Digital Smile Design, Vast Bone Reduction with Surgical Guide and Intraoral Welding - A Case Report
Article Information
Adam Nowicki1, Karolina Osypko2*
1Diamante Clinica dental clinic, Sportowa 48 A/C, 59-300 Lubin, Poland
2Platinum Clinic, Ksiecia Witolda 49, 50-202 Wroclaw, Poland
*Corresponding Authors: Karolina Osypko, Platinum Clinic, Ksiecia Witolda 49, 50-202 Wroclaw, Poland
Received: 08 January 2024; Accepted 18 January 2024; Published: 30 January 2024
Citation: Adam Nowicki, Karolina Osypko. Digital Smile Design, Vast Bone Reduction with Surgical Guide and Intraoral Welding - A Case Report. Dental Research and Oral Health. 7 (2024): 15-22.
View / Download Pdf Share at FacebookAbstract
This case presents a whole treatment of a patient with residual dentition and poor esthetics due to the phenomenon of Godon. The planning of the treatment included conducting face scans, intraoral scans, extraoral photographs in smile and CBCT diagnostic. While the esthetics were as important to the patient as a function, Digital Smile Design was necessary to fulfill these expectations. New digital position of teeth arch dictated the position of the implants (6 in the maxilla and 4 in the mandible) and pointed to the need for bone reduction, as due to the phenomenon of Godon, the excessive bone volume would interfere with prosthetic restoration. Two triple, stacked surgical guides, for both maxilla and mandible, were designed and 3D-printed from dedicated resin. First guide was placed on residual teeth and determined the proper position of the second guide, which was pinned to the bone and served as both guide for alveolar bone reduction and as a base for the third guide for fully navigated implantation. Implants were immediately loaded after intraoral welding of titanium wire and creating a rigid frame for longterm temporary prosthetic reconstruction. After 6 months of healing, allceramic milled superstructures on a titanium anodized bar were delivered and the occlusion was checked with a dedicated electronic device. This case is unique for its fusion of DSD, guided bone reduction and immediate loading on a welded titanium frame, all planned from the very beginning due to proper diagnosis and potential of digital tools.
Keywords
Digital smile design, Bone reduction, Surgical guide, Computer-aided implantology, Intraoral welding, Immediate loading, 3D printing, Case report
Digital smile design articles; Bone reduction articles; Surgical guide articles; Computer-aided implantology articles; Intraoral welding articles; Immediate loading articles; 3D printing articles; Case report articles
Article Details
Introduction
Nowadays clinicians in their everyday practice have at their disposal many modern and digital tools to improve the outcome of the treatment. Occasionally, a patient’s situation is so challenging, that the default approach and standard treatment is highly inefficient (or even harmful) and all accessible options need to be gathered into one thoughtful and refined treatment plan to achieve success.
Patient Information and Clinical Findings
The 46-year-old patient was referred to the dental office due to the need for complex stomatognathic system rehabilitation.
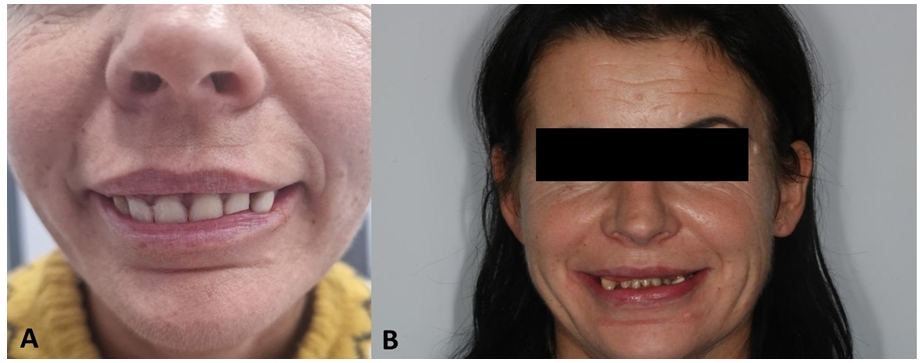
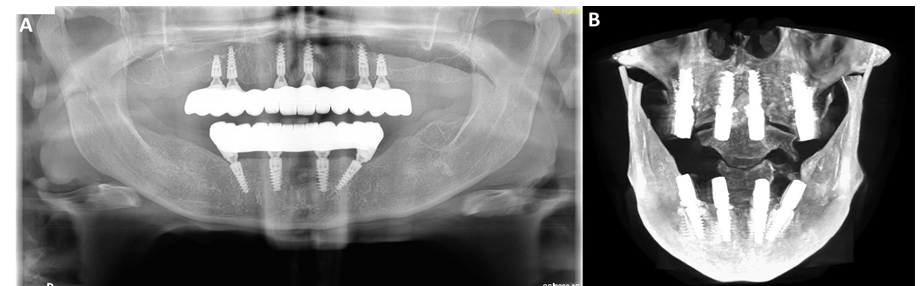
During intraoral examination, it was determined that the patient’s occlusion is a bilateral lingualized occlusion with a compensatory vertical growth of the alveolar process of the maxilla and mandible through the phenomenon of Godon (Figure 1A,B). The majority of remaining residual teeth were already extracted in another dental office.
