Dorsal Second and Third Carpometacarpal Joint Dislocation: A Case Report
Article Information
Charalampos Pitsilos1*, Theofylaktos Kyriakidis1,2, Konstantinos Chitas1, Konstantinos Ditsios1
1Second Orthopaedic Department Aristotle University of Thessaloniki, G. Gennimatas Hospital, Ethnikis Aminis 41, 54635, Thessaloniki, Greece
2Department of Orthopaedic Surgery and Traumatology, Erasme University Hospital, Université Libre de Bruxelles, Route de Lennik 808, 1070 Brussels, Belgium
*Corresponding Author: Charalampos Pitsilos, Second Orthopaedic Department Aristotle University of Thessaloniki, G. Gennimatas Hospital, Ethnikis Aminis 41, 54635, Thessaloniki, Greece
Received: 30 May 2022; Accepted: 06 June 2022; Published: 17 June 2022
Citation: Charalampos Pitsilos, Theofylaktos Kyriakidis, Konstantinos Chitas, Konstantinos Ditsios. Dorsal Second and Third Carpometacarpal Joint Dislocation: A Case Report. Journal of Surgery and Research 5 (2022): 346-351.
View / Download Pdf Share at FacebookAbstract
Background
Carpometacarpal joint dislocations are uncommon hand injuries occurring in less than 1% of hand trauma. On routine postero-anterior view, asymmetry at the carpometacarpal joints should raise suspicion of possible subtle injury, which can be confirmed with CT scan. In literature, there is a scarcity of published cases and the optional treatment is controversial.
Case report
A 28-year-old man presented with dorsal dislocation of the second and third carpometacarpal joints. After initial closed reduction, the computerized tomography scan revealed residual dorsal subluxation. The patient was successfully treated with closed reduction under fluoroscopy and percutaneous pinning. In the follow-up full range of motion was gained and there were no recurrence or signs of degenerative changes.
Conclusion
Closed reduction of traumatic dorsal second and third carpometacarpal dislocation may be associated with incomplete reduction. Reduction under fluoroscopy and percutaneous pinning may be more suitable for the treatment of these injuries.
Keywords
Carpometacarpal Joint, Dorsal, Joint Dislocation, Hand
Carpometacarpal Joint articles; Dorsal articles; Joint Dislocation articles; Hand articles
Carpometacarpal Joint articles Carpometacarpal Joint Research articles Carpometacarpal Joint review articles Carpometacarpal Joint PubMed articles Carpometacarpal Joint PubMed Central articles Carpometacarpal Joint 2023 articles Carpometacarpal Joint 2024 articles Carpometacarpal Joint Scopus articles Carpometacarpal Joint impact factor journals Carpometacarpal Joint Scopus journals Carpometacarpal Joint PubMed journals Carpometacarpal Joint medical journals Carpometacarpal Joint free journals Carpometacarpal Joint best journals Carpometacarpal Joint top journals Carpometacarpal Joint free medical journals Carpometacarpal Joint famous journals Carpometacarpal Joint Google Scholar indexed journals Dorsal articles Dorsal Research articles Dorsal review articles Dorsal PubMed articles Dorsal PubMed Central articles Dorsal 2023 articles Dorsal 2024 articles Dorsal Scopus articles Dorsal impact factor journals Dorsal Scopus journals Dorsal PubMed journals Dorsal medical journals Dorsal free journals Dorsal best journals Dorsal top journals Dorsal free medical journals Dorsal famous journals Dorsal Google Scholar indexed journals Joint Dislocation articles Joint Dislocation Research articles Joint Dislocation review articles Joint Dislocation PubMed articles Joint Dislocation PubMed Central articles Joint Dislocation 2023 articles Joint Dislocation 2024 articles Joint Dislocation Scopus articles Joint Dislocation impact factor journals Joint Dislocation Scopus journals Joint Dislocation PubMed journals Joint Dislocation medical journals Joint Dislocation free journals Joint Dislocation best journals Joint Dislocation top journals Joint Dislocation free medical journals Joint Dislocation famous journals Joint Dislocation Google Scholar indexed journals degenerative changes articles degenerative changes Research articles degenerative changes review articles degenerative changes PubMed articles degenerative changes PubMed Central articles degenerative changes 2023 articles degenerative changes 2024 articles degenerative changes Scopus articles degenerative changes impact factor journals degenerative changes Scopus journals degenerative changes PubMed journals degenerative changes medical journals degenerative changes free journals degenerative changes best journals degenerative changes top journals degenerative changes free medical journals degenerative changes famous journals degenerative changes Google Scholar indexed journals percutaneous pinning articles percutaneous pinning Research articles percutaneous pinning review articles percutaneous pinning PubMed articles percutaneous pinning PubMed Central articles percutaneous pinning 2023 articles percutaneous pinning 2024 articles percutaneous pinning Scopus articles percutaneous pinning impact factor journals percutaneous pinning Scopus journals percutaneous pinning PubMed journals