Eccentricity of Aortic Annulus and Distance of Origin of Left Main and Right Coronary Arteries from Adjacent Aortic Leaflets in Non-Stenotic Aortic Valves by TEE 3D Echocardiography
Article Information
Hakimeh Sadeghian1*, Arash Jalal Omidi1, Arash Jalali2, Parto Siavosh3
1Dr. Shariati hospital, Tehran university of medical sciences, North Kargar street, Tehran, Iran
2Department of research, Tehran heart center, Tehran university of medical sciences, Iran
3School of medicine, Tehran university of medical sciences, Iran
*Corresponding author: Hakimeh Sadeghian, Dr. Shariati hospital, Tehran university of medical sciences, North Kargar street, Tehran, Iran
Received: 12 April 2022; Accepted: 18 April 2022; Published: 22 April 2022
Citation: Hakimeh Sadeghian, Arash Jalal Omidi, Arash Jalali, Parto Siavosh. Eccentricity of Aortic Annulus and Distance of Origin of Left Main and Right Coronary Arteries from Adjacent Aortic Leaflets in Non-Stenotic Aortic Valves by TEE 3D Echocardiography. Cardiology and Cardiovascular Medicine 6 (2022): 196-205.
View / Download Pdf Share at FacebookAbstract
To measure the size of the aortic Annulus (AN) and Left Ventricular Outflow Tract (LVOT) in different views and distance between right and left coronary ostia from aortic annulus by Transesophageal (TEE)3D echocardiography in patients with normal aortic valves.
Method: 31 patients (51.5% F) underwent TEE3D.Full-volume of aortic valve was saved by TEE3D.AN was measured in 3 planes: two orthogonal lines in short-axis plane (D1 & D2), sagittal (D3) and coronal (D4) planes,diameter of LVOT 5-10 mm below AN was measured in sagittal and coronal views (D5 & D6). Area and perimeter of AN were measured and the annulus according to area and perimeter was calculated. Distance of left main and RCA from aortic leaflets and length of left coronary cusp were measured. All measurements were done in mid-systole.
Results: Aortic annulus in sagittal (D3) is smaller than coronal (D4), mean difference=1.97mm, P=0. 002.In 50% of subjects, D4 was greater than D3 more than 1.9 mm. D3 and D4 are not significantly different with D5 and D6. D perimeter is equal to mean D1&D2 and D3&D4 and D area is equal to D3. Mean distance of left main and RCA ostia from AN is 14.2±2.97 and15.25±3.60 mm respectively.Mean length of left coronary cusp is 12.75±2.1 mm.
Conclusion: Aortic annulus is oval shape in normal aortic valves and is larger in coronal than sagittal view in most subjects, D perimeter is equal to mean aortic annulus. D LVOT is non-significantly smaller than the following annulus D. Distance of LM ostium from aortic annulus is longer than RCA,length of left coronary cusp is shorter than left main-annulus distance.
