Dyslipidemia in Pregnancy and the Proper Reference Values: A Retrospective Study in South China
Article Information
Shufan Yue1, Ling Pei1, Wenzhan Chen1, Zeting Li1, Huangmeng Xiao2, Zhuyu Li3, Haitian Chen3, Xiaopei Cao1*
1Department of Endocrinology, First Affiliated Hospital, Sun Yat-sen University, Guangzhou,China
2Department of Pediatrics, First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
3Department of Obstetrics and Gynecology, First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
*Corresponding Author: Xiaopei Cao, Department of Endocrinology, First Affiliated Hospital, Sun Yat-sen University, Guangzhou,China
Received: 11 January 2021; Accepted: 20 January 2021; Published: 10 February 2021
Citation:
Shufan Yue, Ling Pei, Wenzhan Chen, Zeting Li, Huangmeng Xiao, Zhuyu li, Haitian Chen, Xiaopei Cao. Dyslipidemia in Pregnancy and the Proper Reference Values: A Retrospective Study in South China. Obstetrics and Gynecology Research 4 (2021): 043-051.
View / Download Pdf Share at FacebookAbstract
Background: Dyslipidemia during pregnancy is associatied with the risk of adverse pregnancy outcomes. However, there is no uniform diagnostic criteria. “Williams Obstetrics 24th Edition” (WO24) and Wang et al gave different lipid references based on ethnic groups. To address the proper reference values of pregnant lipid, we conducted this retrospective study in pregnant women in South China.
Methods: 642 pregnant women were calculated the normal lipid range by 95th percentile and analyzed the association between lipid levels and adverse pregnancy outcomes by logistic regression models. Prevalence of adverse pregnancy outcomes in dyslipidemia patients diagnosed by the three different references were compared by Pearson’s chi-squared (χ2) test.
Results: The prevalence of dyslipidemia were 15.26% by the references of our research, 11.53% by WO24, and 17.45% by Wang, respectively. TC level was the risk factor of preterm birth (PTB); and TG level was associated with the risk of gestational diabetes mellitus (GDM) and PTB. The odds radio (OR) for GDM in patients with abnormal TG levels were 4.28[1.28-14.28] by WO24’s, 3.06[1.43-6.57] by ours, and 2.62[1.13-6.11] by Wang's. The OR for PTB in patients with abnormal TG levels were 4.22[1.21-14.69] by WO24’s, 3.04[1.22-7.62] by Wang’s, and 2.31 [0.95-5.63] by ours. A increased risk of macrosomia was only seen in patients with abnormal TC level by Wang's reference (OR 3.67 [1.12-12.06]).
Conclusions: Dyslipidemia during pregnancy is associated with the increases of pregnant complications. The reference by Wang et al were more applicable in Southern China.
Keywords
Dyslipidemia, Pregnancy, Complication, Reference Range
Dyslipidemia articles Dyslipidemia Research articles Dyslipidemia review articles Dyslipidemia PubMed articles Dyslipidemia PubMed Central articles Dyslipidemia 2023 articles Dyslipidemia 2024 articles Dyslipidemia Scopus articles Dyslipidemia impact factor journals Dyslipidemia Scopus journals Dyslipidemia PubMed journals Dyslipidemia medical journals Dyslipidemia free journals Dyslipidemia best journals Dyslipidemia top journals Dyslipidemia free medical journals Dyslipidemia famous journals Dyslipidemia Google Scholar indexed journals Pregnancy articles Pregnancy Research articles Pregnancy review articles Pregnancy PubMed articles Pregnancy PubMed Central articles Pregnancy 2023 articles Pregnancy 2024 articles Pregnancy Scopus articles Pregnancy impact factor journals Pregnancy Scopus journals Pregnancy PubMed journals Pregnancy medical journals Pregnancy free journals Pregnancy best journals Pregnancy top journals Pregnancy free medical journals Pregnancy famous journals Pregnancy Google Scholar indexed journals Complication articles Complication Research articles Complication review articles Complication PubMed articles Complication PubMed Central articles Complication 2023 articles Complication 2024 articles Complication Scopus articles Complication impact factor journals Complication Scopus journals Complication PubMed journals Complication medical journals Complication free journals Complication best journals Complication top journals Complication free medical journals Complication famous journals Complication Google Scholar indexed journals Reference Range articles Reference Range Research articles Reference Range review articles Reference Range PubMed articles Reference Range PubMed Central articles Reference Range 2023 articles Reference Range 2024 articles Reference Range Scopus