PMFQ - Parent-rated Mood and Feelings Questionnaire
1. Introduction
According to Beck's cognitive theory of depression, negative thinking styles or ‘negative cognitive schemas’ play a key role in the development, maintenance, and recurrence of depression, Beck also described cognitive triad of depression that consists of negative view about the self, the world, and the future [1]. Negative schemas attribute to errors in information processing that result in negative biased interpretation of experiences. Information processing errors have been identified as cognitive distortions [1]. Negative schemas are hypothesized to develop from interactions with the environment, primarily during childhood through early learning experiences, especially those within the family [2].
Social-cognitive learning theory proposed that individuals tend to internalize the self-concepts, judgment standards, rules-making, and self-regulatory influences which are encountered in their learning environment, so children can learn cognitive disturbances vicariously through parental modelling [3]. Three social learning mechanisms were hypothesized to play a role in the development of depressogenic cognitive styles: modeling of parents’ negative cognitive styles; direct learning from negative parental inferential feedback regarding the causes and consequences of stressful events in the child’s life; and indirect learning from negative parenting practices.
Seligman et al. [4] reported a signi?cant correlation between the attributional styles for negative events of mothers and their elementary school children. Similarly, Stark, et al [5] found a significant relationship between mothers’ and children’s scores on a measure of Beck’s negative cognitive triad. Many other studies support that children may learn their cognitive styles in part by observing and modeling signi?cant others, particularly their parents [6-9]. It is hypothesized that the mother’s cognitive style is modeled more than the father’s cognitive style [10].
In addition to modeling, the feedback that parents provide their children about causes and consequences of negative events in the child’s life has also been found to contribute to the child’s cognitive risk for depression. Children may develop an inferential style consistent with the parental feedback. Perceived parental messages about the self, world, and future were also shown to be predictive of children’s cognitive triad, as well as ratings of depression [5]. The same study found that the relationship between perceived parental messages and depression is completely mediated through children’s cognitive triads [5]. Garber and Flynn [11] reported a relation between mothers’ attributions for events in the child’s life and their child’s attributions. Alloy et al. [10] found that both mothers and fathers of adolescents with high cognitive vulnerability reported that they provided more negative inferential feedback in response to negative events than did parents of adolescents with low cognitive vulnerability.
Children’s development of negative cognitive style influenced not only by direct learning from parental inferential feedback about negative events in the child’s life, but also by indirect learning from parents through negative parenting practices. Young [12] hypothesizes that maladaptive schemas could be the result of inadequate parenting or ongoing aversive experiences within the family environment such as repeated criticism or rejection. Parental rejection and restrictive control in childhood predicted subsequent self-criticism in adolescence [13]. Children’s self-worth, inferential styles, and attitudes are in?uenced by the quality of their relationships with their parents [14, 15].
Children who are raised by parents characterized by low warmth [16] and/or high criticism [17, 18] tend to develop more depressogenic cognitive styles than other children. Parents who impose rigid or perfectionistic standards on their children may influence their children to adopt those same standards in themselves, resulting in the formulation of dysfunctional attitudes [17, 19].
Findings from previously mentioned studies had proposed various potential treatment implications, with special recommendation for greater inclusion of caregivers in the treatment of depressed children [20-22]. Cognitive-behavioral therapy (CBT) has been evaluated by several studies as the best-supported psychosocial intervention for treatment of Major Depressive Disorder depression (MDD) in children and adolescents [23-26]. Recently, many studies supported that the efficacy of CBT can be enhanced by including adjunctive sessions for positive parenting practices to individual CBT sessions [27-32]. Results suggest that including parents is associated with positive treatment outcomes, regarding reduction in depressive symptoms and maintenance of results in short-term follow-ups.
There are many family-focused interventions for childhood MDD that target parenting practices, but few interventions address parental psychopathology. In this study, I proposed an approach addressing psychopathology in parents as well as children through providing cognitive behavioral therapy for both children and their parents, separately, in treatment of childhood MDD. I hypothesized that modifying negative cognitive styles of parents will in turn replace their negative inferential feedbacks with positive and supportive ones, hence parents can model healthy adaptive cognitive styles to their children, helping them to overcome depression. This study’s objective is to evaluate effectiveness of this approach.