Keywords
Aortic valve; Eccentricity; 3D echocardiography
Article Details
Abbreviations:
AS: Aortic stenosis; AA: Aortic Annulus; GRAO: Gradient Aorta; LVDD: Left Ventricular Dimension Diastolic; LVDS: Left Ventricular Dimension Systolic; LM: Left Main; LA: Left Atrium; MSCT: Multi-Slice Computed Tomography; LVEF: Left Ventricular Ejection Fraction; RCA: Right Coronary Artery; LVOT: Left ventricular Outflow Tract; RBG: Red, Blue, Green; AO: Aorta; IVS: Interventricular Septum; PWD: Posterior Wall Dimension; RVD: Right Ventricular Dimension; TAPSE: Tricuspid Annular Plane Systolic Excursion; TEE: Trans Esophageal echocardiography; TAVI: Trans Aortic Valve Implantation; TTE: Trans Thoracic Echocardiography
1. Introduction
It has been identified that aortic annulus is not completely round in normal and stenotic aortic valves, a few studies have described the eccentricity of aortic annulus both by CT and by 3D echocardiography [1-4]. Although many studies have predominantly found that aortic annulus is non-circular, commercially available transcatheter aortic heart valve prostheses are circular [5]. With rising ovality, the pressure difference across the prosthesis increased. Slight ovalities were well tolerated by a self-expanding prosthesis, but more significant ovality led to worsening of prosthesis function and regurgitation [5]. Traditionally, aortic annulus is measured in sagittal view before TAVI and final device size should be oversized compared to annular diameter. Most procedures are performed according to the annular diameter measurement by 2D TTE or TEE, but these methods assume annular circularity, which may result in erroneous dimensions in patients whose annuli are more ovals shaped. This limitation can be overcome using multiplanar tools of either 3D TEE or MSCT [6]. But the precise detection of aortic annulus in different echocardiographic views, diameter according to perimeter and area, distance of LM and RCA ostia from adjacent aortic annulus and length of left coronary cusp by 3D echo are mentioned in few articles [2-4, 7]. It has been already studied that aortic annulus size is not different between aortic stenosis patients and normal subjects, so precise evaluation of aortic annulus in normal subjects can lead us to better understanding of aortic valve annulus shape, ovality and different sizes in different views [2-4]. The aim of this study is to measure aortic annulus and LVOT diameter in different views, and to measure distance of LM and RCA ostia from aortic annulus and length of left coronary cusp and diameter of LVOT in sagittal and coronal views in normal aortic valves.
2. Methods
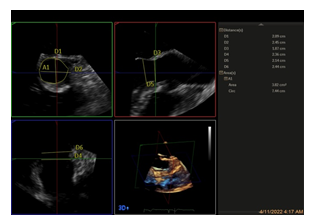
31 patients underwent TEE3D with normal aortic valves sue to other reasons like PFO, etc. Mean aortic valve gradient was<10 mmHg. Full-volume of aortic valve was saved by TEE 3D in short-axis and long-axis views in single beat. Aortic annulus was measured in four diameters. For measurement of aortic annulus, TEE 3D short-axis view by full volume was used in single beat, but if view was poor and not adequate for proper measurement, TEE long-axis 3D full-volume was used. If TEE 3D short-axis full volume view was used, RBG upright modality was selected and then mid systole was chosen, in sagittal view (right upper view, red plane),blue line was put align with aorta and green line is put just at hinge point of aortic cusps. Then in left lower view (blue plane), red line was put align with aorta and green line was put in hing point of aortic cusps, D1 and D2 were measured in left upper view (green plane, short-axis view), D3 and D5 were measured in right upper view (red plane, sagittal view) and D4 and D6 were measured in left lower view (blue plane, coronal view). Perimeter and area were measured in short-axis view (Figure 1) [1].
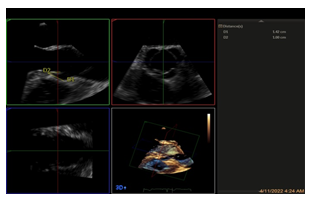
If TEE long-axis full volume 3D view was used, RBG upright modality was used and then by grabbing the blue line in sagittal view and rotating 90-degree counter clock wise, the right upper view is coronal view and left lower view is short-axis view and the measurement were done like described above [1].
The following measurements were done in above described views:
D1: Aortic annulus in TEE short-axis view between junction of left and non-coronary cusps and hinge point of right coronary cusp.
D2: Aortic annulus in TEE short-axis view between hinge point of left and commissure of right and non-coronary cups.
D3: Aortic annulus in TEE sagittal view.
D4: Aortic annulus in TEE 3D coronal view.
D5: LVOT diameter 5-10 mm below aortic annulus in TEE sagittal view (below D3).
D6: LVOT diameter 5-10 mm below aortic annulus in coronal view (below D4).
Perimeter: Circumference of aortic annulus in short-axis view (cm).
Area: Area of aortic annulus in short-axis view (cm2).
Diameter of Aortic annulus according to perimeter: Perimeter of aortic annulus/π.
Diameter of Aortic annulus according to area: 2 *Aortic annulus area /π.