Due to the lack of space for incisors in the neutral zone, the other office proceeded with removable partial prosthesis (Figure 1A), which did not improve the functions, and which also, via protrusive positioning of the upper incisors, suppressed lip contact, thus leading to the drying of the mucosa. Due to professional and social activity, the patient did not agree to temporary edentulism.
Therefore, it was decided to proceed with a one-day extraction protocol along with implantation and a long-lasting temporary treatment, then after osseointegration time to finish with the final work [1].
Therapeutic Intervention and Outcomes
Preparation
The decision regarding the treatment plan was made after preparing the project based on a CBCT, intraoral scans, and a facial scan.
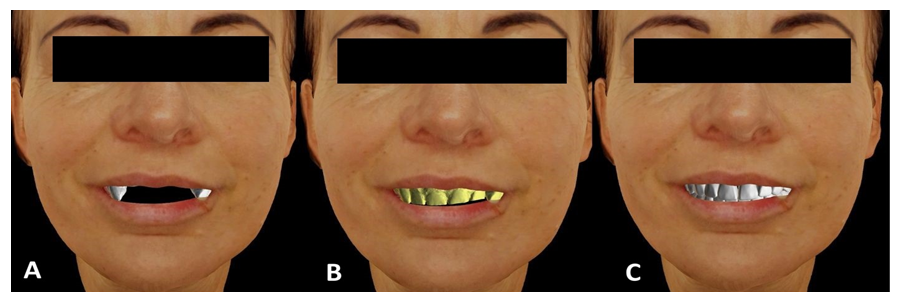
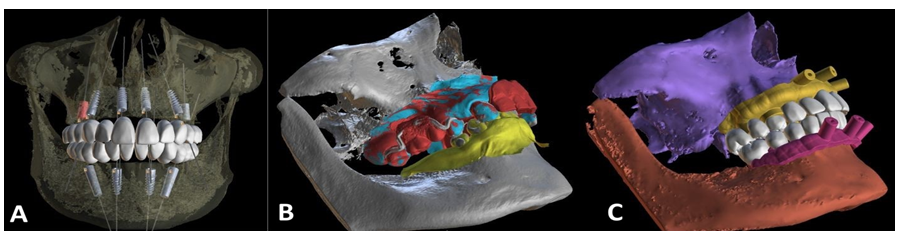
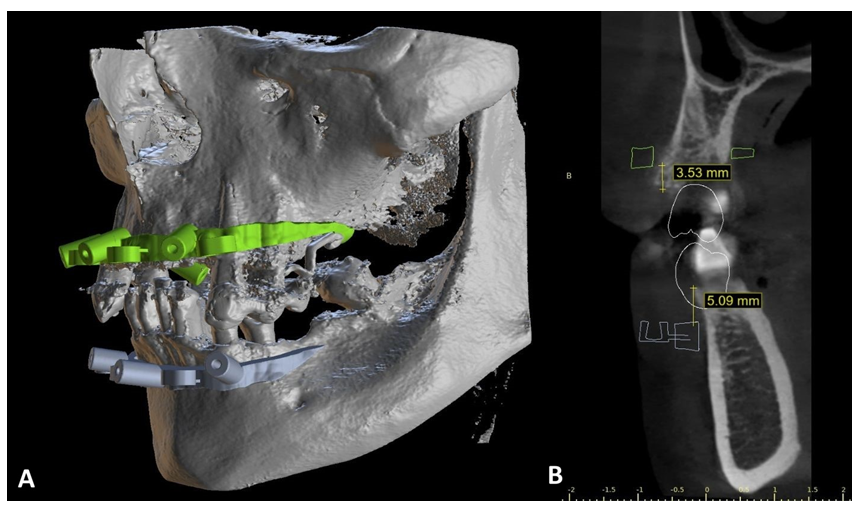
The following scans: intraoral, handled with the application of the Medit i500 scanner (Medit Corporation, Seoul, South Korea), as well as the facial scans (Figure 2A,B,C), handled with the application of the Bellus3D ARC facial scanner (Bellus3D, Campbell, California, USA), were assembled with the CBCT in the Blue Sky Bio software (Blue Sky Bio, LLC, Libertyville, IL, USA) (Figure 3A,B,C).