2. Methods
2.1. Participants
Children and their parents were recruited from child psychiatry out-patient clinic, Abbassia psychiatric hospital. Children were evaluated by specialized child psychiatrists through psychiatric clinical interview based on Diagnostic and statistical manual of mental disorders, 5th edition. (DSM-5) published by American Psychiatric Association [33]. DSM-5 diagnoses were made based on information derived from the parents about the child and from the child about him/herself.
The inclusion criteria were that the child’s age was between 8 and 12 years, the child met DSM-5 criteria for MDD, and that child and his/her parents are willing to participate in treatment. Exclusion criteria were receiving another psychosocial treatment for depression during the 3-month intervention phase, and having primary symptoms of a non-depressive disorders that suggested a need for alternative services, such as severe conduct disorder, schizophrenia-spectrum and other psychotic disorders, intellectual disability. Another exclusion criterion was reporting of acute suicidality, meaning suicidal ideation with a plan and level of intent that made the child a high-risk case.
Children who were taking antidepressant medications were eligible if they continued to meet inclusion criteria and had been on the same medication and dose for at least 3 months prior to entering the study and throughout the 3-month intervention phase. Twenty children and their parents were evaluated for participation in this study. Six children did not meet diagnostic criteria for MDD and were referred to other treatment interventions. Five children presented with intellectual disability and also were referred to other treatment interventions. Two families dropped out before the start of treatment. Thus, seven children and their parents participated in this study, none of them expressed an interest to discontinue participation during the course of the treatment.
The children’s age ranged from 9 to 11 years old (M = 10.1; SD = 0.9), most of them were males (85.7%). Three children were taking antidepressant medication, but they met the requirement of fulfilling criteria of MDD and were using the same medication and dose for at least 3 months prior to enrollment and throughout their participation. Most of parents participating in treatment were mothers (77.8%), see Table 1.
|
Number |
Percentage |
||
|
Child gender |
Male |
6 |
85.7% |
|
Female |
1 |
14.3% |
|
|
Child use of antidepressant medications |
No |
4 |
57.1% |
|
Yes |
3 |
42.9% |
|
|
Parents participating in the treatment |
Mother |
7 |
77.8% |
|
Father |
2 |
22.2% |
|
Table 1: Characteristics of participants.
2.2. Procedure
Cognitive-behavioral therapy was provided separately to children and their parents in 12 weekly sessions, each lasting one hour, in group therapy format. Parents’ sessions were parallel to children sessions, focusing on learning the same cognitive-behavioral therapy skills and techniques taught in the children’s groups, aiming to modify negative cognitive styles of parents as well as children.
Parents’ sessions’ main target was modifying the parents’ negative cognitive styles, which would in turn replace their negative inferential feedback with positive and supportive one, hence parents can model healthy adaptive cognitive styles to their children. This was prepared for by providing psychoeducation about childhood MDD (including symptoms, contributing factors, course, treatment), and supporting the importance of parents’ roles as models and change-agents for their children.
Parents also learned to promote their children’s generalization of skills by using the same terms and concepts learned in sessions at home, and by encouraging their children to practice these new skills outside of session, parents were aided in applying these skills to their own family interactions. So instead of dependence solely on modifying children’s cognitive styles directly, modifying parents’ negative cognitive styles related to parents themselves and to their children would reduce parental negative inferential feedback which indirectly would modify children’s negative cognitive styles through modeling.
