Designing a Resident Led Otolaryngology Clinic at a Community Health Center: An Initial Experience
Article Information
Ethan Frank1*, Christopher Vuong1, Nathan H Lee2, Shannon O Calaguas1, Khanh Nguyen1, Priya Krishna1,2, Daniel I Kwon3
1Department of Otolaryngology - Head and Neck Surgery, Loma Linda University Health, Loma Linda, California, USA
2Loma Linda University School of Medicine, Loma Linda, California, USA
3Department of Otolaryngology - Head and Neck Surgery, Keck School of Medicine, University of Southern California, Los Angeles, California, USA
*Corresponding Author: Ethan Frank, Department of Otolaryngology - Head and Neck Surgery, Loma Linda University Health, Loma Linda, California, USA
Received: 16 June 2023; Accepted: 22 June 2023; Published: 04 August 2023
Citation: Ethan Frank, Christopher Vuong, Nathan H Lee, Shannon O Calaguas, Khanh Nguyen, Priya Krishna, Daniel I Kwon. Designing a Resident Led Otolaryngology Clinic at a Community Health Center: An Initial Experience. Journal of Surgery and Research. 6 (2023): 272-276.
View / Download Pdf Share at FacebookAbstract
Objectives: To report a resident-led otolaryngology clinic experience at an independent Federally Qualified Health Center (FQHC) with an affiliated academic center. We compared delivery of subspecialty care for underserved patients in a unique resident run clinic to standard care at the university staffed subspecialty clinics.
Methods: Retrospective cohort study of surgical patients seen at the Social Action Community Health System (SACHS) otolaryngology clinic over a one-year period compared with a matched control cohort of patients having similar procedures at the affiliated faculty academic practice. Measured endpoints were case type, time of referral to consultation, time interval between surgical decision and date of surgery, surgical complications, as well as post-surgical follow up.
Results: A total of 687 new patients were seen at SACHS clinic, with approximately 18% ultimately undergoing surgery. All otolaryngology subspecialties were represented including otology, facial plastics, and head and neck oncology. SACHS patients had overall slightly higher median interval times from referral to consultation and from surgical decision to date of surgery though this did not reach significance. There were no differences in surgical outcomes or complication rates between the SACHS cohort and faculty cohort.
Conclusions: We demonstrate a mutually beneficial partnership between a fully resourced FQHC system and an otolaryngology residency program to provide reciprocally beneficial training experience and effective health care delivery.
Keywords
Resident run clinic, Community health services, Vulnerable populations, Graduate medical education
Resident run clinic articles; Community health services articles; Vulnerable populations articles; Graduate medical education articles
Resident run clinic articles Resident run clinic Research articles Resident run clinic review articles Resident run clinic PubMed articles Resident run clinic PubMed Central articles Resident run clinic 2023 articles Resident run clinic 2024 articles Resident run clinic Scopus articles Resident run clinic impact factor journals Resident run clinic Scopus journals Resident run clinic PubMed journals Resident run clinic medical journals Resident run clinic free journals Resident run clinic best journals Resident run clinic top journals Resident run clinic free medical journals Resident run clinic famous journals Resident run clinic Google Scholar indexed journals Community health services articles Community health services Research articles Community health services review articles Community health services PubMed articles Community health services PubMed Central articles Community health services 2023 articles Community health services 2024 articles Community health services Scopus articles Community health services impact factor journals Community health services Scopus journals Community health services PubMed journals Community health services medical journals Community health services free journals Community health services best journals Community health services top journals Community health services free medical journals Community health services famous journals Community health services Google Scholar indexed journals Vulnerable populations articles Vulnerable populations Research articles Vulnerable populations review articles Vulnerable populations PubMed articles Vulnerable populations PubMed Central articles Vulnerable populations 2023 articles Vulnerable populations 2024 articles Vulnerable populations Scopus articles Vulnerable populations impact factor journals Vulnerable populations Scopus journals Vulnerable populations PubMed journals Vulnerable populations medical journals Vulnerable populations free journals Vulnerable populations best journals Vulnerable populations top journals Vulnerable populations free medical journals Vulnerable populations famous journals Vulnerable populations Google Scholar indexed journals Graduate medical education articles Graduate medical education Research articles Graduate medical education review articles Graduate medical education PubMed articles Graduate medical education PubMed Central articles Graduate medical education 2023 articles Graduate medical education 2024 articles Graduate medical education Scopus articles Graduate medical education impact factor journals Graduate medical education Scopus journals Graduate medical education PubMed journals Graduate medical education medical journals Graduate medical education free journals Graduate medical education best journals Graduate medical education top journals Graduate medical education free medical journals Graduate medical education famous journals Graduate medical education Google Scholar indexed journals Otolaryngology articles Otolaryngology Research articles Otolaryngology review articles Otolaryngology PubMed articles Otolaryngology PubMed Central articles Otolaryngology 