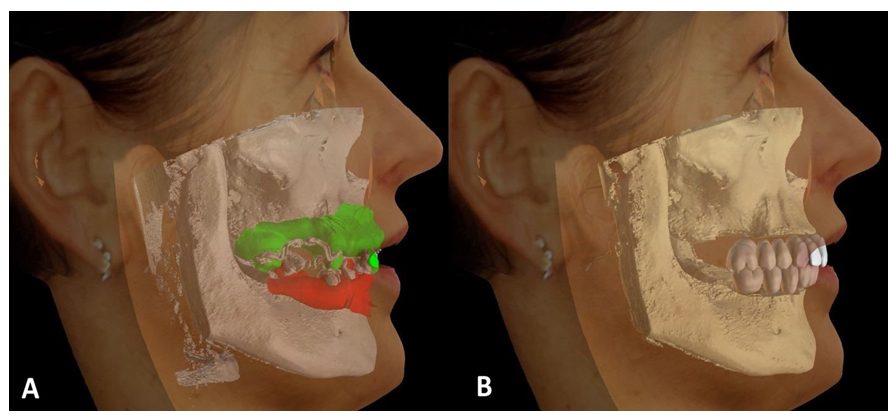
In compliance with the patient’s remarks regarding the esthetic sphere and the performed DSD diagnostics (Smile Designer Pro, Tasty Tech LTD., Toronto, Ontario, Canada), as well as relying on the application of the facial scan and Camper’s plane (established on facial scan’s basis), two new dental arches were designed (Figure 4A,B).
A digital bone reduction was conducted on the basis of the planned position of both arches, and subsequently, the implants planned in regions (FDI numbering system): 16, 14, 11, 21, 24, 26 and 32, 34 (tilted), 42, 44 (tilted) (Figure 3A).
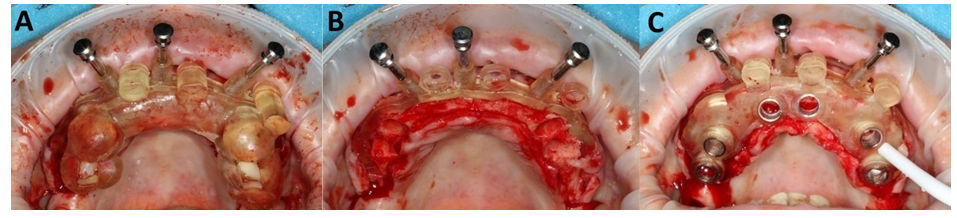
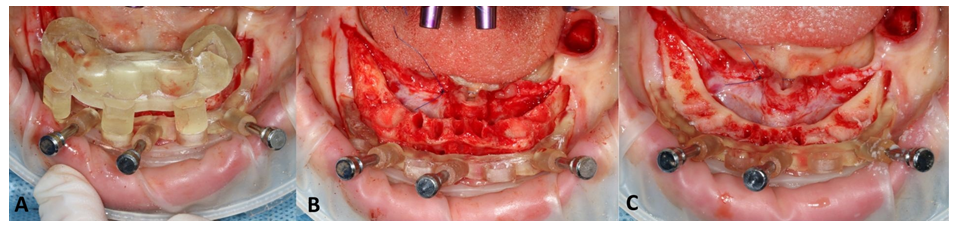
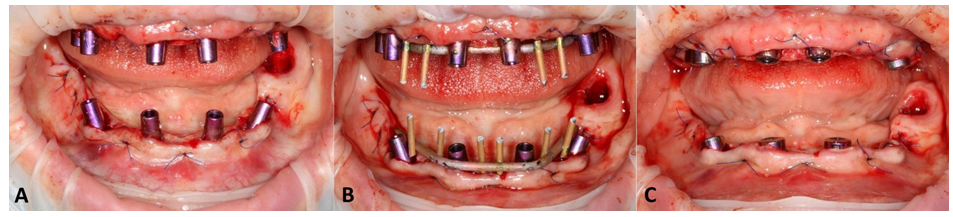
On the basis of the project design, a triple, stacked surgical guide with bone support for alveolar ridge osteotomy, as well as for fully navigated implantation was generated (Figure 5A,B,C; 6A,B,C).
Both, the project of the outer shell of both dental arches in long-term temporaries, as well as the division of surgical guides, were handled in the Meshmixer software (Meshmixer, Autodesk, Inc., ver:3.5.474, San Francisco, CA, USA). The stackable surgical guides and shells of both dental arches were printed on a 3D printer in DLP technology (Phrozen mini 8k, Phrozen Tech. Co., Ltd., Hsinchu City, Taiwan) with the Nextdent C&B bleach and Nextdent Base Light Pink resins (NextDent B.V., Soesterberg, The Netherlands).
Figure 3: Digital planning in Blue Sky Plan software on patient’s CBCT: with new teeth arches and implants’ positions (A), with intraoral scans of baseline maxilla (blue), mandible (yellow) and partial denture (red) (B) and planned teeth arches with surgical guides before separating into division(yellow and pink) (C).