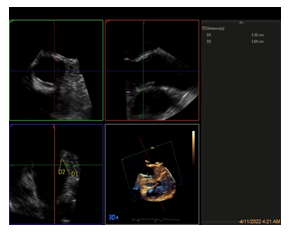
LM distance from aortic annulus: The distance between left main and aortic annulus in coronal view (Figure 2a).
RCA distance from aortic annulus: The distance between RCA and aortic annulus in TEE long-axis view (figure 2b).
Length of left coronary cusp: The length of left coronary cusp in TEE coronal view (Figure 2a).
All measurements are performed in mid- systole.
3. Statistical Analysis
The Statistical Software Package (SPSS for Windows, version 22, SPSS Inc, Chicago, Illinois, USA) was used for the statistical analyses. The continuous variables are presented as mean ± SD, and the categorical variables are expressed as percentages. The continuous variables were compared using the Student t-test or the Mann–Whitney test, if needed. The categorical variables were compared using the χ2 or the Fisher exact test. A P value of equal to or smaller than 0.05 was considered statistically significant. To assess reproducibility of data, data of 5 patients were randomly measured by the second observer for inter-observer variability control and by the first observer at an interval of two weeks for intra-observer variability. Inter- and intra-observer variability was calculated via dividing the mean difference between observations by their average measurement [8].
Inter and Intra observer variability:
Inter and intra observer variability was as follows:
D1: 0.37 and 0.46,
D2: 0.12 1nd 0.11,
D3: 0.47 and 0.21,
D4 was 0.04 and 0.08,
Distance of RCA: 0.06 and 0.06,
Distance of Left main: 0.08 and 0.08,
Length of left main: 0.06 and 0.09,
D perimeter: 0.14 and 0.12,
D area:0.19 and 0.21 respectively.
4. Results
From, 31 patients (48.5% male), mean age 50.61 ±10.78, median LVEF was 55 %, (45%, 25 percentiles and 55%, 75 percentile), mean aortic gradient was 5.43± 2.06 mmHg. Median PAPs =33.5 mmHg (30 mmHg 25 percentile and 43 mmHg 75 percentile), (Table 1).
|
Demographics |
Mean |
Standard Deviation |
|
Mean age |
50.61 |
10.78 |
|
LA |
37.45 |
8.76 |
|
AO |
28.77 |
3.75 |
|
LVDD |
46 |
6.55 |
|
LVDs |
30.06 |
6.23 |
|
IVSd |
11.06 |
2.43 |
|
PWd |
10.84 |
2.06 |
|
RVD |
30.55 |
6.03 |
|
TAPSE |
19.29 |
4.35 |
|
GRAO |
5.43 |
2.06 |
Table 1: Demographic and Echocardiographic Characteristics of the Study Subjects.
D1 is smaller than D3, 22.44 ±2.62 vs 23.06±2.91 mm, mean difference is 0.61mm, P=0.02.
The difference between D2 and D4 is not statistically significant, 24.92±3.15 vs25.03±3.69 mm, P=0.828.
D3 is smaller than D4, 23.06±2.91vs 25.03±3.69 mm, mean difference=1.97 mm,P=0.002.
Empiric distribution of difference between D4 and D3 in each subject is demonstrated by figure 2, median difference is 1.9 mm, maximum difference is 9.3 mm and minimum difference is -3.5 mm (It means that D3 is larger than D4). In 71.9 % of subjects, D4 is larger than D3 and 28.1% D4 is smaller than D3.
Figure 2: Empiric distribution of difference D4 and D3 in each subject by a plot, median difference is 1.9 mm, maximum difference is 9.3 mm and minimum difference is -3.5 mm.