2023 articles Otolaryngology 2024 articles Otolaryngology Scopus articles Otolaryngology impact factor journals Otolaryngology Scopus journals Otolaryngology PubMed journals Otolaryngology medical journals Otolaryngology free journals Otolaryngology best journals Otolaryngology top journals Otolaryngology free medical journals Otolaryngology famous journals Otolaryngology Google Scholar indexed journals Loma Linda University Medical Center articles Loma Linda University Medical Center Research articles Loma Linda University Medical Center review articles Loma Linda University Medical Center PubMed articles Loma Linda University Medical Center PubMed Central articles Loma Linda University Medical Center 2023 articles Loma Linda University Medical Center 2024 articles Loma Linda University Medical Center Scopus articles Loma Linda University Medical Center impact factor journals Loma Linda University Medical Center Scopus journals Loma Linda University Medical Center PubMed journals Loma Linda University Medical Center medical journals Loma Linda University Medical Center free journals Loma Linda University Medical Center best journals Loma Linda University Medical Center top journals Loma Linda University Medical Center free medical journals Loma Linda University Medical Center famous journals Loma Linda University Medical Center Google Scholar indexed journals SACHS Otolaryngology Department articles SACHS Otolaryngology Department Research articles SACHS Otolaryngology Department review articles SACHS Otolaryngology Department PubMed articles SACHS Otolaryngology Department PubMed Central articles SACHS Otolaryngology Department 2023 articles SACHS Otolaryngology Department 2024 articles SACHS Otolaryngology Department Scopus articles SACHS Otolaryngology Department impact factor journals SACHS Otolaryngology Department Scopus journals SACHS Otolaryngology Department PubMed journals SACHS Otolaryngology Department medical journals SACHS Otolaryngology Department free journals SACHS Otolaryngology Department best journals SACHS Otolaryngology Department top journals SACHS Otolaryngology Department free medical journals SACHS Otolaryngology Department famous journals SACHS Otolaryngology Department Google Scholar indexed journals Patients evaluation articles Patients evaluation Research articles Patients evaluation review articles Patients evaluation PubMed articles Patients evaluation PubMed Central articles Patients evaluation 2023 articles Patients evaluation 2024 articles Patients evaluation Scopus articles Patients evaluation impact factor journals Patients evaluation Scopus journals Patients evaluation PubMed journals Patients evaluation medical journals Patients evaluation free journals Patients evaluation best journals Patients evaluation top journals Patients evaluation free medical journals Patients evaluation famous journals Patients evaluation Google Scholar indexed journals parathyroidectomies articles parathyroidectomies Research articles parathyroidectomies review articles parathyroidectomies PubMed articles parathyroidectomies PubMed Central articles parathyroidectomies 2023 articles parathyroidectomies 2024 articles parathyroidectomies Scopus articles parathyroidectomies impact factor journals parathyroidectomies Scopus journals parathyroidectomies PubMed journals parathyroidectomies medical journals parathyroidectomies free journals parathyroidectomies best journals parathyroidectomies top journals parathyroidectomies free medical journals parathyroidectomies famous journals parathyroidectomies Google Scholar indexed journals
Article Details
1. Introduction
Federally Qualified Health Centers (FQHCs) are a critical part of the healthcare safety net in the United State by providing services to underserved communities. The expansion of private health insurance and Medicaid under the Affordable Care Act (ACA) has increased the number of insured patients visiting these centers from 65% in 2013 to 76% in 2015 [1,2]. While initially limited to primary care type practices, increased funding from federal grants and insurer reimbursements have allowed these centers to expand their ability to sub-specialty services such as otolaryngology [2]. To address the needs for high quality sub-specialty care, FQHCs have developed partnerships with tertiary care teaching hospitals [2]. An example of this is the partnership between the Social Action Community Health System (SACHS) located in San Bernardino, California and Loma Linda University Medical Center (LLUMC). SACHS, initially developed in the 1960’s, is an FQHC qualified community health center with the goal of providing low- to- no cost health care services regardless of patients’ employment or insurance. LLUMC is a large private academic tertiary care hospital with associated children’s hospital and allopathic school of medicine. It is the only academic tertiary care center for inland Southern California, which has a population of approximately 5 million. SACHS has been able to partner with LLUMC and its residency training programs to provide the most comprehensive services of any FQHC in the country with 30 participating adult and pediatric specialty services. Most of the patients seen in SACHS are either uninsured or have insurers or funding not contracted with the LLUMC faculty practice. In the SACHS Otolaryngology Clinic, residents maintain a semi-autonomous practice which allows for a unique training experience while providing high quality subspecialty surgical care to an underserved community. Additionally, in the SACHS Otolaryngology clinic, all sub-specialties were represented including pediatric otolaryngology, neuro-otology, facial plastics, laryngology, rhinology, and head and neck oncology. We describe the experience of delivering free to low-cost sub-specialty care to a vulnerable population through the partnership between the SACHS Clinic and the LLUMC Otolaryngology residency program and comparing the delivery and quality of care with the associated faculty practice.
