Early Insertion of Intra-Aortic Balloon Pump after Cardiac Arrest on Acute Coronary Syndrome Patients: A Randomized Clinical Trial
Article Information
Isman Firdaus1*, Yoga Yuniadi1, Hananto Andriantoro1, Cindy Elfira Boom1, Kuntjoro Harimurti2, Rochmad Romdoni3, Dede Kusmana1
1Department of Cardiology and Vascular Medicine University of Indonesia- National Cardiovascular Centre Harapan Kita Hospital, Jakarta, Indonesia
2Department of Internal Medicine, Faculty of Medicine, University of Indonesia- Cipto Mangunkusumo Hospital, Jakarta, Indonesia
3Departement of Cardiology and Vascular Medicine Airlangga University, Surabaya, Indonesia
*Corresponding author: Isman Firdaus, Department of Cardiology and Vascular Medicine University of Indonesia- National Cardiovascular Centre Harapan Kita Hospital, Jakarta, Indonesia
Received: 11 July 2019; Accepted: 19 July 2019; Published: 23 July 2019
Citation: Isman Firdaus, Yoga Yuniadi, Hananto Andriantoro, Cindy Elfira Boom, Kuntjoro Harimurti, Rochmad Romdoni, Dede Kusmana. Early Insertion of Intra-Aortic Balloon Pump after Cardiac Arrest on Acute Coronary Syndrome Patients: A Randomized Clinical Trial. Cardiology and Cardiovascular Medicine 3 (2019): 193-203.
View / Download Pdf Share at FacebookAbstract
Background: The need for mechanical circulatory support to improve organ perfusion may be considered in the management of post cardiac arrest syndrome patients. Intra-Aortic Balloon Pump (IABP) is the most available and convenient used mechanical circulation aid especially in developing countries such as Indonesia.
Objectives: This study aimed to find out whether early insertion of IABP can reduce in-hospital mortality, length of stay, cell death markers, and improving lactate clearance of cardiac arrest patients due to acute coronary syndrome (ACS).
Methods: A randomized trial conducted in National Cardiovascular Center Harapan Kita (NCCHK) Hospital from October 2017–December 2018. Inclusion criteria were all post cardiac arrest due to ACS patients aged 18–75 years. Exclusion criteria were history of stroke, anisocoric pupil, previous IABP use, aortic regurgitation, Brugada syndrome, and congenital long QT syndrome. Primary outcome was in-hospital mortality analyzed with cox regression analysis with intention-to-treat principle.
Results: A total of 60 post cardiac arrest due to ACS patients, 30 in intervention group and 30 controls included in this study. In hospital mortality of intervention group vs control was 18 (60%) vs. 17 (56.67%) respectively ([p = 0.793; hazard ratio 1.29; [CI] 95% 0.66–2.52). There was no differences in length of stay, cell death marker or lactate clearance in both group.
Conclusion: Early insertion of IABP did not reduce in hospital mortality, length of stay, cell death marker or improve lactate clearance in post cardiac arrest patient due to ACS.
Keywords
Cardiac arrest; IABP
Cardiac arrest articles, IABP articles
Article Details
Introduction
Cardiac arrest is the most devastating shock condition, characterized by whole body ischemia which results in cessation of oxygen circulation, reperfusion, and metabolic substrate, leading to accumulation of metabolic waste [1, 2]. Cardiac arrest incidence is still high. Non-traumatic out of hospital cardiac arrest incidence in United States range around 350,000 or 80 per 100,000 adults, with a survival rate of 9.5% after hospitalization [3, 4]. In Europe, out of hospital cardiac arrest incidence was 37-55 per 100.000 population per year [5]. Acute coronary syndrome (ACS) is the most common cause of cardiac arrest. Cardiac arrest requires immediate resuscitation to return spontaneous circulation.
Despite spontaneous circulation returns, the morbidity and mortality in post cardiac arrest patients is still high [6]. Approximately 60% of patients admitted to hospital after cardiac arrest die of complications. Deaths that occur within 24 hours after return of spontaneous circulation (ROSC) are usually caused by refractory shock that causes recurrent cardiac arrest or multi organ failure [7]. Post cardiac arrest syndrome is a complex and unique pathophysiological process, consisting of post cardiac arrest brain injury, myocardial dysfunction, systemic response to ischemia/ reperfusion, and pathological processes that cause cardiac arrest [1, 4]. The severity of the process varies widely, depends on the comorbid before the onset of cardiac arrest, the cause and duration of cardiac arrest.
