Diagnostic Overview of Neurological Manifestation in Pediatric Inflammatory Bowel Disease: A Case Report with Literature Review
Article Information
Zinia Pervin1*, Md Al Hasibuzzaman2, Shuvashis Paul3
1Department of Biomedical Engineering, University of New Mexico, Albuquerque, NM, USA
2Ningbo University Medical School, Ningbo City, Zhejiang Province, PR China
3Department of Pediatrics, Enam Medical College and Hospital, Savar, Dhaka, Bangladesh
*Corresponding Author: Zinia Pervin, M.B.B.S, M.SC, Department of Biomedical Engineering, University of New Mexico, Address: 2425 Camino de Salud, Albuquerque, NM 87106, USA
Received: 08 December 2020; Accepted: 22 December 2020; Published: 26 December 2020
Citation:
Zinia Pervin, Md Al Hasibuzzaman, Shuvashis Paul. Diagnostic Overview of Neurological Manifestation in Pediatric Inflammatory Bowel Disease: A Case Report with Literature Review. Journal of Pediatrics, Perinatology and Child Health 4 (2020): 163-168.
View / Download Pdf Share at FacebookAbstract
Peripheral neuropathy is rare in children, however inflammatory bowel disease (IBD) can lead to neurological manifestation in pediatric patients. IBD is a term for Crohn’s disease (CD) and ulcerative colitis (UC), believed to be resulting from chronic inflammation and unresponsive activation of the mucosal immune system of the gastrointestinal tract. Although extra intestinal manifestation including several systemic dysfunctions has been documented in IBD, the neurological association and its pathogenesis are rare during the early course of IBD. However, the occurrence of neurological manifestation in IBD may cause secondary disability which can persist throughout life, may become life-threatening if left untreated. We reported a child diagnosed case of pediatric inflammatory bowel disease was admitted with a complaint of neurological manifestation. We investigated the possible causes of neuropathy in IBD, after excluding other possible causes related to neuropathy, this case is diagnosed as acute sensorimotor peripheral neuropathy due to nutritional deficiency or immunomodulatory drug associated with Crohn's disease. Immunosuppression is an integral part of the treatment of pediatric IBD but the inconsiderable selection of immunomodulatory drugs may result in irreversible risk including neurological impairment.
Keywords
Peripheral neuropathy, Inflammatory bowel disease, Neurological manifestation, Nutritional deficiency, Immunosuppression
Peripheral neuropathy articles; Inflammatory bowel disease articles; Neurological manifestation articles; Nutritional deficiency articles; Immunosuppression articles
Article Details
Abbreviation:
IBD-Inflammatory bowel disease; CD-Crohn’s disease; UC-ulcerative colitis
1. Case Description
A 14-year-old male patient was admitted to the pediatric ward with the chief complaint of semi-consistent stool slightly mixed with blood and mild abdominal pain for approximately two weeks. He had a history of weight loss and fatigue over 6 months. He was a diagnosed case of inflammatory bowel disease (IBD); the histopathological examination and colonoscopy results established the diagnosis at the age of 13. His parent was reported that he was having experience IBD symptoms prior to his diagnosis of about 9 months. After diagnosis, he was in the treatment of corticosteroids and non-steroidal anti-inflammatory drug, the evaluation was initially favorable but with 2 relapses in 1st year. Then he was given prednisolone for inducing remission with immunomodulators 6-MP for maintenance therapy to prevent the disease exacerbation. At this moment of his third relapse, he presented mild fever, abdominal cramps, diarrheic stool with blood, and massive weight loss of approximately 4 kg in the last 2 months. Besides this syndrome, surprisingly he noticed the mild pain and weakness of his lower extremity during movement and walking over the last 2 months. He was psychologically upset and emotionally disturbed due to he gradually lost his balance. He had a history of neonatal diarrhea, which is caused by gastrointestinal infection, but the causative agent was unknown. Drug history revealed the antibiotic exposure of metronidazole prior to his confirmed diagnosis of IBD.
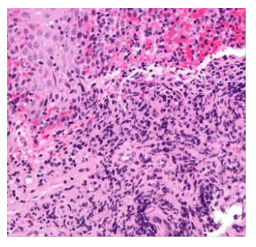
On Physical examination, the patient had minor gait impairment and distal symmetric weakness. The neurological examination confirmed mild peripheral neuropathy, slightly decreasing ankle jerk, with reducing distal vibration and pinprick sensation. Lab examination had revealed the slight leukocytosis with increase erythrocyte sedimentation rate (30mm/hour) and elevated C- reactive protein (20mg/dl). We also investigated the liver function and renal profile including transaminases, urea, and creatinine, which were all within normal physiological limits. A complete blood count shows anemia with Hb 12.5g/dl; the patient’s serum levels of lipid profile and thyroid-stimulating hormone (TSH), T3, T4 were within normal limits. We did not get any positive culture result for bacteria and parasites in stool examination except the only presence of dead leukocytes. His blood glucose log was within normal limit, fasting was less than 110mg/dl and postprandial glucose level was < 130mg/dl, His HbA1c was 5.6%. There were no pathological findings in upper GIT which was excluded by endoscopy. Colonoscopy revealed the pathological appearance of colonic mucosa with follicular edema. The histopathological picture (Figure) of the lower intestinal mucosa (inflammatory infiltration with mucosal disruption) confirmed the diagnosis of ileocolic Crohn’s disease. Hematological profile excludes the provisional diagnosis for peripheral neuropathy like rheumatic diseases, thyroid disorder, and glucose intolerance. Laboratory studies reported a decreased level of B12 (200 ng/dl), vitamin D (20 ng/ml), and iron in serum.