percutaneous pinning medical journals percutaneous pinning free journals percutaneous pinning best journals percutaneous pinning top journals percutaneous pinning free medical journals percutaneous pinning famous journals percutaneous pinning Google Scholar indexed journals posteroanterior radiographs articles posteroanterior radiographs Research articles posteroanterior radiographs review articles posteroanterior radiographs PubMed articles posteroanterior radiographs PubMed Central articles posteroanterior radiographs 2023 articles posteroanterior radiographs 2024 articles posteroanterior radiographs Scopus articles posteroanterior radiographs impact factor journals posteroanterior radiographs Scopus journals posteroanterior radiographs PubMed journals posteroanterior radiographs medical journals posteroanterior radiographs free journals posteroanterior radiographs best journals posteroanterior radiographs top journals posteroanterior radiographs free medical journals posteroanterior radiographs famous journals posteroanterior radiographs Google Scholar indexed journals radiographic evaluation articles radiographic evaluation Research articles radiographic evaluation review articles radiographic evaluation PubMed articles radiographic evaluation PubMed Central articles radiographic evaluation 2023 articles radiographic evaluation 2024 articles radiographic evaluation Scopus articles radiographic evaluation impact factor journals radiographic evaluation Scopus journals radiographic evaluation PubMed journals radiographic evaluation medical journals radiographic evaluation free journals radiographic evaluation best journals radiographic evaluation top journals radiographic evaluation free medical journals radiographic evaluation famous journals radiographic evaluation Google Scholar indexed journals avulsion fracture articles avulsion fracture Research articles avulsion fracture review articles avulsion fracture PubMed articles avulsion fracture PubMed Central articles avulsion fracture 2023 articles avulsion fracture 2024 articles avulsion fracture Scopus articles avulsion fracture impact factor journals avulsion fracture Scopus journals avulsion fracture PubMed journals avulsion fracture medical journals avulsion fracture free journals avulsion fracture best journals avulsion fracture top journals avulsion fracture free medical journals avulsion fracture famous journals avulsion fracture Google Scholar indexed journals
Article Details
1. Introduction
Dislocation of the carpometacarpal (CMC) joints are rare injuries in the hand [1]. Dorsal dislocations are the most frequently reported [2]. Stronger dorsal ligaments and wrist extensor restraints cause failure of the bone dorsally with subsequent rupture of the volar ligaments, allowing for dorsal dislocations to occur more commonly than volar once [3]. In most cases, treatment of such injuries requires closed reduction with percutaneous pinning or open reduction and internal fixation [4]. The purpose of this report was to present a patient with second and third CMC dorsal dislocation, an unusual injury pattern, who was satisfactorily treated with closed reduction and Kirschner-wire (K-wire) fixation.
2. Case Report
A 28-year-old male presented a right-hand injury after a direct trauma during a fight. He complained of oedema, pain, and functional limitation of the injured hand. The clinical examination revealed a significant soft tissue swelling over the dorsal surface of the hand (Figure 1), tenderness over the base of the second and third metacarpals, and limitation of both active and passive range of motion. Standard radiographs demonstrated a dorsal dislocation of the second and third CMC joints with proximal migration of the second and third metacarpal (Figure 2). The hand was well perfused, and no signs of neurologic impairment were found. External maneuvers for reduction were performed by applying longitudinal traction to the involved rays, under local anesthesia, in the emergency room. Afterward, radiographs were taken to verify the reduction. However, an anatomical reduction of the joints was not obtained and thus, a computerized tomography (CT) scan was performed. Dorsal subluxation of both CMC joins and avulsion fracture of the volar base of both metacarpals were identified (Figure 3). Hence, surgical treatment from an expert in hand surgery was decided. In the operating room, under general anesthesia, a closed manipulation was attempted in the form of exaggerating the deformity and maneuvering a gentle distally directed force over the subluxated second and third metacarpal base. Under fluoroscopy guidance, both CMC joints were stabilized with two crossed 1.6 mm K-wires each (Figure 4). A short arm cast was applied for four weeks after which the K-wires were removed and rehabilitation instituted. Over the 12 months of follow-up, there was no evidence of recurrence or signs of degenerative changes (Figure 5). The patient was satisfied about the outcome, regained full range of motion with no functional deficit and returned to pre-injury activities.