Methods
After appropriate institutional review board approval, a retrospective chart review was performed on all patients seen at the SACHS Otolaryngology Department from July 1, 2017 to August 1, 2018. A total of 687 new patients were seen in SACHS clinic, of which 126 underwent surgery. A matched control cohort was compiled of patients seen at the nearby LLUMC faculty medical office (FMO) clinic during the same time period based on Current Procedure Terminology (CPT) codes. In addition to patient demographics, endpoints measured included case type, referral to consultation interval, surgical decision and date of surgery interval, as well post-surgical follow up interval. Also measured were complication rates which were defined as post-operative bleeding/hematoma, surgical site infection, need for revision surgery, readmission, or other adverse or unexpected outcomes. Data analysis was carried out in R (v 3.6.3), utilizing the Wilcox signed rank sum test for comparison of population medians as appropriate. All reported p-values are for comparison of reported medians.
SACHS Otolaryngology Clinic Description
The educational intent of the SACHS resident-led clinic is to provide residents a semi-autonomous clinic experience simulating independent practice. During 4-month blocks, fourth year residents see all new patients and develop treatment strategies with the guidance of university faculty members who are physically present in clinic. Patients evaluation and treatment, including preoperative counseling and decision for surgery, are performed solely by the resident. Once a decision for surgery is made, the case is directed to the appropriate university faculty member according to the patients’ surgical needs and the patient scheduled for surgery at LLUMC facilities under the sponsoring faculty surgeon. Once patients are listed for surgery at LLUMC, there is no distinction in care between patients from SACHS or FMO. Continuity is maintained throughout the patients’ care and residents are expected to perform or assist in the scheduled surgery with the sponsoring faculty surgeon. Residents subsequently see the patients during the post-operative period, either inpatient or outpatient, and continue follow-up care as necessary.
Results
A total of 687 new patients were seen between July 1, 2017 to August 1, 2018 at the SACHS resident clinic with an average of 65 new patients were seen per month. Out of these patients, 126 patients underwent surgery—approximately 18% of all patients. Male to female ratio among operated patients was 1.5:1 in both groups. Adult patients comprised 55% and 56% of the SACHS and FMO cohorts respectively with the remaining patients being pediatric. Cases from all sub-specialties were performed. The most common surgeries performed were tonsillectomies (44), tympanostomy tubes (22), thyroidectomies or parathyroidectomies (13), septoplasties (10), and endoscopic sinus surgeries (7) (Table 1). The median time from decision for surgery to the date of operation was 43 days for SACHS patients versus 34 days for the FMO (p<0.001). For post-operative visits, the median time from surgery to post-operative clinic appointment were 8 days and 10 days for SACHS and FMO respectively (p=0.29).
When considering subsets of common ENT procedures, tonsillectomy SACHS patients had a mean interval between decision for surgery and the operation of 52 days, with a median of 43 days, compared to a mean of 40 days and a median of 35 days at the FMO (p=0.09). Mean time for SACHS tympanostomy tube was 51 days from surgical decision to operation with a median of 43 days, compared to a mean of 43 days and a median of 34 days at the FMO (p=0.58). Septoplasty patients experienced an mean time of 63 days from decision for surgery to operation, with a median of 57 days, compared to an mean of 128 days and a median of 60 days at the FMO (p=0.38). FMO thyroidectomy patients had a statistically significant difference in time (p=0.03) compared to SACHS thyroidectomy patients, which was a median of 18 days (mean of 15 days) compared to 35 days with a mean of 41 days, respectively. In terms of endoscopic sinus surgery, SACHS patients had an improved median of 48 (mean 56) days, compared to a median of 61.5 (mean 44) days at the FMO (p=0.53). There were no significant differences in post-operative complications with only 1 post tonsillectomy bleed each from both the SACHS and FMO populations.