2. Discussions
Recent epidemiological studies have reported global incidence rate of IBD is increased significantly from 1991 to 2017, the prevalence rate is raised from 79.5 to 84.3 per 100 000 population with neurological manifestations varying from 0.25 to 35.6% [1, 2]. In addition, the annual incidence rate of pediatric Crohn's disease is increased or surpassed the UC over the past 40 years, 25- 30% of patients with Crohn's disease are younger than 20 years old [3]. Although the onset or diagnosis of Crohn's disease has typically occurred at approximately 15 years of age, the gender-related onset is different in adults and children; Crohn's disease is a higher risk among boys but risk increase among women in the adult group [4].
The etiology of pediatric IBD is believed to results from a complex variety of factors like inappropriate immune response, genetics, or environmental risks. The genetic abnormality is more common in the onset of pediatric IBD than environmental exposure (more susceptible to adult) such as cigarette smoking, stress, nonsteroidal anti-inflammatory drugs which are required long-term exposure to influence or modify the mucosal immune system. In terms of genetic association, NOD2/CARD15 gene mutation on chromosome 16 has been responsible to develop chron’s disease in children [3]. This type of genetic mutation causes increase activation of proinflammatory cytokines like nuclear factor-kappa B (NF-κB), TNFα which are resulting in imbalance regulation of the intestinal mucosal immune system and disruption of mucosal protection; host immune response can also be abnormally triggered by drug resistance microbes, infectious agents such as virus, bacteria, parasite [5-7]. Patients with IBD have been shown high titer of virus, bacteria, 68% of patients with Crohn's disease showed the perinuclear antineutrophil cytoplasmic antibodies (pANCA) and anti-Saccharomyces cerevisiae antibodies (ASCA) [8, 9]. Immunoglobin IgA and IgG related antibody can be used as a diagnostic accuracy of IBD.
In respective of this case, the patient had a history of exposure to infectious agents which can be the responsible factor to trigger the abnormal immune response of the mucosal defensive system. Activated immune cells increase the production of inflammatory cytokines which can be implicated in pathogenesis and activation of the chronic inflammatory condition including increase susceptibility of IBD [8]. The patient had also a history of growth retardation and weight loss which are the spatial consideration in pediatrics IBD due to increased metabolic demand for growth and sexual maturation during the developmental period but IBD leads to malabsorption of growth essential vitamins with inadequate nutritional supplementation (Table) [10]. In general, pediatric patients with IBD often exhibit essential vitamins and nutritional deficiencies due to malabsorption. Vitamin B12 deficiency is the most common feature of neuropathy in Crohn's disease because vitamin B12 is required for the maturation of DNA genetic material, myelination, and axon formation of the nervous system [11]. In the case of pediatric patients, it is a rare onset of peripheral neuropathy because most of the case's onset of peripheral neuropathy is 50-60 years of age. We cannot specify the phenotype of peripheral neuropathy because the patient refused to do the nerve conduction velocity test, electromyography, and nerve biopsy.