Figure 1: Swelling on the dorsal aspect of the right hand.
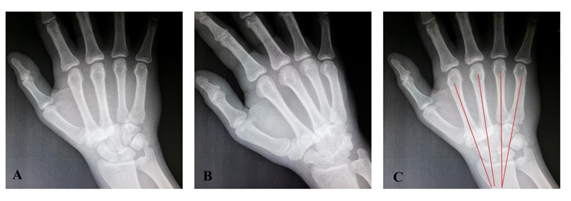
Figure 2: Postero-anterior (A) and oblique (B) radiographs of the right hand showing a dislocation of the second and third CMC joints. Metacarpal cascade lines are not focused to a common spot proximally to radial articular surface (C).
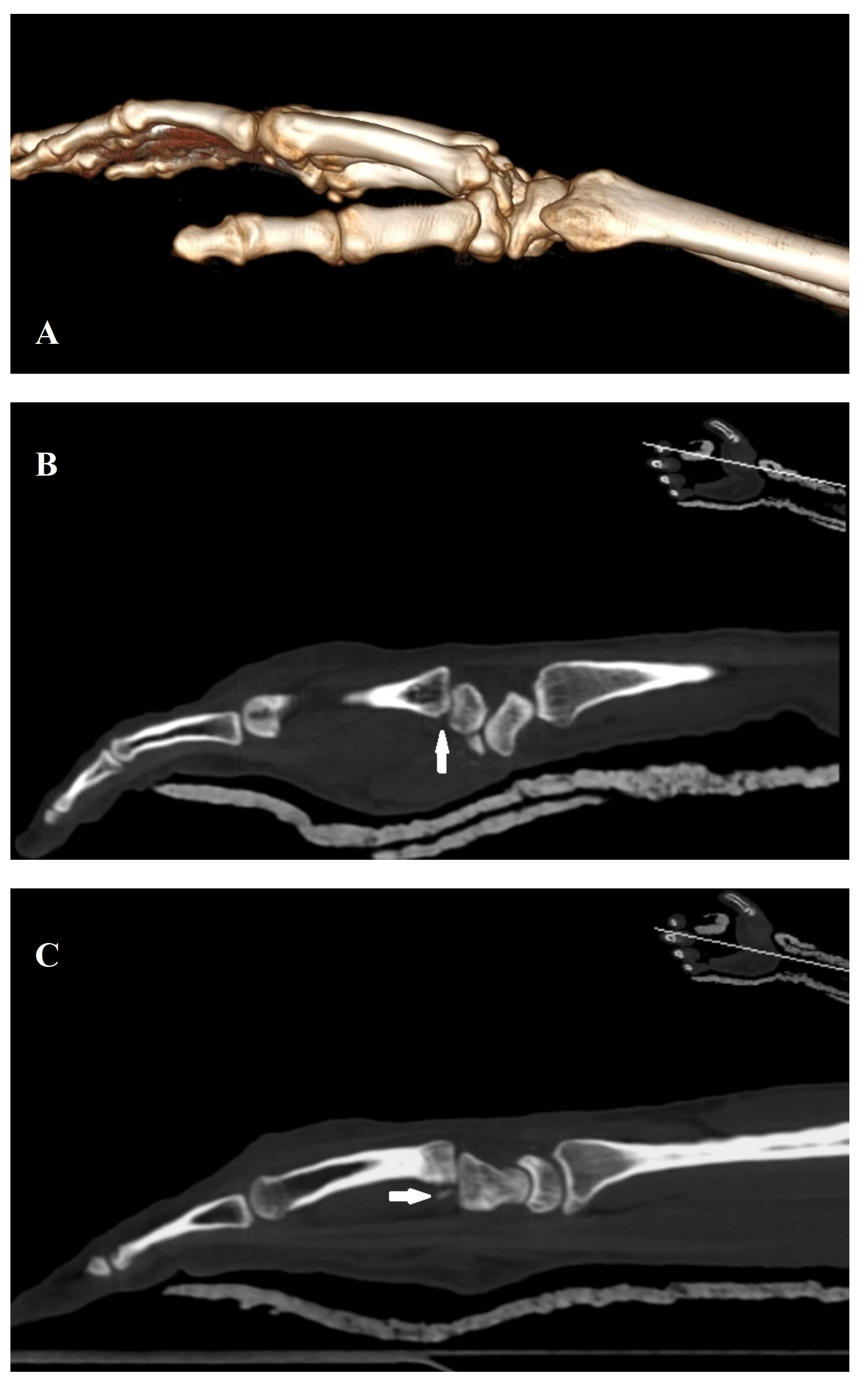
Figure 3: CT images of the right hand demonstrating dorsal subluxation of the second and third CMC joint (A). Avulsion fracture of the base of the second (B) and third (C) metatarsal are obvious (white arrows).