Surgery & immediate loading
On the day of the treatment, the patient was given a local articaine + adrenaline anesthesia (40 mg + 0. 01 mg)/mL). A full-thickness mucosal flap was prepared on the bucco-labial and palatal sides, with the ligation of the soft tissues with a nylon 5-0 suture (Resorba Medical GmbH, Nürnberg, Germany). After placing the surgical guide on the top of the remaining teeth and on the bare bone, the lower guide (the bone reduction guide) was pinned (Figure 5A; 6A).
After detaching the upper part of the guide, all residual dentition was removed and the excessive bone was reduced to template level with the piezotome VarioSurg3 (NSK, Shinagawa City, Tokyo, Japan). About 2-5 mm in the maxilla and 5-7 mm in the mandible (Figure 6B,C; 7A,B). Next, the upper template (the third one) for fully guided implantation was placed on the pinned template with the use of connectors in order to conduct osteotomy and place the implants (Figure 5C).
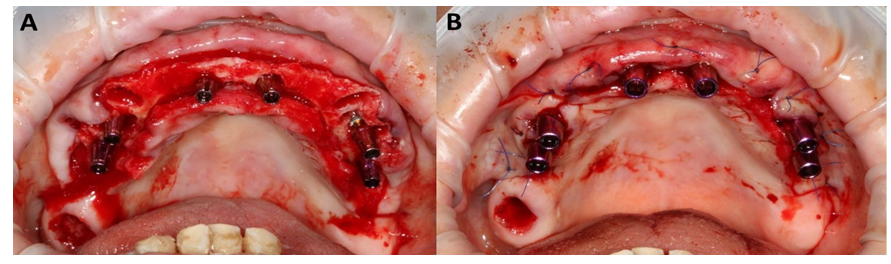
Both of the alveolar processes were provided with ROOTT implants (ROOTT, Trate Ag, Root, Switzerland) (Figure 8A). In the maxilla six were axially loaded and in the mandible four were placed, with the two outermost tilted (Figure 9A,B). The implants primary stability reached 45 Ncm which is above the required value of 30 Ncm [2].
Afterwards, the post-extraction sockets were filled with leukocyte- and platelet-rich fibrin (L-PRF, Intra-Lock, Boca Raton, FL, USA).
Multiunit abutments (MUA) were screwed to the implant platform. Due to philosophy of a one-day loading of the implants, straight AM abutment connectors were tightened to the MUAs (Figure 8B) and welded intraorally with a 2.0 titanium wire, thus creating a rigid titanium frame (Figure 10A,B,C).
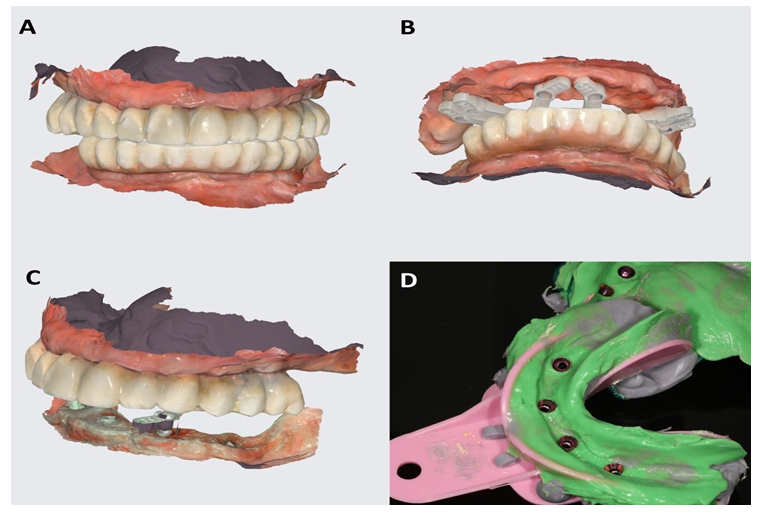
The next step was connecting the above-mentioned rigid structure with the 3D-printed shells of teeth arches in plane occlusal contacts [3] in order to obtain a long-term temporary solution with the reconstruction of the esthetics and functions for the period of osseointegration [4,5] (Figure 11A,B,C). The superstructure's intramucosal side was polished and other surfaces were glazed [6] (Optiglaze clear, GC International AG, Luzern, Switzerland).
Figure 5: Maxilla - intraoral photos of the triple, stacked surgical guide. First guide over the residual teeth connected via connectors with second, pinned guide (A); Second guide for bone reduction (B); Third guide for fully navigated implantation on the second one, also connected via connectors (C).
Figure 6: Mandible - also here intraoral photos of the triple, stacked surgical guide. First guide over the residual teeth connected via connectors with second, pinned guide (A); Second guide for bone reduction and with visible retracting suture of soft tissues from the lingual side (B); Situation after bone reduction with a new shape of the alveolar ridge (C).