In 50% of subjects, D4 was greater than D3 more than 1.9 mm, of which, in 50% this difference was between 1.9-3.8 mm and in 50% this difference was between 3.8 to 9.3 mm. In 50% of subjects, the difference between D3 and D4 was less than 1.9mm of them, in 50%, the difference was between 1.9 to -0.95 and in 50%, this difference was between -0.95 to- 3.5 mm (D3 is greater than D4). In one quarter of patients, D4 is greater than D3 between 1.9 to 3.83 mm. In one quarter of patients, D4 is greater than D3 between 3.83 to 9.3 mm, in one quarter of patients, the difference between D3 and D4 is between 1.9 to -0.95 mm. In one quarter of patients, D4 is smaller than D3 between 0.95 to 3.5 mm. The difference between D3 and D5 is not statistically significant, 23.06±2.91 vs 22.39±3.12mm, mean difference is 0.66 mm,P=0.07. The difference between D4 and D6 is not statistically significant, 25.03±3.69vs24.25±5.70, mean difference is 0.88 mm, P=0.70. The difference between D area and D3 is not statistically significant,23.39±2.58 vs 23.06 ±2.87, P=0.61. D area is smaller than D coronal,mean difference is 1.7 mm, P=0.001.
D perimeter is larger than D area, 24.00±2.69 vs 23.39±2.58 mean difference=0.70 mm,P=0.005.
D perimeter is smaller than D4 (D coronal), 24.00±2.69 vs 25.03±3.69mm, mean difference is 1.03 mm, P=0.037.
D perimeter is larger than D3 (sagittal), 24.00±2.69 vs 23.06 ±2.91, mean difference is 0.93 mm, P=0.019.
Mean D1 and D2 is not different with mean D3 and D4, P=0.39.
Annulus according to area is not different with mean D1&D2, P=0.18, but is significantly smaller than mean D3 &D4, P=0.049.
Annulus according to perimeter is not different with mean D1&D2 and mean D3&D4, P= 0.35 and P=0.88 respectively.
Mean distance between left main ostium and aortic annulus is 14.2±2.94 mm.
Mean distance between right coronary ostium and aortic annulus=15.25±3.60mm.
Mean length of left coronary cusp= 12.75±2.12 mm.
Distance of LM from aortic annulus is longer than distance between RCA and aortic annulus, mean difference=1.05, P=0.052.
Length of left coronary cusp is shorter than distance of left main from aortic annulus, mean difference =1.05, P=0.001 (Table 2).
|
Mean |
Standard Deviation |
|
|
LM distance |
14.2 |
2.94 |
|
RCA distance |
15.26 |
3.61 |
|
Area of Aortic annulus |
4.31 |
0.95 |
|
Perimeter of Aortic annulus |
7.54 |
0.85 |
|
Left coronary cusp length |
12.75 |
2.12 |
|
D1 |
22.44 |
2.62 |
|
D2 |
24.92 |
3.15 |
|
D3 |
23.06 |
2.87 |
|
D4 |
25.03 |
3.69 |
|
D5 |
22.39 |
3.12 |
|
D6 |
24.25 |
5.7 |
Table 2: Echocardiographic Measurements of Aortic Valve of the Study Subjects
5. Discussion
The results of our study showed that the coronal diameter of aortic annulus is about 2mm larger than sagittal diameter in normal aortic valve. Although the median difference between coronal and sagittal aortic annulus is 1.9 mm, in 50% of subjects, D4 is greater than D3 more than 1.9 mm, in 25% this difference was between 1.9-3.8 mm and in 25% this difference was between 3.8 to 9.3 mm. In 50% of subjects, the difference between D3 and D4 was less than 1.9mm, in 25%, the difference was between 1.9 to -0.95 and in 25%, this difference was between -0.95 to- 3.5 mm (coronal diameter is smaller than sagittal diameter of aortic annulus). The aortic annulus diameter according to area is similar to the aortic diameter in sagittal view and aortic diameter according to perimeter is equal to mean aortic annulus. D1 is the smallest aortic diameter according to our study as reported before [9]. Mean RCA distance from aortic annulus is 1mm greater than mean left main distance from aortic annulus and mean left coronary cusp is about 1.2 mm smaller than distance of left main from aortic annulus.