Regarding children’s sessions, cognitive-behavioral therapy skills and techniques were designed to match the generally more concrete cognitive level of children, skills were divided into small components that can be mastered in a step-wise fashion. Exercises were presented as “games” initially to make them more engaging to children and to increase the likelihood that these “games” could become their tools for combating depression. To encourage children to complete home assignments token economy was used, also the term “Home assignment” was avoided as many children have negative associations with it, so it was replaced with “Happiness pills”. Practice-at-home was a crucial part of treatment and was included weekly, so both children and parents received simplified sessions handouts and home assignments to implement and generalize the usage of cognitive-behavioral therapy strategies within children and parents’ daily life. Table 2 demonstrates an overview of the sessions’ objectives.
|
Children’s group |
Parents’ group |
|
|
Session 1 |
Introduction and group rules |
Introduction, group rules, and orientation |
|
Session 2 |
Psychoeducation about symptoms of depression |
Psychoeducation about childhood depression, |
|
Session 3 |
Identifying different types of feelings and situations |
Identifying different types of feelings and situations |
|
Session 4 |
Measuring feelings intensity, and identifying impact |
Measuring feelings intensity, and identifying |
|
Session 5 |
Controlling intense negative feelings by relaxation |
Controlling intense negative feelings by relaxation |
|
Session 6 |
Identifying differences between thoughts, feelings |
Identifying differences between thoughts, feelings |
|
Session 7 |
Identifying different types of thoughts (core beliefs |
Identifying different types of thoughts (core beliefs |
|
Session 8 |
Identifying different types of cognitive distortions, |
Identifying different types of cognitive distortions, |
|
Session 9 |
Challenging and testing negative thoughts and |
Challenging and testing negative thoughts and |
|
Session 10 |
Enhancing self-esteem |
Highlighting impact of positive parenting |
|
Session 11 |
Problem-solving skills training |
Problem-solving skills training |
|
Session 12 |
Anti-bullying techniques training, and review |
Psychoeducation about strategies for |
Table 2: Overview of sessions’ objectives.
2.3. Measures
The Arabic version of Parent-rated Mood and Feelings Questionnaire PMFQ [34] was used pre-treatment and post-treatment to evaluate depression symptoms. It is a 34-item questionnaire developed to measure depressive symptoms for children and adolescents aged between 8 and 18 years old [35]. The PMFQ statements asked parents to rate on a 3-point scale (0 = Not true, 1 = Sometimes, and 2 = True) how their child felt or acted in the past two weeks. A cut-off score of 28 has been recommended to produce optimal sensitivity and specificity [34]. Children were also clinically evaluated pre-treatment and post-treatment by specialized child psychiatrists through psychiatric clinical interview based on DSM-5 [33].
2.4. Ethical considerations
This study was approved by the ethics committee of Abbassia psychiatric hospital. Written consent was obtained from parents on behalf of their children and for their own participation after discussing the aim of the study and the treatment provided with them.
2.5. Statistical analysis
Data were summarized using mean and standard deviation in quantitative data, and using frequency (count) and relative frequency (percentage) for categorical data. For comparison of serial measurements before and after treatment within each patient, the nonparametric Wilcoxon signed-rank test was used. Comparisons between absolute change and percent change of PMFQ scores pre- and post-treatment between children using and children non-using antidepressant medications were done using the nonparametric Mann–Whitney U test. These tests do not assume that dependent variables are normally distributed. Additionally, these tests are less vulnerable to the influence of extreme scores because they rely on ranks. These considerations and the small sample size make this a generally conservative approach.
3. Results
At the end of the treatment, all of the children no longer met DSM-5 criteria for Major depressive disorder according to clinical evaluation by specialized child psychiatrists. Figure 1 demonstrates that the pre-treatment PMFQ score (M = 43.1; SD = 10.8) which indicates depressive disorder, decreased at post-treatment (M =8.1; SD =5.6), a score indicating that depressive disorder was unlikely. The change of reported depressive symptoms on PMFQ pre- and post-treatment is shown in Table 3
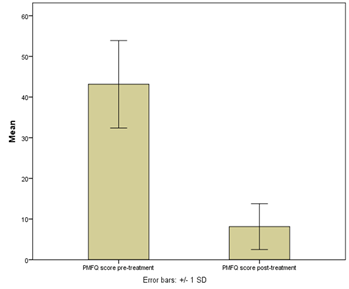
Figure 1: Comparison of pre-treatment and post-treatment mean and standard deviation scores of parent-rated mood and feelings questionnaire PMFQ.