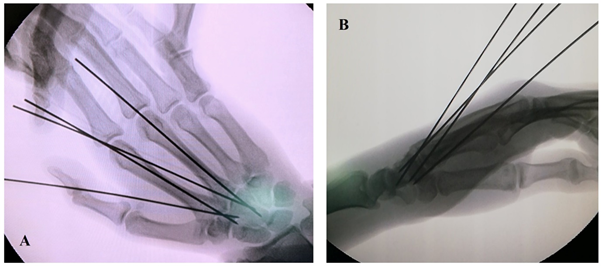
Figure 4: Intraoperative postero-anterior (A) and oblique (B) radiographs of the right hand showing reduction of the CMC joints and K-wire fixation in a crossed manner.
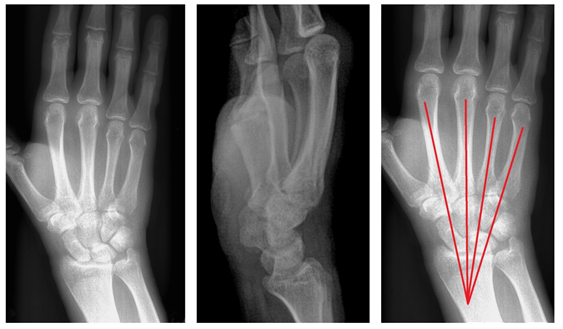
Figure 5: At 12 months, postoperative postero-anterior (A) and oblique (B) radiographs of the right hand showing reduced second and third CMC joints. Metacarpal cascade lines are focused to a common spot proximally to radial articular surface (C).
3. Discussion
This case report presents a patient with concomitant second and third CMC dislocation, treated successfully with closed reduction and percutaneous pinning. This is a rare injury pattern with a scarcity of published cases [5]. CMC joint dislocations are uncommon, representing less than 1% of all hand trauma [1]. This traumatic pathology tends to be related to high-energy mechanism, including motor-vehicle accident and fall from height; still, lower energy mechanism, such as punching, as in our case, has also been described [6]. The direct injury usually results in posterior dislocation of the metacarpal base following a flexion force subjected to the metacarpal head. In contrast, the indirect injury may result in hyperextension force causing anterior dislocation [3,7]. The second and third CMC joints are very rigid compared to the fourth and fifth CMC joints, which have greater mobility due to their saddle configuration combined with looser ligamentous attachments [8]. Generally, second and third CMC dislocations are fracture dislocations, resulted from avulsion of the attached ligaments [9], as in the present case. Dislocations are classified according to the direction of deformity as dorsal or volar, with a higher rate of the former, as the dorsal interosseous ligaments are stronger against their volar counterparts [2]. They are presented with a bump or dimple deformity of the dorsal aspect of the hand, respectively [7]. However, diagnosis of CMC dislocations may be complicated on initial examination by the significant soft tissue swelling and the poorly visualized injury on posteroanterior radiographs. On these radiographs, a method of investigation is the inspection of metacarpal cascade lines, which are superimposed through the central longitudinal axis of each metacarpal and typically focus on a common spot proximally to the radiocarpal joint. In the case of CMC dislocation, these lines diverge. While dislocations are usually evident on lateral or oblique views, they may be challenging to identify in cases of minimal subluxation or inadequate visualization due to improper positioning. In doubt, a computed tomography (CT) is recommended [10]. In our case, the initial diagnosis was evident after the radiographic evaluation; still, the CT demonstrated both the avulsion fracture of the base of metacarpals and the dorsal subluxation of CMC joints after the initial attempt of reduction indicated surgical treatment. The main goal of treatment of CMC dislocation is the successful return to former activity with a functional and pain-free hand [6]. This is achieved by the restoration of articular anatomy which preserves mobility and prevents further displacement, instability and post-traumatic arthritis. Immediate reduction is essential for the better outcome, and closed reduction can be achieved in acute dislocations [4]. Successful conservative treatment of isolated second CMC dislocation or concomitant second through fourth CMC dislocations with closed