The results of our study showed that D1 is significantly smaller than D3, so the annulus in short-axis (smaller diameter) is smaller than the aortic annulus in sagittal view and they are not the same measurement and cannot be replaced by each other. Also, the difference between D2 and D4 is not statistically significant, so the aortic annulus in coronal view and short-axis view (greater diameter) are the same. The aortic annulus in sagittal view is about 2 mm smaller than the aortic annulus in coronal view. So the aortic annulus in normal valves is not round in systole and is oval shape. Although the difference between D3 and D5 is not statistically significant, but mean difference is 0.66 mm and P=0.07, it is probable that with a larger study population and especially in patients with significant aortic stenosis with left ventricular hypertrophy, this difference would be significant [10]. In the study by Otani et al, the minimum diameter of LVOT was not different between AS and normal but maximum diameter of LVOT was significantly smaller in AS group compared to normal [3]. D perimeter in our study is larger than D area which is comparable with study by Blank P et al [11], but in the study by Khalique at al,D perimeter and area was not different by TEE3D but D area is smaller than D perimeter by CT scan[1].According to our results, D perimeter is equal to mean D coronal and D sagittal. In our study, aortic annulus was 23.06±2.87 mm in sagittal view and 25.03±3.69 mm in coronal view by TEE 3D echocardiogeaphy. Our result is comparable with the results of the study by Omar Khalique et al which showed that max aortic annular diameter by TEE 3D echo was 25.3±2.6 mm and minimal aortic diameter was 21.9±2.2 mm, D according to area was 23.4±2.2 mm and D according to perimeter was 23.8±2.2mm, D perimeter was 24.1±2.2mm by CT scan and D area was 23.7±2.1 by CT scan [1].
The results of our study showed that D1 is significantly smaller than D3, so the annulus in short-axis (smaller diameter) is smaller than the aortic annulus in sagittal view and they are not the same measurement and cannot be replaced by each other. Also, the difference between D2 and D4 is not statistically significant, so the aortic annulus in coronal view and short-axis view (greater diameter) are the same. The aortic annulus in sagittal view is about 2 mm smaller than the aortic annulus in coronal view. So the aortic annulus in normal valves is not round in systole and is oval shape. Although the difference between D3 and D5 is not statistically significant, but mean difference is 0.66 mm and P=0.07, it is probable that with a larger study population and especially in patients with significant aortic stenosis with left ventricular hypertrophy, this difference would be significant [10]. In the study by Otani et al, the minimum diameter of LVOT was not different between AS and normal but maximum diameter of LVOT was significantly smaller in AS group compared to normal [3]. D perimeter in our study is larger than D area which is comparable with study by Blank P et al [11], but in the study by Khalique at al,D perimeter and area was not different by TEE3D but D area is smaller than D perimeter by CT scan[1].According to our results, D perimeter is equal to mean D coronal and D sagittal. In our study, aortic annulus was 23.06±2.87 mm in sagittal view and 25.03±3.69 mm in coronal view by TEE 3D echocardiogeaphy. Our result is comparable with the results of the study by Omar Khalique et al which showed that max aortic annular diameter by TEE 3D echo was 25.3±2.6 mm and minimal aortic diameter was 21.9±2.2 mm, D according to area was 23.4±2.2 mm and D according to perimeter was 23.8±2.2mm, D perimeter was 24.1±2.2mm by CT scan and D area was 23.7±2.1 by CT scan [1].
6. Future Studies
1)According to the results of this study, the difference between sagittal and coronal diameter of aortic annulus is between 3.8 to 9.3 mm in 25 percentile of normal aortic valves, so ovality of aortic annulus even in normal aortic valve is remarkable and ovality of aortic valve in AS patients may be a real cause of paravalvular leakage after TAVI, future studies need to describe the relationship between ovality of aortic valve and paravalvular leakage post TAVI.
2)Smaller diameter of LVOT diameter compared to aortic annulus as a probable cause of LBBB and some other complication post TAVI should be evaluated.
3) The design of self-expandable aortic valve prosthesis which LVOT end is smaller than mid-portion may be a cause of LBBB in the patients with smaller LVOT diameter compared to annulus and may be a guide for designing the self-expandable devices which mid-portion and LVOT end have the same diameter.
