Dietary and Medication Management Followed by Metabolic Disorders at the NIPH of Abidjan
Article Information
Kouakou Affoué Valérie1, Gbakayoro Jean-Brice1*, Koné Mohamed Ba2, Tano Kablan3, Aké Odile4, Brou Kouakou1
1Laboratory of Nutrition and Food Safety, UFR Science and Food Technology, Nangui Abrogoua University, Abidjan, Côte d’Ivoire
2UFR of forest and environmental agronomic engineering, Man University, Côte d’Ivoire
3Laboratory of Food Biochemistry and Tropical Products Technology, UFR Science and Food Technology, Nangui Abrogoua University, Abidjan, Ivory Coast
4Nutrition Service, National Institute of Public Health, Abidjan, Côte d’Ivoire
*Corresponding Author: Gbakayoro Jean-Brice, Laboratory of Nutrition and Food Safety, UFR Science and Food Technology, Nangui Abrogoua University 02 BP 801 Abidjan 02, Côte d’Ivoire
Received: 29 July 2019; Accepted: 14 August 2019; Published: 28 August 2019
Citation:
Kouakou Affoué Valérie, Gbakayoro Jean-Brice, Koné Mohamed Ba, Tano Kablan, Aké Odile, Brou Kouakou. Dietary and Medication Management Followed by Metabolic Disorders at the NIPH of Abidjan. Journal of Food Science and Nutrition Research 2 (2019): 188-198.
View / Download Pdf Share at FacebookAbstract
Drug, diet prescriptions and regular physical activity are the main recommendations followed by patients in the management of metabolic diseases, including diabetes, high blood pressure and obesity .The objective of this work was to determine the impact of the follow -up of these recommendations by patients followed at NIPH (National Institute of Public Health) of Abidjan. For this purpose, the socio-economic, management characteristics of patients, morpho-anthropometric, metabolic and biological parameters and the evolution of these parameters during the treatment of the patients were determined. The results Showed a predominance of women (58.1%) and of people over 40 (77.66%), affected by metabolic diseases in this health center. In addition, the majority of patients had a family history (54.35%), a high weight (52% with a BMI>30) and a large waist circumference (52.1% of men with WC>102 cm and ± 88.8% of women with WC>88 cm). The prescriptions had the effect of balancing the follow-up indicators by lowering the morpho-anthropometric (BMI, waist circumference), biological (blood sugar, blood pressure) and serum lipid and protein parameters.
Keywords
Dietary prescription, Metabolic disease, Control status
Dietary prescription articles, Metabolic disease articles, Control status articles
Dietary prescription articles Dietary prescription Research articles Dietary prescription review articles Dietary prescription PubMed articles Dietary prescription PubMed Central articles Dietary prescription 2023 articles Dietary prescription 2024 articles Dietary prescription Scopus articles Dietary prescription impact factor journals Dietary prescription Scopus journals Dietary prescription PubMed journals Dietary prescription medical journals Dietary prescription free journals Dietary prescription best journals Dietary prescription top journals Dietary prescription free medical journals Dietary prescription famous journals Dietary prescription Google Scholar indexed journals Metabolic disease articles Metabolic disease Research articles Metabolic disease review articles Metabolic disease PubMed articles Metabolic disease PubMed Central articles Metabolic disease 2023 articles Metabolic disease 2024 articles Metabolic disease Scopus articles Metabolic disease impact factor journals Metabolic disease Scopus journals Metabolic disease PubMed journals Metabolic disease medical journals Metabolic disease free journals Metabolic disease best journals Metabolic disease top journals Metabolic disease free medical journals Metabolic disease famous journals Metabolic disease Google Scholar indexed journals Control status articles Control status Research articles Control status review articles Control status PubMed articles Control status PubMed Central articles Control status 2023 articles Control status 2024 articles Control status Scopus articles Control status impact factor journals Control status Scopus journals Control status PubMed journals Control status medical journals Control status free journals Control status best journals Control status top journals Control status free medical journals Control status famous journals Control status Google Scholar indexed journals National Institute of Public Health articles National Institute of Public Health Research articles National Institute of Public Health review articles National Institute of Public Health PubMed articles National Institute of Public Health PubMed Central articles National Institute of Public Health 2023 articles National Institute of Public Health 2024 articles National Institute of Public Health Scopus articles National Institute of Public Health impact factor journals National Institute of Public Health Scopus journals National Institute of Public Health PubMed journals National Institute of Public Health medical journals National Institute of Public Health free journals National Institute of Public Health best journals National Institute of Public Health top journals National Institute of Public Health free medical journals National Institute of Public Health famous journals National Institute of Public Health Google Scholar