articles Reference Range impact factor journals Reference Range Scopus journals Reference Range PubMed journals Reference Range medical journals Reference Range free journals Reference Range best journals Reference Range top journals Reference Range free medical journals Reference Range famous journals Reference Range Google Scholar indexed journals Obstetrics articles Obstetrics Research articles Obstetrics review articles Obstetrics PubMed articles Obstetrics PubMed Central articles Obstetrics 2023 articles Obstetrics 2024 articles Obstetrics Scopus articles Obstetrics impact factor journals Obstetrics Scopus journals Obstetrics PubMed journals Obstetrics medical journals Obstetrics free journals Obstetrics best journals Obstetrics top journals Obstetrics free medical journals Obstetrics famous journals Obstetrics Google Scholar indexed journals High-Density Lipid Cholesterol articles High-Density Lipid Cholesterol Research articles High-Density Lipid Cholesterol review articles High-Density Lipid Cholesterol PubMed articles High-Density Lipid Cholesterol PubMed Central articles High-Density Lipid Cholesterol 2023 articles High-Density Lipid Cholesterol 2024 articles High-Density Lipid Cholesterol Scopus articles High-Density Lipid Cholesterol impact factor journals High-Density Lipid Cholesterol Scopus journals High-Density Lipid Cholesterol PubMed journals High-Density Lipid Cholesterol medical journals High-Density Lipid Cholesterol free journals High-Density Lipid Cholesterol best journals High-Density Lipid Cholesterol top journals High-Density Lipid Cholesterol free medical journals High-Density Lipid Cholesterol famous journals High-Density Lipid Cholesterol Google Scholar indexed journals Low-Density Lipid Cholesterol articles Low-Density Lipid Cholesterol Research articles Low-Density Lipid Cholesterol review articles Low-Density Lipid Cholesterol PubMed articles Low-Density Lipid Cholesterol PubMed Central articles Low-Density Lipid Cholesterol 2023 articles Low-Density Lipid Cholesterol 2024 articles Low-Density Lipid Cholesterol Scopus articles Low-Density Lipid Cholesterol impact factor journals Low-Density Lipid Cholesterol Scopus journals Low-Density Lipid Cholesterol PubMed journals Low-Density Lipid Cholesterol medical journals Low-Density Lipid Cholesterol free journals Low-Density Lipid Cholesterol best journals Low-Density Lipid Cholesterol top journals Low-Density Lipid Cholesterol free medical journals Low-Density Lipid Cholesterol famous journals Low-Density Lipid Cholesterol Google Scholar indexed journals Pre-Pregnancy articles Pre-Pregnancy Research articles Pre-Pregnancy review articles Pre-Pregnancy PubMed articles Pre-Pregnancy PubMed Central articles Pre-Pregnancy 2023 articles Pre-Pregnancy 2024 articles Pre-Pregnancy Scopus articles Pre-Pregnancy impact factor journals Pre-Pregnancy Scopus journals Pre-Pregnancy PubMed journals Pre-Pregnancy medical journals Pre-Pregnancy free journals Pre-Pregnancy best journals Pre-Pregnancy top journals Pre-Pregnancy free medical journals Pre-Pregnancy famous journals Pre-Pregnancy Google Scholar indexed journals Gestational Diabetes Mellitus articles Gestational Diabetes Mellitus Research articles Gestational Diabetes Mellitus review articles Gestational Diabetes Mellitus PubMed articles Gestational Diabetes Mellitus PubMed Central articles Gestational Diabetes Mellitus 2023 articles Gestational Diabetes Mellitus 2024 articles Gestational Diabetes Mellitus Scopus articles Gestational Diabetes Mellitus impact factor journals Gestational Diabetes Mellitus Scopus journals Gestational Diabetes Mellitus PubMed journals Gestational Diabetes Mellitus medical journals Gestational Diabetes Mellitus free journals Gestational Diabetes Mellitus best journals Gestational Diabetes Mellitus top journals Gestational Diabetes Mellitus free medical journals Gestational Diabetes Mellitus famous journals Gestational Diabetes Mellitus Google Scholar indexed journals Preeclampsia articles Preeclampsia Research articles Preeclampsia review articles Preeclampsia PubMed articles Preeclampsia PubMed Central articles Preeclampsia 2023 articles Preeclampsia 2024 articles Preeclampsia Scopus articles Preeclampsia impact factor journals Preeclampsia Scopus journals Preeclampsia PubMed journals Preeclampsia medical journals Preeclampsia free journals Preeclampsia best journals Preeclampsia top journals Preeclampsia free medical journals Preeclampsia famous journals Preeclampsia Google Scholar indexed journals
Article Details
