Digital Therapeutics (DTx) for Temporomandibular Disorder (TMD)
Article Information
Sang-Yoon Park1, Daehyun Kim2, Bong-Ju Kim3, Kyung Won Ju3, Young-Kyun Kim4, Joo-Young Park5*, Jong-Ho Lee1,3,6*
1Department of Oral and Maxillofacial Surgery, School of Dentistry and Dental Research Institute, Seoul National University, Seoul, Korea
2Department of Periodontology, College of Dentistry, Yonsei University, Seoul, Republic of Korea
3Innovation Research & Support Center for Dental Science, Seoul National University Dental Hospital, Seoul, Korea
4Dept. of Oral & Maxillofacial Surgery, Section of Dentistry, Seoul National University Bundang Hospital, Korea
5Department of Oral and Maxillofacial Surgery, Seoul National University School of Dentistry, Seoul National University Dental Hospital, Korea
6Oral Oncology Clinic, National Cancer Center, Ilsan, Republic of Korea
*Corresponding Author: Joo-Young Park and Jong-Ho Lee, Department of Oral and Maxillofacial Surgery, Seoul National University School of Dentistry, Seoul National University Dental Hospital. 101 Daehak-ro, Jongno-gu, Seoul 03080, South Korea.
Received: 23 September 2022; Accepted: 27 October 2022; Published: 15 November 2022
Citation: Sang-Yoon Park, Daehyun Kim, Bong-Ju Kim, Kyung Won Ju, Young-Kyun Kim, Joo-Young Park, Jong-Ho Lee. Digital Therapeutics (DTx) for Temporomandibular Disorder (TMD). Archives of Clinical and Medical Case Reports 6 (2022): 725-729.
View / Download Pdf Share at FacebookAbstract
Due to the pandemic situation of the Covid-19 virus, our daily life has changed a lot [1]. Many changes have also taken place in the fields of medicine and dentistry. The most prominent field is the field of digital medicine, and the field of digital therapeutics (DTx) has developed rapidly along with the technology of other fields [2,3]. In the case of digital therapeutics, it is evaluated that it can be remarkably applied in the field that requires behavioral control or the field that requires the approach of mental health medicine. In addition, studies are being carried out notably in high blood pressure, diabetes, heart-related diseases, addiction, dementia, and Attention Deficit/Hyperactivity Disorder (ADHD) that require management as a chronic disease. However, in the field of dentistry, there are not many fields where digital therapeutics are applied prominently, but application to temporomandibular disorder can be devised,4 and the reason for this can be discussed in this article.
Keywords
Cognitive Behavior Therapy; Digital Therapeutics; Digital Medicine; Temporomandibular Disorder (TMD); Teledentistry
Cognitive Behavior Therapy articles; Digital Therapeutics articles; Digital Medicine articles; Temporomandibular Disorder (TMD) articles; Teledentistry articles
Cognitive Behavior Therapy articles Cognitive Behavior Therapy Research articles Cognitive Behavior Therapy review articles Cognitive Behavior Therapy PubMed articles Cognitive Behavior Therapy PubMed Central articles Cognitive Behavior Therapy 2023 articles Cognitive Behavior Therapy 2024 articles Cognitive Behavior Therapy Scopus articles Cognitive Behavior Therapy impact factor journals Cognitive Behavior Therapy Scopus journals Cognitive Behavior Therapy PubMed journals Cognitive Behavior Therapy medical journals Cognitive Behavior Therapy free journals Cognitive Behavior Therapy best journals Cognitive Behavior Therapy top journals Cognitive Behavior Therapy free medical journals Cognitive Behavior Therapy famous journals Cognitive Behavior Therapy Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Digital Therapeutics articles Digital Therapeutics Research articles Digital Therapeutics review articles Digital Therapeutics PubMed articles Digital Therapeutics PubMed Central articles Digital Therapeutics 2023 articles Digital Therapeutics 2024 articles Digital Therapeutics Scopus articles Digital Therapeutics impact factor journals Digital Therapeutics Scopus journals Digital Therapeutics PubMed journals Digital Therapeutics medical journals Digital Therapeutics free journals Digital Therapeutics best journals Digital Therapeutics top journals Digital Therapeutics free medical journals Digital Therapeutics famous journals Digital Therapeutics Google Scholar indexed journals Ultrasound articles Ultrasound Research articles Ultrasound review articles Ultrasound PubMed articles Ultrasound PubMed Central articles Ultrasound 2023 articles Ultrasound 2024 articles Ultrasound Scopus articles Ultrasound impact factor journals Ultrasound Scopus journals Ultrasound PubMed journals Ultrasound