Design of a Challenging Prosthetic Fitting Process and Rehabilitation Training Program to Achieve Functionality in a Complex Quadruple Amputee
Article Information
Raquel Madroñero-Mariscal1,2*, Natalia Palmero-Valdez3, Emilio González-Parra4, Raúl Ramos Izquierdo5, Ricardo Marcelino5, María Pérez-Cuesta Llaneras3, Barbara Nasarre3, Almudena Fernández-Bravo Rueda3, Elisa López-Dolado1,6 and Danielle H Melton7,8
1Rehabilitation Department and Laboratory of Interfaces for Neural Repair (LINER), Hospital Nacional de Parapléjicos, Toledo, Spain
2Rehabilitation Department, Fundación del Lesionado Medular, Madrid, Spain
3Rehabilitation Department, Hospital Universitario Fundación Jiménez Díaz, Madrid, Spain
4Nephrology Department, Hospital Universitario Fundación Jiménez Díaz, Madrid, Spain
5Center for Prosthetics Orthotics PRIM, Madrid, Spain
6Associate Professor, Department of Medicine and Medical Specialities, School of Medicine, Universidad de Alcalá (UAH), Madrid, Spain
7Director of the Amputee and Orthotics and Prosthetics Program at TIRR Memorial Hermann, Houston, Texas, USA
8Assistant professor at the University of Texas Health Science Center-Houston, USA
*Corresponding Author: Raquel Madroñero-Mariscal, Rehabilitation Department, Hospital Nacional de Parapléjicos, Toledo, Spain.
Received: 12 January 2023; Accepted: 23 January 2023; Published: 03 February 2023
Citation: Raquel Madroñero-Mariscal, Natalia Palmero-Valdez, Emilio González-Parra, Raúl Ramos Izquierdo, Ricardo Marcelino, María Pérez-Cuesta Llaneras, Barbara Nasarre, Almudena Fernández-Bravo Rueda, Elisa López-Dolado and Danielle H Melton. Design of a Challenging Prosthetic Fitting Process and Rehabilitation Training Program to Achieve Functionality in a Complex Quadruple Amputee. Archives of Clinical and Medical Case Reports 7 (2023): 44-57.
View / Download Pdf Share at FacebookAbstract
Purpose: Despite the increase in the technological prosthetics development, there is no consensus to decide the best fit for amputees. The aim of the present case report is creating a comprehensive guide to choose the best prosthetic option for a quadruple amputee, focusing on the prosthetic fitting process and rehabilitation.
Methods: A novel TASKA terminal device for the myoelectric prosthesis for transradial right upper limb amputation was the key to do the training for activities of daily life and recover independence. The rehabilitation program was vital to achieve the objective.
Results: The prosthetic chosen options and the rehabilitation plan resulted in a useful and aesthetically acceptable option. After training, there was an improvement on PLUS-M, DASH Scale, Barthel Index and EQ-D-VAS Scale, all related to the patient wearing prostheses.
Conclusions: In order to regain this patient’s basic functions, it was important to start the training with the right upper limb. The TASKA terminal device, recently made available in Spain, has helped her with the donning and doffing of her lower limb prostheses. No prosthetic for left partial amputated hand was needed. As for the lower extremities, microprocessor knees with stance control for safety have demonstrated to be the most appropriate.
Keywords
Amputee; Microprocessor Knees; Prostheses; Rehabilitation; TASKA Terminal Device
Amputee articles; Microprocessor Knees articles; Prostheses articles; Rehabilitation articles; TASKA Terminal Device articles
Amputee articles Amputee Research articles Amputee review articles Amputee PubMed articles Amputee PubMed Central articles Amputee 2023 articles Amputee 2024 articles Amputee Scopus articles Amputee impact factor journals Amputee Scopus journals Amputee PubMed journals Amputee medical journals Amputee free journals Amputee best journals Amputee top journals Amputee free medical journals Amputee famous journals Amputee Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Microprocessor Knees articles Microprocessor Knees Research articles Microprocessor Knees review articles Microprocessor Knees PubMed articles Microprocessor Knees PubMed Central articles Microprocessor Knees 2023 articles Microprocessor Knees 2024 articles Microprocessor Knees Scopus articles Microprocessor Knees impact factor journals Microprocessor Knees Scopus journals Microprocessor Knees PubMed journals Microprocessor Knees medical journals Microprocessor Knees free journals Microprocessor Knees best journals Microprocessor Knees top journals Microprocessor Knees free medical journals Microprocessor Knees famous journals Microprocessor Knees Google Scholar indexed journals Ultrasound articles Ultrasound Research articles Ultrasound review articles Ultrasound PubMed articles Ultrasound PubMed Central articles Ultrasound 2023 articles Ultrasound 2024 articles Ultrasound Scopus articles Ultrasound impact factor journals Ultrasound Scopus journals Ultrasound PubMed journals Ultrasound medical journals Ultrasound free journals Ultrasound best journals Ultrasound top journals Ultrasound free medical journals Ultrasound famous journals Ultrasound Google Scholar indexed journals Prostheses articles Prostheses Research articles Prostheses review articles Prostheses PubMed articles Prostheses PubMed Central articles Prostheses 2023 articles Prostheses 2024 articles Prostheses Scopus articles Prostheses impact factor journals Prostheses Scopus journals Prostheses PubMed journals Prostheses medical journals Prostheses free journals Prostheses best journals Prostheses top journals Prostheses free medical journals Prostheses famous journals Prostheses Google Scholar indexed journals Laryngoplasty articles Laryngoplasty Research articles Laryngoplasty review articles Laryngoplasty PubMed articles Laryngoplasty PubMed Central articles