Management of post cardiac arrest patients still challenging and requires a structured approach for hemodynamic stabilization, neuroprotective strategy, identifying and treating the etiology of arrest to prevent recurrence. The need of mechanical circulatory support to improve organ perfusion during post cardiac arrest syndrome may be considered. Intra-Aortic Balloon Pump (IABP) is the most available and convenient used mechanical circulation aid especially in developing countries such as Indonesia [8]. In several studies on cardiac arrest, IABP have been used with insertion rates of 22% to 46% of phoatients [4]. Nevertheless, the use of IABP is still in debate. Previous multicenter study IABP Shock-II trial found that IABP support does not reduce in hospital mortality in patients with cardiogenic shock complicating myocardial infarction undergone early revascularization [9]. Therefore, in this study we aimed to find out whether early insertion of IABP can reduce in-hospital mortality, length of stay, cell death markers and improve lactate clearance of post cardiac arrest patients due to acute coronary syndrome.
Materials and Methods
Patients Population
This study is a single centered randomized trial conducted in National Cardiovascular Center Harapan Kita (NCCHK) Hospital, Jakarta, Indonesia from October 2017 until December 2018. Study population were post cardiac arrest patients due to acute coronary syndrome aged at least 18 to 75 years. Post cardiac arrest patients defined as patients with returned of spontaneous circulation after cardiopulmonary resuscitation marked by palpable pulse and detectable blood pressure. Cardiac arrest event defined as sudden cessation of heart contraction and spontaneous circulation marked by impalpable pulse, loss of consciousness, absence of breathing or gasping and abnormal cardiac rhythm on ECG monitor (ventricular tachycardia ventricular fibrillation, pulseless electrical activity (PEA), or asystole) happened inside NCCHK hospital.
Exclusion criteria were (1) previous history of stroke, (2) anisocoric pupil, (3) previous used of IABP during hospitalization, (4) aortic regurgitation, (5) Brugada or congenital long QT syndrome. This study was approved by ethics committees of NCCHK Hospital number LB.02.01/VII/190/KEP.042/2017. Patients or their legally authorized representatives provided written informed consent using a previously validated and dedicated informed consent process.
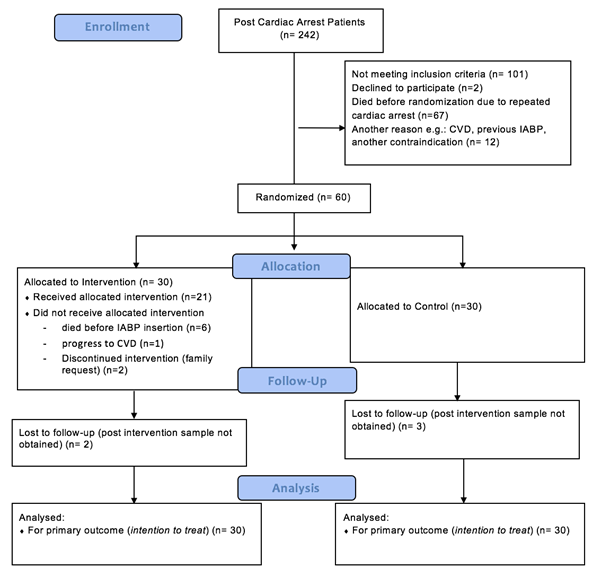
The patient selection algorithm is illustrated in Figure 1.
Between October 2017 until December 2018, there’s 242 cardiac arrest patient with successful resuscitation. A total of 60 patients meeting the inclusion and exclusion criteria comprised the final study population. Patients were randomized into two group (intervention group with early IABP insertion n=30, control group n= 30). The randomization protocol done via an internet-based program and stratification according to center with blocks of six patients from http://www.randomization.com. In intervention arm, there’s only 21 patients receiving intervention because 6 were died before IABP insertion, 1 progressed into cerebrovascular disease, and 2 discontinue treatment by family request. After randomization, vital sign, lactate serum, Interleukin-6, and Caspase-3 were measured in 30 minute after enrollment. Insertion of IABP was done within 180 minutes in designated group. Six hour after ROSC, lactate serum, Interleukin-6, and Caspase-3 were measured as well.