indexed journals metabolic diseases articles metabolic diseases Research articles metabolic diseases review articles metabolic diseases PubMed articles metabolic diseases PubMed Central articles metabolic diseases 2023 articles metabolic diseases 2024 articles metabolic diseases Scopus articles metabolic diseases impact factor journals metabolic diseases Scopus journals metabolic diseases PubMed journals metabolic diseases medical journals metabolic diseases free journals metabolic diseases best journals metabolic diseases top journals metabolic diseases free medical journals metabolic diseases famous journals metabolic diseases Google Scholar indexed journals chronic diseases articles chronic diseases Research articles chronic diseases review articles chronic diseases PubMed articles chronic diseases PubMed Central articles chronic diseases 2023 articles chronic diseases 2024 articles chronic diseases Scopus articles chronic diseases impact factor journals chronic diseases Scopus journals chronic diseases PubMed journals chronic diseases medical journals chronic diseases free journals chronic diseases best journals chronic diseases top journals chronic diseases free medical journals chronic diseases famous journals chronic diseases Google Scholar indexed journals therapeutic strategy articles therapeutic strategy Research articles therapeutic strategy review articles therapeutic strategy PubMed articles therapeutic strategy PubMed Central articles therapeutic strategy 2023 articles therapeutic strategy 2024 articles therapeutic strategy Scopus articles therapeutic strategy impact factor journals therapeutic strategy Scopus journals therapeutic strategy PubMed journals therapeutic strategy medical journals therapeutic strategy free journals therapeutic strategy best journals therapeutic strategy top journals therapeutic strategy free medical journals therapeutic strategy famous journals therapeutic strategy Google Scholar indexed journals diabetic patients articles diabetic patients Research articles diabetic patients review articles diabetic patients PubMed articles diabetic patients PubMed Central articles diabetic patients 2023 articles diabetic patients 2024 articles diabetic patients Scopus articles diabetic patients impact factor journals diabetic patients Scopus journals diabetic patients PubMed journals diabetic patients medical journals diabetic patients free journals diabetic patients best journals diabetic patients top journals diabetic patients free medical journals diabetic patients famous journals diabetic patients Google Scholar indexed journals hypertensive patients articles hypertensive patients Research articles hypertensive patients review articles hypertensive patients PubMed articles hypertensive patients PubMed Central articles hypertensive patients 2023 articles hypertensive patients 2024 articles hypertensive patients Scopus articles hypertensive patients impact factor journals hypertensive patients Scopus journals hypertensive patients PubMed journals hypertensive patients medical journals hypertensive patients free journals hypertensive patients best journals hypertensive patients top journals hypertensive patients free medical journals hypertensive patients famous journals hypertensive patients Google Scholar indexed journals
Article Details
1. Introduction
“Non-communicable” metabolic diseases are conditions that are not caused by a particular pathogen and are therefore “non-communicable”. They are thus distinguished from so-called “transmissible” infectious diseases. These are long-term conditions, which generally evolve slowly, hence their name “chronic diseases”. These diseases are the leading causes of death worldwide, killing more people each year than all diseases combined [1]. The death toll of these diseases is increasing rapidly worldwide. In 2001, these diseases accounted for about 60% of all deaths worldwide. Almost half of all deaths from metabolic diseases are due to cardiovascular disease, obesity and diabetes. These diseases also follow a worryingly increasing trend not only because they already affect a large proportion of the population, but also because they now appear earlier in patients' lives. Nearly 80% of deaths from these diseases occur in low- and middle-income countries [2], notably in Africa and particularly in Côte d'Ivoire, with a prevalence that was estimated at 5.7% in 1979 [3].
Therapeutic strategies for the management of these diseases include drug prescriptions, dietary prescriptions and encouraging regular physical activity. However, dietary prescriptions, also known as “diets”, remain the cornerstone of the therapeutic strategy, particularly in the absence of complications. Unfortunately, more and more, for various reasons (lack of resources, ignorance, etc.), patients followed for these pathologies do not strictly comply with all these prescriptions. This leads to a mixed balance of metabolic tracking markers. The objective of this work was to determine the evolution of morpho-anthropometric, metabolic and biological parameters of patients monitored at the NIPH (National Institute of Public Health), Abidjan's reference center for the management of certain metabolic diseases (diabetes, obesity). To this end, these parameters were recorded as soon as they were entered and during their periodic monitoring inspections.