Laryngoplasty 2023 articles Laryngoplasty 2024 articles Laryngoplasty Scopus articles Laryngoplasty impact factor journals Laryngoplasty Scopus journals Laryngoplasty PubMed journals Laryngoplasty medical journals Laryngoplasty free journals Laryngoplasty best journals Laryngoplasty top journals Laryngoplasty free medical journals Laryngoplasty famous journals Laryngoplasty Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals SRAS-CoV-2 articles SRAS-CoV-2 Research articles SRAS-CoV-2 review articles SRAS-CoV-2 PubMed articles SRAS-CoV-2 PubMed Central articles SRAS-CoV-2 2023 articles SRAS-CoV-2 2024 articles SRAS-CoV-2 Scopus articles SRAS-CoV-2 impact factor journals SRAS-CoV-2 Scopus journals SRAS-CoV-2 PubMed journals SRAS-CoV-2 medical journals SRAS-CoV-2 free journals SRAS-CoV-2 best journals SRAS-CoV-2 top journals SRAS-CoV-2 free medical journals SRAS-CoV-2 famous journals SRAS-CoV-2 Google Scholar indexed journals TASKA Terminal Device articles TASKA Terminal Device Research articles TASKA Terminal Device review articles TASKA Terminal Device PubMed articles TASKA Terminal Device PubMed Central articles TASKA Terminal Device 2023 articles TASKA Terminal Device 2024 articles TASKA Terminal Device Scopus articles TASKA Terminal Device impact factor journals TASKA Terminal Device Scopus journals TASKA Terminal Device PubMed journals TASKA Terminal Device medical journals TASKA Terminal Device free journals TASKA Terminal Device best journals TASKA Terminal Device top journals TASKA Terminal Device free medical journals TASKA Terminal Device famous journals TASKA Terminal Device Google Scholar indexed journals Treatment articles Treatment Research articles Treatment review articles Treatment PubMed articles Treatment PubMed Central articles Treatment 2023 articles Treatment 2024 articles Treatment Scopus articles Treatment impact factor journals Treatment Scopus journals Treatment PubMed journals Treatment medical journals Treatment free journals Treatment best journals Treatment top journals Treatment free medical journals Treatment famous journals Treatment Google Scholar indexed journals
Article Details
1. Introduction
Limb loss can affect people of any age, gender, race or socioeconomic status. There are almost 2 million people in the USA who suffer an amputation (185.000 new cases per year, which corresponds to more than 500 new cases every day), and nearly most of them are able to enjoy a real active life. The main causes of limb loss are: vascular diseases (54%), especially due to diabetes mellitus, and trauma injuries (44%). There are other rarer conditions which can also lead to an amputation such as: cancer (1%) or congenital anomalies (1%) [1]. Limb loss by amputation affects body image perception and function greatly, and the condition worsens as amputation level and the number of involved limbs increase [2,3]. In order to solve this problem, nowadays physicians can dispose a wide range of prosthetic solutions. For a prosthetic knee for a lower limb loss, physicians can choose between multiple options such as: bolt or latch prosthetic knees, which are blocked in extension while walking providing safety during single leg support; monoaxial friction prosthetic knees or polyaxial prosthetic knees, which allow to bend and extent the knee during walking providing a more physiological way throught gait; fluid control prosthetic knees, which allow to adapt to different speed while walking; or electronic control prosthetic knees, which are known as “smart knees”, as their included microprocessor can supply a wider range of gait, providing a greater speed and less effort while walking [4]. These last ones have demonstrated to be superior to non-microprocessor knees because they decrease the number of trips and falls [5-9]. However, even when some clinical practice guidelines try to help physicians to choose between the multiple feet prosthetic options (for example with single axis foot, providing greater stability for patients walking at a single speed with weak knee extensor muscles and poor balance, or energy-storage-and-return foot, for patients at risk for overuse injuries, or for patients capable of changing speed through walking) [10],) it is obvious for the authors that, with the number of prosthetic feet available at orthopaedic market, it is not easy to choose between them. This same wide variety of options needs to be faced when choosing a prosthesis for an upper limb loss, as well. Moreover, there is a current increasing trend of technological development of prostheses which offers multiple prosthetic fitting options, but there is no consensus or algorithm to follow in order to decide which should be the best prosthesis to fit individuals with limb loss. Furthermore, it gets more challenging when there are multiple limbs involved, especially when involving upper levels. The various myoelectric upper limb prostheses available today allow an increasing quantity and quality of movement. Strategies to improve their functionality include target muscle reinnervation (TMR), a sophisticated surgical procedure for high-level arm amputees that takes the nerves previously dedicated to hand, wrist or elbow movement and re-routes them to adjacent muscles. This amplifies the nerve signals and thus improves the neural control of its myoelectric prosthesis by its user [11,12]. Current myoelectric prostheses for disarticulation levels above the elbow and shoulder allow three degrees of freedom: flexion and extension of the elbow, inward or outward rotation of the wrist, opening and closing of the hand or electronic end device. These movements are controlled by electrical signals from one or two muscle points (known as "EMG