Study definition
The primary end-point of this study was in hospital mortality. Early insertion defined by insertion of IABP within 180 minutes (3 hours) after ROSC. Secondary outcome was length of stay, cell death marker (caspase-3), lactate clearance, and Interleukin-6 level 6 hour after ROSC.
Statistical analysis
All data analysis performed with SPSS 24th edition for Mac. Continuous variables are reported as means ± standard deviation if normally distributed and as median (interquartile range) if abnormal. Categorical values are expressed as absolute values and percentages. Continuous variables from independent samples were compared by student’s t-test or Mann Whitney u test depending on normality. Categorical variables were compared with χ2 test or Fisher exact test as appropriate. Survival analysis done with cox regression proportional hazard model adjusted for important risk co-variables. Statistical significance was defined as p < 0.05.
Results
A total of 20.787 in-hospital patients during study period, 742 patients had cardiac arrest. About 242 (32.61%) cardiac arrest patient successfully resuscitated. Of these, 30 patients received IABP and 30 patients did not. Baseline and procedural characteristics of the two groups are presented in Table 1.
|
Characteristics |
IABP (n=30) |
Control (n=30) |
|
Sex |
||
|
Male |
26 (86.67%) |
23 (76.67%) |
|
Female |
4 (13.33%) |
7 (23.3%) |
|
Age (years) |
58.68±9.38 |
60.93±9.56 |
|
Body weight (kg) |
67.11±15.48 |
63.9±12.37 |
|
Body height (cm) |
164.36±5.8 |
162.87±6.57 |
|
BMI (kg/m2) |
24.81±5.32 |
23.95±3.48 |
|
Risk Factor |
||
|
Hypertension |
21 (70%) |
12 (40%) |
|
Diabetes Mellitus |
19 (63.33%) |
15 (50%) |
|
Dyslipidemia |
13 (43.33%) |
6 (20%) |
|
Smoking |
16 (53.33%) |
17 (56.67 %) |
|
Family History |
4 (13.33%) |
5 (16.67%) |
|
Prior Myocardial Infarction Prior PCI Prior CABG Prior valvular heart disease |
14 (46.67%) 8 (26.67%) 4 (13.33%) 3 (10%) |
13 (43.3%) 6 (20%) 1 (3.3%) 1 (3.3%) |
|
CPR duration (minute) |
10 (0.5-60) |
10 (2-50) |
|
Defibrillation (times) |
1(0-4) |
1(0-6) |
|
Intubation |
20 (66.67%) |
19 (63.33%) |
|
Cerebral Performance Category (CPC) 1 2 3 4 5 |
0 8 (26.67%) 5 (16.67%) 17 (56.67%) 0 |
0 7(23.33%) 10 (33.33%) 13 (43.33%) 0 |
|
Systolic BP post ROSC (mmHg) |
102.57±31.32 |
100.53±23.86 |
|
Diastolic BP post ROSC (mmHg) |
62.14±19.26 |
64.77±17.1 |
|
Heart Rate post ROSC (bpm) |
99.57±20.96 |
92.17±21.6 |
|
SGOT |
127(8-7913) |
47(10-3360) |
|
SGPT |
72(5-4491) |
41(10-1734) |
|
Ureum |
74.2(19.2-279) |
77.6(23.2-623) |
|
Creatinin |
1.95(0.8-9.19) |
2.03(0.76-5.08) |
|
Hs TropT |
2066(29-35859) |
1145(76-14394) |
|
NT Pro BNP |
8849(188-97138) |
21634(56-10525) |
|
Caspase-3 30 min after ROSC (pg/mL) |
0.2(0-3.25) |
0.18(0- 1.01) |
|
Lactate serum 30 min after ROSC (mmol/L) |
5.65(1.5-13) |
4.05(1.1-20) |
|
Interleukin-6 30 min after ROSC (pg/mL) |
61.7(7.2-39933) |
112.9(19-17028) |
IABP = Intra-Aortic Balloon Pump; BMI = Body Mass Index; SGOT= Serum glutamic oxaloacetic transaminase; SGPT = serum glutamate-pyruvate transaminase; CPC = Cerebral Performance Category; CABG = Coronary Artery Bypass Graft; HsTropT = high sensitivity Troponin-T; NT-Pro BNP = N-Terminal Pro B-type Natriuretic Peptide; ROSC = Return of spontaneous circulation
Table 1: Baseline Characteristics
The IABP group was predominantly male and had a higher prevalence hypertension, DM, dyslipidemia, prior CABG and valvular heart disease history, worse CPC, higher SGOT, HsTropT, and lower NT Pro BNP level. Of all 60 subjects recruited, overall in-hospital mortality rate was 58,3%. Primary and secondary outcomes are presented in Table 2. In hospital mortality of intervention group vs control was 18 (60%) vs 17 (56,67%) respectively. Chi square analysis showed no difference in mortality between two group [p 0.793; RR= 1.059 (0.690- 1.625)].