Declaration
None of the authors have any conflicts of interest to declare and this study has been ethically approved by Tehran Heart Center. This study is not funded by any organization.
References
- Khalique OK, Kodali SK, Paradis JM, et al. Aortic annular sizing using a novel 3-dimensional echocardiographic method: use and comparison with cardiac computed tomography. Circ Cardiovasc Imaging 7 (2014): 155-163.
- Calleja A, Thavendiranathan P, Ionasec IR, et al. Automated Quantitative 3-Dimensional Modeling of the Aortic Valve and Root by 3-Dimensional Transesophageal Echocardiography in Normals, Aortic Regurgitation, and Aortic Stenosis: Comparison to Computed Tomography in Normals and Clinical Implications. Circulation: Cardiovascular Imaging 6 (2013): 99-108.
- Otani K, TakeuchiM, Kaku K, et al. Assessment of the Aortic Root Using Real-Time 3D Transesophageal Echocardiography. Circulation journal?: official journal of the Japanese Circulation Society 74 (2010): 2649-2657.
- Akhtar M, Tuzcu M, Kaoadia SR, et al. Aortic root morphology in patients undergoing percutaneous aortic valve replacement: evidence of aortic root remodeling. The Journal of Thoracic and Cardiovascular Surgery 137 (2009): 950-956 .
- Kuetting M, Sedaghat A, Utzenrath M, et al. In vitro assessment of the influence of aortic annulus ovality on the hydrodynamic performance of self-expanding transcatheter heart valve prostheses. Journal of biomechanics 47 (2014): 957-965.
- Zamorano JL, Badano LP, Bruce C, et al. EAE/ASE recommendations for the use of echocardiography in new transcatheter interventions for valvular heart disease. J Am Soc Echocardiogr 24 (2011): 937-965.
- Piazza N, de Jaegere P, Schultz C, et al. Anatomy of the aortic valvar complex and its implications for transcatheter implantation of the aortic valve. Circ Cardiovasc Interv 1 (2008): 74-81.
- Sadeghian H, Ahmadi F, Lotfi-Tokaldany, M,et al, Ventricular asynchrony of time-to-peak systolic velocity in structurally normal heart by tissue Doppler imaging. Echocardiography 27 (2010): 823-830.
- Blanke P, Weir-McCall JR, Achenbach S, et al. Computed Tomography Imaging in the Context of Transcatheter Aortic Valve Implantation (TAVI)/Transcatheter Aortic Valve Replacement (TAVR): An Expert Consensus Document of the Society of Cardiovascular Computed Tomography. JACC Cardiovasc Imaging 12 (2019): 1-24.
- Janosi RA, Plicht B, Kahlert P, et al, Quantitative Analysis of Aortic Valve Stenosis and Aortic Root Dimensions by Three-Dimensional Echocardiography in Patients Scheduled for Transcutaneous Aortic Valve Implantation. Curr Cardiovasc Imaging Rep 7 (2014): 9296-9299.
- Blanke P, Willson AB, Webb JG, et al, Oversizing in transcatheter aortic valve replacement, a commonly used term but a poorly understood one: dependency on definition and geometrical measurements. J Cardiovasc Comput Tomogr 8 (2014): 67-76.
- Zamorano JL, Goncalves A, Lang R. Imaging to select and guide transcatheter aortic valve implantation. Eur Heart J 35 (2014): 1578-1587.
- Cavalcanti JS, de Melo NC, de Vasconcelos RS. orphometric and topographic study of coronary ostia. Arq Bras Cardiol 81 (2003): 359-362.
- Tops LF, Wood DA, Delgado V, et al, Noninvasive evaluation of the aortic root with multislice computed tomography implications for transcatheter aortic valve replacement. JACC Cardiovasc Imaging 1 (2008): 321-330.
- Sadeghian H, Ashrafi MM. Transcatheter Aortic Valve Implantation - Tavi. Curr Trends Clin Med Imaging 3 (2019): 59-61.