Effectiveness of Dobutamine to Facilitate Induction of Supraventricular Tachycardia Compared to Isoproterenol
Article Information
Joseph Donnelly1, Ali Seyar Rahyab1, Haisam Ismail1, Laurence Epstein1, Bruce Goldner1
1Northwell Health, North Shore University Hospital, Manhasset, NY, USA
*Corresponding author:Bruce Goldner. Northwell Health, North Shore University Hospital, Manhasset, NY, USA
Received: May 30, 2023; Accepted: June 08, 2023; Published: October 03, 2023
Citation: Joseph Donnelly, Ali Seyar Rahyab, Haisam Ismail, Laurence Epstein, Bruce Goldner. Effectiveness of Dobutamine to Facilitate Induction of Supraventricular Tachycardia Compared to Isoproterenol. Cardiology and Cardiovascular Medicine. 7 (2023): 330-335.
View / Download Pdf Share at FacebookAbstract
Background: Isoproterenol has been utilized for the induction of supraventricular and ventricular arrhythmias during electrophysiological (EP) testing. However, with the increasing number of catheter ablations performed and the significant increase in the price of isoproterenol in 2015, the cost implications led us to explore alternatives, although the price of isoproterenol has decreased since 2015. Dobutamine is a synthetic compound which was developed from isoproterenol with a similar ability to enhance conduction and shorten refractoriness of the AV node, thus making it an ideal choice given its lower cost. The effectiveness of dobutamine to facilitate induction of arrhythmias has not been extensively studied.
Objective: To evaluate the ability of dobutamine to reproduce the properties of isoproterenol to help facilitate induction of arrhythmias. This study also evaluated the safety of dobutamine.
Methods: From January 2014 to January 2017, 174 non-consecutive patients, with a diagnosis of confirmed or suspected supraventricular tachycardia (SVT) were enrolled. Dobutamine was used to induce SVT if patients were non-inducible at baseline using programmed electrical stimulation (PES). Post procedure, dobutamine was used to confirm noninducibility. Data such as demographics, comorbidities, and recurrence of arrhythmia were collected. The procedural end point was confirmation of non-inducible SVT. A different cohort of twenty non-consecutive patients, who received isoproterenol to facilitate induction of SVT, were evaluated in this study commensurate when dobutamine was being used in the other cohort of patients. Twenty patients who received 10, 20 and 30 mcg/kg/min of dobutamine and 10 patients who received 1 and 2 ug/min of isoproterenol were selected to study the electrophysiologic effects of escalating doses of these medications.
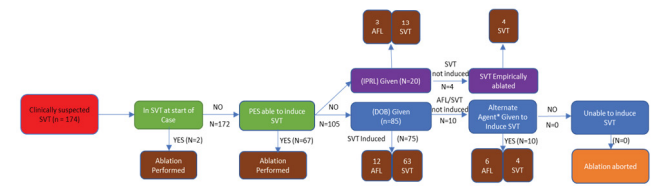
Results: Sixty-seven of 172 patients (39%) did not require pharmacologic intervention to induce AT, AVNRT or AFL. Of the 105 remaining patients, 85 patients received dobutamine to induce AT, AVNRT or AFL and 20 patients received isoproterenol. Overall, there was no difference in inducibility of SVT and atrial flutter with PES and dobutamine compared with PES and isoproterenol. However, when SVT inducibility was evaluated alone without atrial flutter inducibility, dobutamine with PES induced 94% of patients whereas isoproterenol with PES induced 80%, p = 0.03. Sustained polymorphic ventricular tachycardia occurred in 3.5% of dobutamine plus PES cases compared with 5% of isoproterenol plus PES cases. There was no difference in the rate of recurrence of SVT and atrial flutter whether dobutamine or isoproterenol was used.
Conclusion: This study supports the use of dobutamine as an adjunct to electrophysiologic study of patients with SVT and atrial flutter both for the induction of SVT and assessment of procedural success. In our study dobutamine was safe and effective.
Keywords
Isoproterenol; Dobutamine; Svt; Supraventricular Tachycardia; Catheter Ablation; Electrophysiology; Drug Cost
Isoproterenol articles; Dobutamine articles; Svt articles; Supraventricular Tachycardia articles; Catheter Ablation articles; Electrophysiology articles; Drug Cost articles.