|
IABP (n =30) |
Control (n=30) |
P-value |
|
|
Primary Outcome |
|||
|
Mortality |
18 (60%) |
17 (56.67%) |
0.793* [RR= 1.059 (0.690- 1.625)] |
|
Secondary Outcome |
|||
|
Length of Stay (days) |
14 (2-45) |
14 (5-29) |
0.728** |
|
Caspase-3 6 hour after ROSC (pg/mL) |
0.15 (0.11-0.61) |
0.17(0.1-0.78) |
0.458** |
|
Lactate serum 6 hour after ROSC (mmol/L) |
2.7 (0.9-20) |
2.8 (1.5-18.9) |
0.423** |
|
Interleukin-6 6 hour after ROSC (pg/mL) |
36.1(19.3-96046) |
65.55(10.7-16393) |
0.114** |
*chi-square test; **Mann-Whitney U test; ROSC = Return of Spontaneous Circulation
Table 2: Primary and Secondary Outcome of Both Group
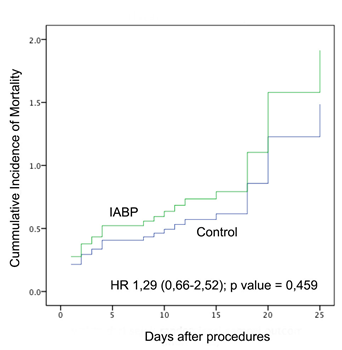
The effectiveness of early IABP in this study was determined by calculating the survival rate during hospitalization and calculating the hazard ratio. The survival rate for IABP group vs control was 11.5% (standard error [SE] 10.3 %) vs 27.5% ([SE] 10.6%) respectively, with log rank test p-value 0.428. Cox’s regression analysis showed increase trend of Hazard Ratio in IABP group (HR 1.29; [CI] 95% 0.66-2.52; p value = 0.459) (See Figure 2). Therefore, early insertion of IABP did not reduce in-hospital mortality of post cardiac arrest patients due to ACS.
Discussion
In this prospective randomized controlled trial of post cardiac arrest patients due to acute coronary syndrome, IABP support did not reduce in hospital mortality compared with control.
Post-cardiac arrest syndrome begins after the return of spontaneous circulation. Studies show that the cardiac arrest mortality rate is still high. This is caused by prolonged systemic ischemia causes brain and heart dysfunction. In this study, the resuscitation’s success rate was 32.61%, but the hospital survival rate for patients was 19.1% ([SE] 8.10%). The UK National Health Service (NHS) study shows the success rate of resuscitation is 13–27% and the degree of hospital survival 2–12% [10]. Resuscitation Council National Cardiac Arrest Audit (NCAA) reports a 45% success rate of resuscitation and hospital survival rate 18.4% [11]. Success resuscitation rate and hospital survival rate are not much different from previous studies.