medical journals Ultrasound free journals Ultrasound best journals Ultrasound top journals Ultrasound free medical journals Ultrasound famous journals Ultrasound Google Scholar indexed journals Digital Medicine articles Digital Medicine Research articles Digital Medicine review articles Digital Medicine PubMed articles Digital Medicine PubMed Central articles Digital Medicine 2023 articles Digital Medicine 2024 articles Digital Medicine Scopus articles Digital Medicine impact factor journals Digital Medicine Scopus journals Digital Medicine PubMed journals Digital Medicine medical journals Digital Medicine free journals Digital Medicine best journals Digital Medicine top journals Digital Medicine free medical journals Digital Medicine famous journals Digital Medicine Google Scholar indexed journals Radiotherapy articles Radiotherapy Research articles Radiotherapy review articles Radiotherapy PubMed articles Radiotherapy PubMed Central articles Radiotherapy 2023 articles Radiotherapy 2024 articles Radiotherapy Scopus articles Radiotherapy impact factor journals Radiotherapy Scopus journals Radiotherapy PubMed journals Radiotherapy medical journals Radiotherapy free journals Radiotherapy best journals Radiotherapy top journals Radiotherapy free medical journals Radiotherapy famous journals Radiotherapy Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Prognosis articles Prognosis Research articles Prognosis review articles Prognosis PubMed articles Prognosis PubMed Central articles Prognosis 2023 articles Prognosis 2024 articles Prognosis Scopus articles Prognosis impact factor journals Prognosis Scopus journals Prognosis PubMed journals Prognosis medical journals Prognosis free journals Prognosis best journals Prognosis top journals Prognosis free medical journals Prognosis famous journals Prognosis Google Scholar indexed journals Seasonality articles Seasonality Research articles Seasonality review articles Seasonality PubMed articles Seasonality PubMed Central articles Seasonality 2023 articles Seasonality 2024 articles Seasonality Scopus articles Seasonality impact factor journals Seasonality Scopus journals Seasonality PubMed journals Seasonality medical journals Seasonality free journals Seasonality best journals Seasonality top journals Seasonality free medical journals Seasonality famous journals Seasonality Google Scholar indexed journals Teledentistry articles Teledentistry Research articles Teledentistry review articles Teledentistry PubMed articles Teledentistry PubMed Central articles Teledentistry 2023 articles Teledentistry 2024 articles Teledentistry Scopus articles Teledentistry impact factor journals Teledentistry Scopus journals Teledentistry PubMed journals Teledentistry medical journals Teledentistry free journals Teledentistry best journals Teledentistry top journals Teledentistry free medical journals Teledentistry famous journals Teledentistry Google Scholar indexed journals
Article Details
1. Introduction
Digital therapy is an Evidence-based therapy, and the most important feature is that it is software-based. It aims to prevent, manage, and treat medical disorders. The easiest explanation is that the patient uses software to self-manage his/her symptoms to relieve symptoms and improve quality of life [5]. In addition, digital therapeutics are still evolving more effectively with the development of various technologies. In addition to the spread of smartphones, for example, artificial intelligence (AI), Internet of Things (IoT), Virtual reality (VR), and Augmented reality (AR) [6,7]. The core concept of digital therapeutics is self-managing and is based on cognitive behavioral therapy. This method can work effectively in many chronic, high-recurring diseases that require behavioral control. For example, it can be effective in drug addiction, alcoholism, or smoking cessation treatment [8]. In fact, the first digital treatment to receive USFDA approval is a drug addiction treatment. (reSET®, Pear Therapeutics Inc., Boston, USA) Since then, research and development in many diseases has been made. For example, high blood pressure, diabetes, Alzheimer's disease, insomnia, depression, etc. are being developed [9-18]. However, the use of digital therapeutics in dentistry, not medicine, is currently insignificant. It is safe to say that there is currently little research and development of digital therapeutics in the field of dental or dentistry other than teledentistry. In this review, the application of digital therapeutics to patients with temporomandibular disorder will be considered.