Figure 10: Intraoral view of both arches: with AM abutments (A); after intraoral welding of titanium wire and creating rigid frame for long-lasting temporary reconstructions (B); healing abutments screwed in to MUAs’ to prevent soft tissues collapsing during the time of preparation and completing the temporary reconstructions (C).
Final reconstruction
After a 6-months healing period, radiological diagnostics was conducted (Carestream 8100 3D, Carestream Dental Germany GmbH, Stuttgart, Germany) (Figure 9A) and the long-temporary restoration was dismounted in order to assess the MUA tightening torque.
The original plan was to complete the case in a fully digital manner (Figure 12A,B,C), although due to:
- reduced basal seat area in the lower arch,
- impossibility to obtain a good-quality scan with the use of scan flags (Figure 12C) and
- debatable precision of intra-oral scanning in edentulism,
it was decided to implement both:
- traditional method - analog impressions on MUA level with the application of an open tray (Figure 12D) and
- digital method - 360° scan of the temporary superstructures along with the basal seat area (mucosa) as well as the emergence profile and interocclusal contacts’ record. Everything was done in coordinates.
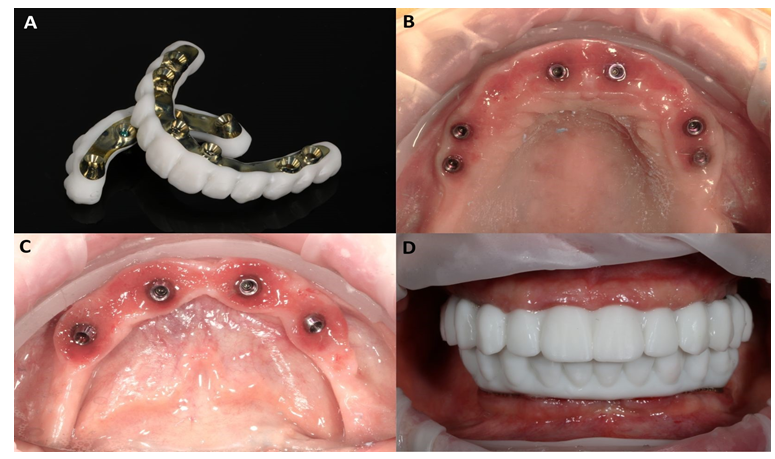
Due to the extensive scans, as well as to the undoubtedly residual scanflag scan, it was possible to connect the intraoral scans with the scan of the plaster model made from the impression. The spontaneous and intuitive overlapping of these structures was minimized, thus it was possible to create the passive 3D-printed superstructures for try-in (Figure 13A,B,C,D).
During the try-in of the printed superstructures with a titanium bar in the patient's mouth (Figure 13D) the passiveness was checked via a Sheffield test. Furthermore, it was also confirmed with a passive fitting of the printed-welded temporaries on a plaster model [7]. Minimal intercuspation modifications were made and marked with a color flow-type composite in order to illustrate them for the technical laboratory.
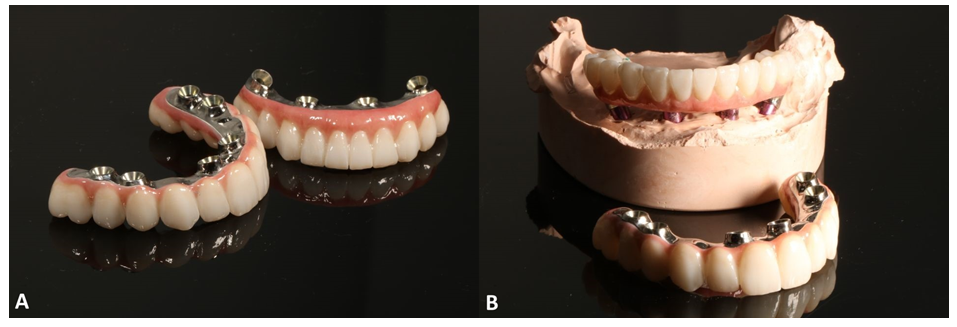
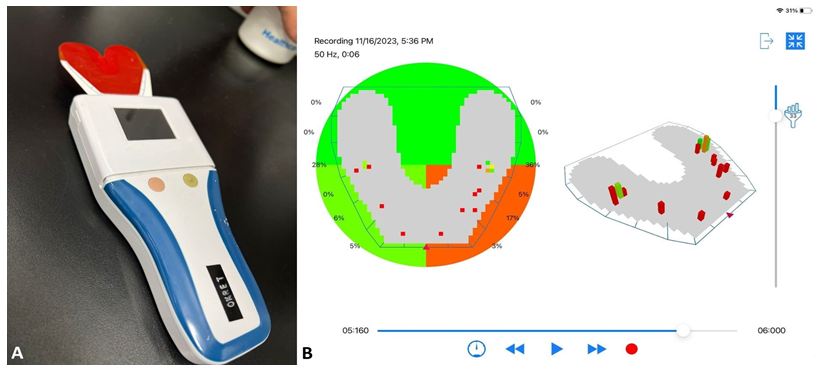
The last stage of the treatment was the delivery of the all-ceramic milled superstructures mounted in the technical laboratory onto a titanium anodized bar [8] (Figure 14A,B). The equilibration of the above-mentioned full-arch prosthetic restorations in static and dynamic occlusion was conducted with the articulating papers and digital pressure meter OccluSense (Baush, Germany GmbH, Hainspitz, Germany) (Figure 15A,B). It was also assured that the dynamic occlusion follows the given pattern of a bilaterally balanced occlusion in dynamics [9,10]. The final outcome was highly satisfactory for the patient (Figure 16).
