Diagnostic Accuracy of Renal Resistive Index for Detecting Diabetic Nephropathy: A Comparative Study Against Biochemical Markers
Article Information
Dr Anika Mahfuz1, Dr Saieef Zaman2, Dr. Kazi Shantono Saiham3, Dr. Md. Immam Hossin4, Dr Kamrun Nahar5, Dr Md. Rasel Ahmad6, Dr S M Yunus Ali*, 7
1Resident Doctor, Radiology and Imaging, Sir Salimullah Medical College, Dhaka, Bangladesh
2Resident Doctor, National Institute of Kidney Disease and Urology, Dhaka, Bangladesh
3Consultant radiologist, Doctors Care General Hospital, Brahmanbaria
4PhD Fellow, Bangladesh Medical University (OSD), DGHS, Mohakhali, Dhaka, Bangladesh
5Professor of Forensic Medicine, International Medical College
6Assistant Professor, Medical Education, Department of Public Health and Informatics, Bangladesh
7Associate professor, Department of Urology, Bangladesh Medical University, Dhaka, Bangladesh
*Corresponding Autho: Dr SM Yunus Ali, Associate Professor, Department of Urology, BMU
Received: 14 November 2025; Accepted: 08 December 2025; Published: 19 December 2025
Citation: Dr Anika Mahfuz, Dr Saieef Zaman, Dr. Kazi Shantono Saiham, Dr. Md. Immam Hossin, Dr Kamrun Nahar, Dr Md. Rasel Ahmad, Dr S M Yunus Ali. Diagnostic Accuracy of Renal Resistive Index for Detecting Diabetic Nephropathy: A Comparative Study Against Biochemical Markers. Fortune Journal of Health Sciences. 8 (2025): 1174-1178.
View / Download Pdf Share at FacebookAbstract
Background: Diabetic nephropathy (DN) is a prominent microvascular complication and the predominant cause of end-stage renal disease, early and precise diagnosis is critical to prevent irreversible kidney dysfunction.
Aim: To evaluate the diagnostic performance of intra-renal index RI in detecting diabetic nephropathy using sensitivity, specificity, predictive values, overall accuracy and likelihood ratios; besides comparing with biochemical markers serum creatinine, eGFR and albumin-to-creatinine ratio (ACR) as a gold standard.
Materials and Methods: This was a cross-sectional observational study, and trains were conducted in the Department of Radiology and Imaging, Sir Salimullah Medical College Hospital, Dhaka between January 2023 to December 2024. A panel of 57 men and women with stringent inclusion/exclusion criteria. This study was approved by the institutional review board, and it met the code of ethics concerning human beings as formulated by The Declaration of Helsinki. The intrarenal RI of all patients was measured by spectral Doppler ultrasound. Statistical analysis Statistical and all data were presented as a mean ± SD using SPSS software (version 26) when appropriate statistical tests of significance are applied.
Results: Among the 57 subjects (mean age 56.39 ± 8.54 years; female, 52.6%), diabetic nephropathy was noted in 82.5% and rose significantly as duration of diabetes increased to a maximum of all cases after >20 years (>100%). Increased intrarenal RI (>0.7) was detected in 78.9% of participants and significantly associated with albuminuria; 93.3% of patients with high RI also had ACR >30 mg/g. The performance measures for the RI were as follows: sensitivity, 89.36%; positive predictive value, 93.33%; overall accuracy, 85.96%; and positive LR, 2.9.
Conclusion: Measurement of intrarenal resistive index by using Doppler ultrasonography is an effective, non-invasive and economic way to predict diabetic nephropathy with greater sensitivity and positive predictive values than standard biochemical parameters and have good correlations.