Article Details
Graphical abstract:
Introduction
Isoproterenol is a β1β2 agonist which has been used during electrophysiology (EP) testing to facilitate induction of both supraventricular and ventricular arrhythmias. However, for various reasons, the cost of isoproterenol increased exponentially such that a 1 mg in 5 cc vial was approximately $1264.70 in 2014 [1-3]. There are instances in which [2] vials were needed which dramatically increased the cost to $2529.40 per EP study. The cost implications were significant given the increasing number of catheter ablations performed since 1992, when there was an increase in the estimated number of ablations performed annually from 10,000, to approximately 50,000 atrial fibrillation ablations only in 2013 [4,5]. Fortunately, there were other pharmacologic agents available that replaced isoproterenol, with similar outcomes and much less cost such as dobutamine which was approximately $28 for a 500mg/250 cc bag. Reasons for the price change were multifactorial; however, the dramatic price increase was cotemporaneous with changes in ownership rights. Marathon pharmaceutical bought isoproterenol from Hospira, and subsequently sold it to Valeant pharmaceuticals, who, on the same day, increased the price from $218 [3]. to $1200 per dose [1-3]. This prompted attention from the public, including senator Bernard Sanders.3 Heart Rhythm Society raised this issue in a Special Notice on April 5, 2015 as members of the Society called for exploration of alternative options. Electrophysiologists and hospitals have coped with the change in various ways, including the rationing of the drug. Others have resorted to using dobutamine in its place. Dobutamine is a synthetic compound which has predominantly β1 agonist with mild β2 properties [6]. It was initially developed by modifying isoproterenol and at equipotent inotropic doses, dobutamine has 25% of the chronotropic effects of isoproterenol [7]. The S-(-)-enantiomer of dobutamine possesses relatively potent α1 adrenoceptor agonist activity, but weak β1 and β2 agonist activity. In contrast, R-(+)-dobutamine possesses predominantly β1 and β2 adrenoceptor agonist activity and possesses only minimal α agonist activity but behaves more as an alpha antagonist. The net effect of dobutamine is mostly β1 activity with mild β2 activity and minor α1 activity. The objective during EP testing is to trigger supraventricular and ventricular arrhythmias. β1 stimulation enhances conduction and shortens refractoriness to facilitate induction of cardiac arrhythmias. Thus, dobutamine is a logical choice to facilitate induction of arrhythmias. To our knowledge, dobutamine has not been extensively studied as an agent to facilitate supraventricular arrhythmia induction. A retrospective chart review study in Bogota, Colombia compared isoproterenol to dobutamine for inducing arrhythmia with programmed electrical stimulation (PES) and found no statistically significant differences in the frequency of arrhythmias between the two drugs [8]. Another retrospective chart review study done in Karachi, Pakistan demonstrated an overall 90% success rate of radiofrequency ablation, of mostly recurrent supraventricular tachycardia (SVT), using dobutamine alone to increase the heart rate 10-20% above baseline in patients who could not be induced with pacing protocols [9]. Another study limited to twenty male patients reported on utilizing dobutamine to help facilitate induction of ventricular outflow tract premature ventricular complexes (PVCs) and ventricular tachycardia (VT) [10]. Gianni and colleagues studied high- dose dobutamine and isoproterenol for inducibility of atrial arrhythmias during atrial fibrillation ablation in a prospective randomized 2x2 crossover study of 50 patients [11]. In that study, atrial arrhythmias induced during dobutamine infusion were comparable to that induced during isoproterenol infusion, with less hypotension when dobutamine was infused [11]. Our group evaluated the site-specific effects of dobutamine on cardiac conduction and refractoriness in 40 patients and found that the sinus cycle length, AV block cycle length, VA block cycle length, AV node effective refractory period and AH intervals all shortened during incremental dosing of dobutamine from 5 mcg/kg/min to 20 mcg/kg/min. We also found that dobutamine was well-tolerated and safe to use during PES [12]. The safety of dobutamine was evaluated predominantly in the setting of stress imaging which was clinically introduced in the 1980s. Overall mortality was <0.01%. Of note, the incidence of SVTs was 1.3% [13].