Abbreviations:
WO24: Williams Obstetrics 24th Edition; TC: Total Cholesterol; TG: Triglycerides; HDL-C: High-Density Lipid Cholesterol; LDL-C: Low-Density Lipid Cholesterol; p-BMI: Pre-Pregnancy Body Mass Index; GDM: Gestational Diabetes Mellitus; PIH: Pregnancy-Induced Hypertension; PE: Preeclampsia; PTB: Preterm Birth
1. Introduction
The levels of serum lipids physiologically raise throughout pregnancy due to unique physiological state and necessary metabolism functional adjustments [1-3]. The significant changes of lipid concentration can be observed from the second trimester of pregnancy [4]. However, evidences suggested that the increased maternal lipid levels are associated with adverse pregnancy outcomes, including gestational diabetes mellitus (GDM), pregnancy-induced hypertension (PIH), preterm birth (PTB), preeclampsia (PE), and macrosomia [5-9]. In addition, dyslipidemia during pregnancy may lead to postpartum dyslipidemia and postpartum impaired glucose tolerance in mothers [10-14] and metabolic disorders in offsprings [15].
However, there is no consensus about normal maternal lipid values during pregnancy. One of the most used reference criteria for lipids during pregnancy was from “Williams Obstetrics 24th Edition” (WO24) [16]. These reference values were calculated according to the 2.5th or 5th percentiles of lipid values from pregnant women mainly from Porto (Portugal), Graz (Austria) and Warsaw (Poland) studies. Recently, a study by Wang et al [17] propose a lipids reference for Northern Chinese pregnant women by calculated the 5th percentiles. The baseline characteristics were mostly similar for dyslipidemia people diagnosed by those two references, including maternal age, p-BMI, family history of diabetes and hypertension. However, it has been shown that the normal blood lipid ranges are different between Western and Eastern populations [18]. Therefore, the reference ranges of blood lipids during pregnancy might also vary from ethnic and regional groups. In this study, we analyzed the lipid profile in the Southern Chinese pregnant women of middle stage. The reference values of pregnant lipid were calculated by the 5th percentiles. And the pregnant complications were compared among the cohorts by three different diagnostic references, for the purpose to address the proper reference values of pregnant lipid in Southern Chinese women.
2. Methods
2.1 Data sources
This retrospective study was performed at one of the largest regional university hospitals in South China (The First Affiliated Hospital of Sun Yat-sen University). A total of 860 pregnant women who delivered at our institution between January 2018 and April 2018 were recruited. Approval was obtained from Institutional Re-view Board. Informed consent was waived because this study was retrospective. Women were excluded if they met the following conditions: (1) diagnosed of diabetes or hypertension before pregnancy; (2) patients with hypothyroidism or hyperthyroidism; (3) patients with chronic kidney disease or hepatic dysfunction damage; (4) multiple pregnancy; (5) missing data of blood lipids in the second trimester. Overall, 642 cases were included in the final analysis.
2.2 Data collection
Since lipid levels raise significantly from 12th week of
pregnancy and both of those two researches had recommended reference of dyslipidemia in second trimester, we compared the reference in the second trimester of pregnancy. The following data were collected from medical records: maternal age, pre-pregnancy body mass index (p-BMI), family history of diabetes and family history of hypertension, and results of pregnancy lipids, pregnancy complications including GDM, PIH, PE, PTB, and macrosomia. In “Williams Obstetrics 24th Edition” [16], the recommended reference unit for blood lipids was mg/dL. We converted the unit to mmol/l according to the conversion factors described in the instructions of the blood fat detection kit provided by Roche Diagnostics GmbH.
2.3 Measures
All blood samples were measured in the laboratory of the Department of Biochemistry of the First Affiliated Hospital of Sun Yat-sen University. Lipid levels were measured with standard enzymatic procedures on an automatic chemistry analyzer (Abbott Aeroset, Chicago, IL, USA). Reference values of the lipids were calculated with 95% confidenceinterval (CI). Abnormal TC, TG and LDL-c level were diagnosed with the value above the 95% percentiles, and abnormal HDL-c level was diagnosed with the value below the 5% percentiles.