Keywords
Ultrasonography, Resistive Index, Albumin, Creatinine, Sensitivity, Spectral Doppler
Article Details
Introduction
Diabetic nephropathy is the most important microvascular complication of DM, it is considered as a major cause of ESRD worldwide burdening the patients and health system. It is important to detect renal damage at an early stage in patients with diabetes, since its progression leads to chronic kidney disease and ultimately to end-stage renal failure [1,4,6]. though they generally reflect established rather than incipient structural damage, and may lag the early hemodynamic changes [1,4,8]. Doppler ultrasonography measured intrarenal resistive index (RI) is a non-invasive hemodynamic parameter, which reflects the intrarenal vascular resistance and was suggested to be used as an adjunctive marker of early renal injury in diabetes [4,5,6,7,8,9]. RI is derived from peak systolic and end-diastolic velocities in intrarenal arteries and elevated RI measures have been correlated with worse renal function, higher albuminuria and histopathological renal injury across a few previous studies [4,5,6,13]. Some cross-sectional and prospective studies have shown higher RI in diabetic subjects with renal insufficiency than in diabetes without nephropathy and healthy controls [5,6,7,11].
Although encouraging results have been obtained, studies addressing optimal RI cutoffs and the diagnostic performance report some heterogeneity and RRI is influenced by systemic vascular factors, which might affect its specificity for renal parenchymal disease [9, 18]. Certain cohorts have described an RI cut-off of approximately 0.65-0.70 for the exclusion of DKD, whereas other cohorts suggest slightly higher values; consequently, sensitivity/specificity estimates in the present literature vary or depend on the biochemical/histological reference standard selected [8,11,12,19]. This cross-sectional study was conducted at Sir Salimullah Medical College Hospital to evaluate the diagnostic accuracy of intrarenal RI for DN in relation to serum creatinine, eGFR and ACR. The goal was to evaluate and ascertain whether RI has an acceptable level of sensitivity, specificity, predictive value and accuracy to be used as a simple, noninvasive ordered step screening test [1].
Materials and Methods
It was a cross-sectional study and was done in the Department of Radiology and Imaging of Sir Salimullah Medical College (SSMC), Dhaka, Bangladesh from 2023 to 2024. Fifty-seven patients with type 2 diabetes mellitus and clinical suspicion of diabetic nephropathy were enrolled by purposive sampling. Inclusion criteria included patients being treated for at least 10 years for type 2 diabetes or clinical evidence of nephropathy. Excluded patients were those who had had obstructive uropathy, a background of glomerulonephritis, single or transplant kidney, and drug or radiation-induced nephropathy. The sample size was estimated by the formula for diagnostic test, and 57 individuals were obtained. Demographic and clinical characteristics, as well as biochemical and Doppler ultrasonographic findings were retrieved. Intrarenal RI was quantified through Doppler ultrasonography, with a value of >0.7 indicative of nephropathy. Grey scale, color Doppler and spectral Doppler imaging were performed in each patient to quantify biochemical measures including serum creatinine, urinary albumin and eGFR. The time for each examination was 30-40 minutes per patient. Doppler observations were then compared with biochemical values to evaluate diagnostic agreement.
Results
The results present distribution of baseline characteristics, prevalence of DN and Doppler derived RI pattern with its association with biochemical markers and diagnostic accuracy of intrarenal RI.
Table 1: Baseline Characteristics of Participants (n = 57)
|
Age group in year |
Frequency |
Percentage |
|
<40 |
4 |
7 |
|
40-50 |
10 |
17.5 |
|
51-60 |
26 |
45.6 |
|
61-70 |
17 |
29.8 |
|
Mean age(±SD) in years |
56.39±8.54 in years |
|
|
Gender |
Frequency |
percentage |
|
Male |
27 |
47.4 |
|
Female |
30 |
52.6 |
|
Total |
57 |
100 |
Table 1 shows that most participants were between 51-60 years of age 45.6%, with a mean age of 56.39 ± 8.54 years. Females comprised slightly more than half of the study population 52.6%.
Table 2: Presence of diabetic nephropathy (n=57)
|
Sex |
Frequency |
Percent |
|
|
Male |
No |
3 |
11.1 |
|
Yes |
24 |
88.9 |
|
|
Total |
27 |
100 |
|
|
Female |
No |
7 |
23.3 |
|
Yes |
23 |
76.7 |
|
|
Total |
30 |
100 |
|
Table 2 displays the Diabetic nephropathy was present in 82.5% of the study population, affecting 88.9% of males and 76.7% of females.