Figure 12: After the 6-months of osseointegration period, the long-term temporaries were scanned (A); the scan of the maxilla for final reconstruction was conducted with scanflags (B), while the in the mandible the scan by itself was insufficient (C) and the traditional impression had to be taken to guarantee the passiveness and precision of the final reconstruction (D).
Figure 13: Preparation for the final reconstruction - a 3D-printed superstructure with a titanium bar (A) created to check the passiveness of the bar; healed mucosa with MUA in maxilla (B) and mandible (C) and after try-in in the mouth (D). At this point the color of the teeth is irrelevant, as it was only made for the purpose of passiveness check up.
Discussion
Complex cases of full-mouth rehabilitation with high esthetic requirements may challenge the clinicians into implementing all existing digital solutions to gain the best possible outcome.
In this case, the patient’s biggest concern was an esthetic issue, which set high standards and guided the rest of the therapeutic workflow. The decision to conduct Digital Smile Design was dictated due to the possibility to better communicate with the patient and fulfill her esthetic needs on both stages of a long-term temporary restoration and a final restoration [11]. Missing this step would led to placing implants in surgically right though prosthetically wrong positions and would create an unmanageable final situation.
DSD
While digital smile design typically refers to restorative dentistry and prosthetic reconstructions on teeth [11], there are only a few studies [12-16] showing DSD combined with immediate loading on implants.
Moreover, at this moment (December 2023) there are only three reported cases [17-19] where additional bone reduction was needed.
In the study by Todaro et al. similarly authors used face scans to establish an ideal teeth position in the prosthetic reconstruction [17]. However, the immediate temporary was a denture (3D printed) without intraoral welding and only the mandible was treated, so the occlusion could be adjusted to maxilla. Moreover, the surgical guide for ostectomy was “closed”, as the fissure in the guide dictated the path of the piezosurgical tip. This potentially could impair the cooling of the bone and be prone to overheating.
In the study by Costa et al. small magnets were used to connect two surgical guides. Similarly as in the previously mentioned study, the temporary prosthesis (from PMMA) was glued in the abutments without intraoral welding. In our case, surgical guides were connected with “connectors” (in a fitting die and counter-die shape) which seems to be cheaper and less complex to manufacture than guides with magnets [18].
In the study by Wang et al. the new bone level has been marked with a few drilled points made with a guide [19]. The bone reduction was conducted using a manual tool (Bone Rongeur). and the burs were only used to smoothen the surface. In that study the bone reduction was limited only to a few particular spots, not in the whole alveolar ridge.
Bone reduction
The “bone reduction” or “alveolar ridge ostectomy” is usually conducted in cases when the bone level of the alveolar ridge is uneven or when the ideal implant position is so deep that an excessive bone volume may interfere with the range of desired prosthetic reconstruction [20]. The surgical guide improves the predictability of the whole procedure (not only bone reduction), reduces the time of the operation and increases the precision of ostectomy, while making it safer for the patient [21].
Some early cases of bone reduction included gutta-percha radiological markers and marking the ostectomy level on the bone surface with a pencil [22]. Fortunately, modern technologies such as the CAD-CAM approach and desktop 3D-printers allow us to create surgical guides specifically for the bone reduction procedure.
In this case, two (one for maxilla and one for mandible) triple stacked surgical guides have been used, both immobilized by pins in order to guarantee stillness of the guide during the operation.
Both of the triple stacked surgical guides consisted of:
- The first guide which surrounded the remaining teeth for unambiguous position.
- The second guide in a shape of a frame, which was pinned to the bone and served as a guide for bone reduction and base for the third guide.
- The third guide which served as a classical implantation guide in full navigation.
As mentioned earlier, the DSD indicated the ideal position of implants, which subsequently unveiled the need for bone reduction, in mean dimensions 3,5 mm in the maxilla and 6 mm in the mandible.