2.4 Definitions of adverse pregnancy outcomes
The diagnosis of GDM was based on the International Association of Diabetes and Pregnancy Study Groups criteria [19], in which any of the three items following 75-g OGTT were reached: FPG levels > 5.1 mmol/L and < 7.0 mmol/L, 1 h PG levels ≥10.0 mmol/L, and 2 h PG levels ≥8.5 mmol/L and < 11.1 mmol/L. Pregnancy induced hypertension (PIH) included both gestational hypertension and PE. Gestational hypertension was defined as blood pressure elevation (systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg) at > 20 weeks’ gestation in the absence of proteinuria [20]. PE was defined as new-onset hypertension (systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg) and new-onset proteinuria (300 mg of protein in 24 h or a urine protein/creatinine ratio of 0.3 mg/dl) after 20 weeks of gestation, in a previously normotensive woman [20]. PTB was defined as gestational age of less than 37 weeks at delivery. Macrosomia was diagnosed when foetal birth weight ≥ 4000 g, regardless of gestational age.
2.5 Statistical analysis
Data analysis was performed by SPSS version 24.0. Continuous data were expressed as means ± standard deviation. Data between groups were compared using Student’s t-test for continuous variables. Categorical data, presented as a frequency were compared with Pearson’s chi-squared (χ2) test or Fisher’s exact test. Multivariate analysis was performed by logistic regression analysis. All statistical tests were two-sided, and P value <0.05 was considered to demonstrate statistical significance.
3. Results
3.1 Basic characteristics
Data of a total of 642 pregnant women of the mid-trimester were collected. The mean age were 32.70 ± 0.18 years. 6.54% of these women had a family history of diabetes and 10.44% had a family history of hypertension. The average lipid levels were presented in Table 1. The prevalence of dyslipidemia were 11.53% by WO24 reference value and 17.45% by Wang’s reference value (P<0.001). There was a trend of increase of TC, TG and LDL-c levels as the pregnant week increase, while the levels of HDL-c remanded stable during the whole pregnancy. The TC and LDL-c levels raised significantly between 16 to 20 weeks and maintained a smooth stage thereafter. However, the TG levels have shown continuous increase in the whole stages (as shown in Figure 1).
3.2 Referent range and risks of adverse pregnancy outcomes
The referent range of the lipids of our cohort were shown in table 2. The prevalence of dyslipidemia was 15.26% by the references of our research. After adjusted by maternal age, p-BMI, and gestational age at the time of lipid measurement, The relation between the lipid levels in second trimesters and the risk of pregnant complications were analyzed by logistic regression analysis. It was observed that increase of TC concentration was associated with increased risk for PTB (odd ratios [OR]: 1.150), increase of TG concentration was associated with increased risk for GDM (OR: 1.494) and PTB (OR: 1.415), and increase of HDL-C concentration was a protective factor for PIH (OR: 0.124) and PE (OR: 0.086). However, when we turned HDL-c concentration into a categorical variable, the protective effect was diminished. The level of LDL-c showed no statistic association with GDM, PIH, PE, PTB, and macrosomia (Table 2).
3.3 The adverse pregnant outcomes of dyslipidemia
The reference values of abnormal lipid levels were
presented in table 3 according to the 95th percentiles of the distributions. There was nosignificantdifferences in the prevalences of any kind adverse pregnant outcomes of abnormal lipid levels diagnosed by the three reference values. The prevalence of PTB among women with abnormal level of TC were 17.65% by ours, 15.79% by WO24’s, and 14.75% by Wang’s, respectively (table 4). The prevalence of GDM and PTB were more closer with abnormal level of TG diagnosed by our research (39.39% , 21.21%) and Wang's (37.04%, 25.93%). And the prevalence of PIH and PE were also more closer with abnormal level of HDL-c diagnosed by our research (8.82%, 2.94%) and Wang's (8.82% , 2.94%).
abnormal TC level from our research (P>0.05), neither WO24 and Wang et al. The risk of GDM increased in women with abnormal TG levels diagnosed by the three references, while the odds ratio in our research (3.06 [1.43-6.57]) were more closer to Wang et al (2.62 [1.13-6.11]) than WO24 (4.28 [1.28-14.28]). The odds radio for PTB raised significantly in those with abnormal TG level by Wang et al (3.04 [1.22-7.62]) and WO24 (4.22 [1.21-14.69]), and there was a trend of raised risk of PTB in abnormal TG level by our research (2.31 [0.95-5.63]). No significant differences in the risks of PIH and PE were observed in people with or without abnormal levels of HDL-c.