|
Pre-treatment |
Post-treatment |
|||||
|
Not true |
Sometimes |
True |
Not true |
Sometimes |
True |
|
|
Miserable or unhappy |
0 (0%) |
0 (0%) |
7 (100%) |
4 (57.14%) |
3 (42.86%) |
0 (0%) |
|
Didn't enjoy anything |
0 (0%) |
0 (0%) |
7 (100%) |
5 (71.43%) |
2 (28.57%) |
0 (0%) |
|
Less hungry |
3 (42.86%) |
0 (0%) |
4 (57.14%) |
5 (71.43%) |
1 (14.29%) |
1 (14.29%) |
|
Ate more |
6 (85.71%) |
0 (0%) |
1 (14.29%) |
6 (85.71%) |
0 (0%) |
1 (14.29%) |
|
Tired |
2 (28.57%) |
0 (0%) |
5 (71.43%) |
6 (85.71%) |
1 (14.29%) |
0 (0%) |
|
Moving and walking slowly |
4 (57.14%) |
1 (14.29%) |
2 (28.57%) |
7 (100%) |
0 (0%) |
0 (0%) |
|
Restless |
3 (42.86%) |
0 (0%) |
4 (57.14%) |
4 (57.14%) |
3 (42.86%) |
0 (0%) |
|
No good |
0 (0%) |
0 (0%) |
7 (100%) |
5 (71.43%) |
2 (28.57%) |
0 (0%) |
|
Blamed self |
3 (42.86%) |
0 (0%) |
4 (57.14%) |
6 (85.71%) |
1 (14.29%) |
0 (0%) |
|
Indecisive |
5 (71.43%) |
0 (0%) |
2 (28.57%) |
6 (85.71%) |
1 (14.29%) |
0 (0%) |
|
Irritable |
0 (0%) |
0 (0%) |
7 (100%) |
1 (14.29%) |
6 (85.71%) |
0 (0%) |
|
Talking less |
2 (28.57%) |
0 (0%) |
5 (71.43%) |
6 (85.71%) |
1 (14.29%) |
0 (0%) |
|
Talking slowly |
2 (28.57%) |
0 (0%) |
5 (71.43%) |
6 (85.71%) |
1 (14.29%) |
0 (0%) |
|
Cried a lot |
1 (14.29%) |
0 (0%) |
6 (85.71%) |
5 (71.43%) |
2 (28.57%) |
0 (0%) |
|
No good in future |
2 (28.57%) |
0 (0%) |
5 (71.43%) |
5 (71.43%) |
2 (28.57%) |
0 (0%) |
|
Not worth living |
2 (28.57%) |
0 (0%) |
5 (71.43%) |
5 (71.43%) |
2 (28.57%) |
0 (0%) |
|
Thoughts of death |
2 (28.57%) |
1 (14.29%) |
4 (57.14%) |
7 (100%) |
0 (0%) |
0 (0%) |
|
Better off without |
6 (85.71%) |
0 (0%) |
1 (14.29%) |
7 (100%) |
0 (0%) |
0 (0%) |
|
Suicidal thoughts |
4 (57.14%) |
0 (0%) |
3 (42.86%) |
7 (100%) |
0 (0%) |
0 (0%) |
|
Not see friends |
1 (14.29%) |
1 (14.29%) |
5 (71.43%) |
5 (71.43%) |
2 (28.57%) |
0 (0%) |
|
Poor concentration |
3 (42.86%) |
0 (0%) |
4 (57.14%) |
4 (57.14%) |
3 (42.86%) |
0 (0%) |
|
Bad things happen |
3 (42.86%) |
0 (0%) |
4 (57.14%) |
4 (57.14%) |
3 (42.86%) |
0 (0%) |
|
Hated self |
3 (42.86%) |
0 (0%) |
4 (57.14%) |
5 (71.43%) |
2 (28.57%) |
0 (0%) |
|
Bad person |
2 (28.57%) |
1 (14.29%) |
4 (57.14%) |
5 (71.43%) |
2 (28.57%) |
0 (0%) |
|
Looked ugly |
4 (57.14%) |
1 (14.29%) |
2 (28.57%) |
6 (85.71%) |
1 (14.29%) |
0 (0%) |
|
Worried about aches and pains |
5 (71.43%) |
0 (0%) |
2 (28.57%) |
6 (85.71%) |
1 (14.29%) |
0 (0%) |
|
Lonely |
1 (14.29%) |
0 (0%) |
6 (85.71%) |
6 (85.71%) |
1 (14.29%) |
0 (0%) |
|
Unloved |
0 (0%) |
1 (14.29%) |
6 (85.71%) |
4 (57.14%) |
3 (42.86%) |
0 (0%) |
|
No fun at school |
3 (42.86%) |
0 (0%) |
4 (57.14%) |
5 (71.43%) |
2 (28.57%) |
0 (0%) |
|
Never be as good |
1 (14.29%) |
2 (28.57%) |
4 (57.14%) |
4 (57.14%) |
3 (42.86%) |
0 (0%) |
|
Did everything wrong |
1 (14.29%) |
1 (14.29%) |
5 (71.43%) |