Intra-Aortic Balloon Pump is used in subjects with especially high risk of death in real-world practice. Similar findings regarding the unavailing effects of IABP use on certain population mortality have been reported in several previous studies. IABP use in populations of cardiogenic shock complicating AMI was reported to have no benefit in SHOCK II study by Thiele et al compared with controls, with 30-day mortality rate 43% vs 45% respectively [9]. IABP use in the population after cardiac arrest is also reported by the KAMIR study to be of no benefit. In 2015, Kim et.al investigate IABP use in patients with cardiogenic shock complicating AMI after cardiac arrest. This study was conducted in 1359 AMI patients with complications from cardiogenic shock after cardiac arrest. This study obtained that compared to control, the IABP group had worse outcomes in terms of mortality rates after multivariate analysis [hazard ratio (HR) 1.22, 95% confidence interval (CI) 1.02–1.47, p = 0.034] without increasing the incidence of recurrent MI, stroke, and major bleeding [12]. Burkoff et al. In 2006 reported in patients with cardiogenic shock, IABP improved hemodynamics but had the same mortality as controls. Studies comparing IABP use with Impella, the 2008 ISAR-SHOCK trial and IMPRESS in Severe Shock Trial in 2017, show IABP and Impella have no different 30-day mortality rates, even though Impella improves the cardiac index [13, 14].
Cerebral performance category remains significant risk factor for mortality after adjustment for other variable in this study. Previous studies by Sinkovic et al. in 2018 stated that post cardiac arrest brain injury assessed by CPC was an independent predictor of mortality out-of-hospital cardiac arrest (OHCA) with adjusted OR 50.47 (6.74 -377.68); p value <0.001 [15]. In our study, cerebral performance category remains significant risk factor for mortality with hazard ratio = 2.178, CI (1.089-4.357); p <0.05. We hypothesized that poor cerebral performance category in IABP group explained why intervention did not improve mortality in this population. Post resuscitation period is dominated by the process of global ischemia and complex reperfusion injury resulting in oxygen depletion, membrane dysfunction, and re-oxygenation reactions, resulting in the toxicity of free radicals. The pathophysiology background results in particular severe cardio-circulatory shock, post cardiac arrest brain injury, multi-organ failure, and inflammation. Post cardiac arrest brain injury is a complication of a syndrome after long-term resuscitation that depends on the time of ischemia and reperfusion [15].
The process of dying is goes through very complex mechanisms. During the ischemic phase, when cardiac arrest occurs and there is no spontaneous circulation, the production of adenosine triphosphate (ATP) decreases. Decreased ATP production causes membrane plasma depolarization, opening of calcium channels and disruption of potential mitochondrial membranes. This causes an increase in the concentration of calcium in the cytoplasm resulting in cell death. Cellular hypoxia also triggered stress in reticulum endoplasm, which subsequently activate executor Caspases to initiate apoptosis cascade [16]. Previous study by Prescimone et al. show his study of end-stage heart failure patients who performed LVAD installation showed that LVAD as a mechanical aid increased cardiac output and improved organ perfusion, thereby reducing apoptosis marked by reduce in Caspase-3 level [17]. In our study IABP did not improve apoptosis in post cardiac arrest as there’s no significant difference in 6 hour Caspase-3 level.
In the reperfusion phase, when blood flow starts from chest compression or spontaneously, free radicals are formed. Free radicals cause cell death and endothelial damage. Damaged endothelium triggers systemic inflammation characterized by an increase in one of the levels of inflammatory cytokines interleukin-6 (IL-6). These factors cause pathological vasodilation, decreased heart function, to multi-organ failure. Neutrophils that are activated in the lungs and other organs become triggers for multi-organ failure [1, 18].
Increase in lactate serum also occurs in the early phase of cardiac arrest. Several studies reported that a decrease in lactate levels is one of the prognostic values of successful management of shock and cardiac arrest. Donnino et al. reported that effective lactate clearance is associated with decreased early and overall in-hospital mortality in post-cardiac arrest patients, they show rapid restoration of tissue perfusion [19]. Lee et.al also stated also reported that in patients treated with hypothermia, lactate clearance of 6 hours and 12 hours had a significant association with better neurological status [20].
Several limitations in this study are first, the study population are limited in survival. Second, there’s few subjects dropped out from the study because of several reasons, such as repeated cardiac arrest, family request, and progression to stroke.
Conclusions
Management of post cardiac arrest syndrome is still challenging with high mortality rate. Early insertion of IABP did not show any clinical benefit in post cardiac arrest patients due to acute coronary syndrome. Further studies are needed to observed the effect of IABP in cardiac arrest in different population.
Conflict of Interest
The authors declare that there is no conflict of interest.
Acknowledgments
This study was performed with the support of Department of Cardiology and Vascular Medicine University of Indonesia- National Cardiovascular Centre Harapan Kita Hospital, Jakarta, Indonesia.