|
Characteristics |
Mean ± SD |
|
Maternal age (year) |
32.70 ± 0.18 |
|
p-BMI (kg/m2) |
21.07 ± 0.11 |
|
TC (mmol/L) |
6.09 ± 0.04 |
|
TG (mmol/L) |
2.12 ± 0.03 |
|
HDL-c (mmol/L) |
1.94 ± 0.14 |
|
LDL-c(mmol/L) |
3.48 ± 0.03 |
Abbreviations: p-BMI, pre-pregnancy body mass index; TC, total cholesterol; TG, triglycerides; HDL-C, high-density lipid cholesterol; LDL-C, low-density lipid cholesterol
Table 1: Basic characteristics of pregnant women.
TC, total cholesterol; TG, triglycerides; HDL-C, high-density lipid cholesterol; LDL-C, low-density lipid cholesterol
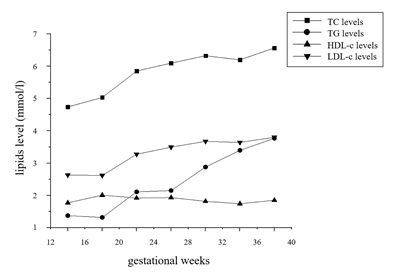
Figure 1: The changing curve of lipids level during pregnancy.
Adjusted for maternal age, pre-pregnancy body mass index, and gestational age at the time of lipid measurement. OR (95% CI) and P values were calculated by logistics regression analysis. TC, total cholesterol; TG, triglycerides; HDL-C, high-density lipid cholesterol; LDL-C, low-density lipid cholesterol; GDM, gestational diabetes mellitus; PIH, pregnancy-induced hypertension; PE, preeclampsia; PTB, Preterm birth
Table 2: Referent ranges and risk of adverse pregnancy outcomes.
|
TC (mmo/l) |
TG (mmo/l) |
HDL-c (mmo/l) |
LDL-c (mmo/l) |
|
|
WO241 |
< 7.74 |
<4.32 |
>1.35 |
<4.77 |
|
Wang et al.2 |
<7.50 |
<3.56 |
>1.41 |
<4.83 |
|
Our research3 |
< 7.90 |
<3.51 |
>1.38 |
<4.78 |
1WO24: reference from “Williams Obstetrics 24th Edition”
2Wang et al.: reference from Wang et al.
3Our research: 95th percentage from our population
TC, total cholesterol; TG, triglycerides; HDL-C, high-density lipid cholesterol; LDL-C, low-density lipid cholesterol
Table 3: Reference values for lipids level in middle pregnancy.
|
Serum Lipid |
TC |
TG |
HDL-c |
|||
|
Adverse pregnancy outcomes |
PTB |
GDM |
PTB |
PIH |
PE |
|
|
Our research1 |
prevalence |
17.65% |
39.39% |
21.21% |
8.82% |
2.94% |
|
OR (95% CI) |
2.14 (0.84-5.44) |
3.06 (1.43-6.57) |
2.31 (0.95-5.63) |
2.25 (0.62-8.22) |
1.10 (0.13-8.93) |
|
|
P valuesa |
0.052 |
0.004 |
0.066 |
0.219 |
0.926 |
|
|
WO242 |
prevalence |
15.79% |
50.00% |
33.33% |
4.35% |
NC # |
|
P valuesb |
0.833 |
0.524 |
0.448 |
0.641 |
1.000 |
|
|
OR (95% CI) |
1.79 (0.71-4.50) |
4.28 (1.28-14.28) |
4.22 (1.21-14.69) |
0.95 (0.12-7.54) |
NC # |
|
|
P valuesa |
0.166 |
0.025 |
0.034 |
0.193 |
NC # |
|
|
Wang3 |
prevalence |
14.75% |
37.04% |
25.93% |
8.82% |
2.94% |
|
P valuesb |
0.711 |
0.852 |
0.668 |
1.000 |
1.000 |
|
|
OR (95% CI) |
1.66 (0.77-3.57) |
2.62 (1.13-6.11) |
3.04 (1.22-7.62) |
2.06 (0.56-7.50) |
1.03 (0.13-8.36) |
|
|
P valuesa |
0.198 |
0.025 |
0.018 |
0.275 |
0.975 |
|
a P values of OR (95% CI). OR (95% CI) and P valuesa were calculated by logistics regression analysis
bCompare with our research, calculated by Fisher exact test
# No case observed
1 95th percentage from our population
2 reference from “Williams Obstetrics 24th Edition”
3 reference from Wang et al.