5 (71.43%) |
2 (28.57%) |
0 (0%) |
|
Poor sleep |
4 (57.14%) |
1 (14.29%) |
2 (28.57%) |
7 (100%) |
0 (0%) |
0 (0%) |
|
Slept more |
4 (57.14%) |
0 (0%) |
3 (42.86%) |
7 (100%) |
0 (0%) |
0 (0%) |
|
Not cheered up |
0 (0%) |
0 (0%) |
7 (100%) |
7 (100%) |
0 (0%) |
0 (0%) |
Table 3: Reported depressive symptoms on PMFQ pre and post treatment.
Results of the nonparametric Wilcoxon signed-rank test indicated that participated children demonstrated significant improvement of depression symptomology as evidenced by differences between pre-treatment and post-treatment PMFQ scores (W value = 0, P-value = 0.025). See Table 4.
|
Minimum |
Maximum |
Mean |
SD |
P-value |
||
|
PMFQ |
Pre-treatment |
30 |
54 |
43.1 |
10.8 |
0.025 |
|
Post-treatment |
2 |
19 |
8.1 |
5.6 |
PMFQ; Parent-rated mood and feelings questionnaire
Table 4: Pre- and post-treatment PMFQ scores.
The nonparametric Mann–Whitney U test did not demonstrate a statistically significant difference between absolute change (U value = 2, P-value > 0.2) and percent change (U value = 6, P-value >0.2) between pre- and post-treatment PMFQ scores among children using and children non-using antidepressant medications. See Table 5.
|
Number |
Mean |
SD |
P-value |
||
|
Absolute change |
Children non-using medications |
4 |
40.5 |
8.0 |
> 0.2 |
|
Children using medications |
3 |
27.7 |
9.1 |
||
|
Percent change |
Children non-using medications |
4 |
81.4% |
13.7% |
> 0.2 |
|
Children using medications |
3 |
80.2% |
10.2% |
Table 5: Change between pre-/post-treatment PMFQ scores among children using/non-using medications.
4. Discussion
This pilot study examined the effectiveness of providing cognitive-behavioral group therapy for both children and parents, separately, in treatment of childhood MDD. After participating in this study, all the children no longer met DSM-5 criteria for MDD according to clinical evaluation by specialized child psychiatrists. Results demonstrated statistically significant reductions of depressive symptoms of children as reported by their parents. The results also demonstrated that none of the children had a score indicative of depressive disorder at the end of treatment. However, results did not demonstrate statistically significant difference between improvement of children using and children non-using antidepressant medications. These findings suggested efficacy of this approach and supported the study’s hypothesis.
The addition of parents’ sessions followed findings from studies linking development of childhood depression to modeling of parents’ negative cognitive styles, direct learning from negative parental inferential feedback and indirect learning from negative parenting practices [5-9, 16-17, 19], and recommendations for greater inclusion of parents in the treatment of depressed children [20-22].