In this study, like in a previous study [12], we intended to formally evaluate the ability of dobutamine to reproduce the properties of isoproterenol, i.e., accelerate heart rate, shorten AH interval, the antegrade AV block cycle length and the antegrade AV node effective refractory period, to help facilitate induction of arrhythmias. This study also evaluated the safety of dobutamine.
Materials and Methods
Study population:
From January 2014 to January 2017, 174 non-consecutive patients with a diagnosis of suspected or confirmed supraventricular tachycardia (SVT) met criteria for inclusion. The study consisted of two groups. Group 1 consisted of patients with known SVT undergoing ablation of either AV nodal reentrant tachycardia (AVNRT) or focal atrial tachycardia. Group 2 consisted of patients with sustained cavotricuspid isthmus dependent atrial flutter (CTI AFL) at baseline. EP study and ablation were performed at a single center. Inclusion criteria were: (1) History of SVT or CTI AFL. (2) Inability to induce SVT with incremental atrial pacing. (3) Absence of absolute contraindication to isoproterenol or dobutamine.
Procedure descriptions
Written consent was obtained in all patients prior to study. All patients were studied in a fasting, sedated state. All antiarrhythmic drugs were discontinued the day of the case.
Patients with known SVT undergoing ablation (Group 1), underwent ablation per the standard procedure outlined below. Dobutamine was used to induce SVT if patients were non- inducible at baseline using programmed atrial and ventricular stimulation. Post procedure, dobutamine was used to confirm non-inducibility. Patients with either spontaneous or induced sustained CTI AFL at baseline (Group 2), underwent ablation, and dobutamine was used to confirm non-inducibility.
All procedures were performed under conscious sedation using fentanyl and midazolam. Quadripolar electrode catheters were inserted via the femoral vein and positioned in the heart using fluoroscopic guidance. Programed atrial and ventricular stimulation was performed using a protocol described by Cossú and colleagues .13 After failure to induce SVT using programmed atrial and ventricular stimulation, a continuous infusion of dobutamine at 5ug/min/kg was administered. The infusion rate was increased to achieve a heart rate of at least 20% above baseline. Isoproterenol was used in a separate cohort using escalating doses starting at 0.5 mcg/min and increasing the dose to achieve a heart rate of 20% above baseline.
Data was collected on demographics, co-morbidities, and recurrence of arrhythmia. Severe hypertension was defined as a systolic blood pressure >180 mm Hg and hypotension as a systolic blood pressure of < 90 mm Hg. The procedural end point was confirmation of non-inducible SVT.
A second sub-study was performed to assess the effect of isoproterenol and dobutamine on cardiac conduction and refractoriness. Parameters of sinus cycle length, AH interval, HV interval, QRS duration, QT interval, AV nodal effective refractory period and AV block cycle length before and after infusion of the selected drug were recorded.
Statistics
Continuous variables were expressed as mean ± standard deviation. Unpaired Student t test was applied for comparisons of continuous variables. Data were expressed with 95% confidence intervals. Categorical data were compared using Fisher’s Exact Test. Statistical significance was considered a p value <0.05.
Results
Baseline demographics are provided in Table 1. There was no significance difference with respect to age, gender, medications, ejection fraction and patients with coronary disease amongst the patients who underwent PES only, dobutamine + PES and isoproterenol +PES. However, the baseline systolic blood pressure was higher, and the baseline heart rate was lower in the group of patients who underwent isoproterenol infusion + PES. Table 2 demonstrated that there was no significant difference in the distribution of atrial arrhythmias in the patients who underwent PES, compared with those who received dobutamine + PES or isoproterenol + PES.