2. Material and Methods
2.1 Type of study
A prospective descriptive study was carried out during this work. It consisted in determining the characteristics of diabetic patients and obese adult patients based on the analysis of their records.
2.2 Study period
Records of new patients registered from January 1 to December 31, 2017 were taken into account for this study.
2.3 Study site
The study was conducted at the Anti-Diabetic Centre of Abidjan (ADCA) for diabetic patients and at the Adult Nutrition Service (ANS) for obese patients. These services are located within the National Institute of Public Health (NIPH) in the municipality of Adjamé, in Abidjan, Côte d'Ivoire.
2.4 Criteria for selecting files
2.4.1 Inclusion criteria: For this study, the properly informed records of diabetic, obese and hypertensive patients followed were taken into account.
2.4.2 Criteria for non-inclusion: Records of diabetic, obese and hypertensive patients not monitored in these 2 departments, those of patients who stopped treatment for a period of time, duplicate records and unusable records were not admitted for this study.
2.5 Study variables
Before being reported in the file, the weight (W), in kg, was determined by a bathroom scale; the height (H), in meters by a height gauge or taken from the identity document, the waist circumference (WC), in cm at the umbilical level and in standing position, by a tape measure. The body mass index (BMI) was obtained by the ratio of weight to height square (BMI=W/H2). Blood pressure (BP), in mm Hg, was measured by an electronic blood pressure monitor after a 10 minute rest. Blood sugar in mmol/l, serum lipids (Triglycerides, total cholesterol, HDL-Chol), serum proteins (uric acid, urea and creatinine) were determined by a biological blood test in fasting patients.
2.6 Evolution of morpho-anthropometric and metabolic parameters
This evolution was measured by comparing the morpho-anthropometric and metabolic parameters of patients on arrival and those obtained at the various control appointments scheduled on average every 3 months. The following scales of evolution have been affected: (i) Decrease, when the values obtained during the control appointments move from a higher to a lower level of severity according to the indicated parameter; (ii) Stabilization, when the values obtained during the control appointments increase or decrease but not significantly and remain at the same level of severity according to the indicated parameter; (iii) Increase, when the values obtained during the control appointments increase and move to a level of severity higher than the level at the patient input, according to the indicated parameter.
2.7 Statistical analysis
Data analysis was performed using Excel 2007 software. For comparison, Fisher's chi-square was used with a significance level of p <0.05.
3. Results and Discussion
3.1 Results
3.1.1 Socio-economic characteristics of patients: The majority of patients cared for in these centers belonged to the Akan ethnic group (49.24% of diabetics and 46% of obese), were female (58.1% of diabetics and 85.2% of obese), were between 41 and 59 years of age (50% of diabetics and 49.8% of obese), resided in Abidjan (80.04% of diabetics and 83.2% of obese) and were private agents (53.56% of diabetics and 72.8% of obese) (Table 1).
3.1.2 Characteristics of patient care: The reasons for consultation were specific to each pathology. They were often for reasons of diabetes management (69.16%) or diabetes combined with hyper tension (30.84%), weight loss (76.8%) or any other reason related to poor metabolic parameters (23.2%). The majority of diabetic patients had no family history of diabetes (54.35%) and those with diabetes had much more than one known relative with 1st degree diabetes (27.47%). However, most obese patients had no family history of obesity or other pathologies, with much more, a 1st degree relative affected by the pathology (54%). The types of treatment received by patients were much more drug treatments (91%) for diabetic patients (ADO or insulin or ADO + Insulin) or a combination of a drug prescription, a dietary prescription and regular physical activity for obese patients (Table 2).
3.1.3 Morpho-anthropometric and metabolic characteristics of diabetic patients: The majority of patients (52%) were overweight (27.6% overweight and 24.4% obese), had a high waist circumference (19.8% of men with a waist circumference greater than 102 cm and 74.2% of women with a waist circumference greater than 88 cm), normal blood pressure (47.6%) and hyperglycemia (96.5% with blood glucose greater than 1.1 g/l) (Figure 1). Their serum lipid levels were generally normal (72% with triglycerides below 1.5 g/l, 58.4% with total cholesterol below 2 g/l. 52.8% with HDL cholesterol above 0.5 g/l) and their serum protein levels also normal over all (91.3% with uric acid levels below 70 g/l, 96.7% with urea levels below 0.4 g/l. 80% with creatinine levels below 12 g/l) (Figure 2). However, a significant fringe of patients have abnormal values for these studied parameters.