This study’s approach focused on addressing psychopathology of parents as well as their children through providing cognitive behavioral group therapy for both children and parents in treatment of childhood MDD, hypothesizing that modifying negative cognitive styles of parents will in turn replace their negative inferential feedbacks with positive and supportive ones, hence parents can model healthy adaptive cognitive styles to their children, helping them to overcome depression. Throughout the course of the treatment none of the participating children nor their parents expressed an interest to discontinue participation which suggest high acceptability of this approach.
The main limitations of this pilot study were small sample size, absence of control group, and lack of follow-up data. This study aimed at providing preliminary data on treatment impact, feasibility, acceptability; a randomized controlled trial using large numbers and long-term follow up is needed to clarify treatment ef?cacy.
5. Conclusions
In conclusion, the present results of this Pilot study supported the ef?cacy of providing cognitive behavioral group therapy for both children and their parents, separately, in the treatment of childhood MDD. A randomized controlled trial is needed to further clarify the promise of this study’s ?ndings and determine the degree to which this approach is effective regarding long-term improvement and relapse prevention of childhood MDD.
Acknowledgments
I would like to thank the children and their parents who participated in this study.
Role of Funding Resources
There are no funding resources.
Conflicts of Interest
There are no conflicts of interest.
References
- Beck AT. Depression: clinical, experimental and theoretical aspects. New York, NY: Harper & Row (1967).
- Beck AT, Rush AJ, Shaw BF, et al. Cognitive therapy of depression. New York: Guilford Press (1979).
- Bandura A. Social foundations of thought and action: A social-cognitive theory. Upper Saddle River, NJ: Prentice Hall (1986).
- Seligman MEP, Peterson C, Kaslow NJ, et al. Attributional style and depressive symptoms among school children. J Abnorm Psychol 93 (1984): 235-238.
- Stark KD, Schmidt KL, Joiner TE. Cognitive triad: Relationship to depressive symptoms, parents’ cognitive triad, and perceived parental messages. J Abnorm Child Psychol 24 (1996): 615-631.
- Abramson LY, Alloy LB, Hogan ME, et al. Cognitive vulnerability to depression: Theory and evidence. J Cogn Psychother: An International Quarterly 13 (1999): 5-20.
- Alloy LB, Abramson LY. The Temple–Wisconsin Cognitive Vulnerability to Depression (CVD) Project: Conceptual background, design, and methods. J Cogn Psychother: An International Quarterly 13 (1999): 227-262.
- Garber J, Flynn C. Origins of the depressive cognitive style. In D. Routh & R. J. DeRubeis (Eds.). The science of clinical psychology: Evidence of a century’s progress, pp. 53-93. Washington, DC: American Psychological Association (1998).
- Haines BA, Metalsky GI, Cardamone AL, et al. Interpersonal and cognitive pathways into the origins of attributional style: A developmental perspective. In T. Joiner & J. C. Coyne (Eds.), The interactional nature of depression, pp. 65-92. Washington, DC: American Psychological Association (1999).
- Alloy L, Abramson L, Tashman N, et al. Developmental Origins of Cognitive Vulnerability to Depression: Parenting, Cognitive, and Inferential Feedback Styles of Parents of Individuals at High and Low Cognitive Risk for Depression. Cognit Ther Res 25 (2001): 397-423.
- Garber J, Flynn C. Predictors of depressive cognitions in young adolescents. Cognit Ther Res 25 (2001): 353-376.
- Young J. Cognitive therapy for personality disorders: A schema-focused approach. Sarasota, FL: Professional Resource Exchange (1991).
- Koestner R, Zuroff DC, Powers TA. Family origins of adolescent self-criticism and its continuity into adulthood. J Abnorm Psychol 100 (1991): 191-197.
- Bowlby J. Developmental psychiatry comes of age. Am J Psychiatry 145 (1988): 1-10.