Inducibility of SVT during PES with and without Addition of Pharmacological Agent
PES alone induced SVT or cavotricuspid isthmus dependent atrial flutter (CTI AFL) in 67 of 172 (39%) of cases. Of the 105 remaining patients, 85 underwent PES with dobutamine. Of the 67 patients known to have SVT, 63 (94%) were induced with PES and dobutamine. The other 4 patients required the addition of atropine for induction. Of the 18 patients who had CTI AFL, 12 (67%) were induced with PES and dobutamine and 6 (33%) were induced with PES, dobutamine and atropine. Of the remaining 20 patients who received isoproterenol after PES failed to induce tachycardia, SVT was induced in 13 (76%) of the 17 patients
Table 1: Baseline Characteristics
|
PES N=67 |
DOB n=85 |
ISPRL n=20 |
P DOB v ISPRL |
|
|
Age (years) |
46 ± 6.8 |
58 ± 12.1 |
62 ± 9.8 |
0.25 |
|
Male n (%) |
29 (43) |
41 (48) |
10 (50) |
0.9 |
|
NDP CCB n (%) |
3 (4) |
5 (6) |
2 (10) |
0.5 |
|
DP CCB n (%) |
4 (6) |
9 (11) |
0 (0) |
N/A |
|
ACE/ARB n (%) |
9 (13) |
14 (16) |
5 (25) |
0.35 |
|
Nitrates n (%) |
3 (4) |
2 (2) |
0 |
N/A |
|
Beta Blocker n (%) |
19 (28) |
30 (35) |
9 (45) |
0.45 |
|
EF (%) |
55.4 ± 3.7 |
57.8 ± 3.7 |
55.6 ± 7.6 |
0.7 |
|
SBP (mm Hg) |
123.6 ± 5.1 |
114.7± 3.4 |
130.5 ± 8.2 |
0.001 |
|
HR (BPM) |
89.3 ± 6.8 |
84.8 ± 4.5 |
70 ± 5.9 |
0.001 |
|
CAD |
12 (18) |
15 (18) |
6 (30) |
0.2 |
ACE/ARB Angiotensin converting enzyme inhibitor/Angiotensin Receptor Blocker, BPM Beats Per Minute, CAD Coronary Artery Disease, DOB Dobutamine, DP Dihydropyridine Calcium Channel Blocker, EF (Ejection Fraction), ISPRL Isoproterenol, NDP CCB Non-Dihydropyridine Calcium Channel Blocker, PES Programmed Electrical Stimulation, SBP Systolic Blood Pressure. Continuous variables are reported as mean ± standard deviation. Categorical data are reported as frequency (percentage). P values reflect the comparison between the DOB and ISPRL groups. A P value < 0.05 was considered significant.
known to have SVT and 3 (100%) of the patients known to have CTI AFL. Dobutamine was able to facilitate SVT at a higher rate than isoproterenol in those patients who could not be induced with PES alone (94% versus 76%, p = 0.03) in this study. Overall, however, there was no significant difference in inducibility of both SVT and CTI AFL with dobutamine versus isoproterenol (88% versus 80, p = 0.35). There was no significant difference in arrhythmia recurrence at a mean of 52 days whether the patients were induced with PES and dobutamine or with PES and isoproterenol. In addition, there was no significant difference in the occurrence of atrial fibrillation during a mean of 52 days of follow-up between the group of patients undergoing PES and dobutamine and PES and isoproterenol (Table 3).
Data on adverse events were collected (Table 4). There were no deaths during this study. Polymorphic sustained ventricular tachycardia occurred in 3.5% of cases in the dobutamine group and 5% of cases in the isoproterenol groups (p = 0.6). There was a higher incidence of severe hypertension in the patients who received dobutamine, but the difference was not statistically significant (p = 0.12). There was a statistically significant higher incidence of hypotension in the patients who received isoproterenol compared with those who received dobutamine (p < 0.01).
In the sub study of conduction effects, 30 patients had data recorded for electrophysiologic parameters before and after infusion. Results are reported in Table 5. Dobutamine and isoproterenol had similar effects on cardiac conduction.
Table 2: Spontaneous Arrhythmias Induced with PES Alone, DOB or ISPRL
|
PES n=67 |
DOB n=85 |
ISPRL n=20 |
P |
|
|
AT |
4 (6) |
2 (2) |
2 (10) |
0.11 |
|
AVNRT |
29 (43) |
65 (76) |
15 (75) |
0.89 |
|
AFL |
34 (51) |
18 (21) |
3 (15) |
0.54 |
AVNRT Atrioventricular nodal reentrant tachycardia; AT atrial tachycardia; AFL atrial flutter. DOB dobutamine; ISPRL isoproterenol; PES programmed electrical stimulation. Categorical data are reported as frequency (percentage). P values reflect the comparison between the DOB and ISPRL groups. A P value < 0.05 was considered significant.