3.1.4 Morpho-anthropometric and metabolic characteristics of obese patients: The vast majority of patients followed (97%) were overweight (15.2% overweight and 81.8% obese), had a high waist circumference (52.1% of men with a waist circumference greater than 102 cm and 88.8% of women with a waist circumference greater than 88 cm), normal blood pressure (53%) and normal blood sugar (94.6% with blood glucose levels between 0.7 and 1.1 g/l) (Figure 3). Their serum lipid levels were generally normal (90.2% with triglycerides below 1.5 g/l, 51.4% with total cholesterol below 2 g/l, 64.4% with HDL cholesterol above 0.5 g/l) and their serum protein levels also normal over all (84% with uric acid levels below 70 g/l, 96.4% with urea levels below 0.4 g/l. 89.4% with creatinine levels below 12 g/l) (Figure 4).
3.1.5 Evolution of morpho-anthropometric and metabolic parameters: In general, for diabetic patients, the treatments resulted in a decrease in morphoanthropometric parameters in some patients (BMI and WC decreased for 22% and 41% of patients respectively), a decrease in BP (66% of patients) and a decrease in blood sugar (72% of patients). Also, these treatments resulted in a stabilization of serum proteins and lipids (stabilization of TG, TC, HDL-C, Ac. uriq, creatine from 85 to 92% of patients) that remained at normal values in patients during treatment (Table III). In obese patients, these treatments also resulted in a stabilization of biological par ameters (BP, blood sugar), serum lipids and proteins, which were at normal values in these patients during treatment. These treatments have mainly had the effect of lowering in particular the anthropometric morpho parameters (BMI and WC decreases for 70% and 34% of patients respectively).
Table 1: Socio-economic characteristics of patients.
HTA-Hypertension; ADO-Anti Diabetic Oral; Diet P-Dietary Prescription; PA-Physical Activity; Drug P-Drug Prescription
Table 2: Characteristics of patient care.
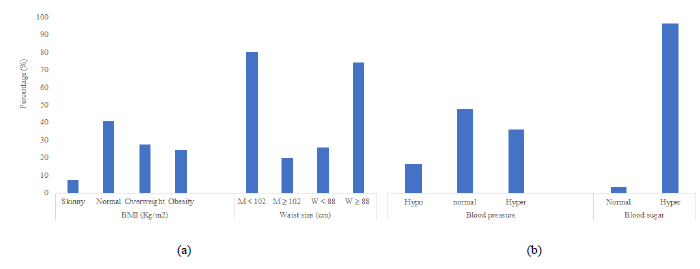
Figure 1: Anthropometric and biological parameters of diabetic patients (M-Man; W-Woman) (a) BMI and waist circumference; (b) Blood pressure and blood glucose.
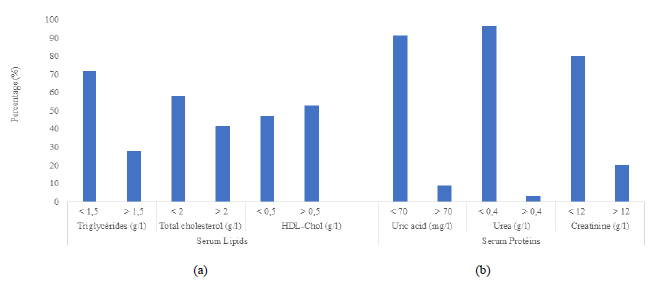
Figure 2: Serum Lipids and proteins of diabetic patients; (a) Serum lipids; (b) Serum proteins.
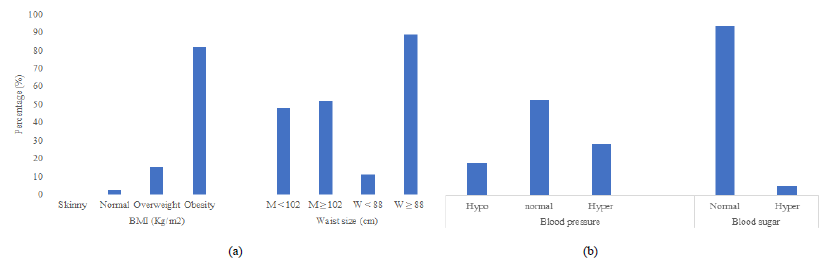
Figure 3: Anthropometric and biological parameters of obese patients (M-Man; W-Woman); (a) BMI and waist circumference; (b) Blood pressure and blood glucose.