Table 3: Association between duration of diabetes mellitus with presence of diabetic nephropathy
|
Presence of Diabetic Nephropathy |
Total |
|||
|
No |
Yes |
|||
|
Duration of dm categories in years |
<10 |
6 |
4 |
10 |
|
Oct-20 |
4 |
36 |
40 |
|
|
>20 |
0 |
7 |
7 |
|
|
Total |
10 |
47 |
57 |
|
Table 3 indicates the prevalence of only 40% of participants with <10 years of diabetes had nephropathy, compared with 90% in the 10-20year group, and 100% among those with diabetes for more than 20 years.
Table 4: Renal artey doppler findings of the suspected diabetic nephropathy cases (n=57)
|
RI category |
N |
Mean |
Std. Deviation |
|
|
<.7 |
Lt. renal resistive index |
12 |
0.646 |
0.02413 |
|
Rt. renal resistive index |
12 |
0.634 |
0.04116 |
|
|
>.7 |
Lt. renal resistive index |
45 |
0.7819 |
0.07209 |
|
Rt. renal resistive index |
45 |
0.7751 |
0.06111 |
|
Table 5: Doppler findings of renal artery in both diabetic kidney and normal diabetic patients.
|
RI category |
Total |
||||
|
<.7 |
>.7 |
||||
|
Albuminuria category |
<30 |
Count |
7 |
3 |
10 |
|
% within RI category |
58.30% |
6.70% |
17.50% |
||
|
>30 |
Count |
5 |
42 |
47 |
|
|
% within RI category |
41.70% |
93.30% |
82.50% |
||
|
Total |
Count |
12 |
45 |
57 |
|
|
% within RI category |
100.00% |
100.00% |
100.00% |
||
Table 5 elevated resistive index >0.7 was strongly associated with albuminuria, with 93.3% of participants in this category showing ACR >30 mg/g. Conversely, normal RI <0.7 was more frequently observed among participants with normal albuminuria 58.3%.
Table 6: Diagnostic Accuracy
|
Type |
Percentage |
|
Sensitivity |
89.36% |
|
Specificity |
70% |
|
Accuracy |
85.96% |
|
positive predictive value |
93.33% |
|
negative predictive value |
58.33% |
|
LR+ |
2.9 |
|
LR- |
0.1 |
Table 6 also demonstrates high sensitivity 89.36% and a robust PPV 93.33% of RI in identifying diabetic nephropathy, but the accuracy values are as high as 85.96%. Specificity was fairly good 70% and NPV was moderate 58.33%. High and normal RIs significantly increase and decrease, respectively, the odds for nephropathy as suggested by the LR values 2.9 and 0.1.
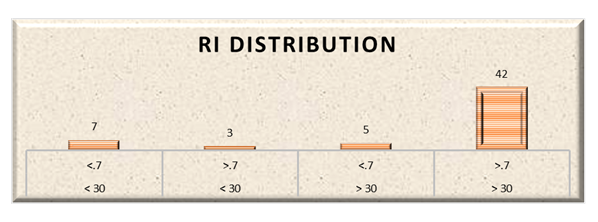
Figure 1 shows a positive association between higher albuminuria >30 and higher RI category >0.7, which could be clinically significant.
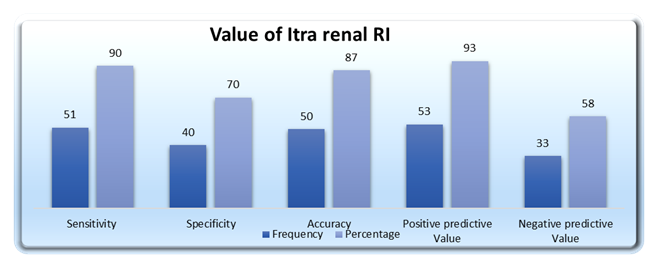
Figure 2 shows Intra-renal RI had high sensitivity and specificity 90%, 70%. Overall accuracy was 87% while the positive predictive value, and hence the reliability for identifying diabetic nephropathy, was high 93%.