Table 3: Outcomes
CTI AFL Cavotricuspid isthmus dependent atrial flutter; DOB dobutamine; ISPRL isoproterenol; PES programmed electrical stimulation; SVT supraventricular tachycardia. Categorical data are reported as frequency (percentage). P values reflect the comparison between the DOB and ISPRL groups. A P value < 0.05 was considered significant.
Table 4: Adverse Events
|
Dobutamine n=85 |
Isoproterenol n=20 |
P |
|
|
Severe Hypertension with Infusion |
31 (49) |
4 (20) |
0.12 |
|
Severe Hypotension with Infusion |
1 (2) |
5 (25) |
< 0.01 |
|
Sustained Ventricular Tachycardia |
3 (3.5) |
1 (5) |
0.6 |
Severe Hypertension was defined as a systolic blood pressure of > 180 mm Hg. Severe hypotension was defined as a systolic blood pressure < 90 mm Hg. Sustained Ventricular Tachycardia was in all cases polymorphic ventricular tachycardia. Categorical data are reported as frequency (percentage). P values reflect the comparison between the DOB and ISPRL groups. A P value < 0.05 was considered significant.
Table 5: Measurement EP Parameters at Incremental Doses of ISPRL and DOB
|
Baseline n=30 |
ISPRL |
ISPRL |
DOB |
DOB |
DOB |
|
|
1 ug/min |
2 ug/min |
10 mcg/kg/min n=5 |
20 mcg/kg/min |
30 mcg/kg/min |
||
|
n=5 |
n=5 |
n=7 |
N=8 |
|||
|
SCL |
811 ± 211 |
610 ± 72 |
536 ± 83 |
679 ± 206 |
574 ± 98 |
692 ± 150 |
|
(-31±22) |
(-39 ± 22) |
(-23 ± 23) |
(-35 ± 19) |
(-22 ± 18) |
||
|
AH |
90 ± 28 |
73±13 |
60 ± 6 |
67 ± 35 |
64 ± 41 |
78 ± 24 |
|
(-19±29) |
(-33 ± 29) |
(-26 ± 31) |
(-29 ± 28) |
(-13 ± 24) |
||
|
HV |
47 ± 8 |
45 ± 4 |
43 ± 7 |
48 ± 5 |
43 ± 6 |
51 ± 10 |
|
(-5 ± 15) |
(-8 ± 17) |
(3 ± 12) |
(-9 ± 15) |
(9 ± 15) |
||
|
QRS |
96 ± 19 |
100 ± 18 |
87 ± 9 |
101 ± 24 |
99 ± 23 |
88 ±9 |
|
(4 ± 19) |
(-9 ± 18) |
(5 ± 20) |
(3 ± 18) |
(-8 ± 15) |
||
|
QT |
379 ± 41 |
347 ± 22 |
319 ± 59 |
362 ± 39 |
342 ± 38 |
358 ± 54 |
|
(-8 ± 10) |
(-16 ± 11) |
(-4 ± 11) |
(-8 ± 9) |
(-6 ± 9) |
||
|
AVBCL |
379 ± 85 |
288 ± 50 |
250 ± 57 |
296 ± 36 |
314 ± 69 |
304 ± 63 |
|
(-24 ± 21) |
(-34 ± 21) |
(-22 ± 21) |
(-17 ± 18) |
(-20 ± 17) |
DOB dobutamine; ISPRL isoproterenol. Data are presented as mean ± standard deviation of electrophysiologic parameters in milliseconds.
Values in parentheses represent the percent change from baseline, with 95% confidence intervals.