2. Temporomandibular Disorder and Digital Therapeutics (DTx)
Temporomandibular disorder refers to pain and functional limitation occurring in the maxillofacial region. According to a relatively recent study, it is reported that about 5-15% of the total adult population suffers from it [19]. Interestingly, there is also a study result that TMD occurs more frequently in modern people [20]. A recent systematic review and meta-analysis in 2021 concluded that the prevalence of TMD was 31% for adults and 11% for children and adolescence [21]. The etiology of TMD is known to be multifactoral, and the exact mechanism has not been elucidated. However, it is known that physical factors and psychological factors contribute together [22-24]. In practice, skeletomuscular problems can lead to problems with internal derangement of temporomandibular joint (TMJ). This can lead to pain and other symptoms and, in severe cases, osteroarthritis. The presence of skeletomuscular anomalies does not result in the same degree of symptoms and pain. We should therefore pay attention to biopsychosocial factors, and there have been many studies on this point [23,25]. High levels of depression and anxiety were significantly associated with the development of symptoms of TMD. In addition, in patients with existing TMD symptoms, stress became a factor that accelerated and worsened symptoms. In addition, there is a study reporting that depression and stress were increased along with symptoms related to TMD during social lockdown and personal isolation due to COVID-19 [26,27]. There are many difficulties in accurately classifying and treating TMD itself. Recently, there have been many studies to classify these TMDs. As a result, the Diagnostic Criteria for Temporomandibular Disorder (DC/TMD) is the most widely known and accepted for classification and standardization of TMD. In DC/TMD, classification and diagnosis are made through two axes. Axis-I focuses on biological based factors of joints and musculature. On the other hand, Axis-II focuses on psychosocial & behavioral factors [28]. Clinicians treating TMD must record these assessment items. Clinicians also need to determine if the patient has any habits (smoking, drinking, bruxism or clenching etc). It is also necessary to understand the psychological history (Figure 1).
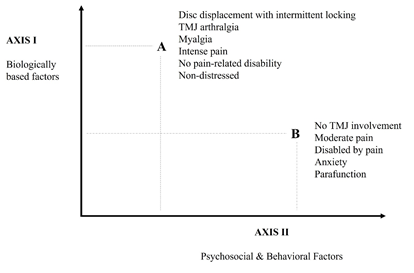
Figure 1:Biopsychosocial model of disease applied to TMD.
The answer to the question of how and how important psychosocial factors affect TMD is that they are very important factors. Evidence from many studies has demonstrated that psychosocial factors develop and aggravate the state of chronic pain, and that this tendency is also seen in patients with TMD [29-31]. It is also important to note that psychosocial and cognitive behavioral interventions in these patients with acute TMD are sufficiently effective in preventing the transition to chronic TMD [32]. The start of treatment and management of TMD patients begins with understanding the importance of education and self-management, not drug treatment and the use of splint devices. Many clinicians give patients an anatomical schematic or explanation of the mechanism of TMD. It also explains and recommends self-management methods in daily life. For example, sleep hygiene, avoiding parafunctional habits, and abstaining from caffeine and alcohol [33]. Factors influencing pain include the patient's own beliefs, surrounding environment, family relationships, and interpersonal relationships, which affect the onset, development, and persistence of pain. In this sense, the axis-II classification of DC/TMD shows the importance of psychosocial aspect. This allows us to understand the factors that are variously related to the patient's depression, anxiety, and parafunctional behaviors, as well as the aspects that make judgments about pain or symptoms. However, allowing this approach to treat TMD can make it seem like the dental clinician has given up on the patient and has entered the final stage. These impressions can in turn negatively affect the patient and aggravate the disease [33]. Therefore, it is necessary to approach, evaluate, and explain to the patient the Axis-II part from the initial treatment stage of TMD. This will be very important in suppressing the chronicity of TMD and reducing the recurrence rate (Table 1).
|
Domain |
Instrument |
No. of items |
|
Pain intensity |
Graded Chronic Pain Scale (GCPS) |
3 |
|
Pain Location |
Pain drawing |
1 |
|
Physical Function |
Graded Chronic Pain Scale (GCPS) |
4 |
|
Limitation |
Jaw-function limitation Scale-short form (JFLS) |
8 |
|
Jaw-function limitation Scale-long form (JFLS) |
20 |
|
|
Distress |
Patient Health Quesionnarie-4 (PHQ-4) |
4 |
|
Depression |
Patient Health Quesionnarie-9 (PHQ-9) |
9 |
|
Anxiety |
Generalized Anxiety Disorder-7 (GAD-7) |
7 |
|
Physical Symptoms |
Patient Health Quesionnarie-15 (PHQ-15) |
15 |
|
Parafunction |
Oral Behaviours checklist (OBC) |
21 |
Table 1: DC TMD Axis II assessment protocol.