References
- Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Bottiger BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation 118 (2008): 2452-2483.
- Adams JA, Uryash A, Nadkarni V, Berg RA, Lopez JR. Whole body periodic acceleration (pGz) preserves heart rate variability after cardiac arrest. Resuscitation 99 (2016): 20-25.
- Koenig MA. Brain resuscitation and prognosis after cardiac arrest. Critical care clinics 30 (2014): 765-783.
- Stub D, Bernard S, Duffy SJ, Kaye DM. Post cardiac arrest syndrome: a review of therapeutic strategies. Circulation 123 (2011): 1428-1435.
- Schewe JC, Kappler J, Heister U, Weber SU, Diepenseifen CJ, Frings B, et al. Outcome of out-of-hospital cardiac arrest over a period of 15 years in comparison to the RACA score in a physician staffed urban emergency medical service in Germany. Resuscitation 96 (2015): 232-238.
- Pellis T, Sanfilippo F, Ristagno G. The optimal hemodynamics management of post-cardiac arrest shock. Best practice & research Clinical anaesthesiology 29 (2015): 485-495.
- Jentzer JC, Chonde MD, Dezfulian C. Myocardial Dysfunction and Shock after Cardiac Arrest. BioMed research international 2015 (2015): 314796.
- Parissis H, Soo A, Al-Alao B. Intra aortic balloon pump: literature review of risk factors related to complications of the intraaortic balloon pump. Journal of Cardiothoracic Surgery 6 (2011): 147.
- Thiele H, Zeymer U, Neumann FJ, Ferenc M, Olbrich HG, Hausleiter J, et al. Intraaortic balloon support for myocardial infarction with cardiogenic shock. The New England journal of medicine 367 (2012): 1287-1296.
- Perkins G, Brace-McDonnell S. The UK Out of Hospital Cardiac Arrest Outcome (OHCAO) Project. BMJ Open 2015 (2015): 1-12.
- Nolan JP, Soar J, Smith GB, Gwinnutt C, Parrott F, Power S, et al. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation 85 (2014): 987-992.
- Kim YW, Cha KC, Cha YS, Kim OH, Jung WJ, Kim TH, et al. Shock duration after resuscitation is associated with occurrence of post-cardiac arrest acute kidney injury. Journal of Korean medical science 30 (2015): 802-807.
- Thiele H, Zeymer U, Neumann F-J, Ferenc M, Olbrich H-G, Hausleiter J, et al. Intra-aortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock (IABP-SHOCK II): final 12 month results of a randomised, open-label trial. The Lancet 382 (2013): 1638-1645.
- Poulidakis E, Spaulding C. Cardiac Assist Devices in Cardiogenic Shock : What You See Is What You Get? Circulation 139 (2019): 1259-1261.
- Sinkovic A, Markota A, Marins?ek M, Svens?ek F. Independent Predictors of 6-Month Mortality in Patients Successfully Resuscitated for Out-of-Hospital Cardiac Arrest: Observational Retrospective Single Center Study. BioMed research international 2018: 2018.
- Kumar A, Cannon CP. Acute Coronary Syndromes: Diagnosis and Management, Part I. Mayo Clinic proceedings 84 (2009): 917-938.
- Prescimone T, Masotti S, D'Amico A, Caruso R, Cabiati M, Caselli C, et al. Cardiac molecular markers of programmed cell death are activated in end-stage heart failure patients supported by left ventricular assist device. Cardiovascular pathology : the official journal of the Society for Cardiovascular Pathology 23 (2014): 272-282.
- Mongardon N, Dumas F, Ricome S, Grimaldi D, Hissem T, Pene F, et al. Postcardiac arrest syndrome: from immediate resuscitation to long-term outcome. Annals of intensive care 1 (2011): 45.
- Donnino MW, Miller J, Goyal N, Loomba M, Sankey SS, Dolcourt B, et al. Effective lactate clearance is associated with improved outcome in post-cardiac arrest patients. Resuscitation 75 (2007): 229-234.
- Lee T, Kang M, Cha W, Shin T, Sim M, Jo I, et al. Better Lactate Clearance Associated with Good Neurologic Outcome in Survivors Who Treated With Therapeutic Hypothermia After Out-of Hospital Cardiac Arrest. Critical Care 17 (2013): 1-8.