While planning the bone reduction volume, it was meant to ensure implant placement 2 mm subcrestally [23,24] and 4-6 mm below the free gingiva margin (depending on the shape of the margin and presence of papilla) in order to maintain the soft tissue thickness at least 3 mm [25], as proper soft tissue thickness contributes to the stability of the bone level and minimizes the risk of implant loss [26,27].
In simpler cases of minor bone reduction it can be done from free hand, without surgical guide, as presented by Vizcaya [28], while in other cases even the dynamic navigation may be applied [29].
In the case of such vast bone reduction as presented in this study, without the surgical guide the surgeon might have easily lost orientation and cut out excessive or insufficient bone volume, which would have led to subsequent poor esthetic outcome.
While full arch implantations with immediate loading and intraoral welding is commonly known and practiced technique, the combination of all of these elements with bone reduction based on DSD and face scans have never been described in the literature.
Full-digital protocol
Although in the described case, the final long-term mandible restoration was done combining digital and traditional way due to difficulties with scanning the mandible for the intra-oral scanner to work properly, a full-digital workflow is perfectly possible in this and in similar cases [18,30].
Occlusion
During designing the case the minimisation of the cantilever was planned. With the use of Occlusense the balanced occlusion was checked and there was a strive for minimal overbite. Relatively flat cusps were used to lower inclination of cuspal planes not exceeding the inclination of condylar path.
Conclusions
Some cases may require only basic surgical and prosthetic skills, while others, such as presented above, must combine complex approaches in order to achieve rewarding results. This case shows a unique combination of advanced technological amenities, such as DSD, face scans, digital planning of the surgery (on many levels) and designing and manufacturing prosthetic reconstructions which allowed a difficult treatment to succeed. While the sole topic of bone reduction is commonly known and practiced, now with surgical guides its process can be more predictable, safe and faster than with any other traditional method.
Abbreviations
CAD-CAM - Computer Aided Design-Computer Aided Manufacturing
CBCT - Cone Beam Computed Tomography
DSD - Digital Smile Design
IOS - Intra Oral Scan
MUA - Multiunit abutment
OPG - orthopantomogram
Author contributions
A.N.: conceptualization; methodology; software; validation; formal analysis; writing—original draft preparation; writing—review and editing; supervision. K.O.: validation; formal analysis; data curation; writing—original draft preparation; writing—review and editing; visualization; supervision; project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical approval for this study was not required according to the rules of Komisja Bioetyczna przy Uniwersytecie Medycznym we Wroclawiu because the study was not a medical experiment, only a comprehensible summary of different treatment options already existing and scientifically proven.
Informed consent statement
Informed consent was obtained from all subjects involved in the study.
Data availability statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy isuues.
Acknowledgments
We would like to thank our patient, as he agreed to the whole photographic documentation of the conducted procedures and their publication for scientific purposes. Moreover, we would like to thank the Cadman laboratory for professionally manufacturing the final restoration.
Conflicts of interest
The authors declare no conflicts of interest.
References
- Del Fabbro M, Testori T, Kekovic V, et al. A systematic review of survival rates of osseointegrated implants in fully and partially edentulous patients following immediate loading. J Clin Med 8 (2019).
- Slutzkey GS, Cohen O, Chaushu L, et al. Immediate Maxillary Full-Arch Rehabilitation of Periodontal Patients with Terminal Dentition Using Tilted Implants and Bone Augmentation: A 5-Year Retrospective Cohort Study. J Clin Med 11 (2022).
- Marconcini S, Giammarinaro E, Covani U, et al. Immediate restoration of fixed full-arch prostheses placed on implants in both fresh and healed sockets using the flat one-bridge technique: a 7-year retrospective study. BMC Oral Health 21 (2021): 617.
- Degidi M, Nardi D, Piattelli A. A six-year follow-up of full-arch immediate restorations fabricated with an intraoral welding technique. Implant Dent 22 (2013): 224-231.
- Albiero AM, Benato R, Benato A, et al. Use of Intraoral Welding to Increase the Predictability of Immediately Loaded Computer-Guided Implants. Int J Periodontics Restorative Dent 37 (2017): 591-598.
- Mazurek-Popczyk J, Nowicki A, Arkusz K, et al. Evaluation of biofilm formation on acrylic resins used to fabricate dental temporary restorations with the use of 3D printing technology. BMC Oral Health 22 (2022): 442.
- Buzayan MM, Yunus NB. Passive Fit in Screw Retained Multi-unit Implant Prosthesis Understanding and Achieving: A Review of the Literature. J Indian Prosthodont Soc 14 (2014): 16-23.
- Scarano A, Stoppaccioli M, Casolino T. Zirconia crowns cemented on titanium bars using CAD/CAM: a five-year follow-up prospective clinical study of 9 patients. BMC Oral Health 19 (2019): 286.