|
Total cases |
|
|
Tonsillectomy |
44 |
|
Tympanostomy tube |
22 |
|
Thyroid/Parathyroid |
13 |
|
Septoplasty |
10 |
|
Endoscopic Sinus Surgery |
7 |
|
Excision of Benign mass |
6 |
|
Excision of malignant mass |
6 |
|
Direct laryngoscopy with intervention |
5 |
|
Open Septorhinoplasty |
4 |
|
Tympanoplasty |
3 |
|
OCR |
2 |
|
Stapedotomy |
2 |
|
Other |
2 |
Table 1: Type of cases
|
SACHS |
FMO |
p- value |
|||
|
Median |
Range |
Median |
Range |
||
|
Referral to consultation |
40 |
0 - 162 |
38 |
0 - 136 |
0.04 |
|
Decision for surgery to operation |
43 |
41 - 105 |
28 |
3 - 454 |
<0.001 |
|
Operation to Post-operative visit |
8 |
Aug-56 |
10 |
Jun-45 |
0.29 |
|
Decision for surgery to operation for most common procedures |
|||||
|
Thyroid/ Parathyroid |
35 |
8 - 137 |
18 |
Jan-22 |
0.03 |
|
Tonsillectomy |
43 |
17 - 125 |
35 |
8 - 205 |
0.09 |
|
Tympanostomy |
43 |
11 - 267 |
34 |
8 - 202 |
0.58 |
|
Septoplasty |
57 |
18 - 99 |
60 |
16 - 153 |
0.38 |
|
Endoscopic Sinus |
48 |
7 - 133 |
61.5 |
38 - 88 |
0.53 |
Table 2: Number of days between interval visits
† Functional Endoscopic Sinus Surgery, ‡ Pressure Equalization Tubes
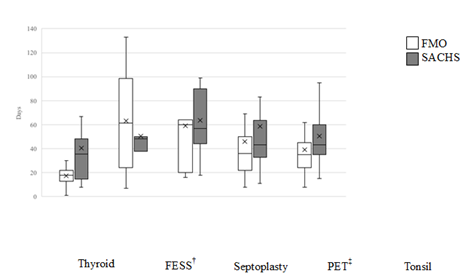
Figure 1: Median Interval Decision to Surgery Time for SACHS versus FMO Patients by Surgery Type
Discussion
Community Health Centers have existed throughout the United States for decades for the purpose of treating underserved populations. These FQHC’s traditionally focused on primary care, obstetrics, and mental care with sub-specialty services often out of reach for many. With the passage of the ACA in 2010, increased funding has allowed these centers to proliferate and expand their capabilities [2]. In 2015, roughly 1300 health centers served 24.3 million people—an increase from 19.5 million in 2010 [1,2]. Approximately 76% of FQHC patients were insured (49% through Medicaid), up from 65% in 2013 [1,2]. Nearly 1 in 12 Americans were being seen at these clinics, with 6 in 10 being women, and hundreds of thousands veterans [1,2]. FQHC facilities have sought to expand their subspecialty medical and surgical care by forming partnerships with nearby hospitals and community mental health organizations [2]. Partnerships between FQHC’s, like the SACHS clinic in San Bernardino, CA, and larger institutions provide unique learning opportunities for residency programs while also providing previously unattainable sub-specialty care to medically underserved population. Previous studies have shown that resident-directed or resident-run clinics are highly beneficial in developing resident autonomy in a safe, effective manner [3-6]. Currently however, no studies have examined the effectiveness or clinical outcomes of an ENT resident-led clinic. For decades, many plastic surgery programs have incorporated resident-led aesthetic clinics with similar semi-autonomous models into their training in an effort to meet required key indicator cases [7-10]. Many program directors and plastic surgery residents consider these experiences invaluable for their training—particularly in developing autonomous decision making and operative skills—regardless of their final career goals [6]. Additionally, resident led surgery clinics provides an ideal environment to enhance knowledge in systems- based practice, patient care, communication skills, and professionalism [7-10]. Wojcik et al. showed that residents experienced significant improvements in both surgical skills and confidence in surgical ability during a rotation at a resident-run procedure clinic wherein residents were solely responsible for performance of various soft tissue procedures [5]. However, the longitudinal educational value of this resident-run experience was limited by lack of resident involvement in either pre-procedure consultation or post-procedural follow up. Witherspoon et al. similarly showed that a resident-run Urology clinic resulted in high levels of resident confidence in patient management, with low rates of changes in patient management following faculty review [6]. While previous studies have shown resident-run clinic to provide patient care with complication rates and satisfaction scores equivalent to national outcomes—similar to the findings of this paper—the effectiveness of the coordination of patient care in a resident run clinic has not been established [10-12]. This study demonstrates overall comparable outcomes in delivery of Otolaryngology sub-specialty care between the resident-run, SACHS clinic population and the mostly privately insured population of LLUMC faculty clinic. This was evident in time of referral to consultation as well as interval of time between decision for surgery and date of operation, and subsequent post-operative visits. While the overall median interval time to surgery was statistically significantly increased for SACHS patients, analysis by surgery type showed predominantly equivalent times between decision for surgery and the surgery itself. Interval times were only minimally increased for SACHS patients with notable exceptions being markedly—although not statistically significantly—decreased interval times for SACHS patients requiring endoscopic sinus surgery and a nearly doubled interval time to surgery for those requiring thyroid or parathyroid surgery. The latter discrepancy—the only subgroup to reach statistical significance—is likely attributable to the Loma Linda University Thyroid Center—a very high-volume practice of a single faculty surgeon with low participation with the SACHS clinic. On further review of outliers for median time interval were typically due to a variety of patient factors (e.g. preference, need for medical clearance, etc.).