reduction and immobilization in short arm splint have been reported [7]. As recurrent dislocation occurs most commonly in the first two weeks, a weekly radiographic evaluation is recommended in such cases [4]. However, in literature, surgical treatment has been preferred in concomitant second and third CMC dislocation. Operative management includes closed reduction and percutaneous pinning and open reduction and osteosynthesis with K-wires [5,7]. Open reduction is recommended in cases of unsuccessful closed reduction due to soft tissue interposition, contractures from delayed presentation or diagnosis, and displaced avulsion fractures of ligaments or extrinsic tendons [6]. Postoperatively, immobilization is initiated and may last from 3 to 8 weeks, after which the K-wires are removed and range of motion exercises are instituted [7]. In our case, closed reduction and percutaneous K-wire fixation was applied, as the injury was acute and reduction was achievable, and immobilization lasted for four weeks, followed by K-wire removal and rehabilitation. Dorsal dislocation of the second and third CMC joints compromises rare injuries. They may be missed in an acute setting, and swelling around the wrist with painful restriction of motion should alert the clinician towards the possibility of such injuries. On standard postero-anterior view, overlap of joint surfaces and asymmetry at the CMC joints should raise suspicion of a subtle injury, which can be confirmed with a CT scan. Given that there is a lack of published cases and the appropriate treatment is controversial, we reported a case early diagnosed and successfully treated with closed reduction and K-wire fixation.
References
- Eichhorn-Sens J, Katzer A, Meenen NM, et al. Handchirurgie, Mikrochirurgie, plastische Chirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft fur Handchirurgie: Organ der Deutschsprachigen Arbeitsgemeinschaft fur Mikrochirurgie der Peripheren Nerven und Gefasse 33 (2001): 189.
- Giacomo LMD, Khan MS, Illuminati I, et al. Carpometacarpal Joint Concurrent Dislocation of Four Long Finger: Results of A Non-Operative Management (2016).
- Kumar R, Malhotra R. Divergent fracture-dislocation of the second carpometacarpal joint and the three ulnar carpometacarpal joints. The Journal of hand surgery 26 (2001): 123-129.
- Storken G, Bogie R, Jansen EJ. Acute ulnar carpometacarpal dislocations. Can it be treated conservatively? A review of four cases. Hand (New York, NY) 6 (2011): 420-423.
- Mueller JJ. Carpometacarpal dislocations: report of five cases and review of the literature. The Journal of hand surgery 11 (1986): 184-188.
- Bhardwaj P, Sivakumar BS, Vallurupalli A, et al. Fracture dislocations of the carpometacarpal joints of the fingers. Journal of clinical orthopaedics and trauma 11 (2020): 562-569.
- Cardozo DF, Plata GV, Casas JA, et al. Acute Dislocation of the Metacarpal-Trapezoid Joint. Clinics in orthopedic surgery 8 (2016): 223-227.
- Nakamura K, Patterson RM, Viegas SF. The ligament and skeletal anatomy of the second through fifth carpometacarpal joints and adjacent structures. The Journal of hand surgery 26 (2001): 1016-1029.
- Yoshida R, Shah MA, Patterson RM, et al. Anatomy and pathomechanics of ring and small finger carpometacarpal joint injuries. The Journal of hand surgery 28 (2003): 1035-1043.
- Hodgson PD, Shewring DJ. The 'metacarpal cascade lines'; use in the diagnosis of dislocations of the carpometacarpal joints. The Journal of hand surgery 32 (2007): 277-281.