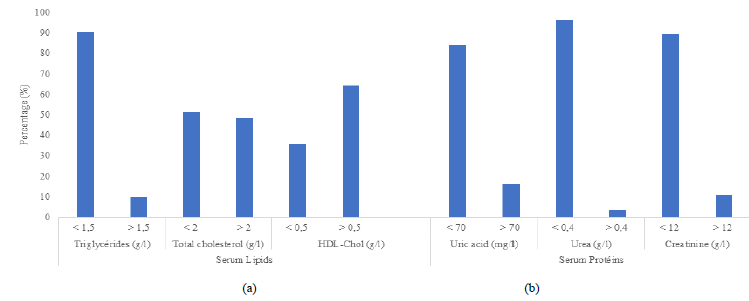
Figure 4: Serum Lipids and proteins of obese patients. (a) Serum lipids; (b) Serum proteins.
BMI-Body mass index; WS-waist circumference; BP-blood pressure; BS-Blood sugar; TG-Triglycérides; TC-Total cholesterol; HDL-C-HDL Cholestérol; UA-Uric acid; Créat-Creatinine; Inc-increase; Stab-stabilization.
Table 3: Evolution of morpho-anthropometric and metabolic parameters of patients.
3.2 Discussion
The objective of this work was to determine the evolution of morpho-anthropometric, metabolic and biological parameters of patients followed at the NIPH. To do this, we first determined the socio-economic and management characteristics of the patients, then the morphoanthropometric, metabolic and biological parameters for monitoring patients at their entry and during their management and finally, established the evolution of these parameters during their treatment. In terms of socio-economic and patient care characteristics, the results showed that populations of all ethnic groups are affected by the diseases studied, but at different proportions. However, a higher prevalence of these diseases is observed in the Akan ethnic group with a high proportion of non-nationals. These results could be explained by the fact that these two population groups are among the largest in the Ivorian population. This was revealed by the general population and housing census [4].
A female predominance for diabetes has also been identified. This predominance of women can be explained by the regularity of consultations observed among women. Also, this has been linked to the various anthropometric indices significantly associated with type 2 diabetes such as body mass index, waist circumference, waist-to-hip ratio, which are much more pronounced in women than in men. Indeed, according to the work of [5] and [6], higher adiposity indices in women than in men, expose them much more to metabolic diseases such as diabetes, high blood pressure etc. Also, biochemical and physiological changes during pregnancy, evidenced by weight gain and adverse effects of estrogen on fat, predispose them first to gestational diabetes mellitus but also to the development of diabetes later [7-9]. However, globally, World Diabetes Federation statistics have shown that men with diabetes outnumber women [10]. This is mainly due to android (visceral) obesity, typically found in men and more likely to cause diabetes than gynoid obesity, typically found in women [11].
A comparison of the age groups affected by the pathologies studied shows an increase in their occurrence beyond the age of 40. This is in line with the results obtained by [12-14] which showed a peak in the prevalence of these diseases and in particular diabetes between 40 and 59 years of age but also an increased risk of their occurring after the age of 44 years. This may also be related to the gradual increase in insulin resistance with age and physical inactivity [15, 16]. The distribution of patients by family history showed a positive association of this risk factor with the occurrence of these conditions. These results were also obtained during the work of [17] and [18] who showed a predominance of genetic factors in the occurrence of these pathologies. However, a fringe of these patients reported no family history. The occurrence of these pathologies could be related to their level, to environmental factors such as poor eating habits, physical inactivity and obesity, especially abdominal obesity.
The results of the morpho-anthropometric, metabolic and biological patient follow-up parameters showed that the majority of patients with these diseases had an above-normal weight and a high waist circumference. This is explained by the insulin resistance gradually created by this morphological state of obesity which, in addition to the sedentary nature of patients, constitutes a real risk factor for the occurrence of these diseases in these patients [19]. In addition, the results showed that almost all diabetic patients had a blood glucose disorder while some of the obese patients (5.4%) also had this hyperglycemia. This disorder of carbohydrate homeostasis in diabetics is justified because it is characteristic of the disease, but in obese patients, it is also due to a progressive insulin resistance in the obese subject. This has led to the progressive onset of diabetes, which is a condition that cannot be detected in obese subjects because it is described as asymptomatic and silent [14]. The results showing normal lipid and serum protein levels in patients could be explained by prescriptions already followed by patients, which have prevented the development of metabolic complications due to these pathologies in the medium to long term [20]. With regard to the evolution of these follow-up parameters during patients' treatments, the results showed a decrease in morphoanthropometric parameters (BMI, WC) in both obese and diabetic patients, a decrease in blood glucose levels (GAJ) especially in diabetic patients and a stabilization of BP, lipids and blood proteins in all patients. All these positive developments show the effectiveness of the treatments followed by patients [21- 23].