Digital therapeutics have advantages in many ways, but the advantage is that they can aid in this self-management and amplify the therapeutic effect resulting from the patient's self-evaluation and continuous cognition. As mentioned in the previous paragraph, this aspect of TMD treatment is very important. Therefore, among dental treatment or oral maxillofacial treatment, digital therapeutic seems to be very effective, especially for TMD. In the past, Turner and colleagues have studied cognitive behavioral therapy for TMD using a daily electronic device. This study was conducted in 2005 and before the development of smartphones. It is thought that the size and performance of the device would have been much more inconvenient than it is now. In the study, after TMD treatment at the clinic, it was divided into a group that performed self-management and a group that performed pain-management using an electronic device. Check lists include pain, interference, jaw limitation, negative mood, and pain-related belief. As a result, in the group that proceeded with the cognitive behavioral approach, there was more improvement, and the improvement effect was significant in the psychological aspect. This study has proven that the cognitive behavioral approach based on self-monitoring through the device daily in TMD patients helps normalize the symptoms of TMD and jaw limitation and influences the psychological aspect [36]. However, the study discussed that a long-term follow-up is needed in the future and a high degree of patient participation is needed. In addition, it was expected that the device would be changed to be simple and convenient for users to solve it. Now, about 20 years later, with the development of smartphone-based electric devices and technologies, digital therapeutics are expected to be effective and as a basis for sufficiently applying to TMD.
According to a review by Minervini et al [34]., after covid-19, the incidence of TMD was higher due to emotional stress, and when 'Teledentistry' was applied, it was found to be effective as an adjunct to existing treatment. In addition, Salazar-Fernandez and colleagues [35] positively evaluated teledentistry and its effectiveness in patients with TMD. In addition, with the development of Internet of Things (IOT) technology and artificial intelligence (AI), digital therapeutics are expected to become more sophisticated.
3. Conclusion
Digital therapeutics are expected to cause a paradigm shift that will change the medical world in the future [37,38]. Although a lot of development and research is still needed, evidence-based studies have been published that prove a good effect in various diseases. Digital therapeutics can be effectively used in areas where behavior correction, self-monitoring, cognitive behavioral treatment, etc. must be applied or needed. In the field of dentistry or oral and maxillofacial region, there are patients with TMD that require this type of treatment. Psychosocial factors have been proven to be major factors in the cause and development of TMD. Clinicians need not only symptomatic treatment but also psychosocial and habitual approaches and active treatment. However, this aspect tends to be overlooked and difficult to access by most clinicians. However, with the introduction of digital therapeutics, intervention in the DC/TMD axis-II region in TMD patients is expected to become easier, and the development of the underlying technologies is also expected to help make application easier and simpler for patients. In the future, digital therapeutics have great potential to be used in the TMD field. Expectations for effectiveness can be evaluated positively when referring to previous and recent studies.
References
- Bahl, Shashi, et al. Telemedicine technologies for confronting COVID-19 pandemic: A review. Journal of Industrial Integration and Management 5 (2020): 547-561.
- Ghai, Suhani. Teledentistry during COVID-19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 14 (2020): 933-935.
- Rahman, Naomi, Nathwani S, et al. Teledentistry from a patient perspective during the coronavirus pandemic. British dental journal (2020): 1-4.
- Minervini, Giuseppe, et al. Teledentistry in the Management of Patients with Dental and Temporomandibular Disorders. BioMed Research International 2022 (2022).
- Dang, Amit, Arora D, et al. Role of digital therapeutics and the changing future of healthcare. Journal of Family Medicine and Primary Care 9 (2020): 2207.
- Abbadessa, Gianmarco, et al. Assessment of multiple sclerosis disability progression using a wearable biosensor: a pilot study. Journal of Clinical Medicine 10 (2021): 1160.
- Lavorgna, Luigi, et al. Disability assessment using Google Maps. Neurological Sciences 43 (2022): 1007-1014.
- Webb, Thomas, et al. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of medical Internet research 12 (2010): e1376.
- Hixon, Todd. Digital Therapeutics Have Huge Promise And They Are Real Today. Forbes (2016).
- Webb, Thomas, et al. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of medical Internet research 12 (2010): e1376.
- Cymerys, Ed, Sean D. Implementing USPSTF Recommendations on Behavioral Counseling for Cardiovascular Disease. Health Watch (2015).
- Pinto, Melissa D, et al. Assessing the critical parameters of eSMART-MH: a promising avatar-based digital therapeutic intervention to reduce depressive symptoms. Perspectives in psychiatric care 52 (2016): 157-168.
- Lorenzetti, Laura. This Company Is Tackling Diabetes With 'Digital Therapeutics. Fortune (2016).
- Elliott, William J, Izzo JL Jr. Device-guided breathing to lower blood pressure: case report and clinical overview. Medscape General Medicine 8 (2006): 23.
- Baum, Stephanie (30 April 2016). "Digitizing substance abuse treatment and recovery. Med City News (2016).