- Eisner JP. The origins of explanatory style: Trust as a determinant of optimism and pessimism. In G. M. Buchanan & M. E. P. Seligman (Eds.), Explanatory style, pp.49-55. Hillsdale, NJ: Erlbaum (1995).
- Whisman MA, Kwon P. Parental representations, cognitive distortions, and mild depression. Cognit Ther Res 16 (1992): 557-568.
- Gamble S, Roberts J. Adolescents’ perceptions of primary caregivers cognitive style: The roles of attachment security and gender. Cognit Ther Res 29 (2005): 123-141.
- Randolph J, Dykman B. Perceptions of parenting and depression-proneness in the offspring: Dysfunctional attitudes as a mediating mechanism. Cognit Ther Res 22 (1998): 377-400.
- Ingram RE, Overbey T, Fortier M. Individual differences in dysfunctional automatic thinking and parental bonding: Specificity of maternal care. Pers Individ Differ 30 (2001): 401-412.
- Hammen C, Rudolph K, Weisz J, et al. The context of depression in clinic referred youth: Neglected areas of treatment. J Am Acad Child Adolesc Psychiatry 38 (1999): 64-71.
- Stark KD, Swearer S, Kurowski C, et al. Targeting the child and the family: A holistic approach to treating child and adolescent depressive disorders. In E. D Hibbs & P. S. Jensen (Eds.), Psychosocial treatments for child and adolescent disorder: Empirically based strategies for clinical practice. Washington, DC: American Psychological Association (1996): 207-238.
- Vuchinich S, Wood B, Angelelli J. Coalitions and family problem solving in the psychosocial treatment of preadolescents. In E. D. Hibbs & P. S. Jensen (Eds.), Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. Washington, DC: American Psychological Association (1996): 497-518.
- Harrington R, Whittaker J, Shoebridge P. Psychological treatment of depression in children and adolescents. Br J Psychiatry 173 (1998): 291-298.
- Weersing VR, Weisz JR. Community clinic treatment for depressed youth: Benchmarking usual care against CBT clinical trials. J Consult Clin Psychol 70 (2002): 299-310.
- Weisz JR, Hawley KM, Jensen-Doss A. Empirically tested psychotherapies for youth internalizing and externalizing problems and disorders. Child Adolesc Psychiatr Clin N Am 13 (2004): 729-815.
- Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychol. Bull 132 (2006): 132-149.
- Eckshtain D, Gaynor ST. Combining individual Cognitive Behaviour Therapy and caregiver–child sessions for childhood depression: An open trial. Clin Child Psychol Psychiatry 17 (2012): 266-283.
- Eckshtain D, Gaynor ST. Combined Individual Cognitive Behavior Therapy and Parent Training for Childhood Depression: 2-3-Year Follow-Up. Child Fam Behav Ther 35 (2013).
- Fristad MA, Goldberg-Arnold JS, Gavazzi SM. Multi-family psychoeducation groups in the treatment of children with mood disorders. J Marital Fam Ther 29 (2003): 491-504.
- McLeod BD, Weisz JR. The Therapy Process Observational Coding System - Alliance Scale: Measure characteristics and prediction of outcome in usual clinical practice. J Consult Clin Psychol 73 (2005): 323-333.
- Sander JB, McCarty CA. Youth depression in the family context: familial risk factors and models of treatment. Clin Child Fam Psychol Rev 8 (2005): 203-219.
- Tompson MC, Pierre CB, Haber FM, et al. Family-focused Treatment for Childhood-onset Depressive Disorders: Results of an Open Trial. Clin Child Psychol Psychiatry 12 (2007): 403-420.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author (2013).
- Tavitian L, Atwi M, Bawab S, et al. The Arabic Mood and Feelings Questionnaire: Psychometrics and Validity in a Clinical Sample. Child Psychiatry Hum Dev 45 (2014): 361-368.
- Costello EJ, Angold A. Scales to assess child and adolescent depression: checklists, screens, and nets. J Am Acad Child Adolesc Psychiatry 27 (1988): 726-737.