4. Conclusion
The different anthropometric (BMI, waist circumference), metabolic and biological (blood glucose, blood pressure, total cholesterol, HDL-cholesterol, triglycerides, uric acid, urea and creatinine) morpho parameters of diabetic and obese patients followed during their treatments have had variable evolutions. For most of these parameters, drug, dietary and physical activity prescriptions allowed them to be rebalanced, although for a number of patients, an unsatisfactory evolution was recorded. This undesirable change in these parameters is in most cases due to poor compliance with these recommendations.
Acknowledgements
The authors sincerely thank the Direction of the National Institute of Public Health (NIPH) for opening the doors of the antidiabetic center of Abidjan (ADCA) and the nutrition service. This allowed us to complete this study.
Conflicts of Interest
No conflicts of interest have been registered on this work to the best of our knowledge.
References
- (World Health Organization), Report on the State of the World's Noncommunicable Diseases, Executive Summary (2011).
- Popkin B. The shift in stages of the nutritional transition in the developing world differs from past experiences! Public Health Nutrition 5 (2002): 205-214.
- Zmirou D. Epidemiology of diabetes in Côte d'Ivoire [thesis] Grenoble: University of Grenoble (1979).
- General Census of Population and Housing. Main preliminary results. Permanent Technical Secretariat of the RGPH Technical Committee (2014): 1-23.
- Karangwa J. Study of the prevalence of diabetes mellitus in Bujumbura. Thesis Med Buj (1995): 167.
- Meisinger C, Doring A, Thorand B, et al. Body fat distribution and risk of type 2 diabetes in the general population: are there differences between men and women? The MONICA/KORA Augsburg cohort study. American Journal of Clinical Nutrition 84 (2006): 483-489.
- Jovanovic-Peterson L, Biermann J. The diabetic woman. New York: GP Putnam's Sons (1996): 16-18.
- Prasanna K. Gender difference in diabetes mellitus. International Journal of Diabetes in Developing Countries 16 (1996): 103-104.
- Grant J, Hicks N, Taylor A, et al. North West Adelaide Health Study Team. Gender-specific epidemiology of diabetes: a representative cross-sectional study. Int J Equity Health 8 (2009): 6.
- International Diabetes Federation (IDF). IDF Diabetes Atlas (6th) (2013): 11.
- Grimaldi A. Internship issues. Faculty of Medicine, Diabetology. Pierre and Marie Curie (2000): 22.
- Akinkugbe O. Non-communicable disease in Nigeria: final report of National Survey. Lagos: Federal Ministry of Health and Social Services (1997): 64-90.
- King H, Aubert R, Herman W. Global burden of diabetes, 1995-2025: prevalence, numerical estimates and projections. Diabetes Care 21 (1998): 1414-1431.
- International Diabetes Federation. Diabetes Atlas (5th) Brussels (2011).
- Burattini R, Di Nardo F, Boemi M, et al. Deterioration of insulin sensitivity and glucose effectiveness with age and hypertension. American Journal of Hypertension 19 (2006): 98-102.
- Laura D. What is insulin resistance? (2011).
- Meigs J, Cupples L, Wilson P. Parental transmission of type 2 diabetes: the Framingham Offspring Study. Diabetes 49 (2000): 2201-2207.
- Papazafiropoulou A, Sotiropoulos A, Skliros E, et al. Familial history of diabetes and clinical characteristics in Greek subjects with type 2 diabetes. BioMed Central Endocrine Desorders 9 (2009): 12.
- Shulman G. Cellular mechanisms of insulin resistance. Journal of Clinical Investigation 106 (2000): 171-176.
- Monnier L. Hyperglycemic effects of food. Treaty of diabetology. Paris: Pradel (1990): 11323.
- Hankey CR, Rumley A, Lowe GDO, et al. Weight loss improves thrombotic and rheological risk factors for ischaemic heart disease risk. Proc Nutr Soc (1995): 54.
- Maggio CA, Pi-Sunyer FX. The prevention and the treatment of obesity. Application to type 2 diabetes. Diabetes Care 20 (1997): 1744-1766.
- Marks SJ, Moore NR, Clark ML, et al. Reduction of visceral adipose tissue and, improvement of metabolic indices. Effect of dexfenfluramine in NIDDM. Obesity Res 4 (1996): 18.