- Kario, Kazuomi, et al. A multicenter clinical trial to assess the efficacy of the digital therapeutics for essential hypertension: rationale and design of the HERB-DH1 trial. The Journal of Clinical Hypertension 22 (2020): 1713-1722.
- Kario, Kazuomi, et al. Efficacy of a digital therapeutics system in the management of essential hypertension: the HERB-DH1 pivotal trial. European heart journal 42 (2021): 4111-4122.
- Nordyke, Robert J, Appelbaum K, et al. Estimating the impact of novel digital therapeutics in type 2 diabetes and hypertension: health economic analysis. Journal of medical Internet research 21 (2019): e15814.
- Shuren J, Doraiswamy PM. Digital Therapeutics for MCI and Alzheimer’s disease: A Regulatory Perspective—Highlights From the Clinical Trials on Alzheimer ’s disease conference (CTAD). The Journal of Prevention of Alzheimer's Disease (2022): 1-5.
- Lipton, James, Ship J, et al. Estimated prevalence and distribution of reported orofacial pain in the United States. The Journal of the American Dental Association 124 (1993): 115-121.
- Ebrahimi M, Dashti H, Mehrabkhani M, et al. Temporomandibular Disorders and Related Factors in a Group of Iranian Adolescents: A Cross-sectional Survey. J. Dent. Res. Dent. Clin. Dent. Prospect 5 (2011): 123-127.
- Valesan LF, Da-Cas CD, Reus JC, et al. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral Investig (2021).
- Rollman GB, Gillespie JM. The role of psychosocial factors in temporomandibular disorders. Curr. Rev. Pain 4 (2000): 71-81.
- Auerbach SM, Laskin DM, Frantsve LM, et al. Depression, pain, exposure to stressful life events, and long-term outcomes in temporomandibular disorder patients. J. Oral Maxillofac. Surg 59 (2001): 628-633.
- Toh AQJ, Chan JLH, Leung YY. Mandibular asymmetry as a possible etiopathologic factor in temporomandibular disorder: A prospective cohort of 134 patients. Clin. Oral Investig (2021).
- Kim, Young-Kyun, et al. Clinical survey of the patients with temporomandibular joint disorders, using Research Diagnostic Criteria (Axis II) for TMD: preliminary study. Journal of Cranio-Maxillofacial Surgery 40 (2012): 366-372.
- Saccomanno S, Bernabei M, Scoppa F, et al. Coronavirus Lockdown as a Major Life Stressor: Does It Affect TMD Symptoms? Int. J. Environ. Res. Public Health 17 (2020): 8907.
- Medeiros RA, Vieira DL, Silva E, et al. Prevalence of symptoms of temporomandibular disorders, oral behaviors, anxiety, and depression in Dentistry students during the period of social isolation due to COVID-19. J.Appl. Oral Sci 28 (2020): e20200445.
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Groupdagger. J. Oral Facial Pain Headache 28 (2014): 6-27.
- Phillips K, Clauw DJ. Central pain mechanisms in chronic pain states—maybe it is all in their head. Best Pract Res Clin Rheumatol 25 (2011): 141-154.
- Velly AM, Look JO, Carlson C, et al. The effect of catastrophizing and depression on chronic pain a prospective cohort study of temporomandibular muscle and joint pain disorders. Pain 152 (2011): 2377-2383.
- Fillingim RB, Ohrbach R, Greenspan JD, et al. Psychological actors associated with development of TMD: the OPPERA prospective cohort study. J Pain 14 (2013): T75-90.
- Gatchel RJ, Stowell AW, Wildenstein L, et al. Efficacy of an early intervention for patients with acute temporomandibular disorder-related pain: a one-year outcome study. J Am Dent Assoc 137 (2006): 339-347.
- Durham J, Newton-John TRO, Zakrzewska JM. Temporomandibular disorders. BMJ 350 (2015): h1154.
- Minervini, Giuseppe, et al. Teledentistry in the Management of Patients with Dental and Temporomandibular Disorders. BioMed Research International 2022 (2022).
- Salazar-Fernandez CI, Herce J, Garcia-Palma A, et al. Telemedicine as an effective tool for the management of temporomandibular joint disorders. Journal of Oral and Maxillofacial Surgery 70 (2012): 295-301.
- Turner, Judith A, Mancl L, et al. Brief cognitive-behavioral therapy for temporomandibular disorder pain: effects on daily electronic outcome and process measures. Pain 117 (2005): 377-387.
- Park, Sang-Yoon. Teledentistry and Digital Therapeutics (DTx) for dentistry. Journal of Clinical Advances in Dentistry 6 (2022): 028-030.