TC, total cholesterol; TG, triglycerides; HDL-C, high-density lipid cholesterol; LDL-C, low-density lipid cholesterol; PTB,
Preterm birth; GDM, gestational diabetes mellitus; PIH, pregnancy-induced hypertension; PE, preeclampsia
Table 4: Prevalences and risk of adverse pregnancy outcomes in people with abnormal lipids levels.
4. Discussion
It has been demonstrated that lipid levels raised significantly during middle pregnancy and abnormally elevated lipid levels were associated with adverse pregnant outcomes [6-7]. However, the recommended normal range of serum lipid level during pregnancy is still controversial. In the current study, wefor thefirsttime evaluated the different reference values of lipid levels in the second trimester pregnancy among southern Chinese women. Our study found that there were no significant differences between the reference values of lipid levels at mid-trimester pregnancy by WO24 and by Wang et al. However, the prevalence of dyslipidemia was significantly higher by Wang et al (17.45%) than that by WO24 (11.53%, vs Wang’s P<0.001). Our data has confirmed that abnormally elevated lipid levels were associated with increases of adverse pregnant outcomes. After adjusted by maternal age, p-BMI, and gestational age at the time of lipid measurement, TC levels was associated with an increased risk of PTB, and TG levels was associated with an increased risk of GDM and PTB.
There were no significant differences of prevalence or ORs of the abnormal pregnant outcomes were observed among the dyslipidemia pregnant women diagnosed with the three different reference values. Risk of GDM raised in women with abnormal level of TG by the three references, and risk of PTB raised in women with abnormal level of TG by WO24 and Wang et al., while risk of macrosomia was only raised in women with abnormal level of TC by Wang et al. There were nosignificant differencesin the prevalence of GDM, PTB, PIH, PE, and macrosomia in women with abnormal levels of TC, TG, HDL-c and LDL-c diagnosed by the references of our research, WO24’s, and Wang’s. However, the prevalence and the ORs of adverse pregnancy outcomes were more closer in dyslipidemia people diagnosed by our research and Wang et al than that by WO24 (Table 4). Considering that Caucasians were the main objects of WO24 study and it has been indicated that lipid levels were different between Asian pregnant women and European pregnant women [4], the differences of culture and ethnicity might account for the above differences.
This study found that every 1 mmol/l elevation in HDL-c concentration in second trimester was associated with a significant decreased risk of PIH and PE. However, when we turned HDL-c concentration into a categorical variable, the protective effect was diminished. Together with that there was no significant changes of HDL-c levels during the whole pregnancy, we consider the levels of HDL-c play a limited role in the adverse pregnant outcomes. Same is the LDL-c level as we found no statistic association between LDL-c level and any kind of adverse pregnant outcomes. TG was the lipid with the most obvious increase during pregnancy and was significantly associated with both the increase of GDM and PIH. TC levels raised significantly at 16 to 20 pregnant weeks and stabled in the following stages. It is also associated with increased risk of PIH. Taken together, attentions should be paied on the abnormally increases in the TG and TC levels during the second trimester of pregnancy, as it may be a mark of metabolic syndrome developed in pregnant mother that relates to the long term postpartum metabolic disorders in both mother and offsprings.
Our study showed that both WO24 and Wang’s study
provided applicable serum lipid reference values to the pregnant women in Southern China. The reference by Wang et al may be more applicable as the prevalence of dyslipidemia and the ORs of adverse outcomes were more similar with ours. Abnormally increased TG and TC levels at mid-stage of pregnacy play important role in the adverse pregnant outcome and may be associated with long term postpartum metabolic statements. There were several limitations in our study. First, the limited sample size of our study might weaken its power of presentative of women in Southern China. Second, the risk of selection bias is unavoidable in observational study. Therefore, furtherprospective multicenter randomized controlled investigations for lipid reference during the whole pregnancy are needed.
5. Conclusion
In conclusion, this study showed that dyslipidemia during pregnance is associated with the increases of pregnant complications. Futhermore, both the pregnant serum lipid references of WO24 and Wang’s study are applicable to pregnant women in Southern China. However, the reference by Wang et al provided a trend of more applicable. This finding provides evidence for lipids screening during pregnancy.