Discussion
In the current study serum prolactin levels of Bangladeshi women from 20 to 40 years of age with and without endometriosis were measured and correlated with their menstrual/reproductive factors. In keeping with previous studies that reported a higher rate of hyperprolactinemia in endometriosis cases [3,5,7], we found an increase in serum prolactin levels of women with vs. without endometriosis. In addition, hyperprolactinemia has been associated with the pathophysiology of endometriosis through its immuno-modulation and pro-augmentation of angiogenesis which could support survival and an inflammatory response in the ectopic endometrial cells [6,11]. Consistent with previous studies, the degree of prolactin elevation was greater in women with dysmenorrhea and shorter cycle length as seen in [8,10], supporting that prolactin may influence pain pathways and cycle control. The association of RL with reproductive history in the present study confirms the prior literature concerning endometriosis and hormonal disarray. Women with nulliparity and history of infertility were observed to have high levels of prolactin, like many other studies that showed an association between hyperprolactinemia and fecundity impairment [12,13,15]. Prolactin influence on gonadotroph secretion, luteal phase function and ovulation has been described in reproductive endocrinology literature [9,14,18]. Our findings support these physiological processes, and we venture to suggest that prolactin may be a marker of disease severity and/or an agent in the reproductive disturbance experienced by these women affected with this disorder.
In comparison to other global studies, the median prolactin levels of these women with endometriosis were similar to that of South Asian and Middle Eastern populations [16,17,19] suggesting a certain regional hormonal patterns. Serum prolactin was also reported to be significantly elevated in the 14 advanced-staged patients when compared with low/insignificant disease, and there is the evidence that serum prolactin levels correlate with disease extension and related inflammatory activity [20,21]. Some researchers recommend prolactin is also involved in neuroimmune interactions related to chronic pelvic pain, which could account for our result that painful symptoms were more common in the high- prolactin group [21]. This study is homogenous, uses a specific diagnostic criterion, and takes several menstrual and reproductive variables into account at once. But there is still a downside to being acknowledged. The cross-sectional data design does not allow for causative conclusions, and stress [2], sleep-wake pattern variation [22]; and medication use (only incompletely controlled in our study) may all influence prolactin level as other investigators have reported. A further limitation is the small number of samples, and large multicenter studies are needed to support the regional population feature.
Conclusion
The study proves that intrarenal resistive index is a simple, safe, and effective non-invasive marker for diabetic nephropathy. Increase in RI is correlated closely with albuminuria and serum creatinine and may be used adjunctively as a very good diagnostic tool for early renal involvement detection and screening in diabetic patients.
Conflict of Interest: The authors have declared that no conflict of interest exists regarding the publication of this article.
Authors Contributions: Dr Anika Mahfuz conceived the study and the methodology. Dr Saieef Zaman and Dr Kazi Shantono Saiham helped with data management and statistical analysis. Dr Md. Immam Hossin and Dr S. M. Yunus Ali assisted with manuscript writing and critical corrections. Dr Md. Rasel Ahmad provided final approval of the manuscript. All authors read and approved the final version.
Reference
- Khairallah MK, Sobh MA, Mansour E, et al. Renal Resistive Index as a Promising Tool in Early Identification of Diabetic Nephropathy. Egypt J Hosp Med 90 (2023): 1983–1987.
- D’Souza AVL, D'Souza RC, Adiga PK, et al. The Renal Resistive Index as a Early Predictor of Renal Dysfunction in Patients with Type 2 Diabetes Mellitus. Clin Res J Intern Med 5 (2024): 129–133.
- Geraci G, Bolignano D, Cerasola G. Renal Resistive Index from Renal Hemodynamics to Cardiovascular Risk: An Update. Clin Med Insights Nephrol 13 (2025): 178.
- Platt JF, Rubin JM, Ellis JH. Diabetic nephropathy: evaluation with renal duplex Doppler US. Radiology 190 (1994): 343–346.