There are noteworthy limitations to the strength of conclusions that can be made from this study. Firstly, surgical scheduling and insurance approval is done separately from the standard electronic medical record and thus the direct contribution of insurance status or provider on time to surgery was unable to be assessed. Additionally, as with any retrospective study, data is limited by the completeness of medical documentation and there exists potential bias in treatment and outcomes due to non-randomization of patients. Lastly, the relatively small sample size with heterogeneous patient populations both introduces potential selection bias as well as limiting the ability to accurately detect statistical significance between groups.
Conclusion
Community FQHC sites which are poised to provide more comprehensive access rather than basic primary care. The experience of our Otolaryngology specialty clinic demonstrates that partnerships between academic centers and FQHC sites allow for effective delivery of sub-specialty surgical care, comparable to that seen in university clinics, to populations previously under-served.
Funding
This study was carried out without any internal or external funding.
Conflict of interest
The authors have no conflicts of interest to report.
References
- Shin P, Sharac J, Rosenbaum S. Community Health Centers and Medicaid At 50: An Enduring Relationship Essential For Health System Transformation. Health Aff (Millwood) 34 (2015): 1096-1110.
- Paradise J, Markus A, Sharac J, et al. Community Health Centers: Recent Growth and the Role of the ACA. Mediaid 12 (2017): 67.
- Wojcik BM, Fong ZV, Patel MS, et al. The Resident-Run Minor Surgery Clinic: A Pilot Study to Safely Increase Operative Autonomy. J Surg Educ 73 (2016): e142-e149.
- Jarman BT, O'Heron CT, Kallies KJ, Cogbill TH. Enhancing Confidence in Graduating General Surgery Residents: Establishing a Chief Surgery Resident Service at an Independent Academic Medical Center. J Surg Educ 75 (2018): 888-894.
- Wojcik BM, McKinley SK, Fong ZV, et al. The Resident-Run Minor Surgery Clinic: A Four-Year Analysis of Patient Outcomes, Satisfaction, and Resident Education. J Surg Educ 3 (2021): S1931
- Witherspoon L, Jalali S, Roberts MT. Resident-run urology clinics: A tool for use in competency-based medical education for teaching and assessing transition-to-practice skills. Can Urol Assoc J 13 (2019): E279-E284.
- Ingargiola MJ, Molina BF, Yao A, et al. Plastic Surgery Resident-Run Cosmetic Clinics: A Survey of Current Practices. Aesthet Surg J 38 (2018): 793-799.
- Qureshi AA, Parikh RP, Myckatyn TM, et al. Resident Cosmetic Clinic: Practice Patterns, Safety, and Outcomes at an Academic Plastic Surgery Institution. Aesthet Surg J 36 (2016): NP273-280.
- Weissler JM, Carney MJ, Yan C, et al. The Value of a Resident Aesthetic Clinic: A 7-Year Institutional Review and Survey of the Chief Resident Experience. Aesthet Surg J 37 (2017): 1188-1198.
- Hultman CS, Wu C, Bentz ML, et al. Identification of Best Practices for Resident Aesthetic Clinics in Plastic Surgery Training: The ACAPS National Survey. Plast Reconstr Surg Glob Open 3 (2015): e370.
- Buchanan TR, Johns EA, Massad LS, et al. A fellow-run clinic achieves similar patient outcomes as faculty clinics: A safe and feasible model for gynecologic oncology fellow education. Gynecol Oncol 159 (2020): 209-213.
- Shin P, Sharac J, Rosenbaum S. Community Health Centers And Medicaid At 50: An Enduring Relationship Essential For Health System Transformation. Health Aff (Millwood) 34 (2015): 1096-1104