- Wismeijer D, Van Waas MA, Kalk W. Factors to consider in selecting an occlusal concept for patients with implants in the edentulous mandible. J Prosthet Dent 74 (1995): 380-384.
- Rangarajan V, Yogesh PB, Gajapathi B, et al. Concepts of occlusion in prosthodontics: A literature review, part II. J Indian Prosthodont Soc 16 (2016): 8-14.
- Thomas PA, Krishnamoorthi D, Mohan J, et al. Digital Smile Design. J Pharm Bioallied Sci 14 (2022): S43-S49.
- Haider KG. Digital smile design, guided surgery, delivering facial driven implant treatment in A failed dentition: case reports. OJDOH 1 (2018): 56.
- Cattoni F, Chirico L, Merlone A, et al. Digital Smile Designed Computer-Aided Surgery versus Traditional Workflow in “All on Four” Rehabilitations: A Randomized Clinical Trial with 4-Years Follow-Up. Int J Environ Res Public Health 18 (2021): 62.
- Coachman C, Calamita MA, Coachman FG, et al. Facially generated and cephalometric guided 3D digital design for complete mouth implant rehabilitation: A clinical report. J Prosthet Dent 117 (2017): 577-586.
- Lerner H, Hauschild U, Sader R, et al. Complete-arch fixed reconstruction by means of guided surgery and immediate loading: a retrospective clinical study on 12 patients with 1 year of follow-up. BMC Oral Health 20 (2020): 15.
- Creagh J, Bohner L, Sesma N, et al. Integrating a facially driven treatment planning to the digital workflow for rehabilitation of edentulous arches: A case report. J Contemp Dent Pract 21 (2020): 1393-1397.
- Todaro C, Cerri M, Isola G, et al. Computer-Guided Osteotomy with Simultaneous Implant Placement and Immediately Loaded Full-Arch Fixed Restoration: A Case Report. Prosthesis 5 (2023): 221-233.
- Costa AJ de M, Teixeira Neto AD, Burgoa S, et al. Fully Digital Workflow with Magnetically Connected Guides for Full-Arch Implant Rehabilitation Following Guided Alveolar Ridge Reduction. J Prosthodont 29 (2020): 272-276.
- Wang J, Fang M, Xin H, et al. Use of a digitally guided triple technique for bone reduction, implant placement, and immediate interim prostheses in complete-arch implant surgery. J Prosthet Dent 127 (2022): 703-708.
- Mijiritsky E, Ben ZH, Shacham M, et al. Variety of surgical guides and protocols for bone reduction prior to implant placement: A narrative review. Int J Environ Res Public Health 18 (2021): 91.
- Alzoubi F, Massoomi N, Nattestad A. Bone reduction to facilitate immediate implant placement and loading using CAD/CAM surgical guides for patients with terminal dentition. J Oral Implantol 42 (2016): 406-410.
- Bidra AS. Technique for systematic bone reduction for fixed implant-supported prosthesis in the edentulous maxilla. J Prosthet Dent 113 (2015): 520-523.
- Valles C, Rodríguez-Ciurana X, Clementini M, et al. Influence of subcrestal implant placement compared with equicrestal position on the peri-implant hard and soft tissues around platform-switched implants: a systematic review and meta-analysis. Clin Oral Investig 22 (2018): 555-570.
- Koh RU, Oh TJ, Rudek I, et al. Hard and soft tissue changes after crestal and subcrestal immediate implant placement. J Periodontol 82 (2011): 1112-1120.
- Tomasi C, Tessarolo F, Caola I, et al. Morphogenesis of peri-implant mucosa revisited: an experimental study in humans. Clin Oral Implants Res 25 (2014): 997-1003.
- Tavelli L, Barootchi S, Avila-Ortiz G, et al. Peri-implant soft tissue phenotype modification and its impact on peri-implant health: A systematic review and network meta-analysis. J Periodontol 92 (2021): 21-44.
- Linkevicius T, Apse P, Grybauskas S, et al. Influence of thin mucosal tissues on crestal bone stability around implants with platform switching: a 1-year pilot study. J Oral Maxillofac Surg 68 (2010): 2272-2277.
- Rojas-Vizcaya F. Prosthetically guided bone sculpturing for a maxillary complete-arch implant-supported monolithic zirconia fixed prosthesis based on a digital smile design: A clinical report. J Prosthet Dent 118 (2017): 575-580.
- Magic M, Wang F, Fan S, et al. Dynamic navigation guidance for bone reduction in maxilla: case report. Int J Oral Maxillofac Implants 36 (2021): Ie1-e6.
- Nowicki A, Osypko K. Digital Workflow in Full Mouth Rehabilitation with Immediate Loading, Intraoral Welding and 3D-Printed Reconstructions in a Periodontal Patient: A Case Report. Reports 6 (2023): 52.