- Shirin M, Sharif MM, Gurung A, et al. Resistive Index of Intrarenal Artery in Evaluation of Diabetic Nephropathy. Bangladesh Med Res Counc Bull 41 (2015): 125–130.
- Jinadu YO, Raji YR, Ajayi SO, et al. Resistivity index in the diagnosis and assessment of loss of renal function in diabetic nephropathy. Cardiovasc J Afr 33 (2022): 26–32.
- Baz AA, Abd El-Motaleb AA, Shehata A, et al. Diagnostic utility of renal shear wave elastography and renal resistivity index in diabetic kidney disease. Egypt J Radiol Nucl Med 55 (2024): 139.
- Li H, Shen Y, Yu Z, et al. Potential Role of the Renal Arterial Resistance Index in Discriminating Diabetic Kidney Disease from Nondiabetic Kidney Disease. Front Endocrinol (Lausanne) (2022).
- Darabont R, Ion DA, Balanescu A, et al. Current Insights into Renal Resistive Index Significance in Systemic and Renal Disease. Diagnostics (Basel) 13 (2023): 1687.
- (Generic review / classic physiology citations) several standard reviews describe renal hemodynamics and RI; representative historical overview: Derchi LE. Ultrasonographic imaging and Doppler analysis of renal hemodynamics (1994).
- Ali NO, Khalaf-Awada AM, Fayed HM, et al. Role of Renal Resistive Index in early detection of Diabetic Nephropathy in Type II Diabetic Patients. SVU-International Journal of Medical Sciences 7 (2024): 1011–1021.
- Kuttancheri T, Das SK, Shetty MS, et al. Renal resistive index as a marker of histopathological damage in diabetic and non-diabetic chronic kidney disease. Egyptian Journal of Radiology and Nuclear Medicine, 54 (2023):
- Kuttancheri T, Das SK, Shetty MS, et al. Renal resistive index as a marker of histopathological damage in diabetic and non-diabetic chronic kidney disease. Egypt J Radiol Nucl Med 54 (2023): 159.
- Khan A, Ahmed A, Bhutta MR, et al. Correlation between resistive index and serum creatinine in patients with diabetic nephropathy. Pak Armed Forces Med J 73 (2023): 435–438.
- Kuttancheri T, Das SK, Shetty MS, et al. Renal resistive index as a marker of histopathological damage in diabetic and non-diabetic chronic kidney disease. Egyptian Journal of Radiology and Nuclear Medicine, 54 (2023):
- Dsouza AVL, D'Souza R, Adiga K P, et al. The Renal Resistive Index as A Early Predictor of Renal Dysfunction in Patients with Type 2 Diabetes Mellitus: Renal Resistive Index Predictor of Renal Dysfunction Type 2 Diabetes Mellitus. CRJIM 5 (2024): 129-33.
- Shirin M, Sharif M, Gurung A, Datta A. Resistive index of intrarenal artery in evaluation of diabetic nephropathy. Bangladesh Med Res Counc Bull 41 (2015): 155–160.
- Li H, Shen Y, Yu Z, et al. Potential Role of the Renal Arterial Resistance Index in the Differential Diagnosis of Diabetic Kidney Disease. Frontiers in Endocrinology 12 (2022): 731187.
- Darabont, R., Mihalcea, D., & Vinereanu, D. Current Insights into the Significance of the Renal Resistive Index in Kidney and Cardiovascular Disease. Diagnostics 13 (2022): 1687.
- Shaker AM, Sleem SY, Aly MI, et al. Role of shearing wave elastography in detecting early diabetic nephropathy. Irish journal of medical science 194 (2025): 529–535.
- Kuttancheri T, Das SK, Shetty MS, et al. Renal resistive index as a marker of histopathological damage in diabetic and non-diabetic chronic kidney disease. Egyptian Journal of Radiology and Nuclear Medicine, 54 (2023):
- Jinadu YO, Raji YR, Ajayi SO, et al. Resistivity index in the diagnosis and assessment of loss of renal function in diabetic nephropathy. Cardiovascular journal of Africa 33 (2022): 26–32.