|
Causes of neurological manifestations associated with IBD |
Pathophysiology |
Features/ phenotypes of neuropathy |
Diagnostic test |
Treatment/ Prognosis |
|
Malabsorption and vitamin B12 deficiency |
The disease of terminal ileum reduce the absorption of B12 which may progress to demyelination and axonal degeneration (decrease enzymatic activity) |
Symmetric polyneuropathy myelopathy. sensory ataxia and loss of cutaneous sensation |
Serum level of vitamin B12, schilling test, intrinsic factor antibodies. |
Increase vitamin B12 dietary supplementation or intramuscular monthly injections |
|
Vitamin D and E deficiency |
Intestinal inflammation causes decrease absorption of Vitamin D, E which causes pathologic changes of the sensory root, peripheral nerve and may impair nociceptor function, worsens nerve damage, and lowers the pain threshold. |
Myopathy, sensory axonal peripheral neuropathy including numbness, tingling, burning sensation |
Bloodstream analysis for vitamin E, D2, and D3 |
Dietary or parenteral vitamin D supplementation, IV/IM injection. |
|
Immuno-suppression |
Immunosuppressive agents (anti-TNF or the immunomodulatory) are used in IBD treatment which leads to neurotoxicity |
Multifocal demyelinating and axonal neuropathy |
Drug history, antibody titers |
Discontinued the biologic agents with supportive treatment |
|
Neuronal influence of GIT(enteric nervous system linked digestive disorder) |
GIT neurochemistry, absorption disorder, stress are considered as a modulator to enhance the degree of intestinal inflammation through a neural or neuroendocrine pathway which leads to neuronal intoxication. |
Adversely affect peripheral nerves, potentially worsening the numbness, burning, and tingling sensations (skin and peripheral joint). |
History and psychological assessment |
Psychological cognition therapy, Anxiolytic, antidepressant |
|
Drug-induced neurotoxicity |
Metronidazole, sulfasalazine, cyclosporine, biological agents |
sensorimotor axonal Peripheral neuropathy with ataxia. |
Related drug exposure history |
Discontinuation of responsible drug with monitoring the neurological outcome |
|
Thrombo-embolism or thrombosis |
IBD increases the risk of hypercoagulability related to venous engorgement |
Sciatic neuropathy, peripheral neuropathy |
Coagulation profile |
Anticoagulant therapy |
|
Malabsorption |
The small intestine is unable to absorb nutrients properly (Vitamin A, B1, B6, folic acid, copper) |
Primarily Sensory neuropathy, Later polyneuropathy, |
Intestinal biopsy and histo-pathology |
Nutritional supplementation, IV /IM supplementation |
Table: Neurological manifestations and pathophysiology of neurological disorder in IBD with treatment outcome [2, 12-15].
3. Diagnosis
Recurrent Crohn’s disease with sensory motor peripheral neuropathy due to nutritional or immunomodulatory agents.
4. Management
We initiated treatment with antibiotics for 7 days and probiotics for one month along with long-term anti-inflammatory (steroid) therapy. Discharged with recommended high-dose oral vitamin D and vitamin B12 tablets (1000 to 2000 µg) taken daily or intramuscular monthly injections to correct blood and
neurologic abnormalities along with antidepressants.
Acknowledgments
Department of Pediatrics, Enam Medical College, and Hospital.
Conflicts of Interest
The authors do not have any conflicts of interest.
Funding
This research did not receive any specific grant from the public, commercial or non-profit organization.
References
- Alatab S, Sepanlou SG, Ikuta K, et al. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 5 (2020): 17-30.
- Zois CD, Katsanos KH, Kosmidou M, et al. Neurologic manifestations in inflammatory bowel diseases: Current knowledge and novel insights. Journal of Crohn’s and Colitis 4 (2010): 115-124.
- Diefenbach KA, Breuer CK. Pediatric inflammatory bowel disease. World Journal of Gastroenterology 12 (2006): 3204-3212.
- Sýkora J, Pomahacová R, Kreslová M, et al. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World Journal of Gastroenterology 24 (2018): 2741-2763.
- Fiocchi C. Inflammatory bowel disease: Etiology and pathogenesis. Gastroenterology 115 (1998): 182-205.
- Pervin Z, Hassan MM. Synergistic therapeutic actions of antimicrobial peptides to treat multidrug-resistant bacterial infection. Rev Med Microbiol; Publish Ah. Epub ahead of print doi: 10.1097/MRM.0000000000000239 (2020).
- Marginean CO, Melit LE, Mocanu S, et al. Inflammatory bowel diseases. Medicine (Baltimore) 96 (2017): e6329.
- Guan Q. A Comprehensive Review and Update on the Pathogenesis of Inflammatory Bowel Disease. J Immunol Res (2019).
- Zhang YZ, Li YY. Inflammatory bowel disease: Pathogenesis. World J Gastroenterol 20 (2014): 91-99.
- Ye Y, Manne S, Treem WR, et al. Prevalence of Inflammatory Bowel Disease in Pediatric and Adult Populations: Recent Estimates from Large National Databases in the United States, 2007-2016. Inflamm Bowel Dis 26 (2020): 619-625.
- Hammond N, Wang Y, Dimachkie MM, et al. Nutritional neuropathies. Neurologic Clinics 31 (2013): 477-489.
- Spagnoli C, Pisani F, Di Mario F, et al. Peripheral neuropathy and gastroenterologic disorders: An overview on an underrecognized association. Acta Biomedica 89 (2018): 22-32.
- Cohen BL, Torres J, Colombel JF. Immunosuppression in inflammatory bowel disease: How much is too much? Current Opinion in Gastroenterology 28 (2012): 341-348.
- Gondim FAA, Brannagan Iii TH, Sander HW, et al. Peripheral neuropathy in patients with inflammatory bowel disease. Brain 128 (2005): 867-879.
- Ståhlberg D, Bárány F, Einarsson K, et al. Neurophysiologic studies of patients with crohn’s disease on long-term treatment with metronidazole. Scand J Gastroenterol 26 (1991): 219-224.