Funding
This study was supported by grants from the 5010 Project Foundation of Sun Yat-sen University (No. 2017001), National major and development projects (No. 2018YFC1314100) and the Science and Technology Foundation of Guangzhou City (No. 201803010101).
References
- Herrera E, Ortega-Senovilla H. Lipid metabolism during pregnancy and its implications for fetal growth. Curr Pharm Biotechnol 15 (2014): 24-31.
- Grimes SB, Wild R. Effect of Pregnancy on Lipid Metabolism and Lipoprotein Levels (2018).
- Mudd LM, Holzman CB, Evans RW. Maternal mid-pregnancy lipids and birthweight. Acta Obstet Gynecol Scand 94 (2015): 852-860.
- Aguilar Cordero MJ, Baena García L, Sánchez López AM, et al. Nivel De Triglicéridos Como Factor De Riesgo Durante El Embarazo; Modelado Biológico; Revisión Sistemática [Triglyceride Levels As A Risk Factor During Pregnancy; Biological Modeling; Systematic Review]. Nutr Hosp 32 (2015): 517-527.
- Retnakaran R, Wen SW, Tan H, et al. Maternal pre-gravid cardiometabolic health and infant birthweight: A prospective pre-conception cohort study. Nutr Metab Cardiovasc Dis 27 (2017): 723-730.
- Jin WY, Lin SL, Hou RL, et al. Associations between maternal lipid profile and pregnancy complications and perinatal outcomes: a population-based study from China. BMC Pregnancy Childbirth 16 (2016): 60.
- Shen H, Liu X, Chen Y, et al. Associations of lipid levels during gestation with hypertensive disorders of pregnancy and gestational diabetes mellitus: a prospective longitudinal cohort study. BMJ Open 6 (2016): e013509.
- Sharami SH, Gholipour M, Milani F, et al. The Association between Dyslipidemia and Preterm Birth: A Prospective Cohort Study in The North of Iran. Endocr Metab Immune Disord Drug Targets 20 (2020): 227-233.
- Wang J, Moore D, Subramanian A, et al. Gestational dyslipidaemia and adverse birthweight outcomes: a systematic review and meta-analysis. Obes Rev 19 (2018): 1256-1268.
- Xiao H, Chen Y, Pei L, et al. Influence of Dyslipidemia during Pregnancy on Postpartum Glucose and Lipid Metabolism in GDM Patients. Journal of Sun Yat-sen University (Medical Sciences) 41 (2020): 479-484.
- Wang D, Ding W, Xu S, et al. The relationship between total cholesterol and postpartum impaired glucose tolerance in women with gestational diabetes mellitus. Lipids Health Dis 19 (2020): 142.
- Pei L, Xiao H, Lai F, et al. Early postpartum dyslipidemia and its potential predictors during pregnancy in women with a history of gestational diabetes mellitus. Lipids Health Dis 19 (2020): 220.
- Abdel-Hamid TA, AbdelLatif D, Ahmed E, et al. Relation between Maternal and Neonatal Serum Lipid Profile and Their Impact on Birth Weight. Am J Perinatol (2020).
- Adank MC, Benschop L, van Streun SP, et al. Gestational lipid profile as an early marker of metabolic syndrome in later life: a population-based prospective cohort study. BMC Med 18 (2020): 394.
- Qiao L, Wattez JS, Lim L, et al. Prolonged Prepregnant Maternal High-Fat Feeding Reduces Fetal and Neonatal Blood Glucose Concentrations by Enhancing Fetal β-Cell Development in C57BL/6 Mice. Diabetes 68 (2019): 1604-1613.
- Gary Cunningham F, Kenneth J Leveno, Steven L Bloom, et al. Williams obstetrics-24th edition. New York: McGraw-hill education (2014).
- Wang C, Kong L, Yang Y, et al. Recommended reference values for serum lipids during early and middle pregnancy: a retrospective study from China. Lipids Health Dis 17 (2018): 246.
- Chinese guidelines for prevention and treatment of hypertension (2018 revision). Chinese Journal of Cardiovascular Diseases 24 (2019): 24-56.
- Diagnostic Criteria and Classification of Hyperglycaemia First Detected in Pregnancy. Geneva: World Health Organization (2013).
- Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol 122 (2013): 1122-1131.