Discussion
In this study, dobutamine was used to facilitate induction of SVT, both prior to and after ablation. Dobutamine improved the detection of inducibility post-procedure. The absence of inducibility with dobutamine had a negative predictive value of SVT recurrence of 93.9% at 52 days post ablation. There were no major complications during this study. The most common adverse findings associated with dobutamine infusion were severe hypertension and inducible sustained polymorphic ventricular tachycardia with PES both occurring in a small percentage of cases. Of note there were more cases of hypotension in the isoproterenol group than the dobutamine group. In this study, the dose of dobutamine and isoproterenol were increased to achieve a heart rate of at least 20% above baseline. If the patient had chronotropic incompetence, stimulation still commenced since the effect on the sinus node was not always a surrogate for the effect on AV nodal function. Induction of SVT was facilitated despite the lack of heart rate (sinus nodal) response to dobutamine. Since the study was completed, we now initiate dobutamine at 5 mcg/kg/min and increase the dose by 5 mcg/kg/min every 3 minutes. We are hopeful that by starting at a lower dose of dobutamine, that the frequency of severe hypertension during dobutamine infusion will decrease. When compared to studies on isoproterenol, dobutamine appears to have similar efficacy and safety. Dobutamine was chosen due to its pharmacological similarities to isoproterenol, particularly regarding its agonist effects on β1 and β2 receptors. If further therapeutic options are sought, the (+) isomer of dobutamine has been noted to have increased β1 effects, which is believed to be the primary mechanism of action of isoproterenol [14]. Perhaps future studies could evaluate the efficacy and safety of the (+) isomer of dobutamine. This study was limited by the small number of patients included.
Conclusions
This study supports the practice of dobutamine use as an adjunct to electrophysiologic study of patients with SVT and AFL. Given the relative price increase of isoproterenol and increasing rates of radiofrequency ablation procedures, the financial and clinical implications support the use of dobutamine as an alternative to isoproterenol both for the induction of SVT, and assessment of procedural success. In our study it was safe and effective. In this respect, we propose the use of our revised protocol in centers affected by changes in the availability of isoproterenol.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors. This study was exempted from the investigational new drug (IND) based upon a Food and Drug Administration (FDA) review.
References
- Knight The rising cost of isoproterenol. EP Lab Dig 17 (2017).
- Khot UN, Vogan ED, Militello MA. Nitroprusside and Isoproterenol Use after Major Price Increases. N Engl J Med 377 (2017): 594-595.
- D’Ambrosi J, Amin N. Hyperinflation of Isoproterenol. J Pharm Pract 31 (2018): 390-394.
- Zipes DP, DiMarco JP, Jackman WM, et ACC/AHA Task Force Report: Guidelines for Clinical Intracardiac Electrophysiological and Catheter Ablation Procedures. J Am Coll Cardiol 26 (1995): 555-573.
- D’Silva A, Wright M. Advances in imaging for atrial fibrillation Radiol Res Pract 2011 (2011): 714864.
- Overgaard C, Dzavik Inotropes and Vasopressors. Circulation 118 (2008): 1047-1056.
- Tuttle RR, Mills J. Dobutamine: development of a new catecholamine to selectively increase cardiac Circ Res 36 (1975): 185-196.
- Vanegas DI, Perez C de J, Montenegro J de J, et al. Dobutamine use for arrhythmia induction during electrical programmed heart stimulation. Rev Colomb Cardiol 12 (2006): 479-483.
- Shafquat A, Imdad A, Khalid S, et Cardiac electrophysiology studies and ablations for treatment of supraventricular arrhythmias an initial experience from Karachi. J Pakistan Med Assoc 61 (2011): 173-175.
- Stambler BS, Akosah KO, Mohanty PK, et Myocardial ischemia and induction of sustained ventricular tachyarrhythmias: evaluation using dobutamine stress echocardiography-electrophysiologic testing. J Cardiovasc Electrophysiol 15 (2004): 901-907.
- Gianni C, Sanchez JE, Mohanty S, et High-dose dobutamine for inducibility of atrial arrhythmias during atrial fibrillation ablation. JACC Clin Electrophysiol 6 (2020):1701-1710.
- Ismail H, Gabriels JK, Chang D, et Site-specific effects of dobutamine on cardiac conduction and refractoriness J Journal of Interventional Cardiac Electrophysiology (2023).
- Geleijnse ML, Krenning BJ, Nemes A, et al. Incidence, Pathophysiology, and Treatment of Complications During Dobutamine-Atropine Stress Echocardiography. Circulation 121 (2010): 1756-1767.
- Cossú SF, Rothman SA, Chmielewski IL, et al. The effects of isoproterenol on the cardiac conduction system: site- specific dose dependence. J Cardiovasc Electrophysiol 8 (1997): 847-853.
- Ruffolo RR, Messick K. Effects of Dopamine, (+/-)-Dobutamine and the (+)- and (-)- Enantiomers of Dobutamine on Cardiac Function in Pithed Rats. J Pharmacol Exp Ther 235 (1985): 558-565.