points") in the residual limb or upper shoulder area individually and separately. TMR surgery creates additional EMG sites that are controlled by distinct and intuitive muscle contractions, some of which can occur simultaneously and with less mental effort. When this technique is combined with occupational therapy, the result is a high level of intuitive control and a significant improvement in the functional use of the prosthesis. Achieving this improved functionality will be an imperative goal going forward, as researchers and manufacturers are investing enormous efforts in creating additional degrees of freedom in prosthetic systems, which will require additional EMG sites to fully optimize their increasing complexity and capability. Another way to look for the same effect of developing motion in a more natural way includes the recognition technology for prosthetic hand control [13]. Ottobock has recently marketed their system Myo Plus, which consists of a ring of 8 electrodes (instead of 2) that are placed on the residual muscles of the amputated stump, generating maps of muscular movements generated with natural movements. For example, the movement map for a supination movement is completely different than the movement map for a clamp movement, as it involves precision. Even when the patient does not notice it, there is a drawing generated and captured by the system, consequently associated with the generation of a natural movement and later on translated to a movement in the prosthetic hand, quickly generating a very similar movement without the need for co-contractions or other unnatural strategies to check the prosthesis [14]. Another current example of a commercially available advanced prosthesis is the LUKE arm from Mobius Bionics, the only commercially available prosthesis with a motorised shoulder (up to 10 motorised joints), which allows a shoulder-width amputee to reach above his or her head. It also has an intuitive arm movement control interface via the wireless "IMU" foot placed in the user's shoes, which, by reading the tilt of the foot, is able to interpret and control every functional movement of the arm. The wrist fluidly combines flexion and extension with ulnar and radial deviation, allowing users to grip objects above the head or below the waist while keeping the hand level. As for its hand grip features, they include power grip, tool grip, closed fine grip, open fine grip, side grip and chuck grip [15,16]. There are some studies that have tried to systematize the management of the rehabilitation of multiple limb amputees. Their general recommendation is to transfer these patients to specialized facilities where physicians who might be able to find further injuries will examine them. At the very beginning of the rehabilitation program, the main concerns would be to successfully perform the stump bandaging, to manage the stump and phantom limb pain, and to achieve the stump desensitization. At the first pre-prosthetic phase, the principal goals should be the preservation of strength and range of motion in order to achieve an early ambulation and to change the dominance if necessary; some authors prefer to use traditional adaptations for doing activities of daily life, instead of the imposition of an artificial behavior with the use of a prosthesis to recover the ability of an autonomous ambulation and independent driving, as well as to treat psychological disorders that may appear due to the new condition (isolation, decreased sexual activity, depression, alcohol abuse). Many of these guidelines support that bilateral transfemoral individuals with limb loss will require the use of a wheelchair, especially if upper limbs are affected too, due to the walking energy cost with the use of prostheses. At the prosthetic phase, the vast majority of studies support that rehabilitation of lower limbs needs to be delayed for at least two weeks before the beginning of weight loading and always when proper healing has been attained, whereas rehabilitation of the upper limbs should start as soon as possible even with a temporary upper limb prosthesis. Moreover, these studies defend that it is preferable to start upper limb training with a body powered prosthesis, thought the patient finally would be destined to wear a myoelectric prosthesis and even considering that the training rehabilitation is completely different in both prosthesis options, since (those works) state that a delay in the beginning of the rehabilitation of the upper limb would be damaging [17]. The aim of this study is to describe the prosthetic chosen options and the physical treatment plan to achieve the restoration of the function in this particular patient, a quadruple amputee with a septic diagnostic. This article intends to describe an innovative approach that the readers may not have seen before. The presented rehabilitation training program has been based in some non-usual treatment methods for amputee patients such as Vojta therapy, here is presented as a key tool, particularly at the initial part of the training. Vojta therapy provides a neurophysiologic facilitation system to recover the reflex residual locomotion which is lost in different diseases, such as the ones that affect the central or peripheral nervous coordination systems, myopathies, or neuromuscular and orthopaedic disorders, as it occurs in complex amputee patients. The choice of the Vojta therapy is based on the evidence of some authors such as Bauer H., et al, 1992, whose work has proved that Vojta therapy enhances the EMG-detection [18], as well as has further positive results promoting the activation of some brain structures as ipsilateral putamen that take part in different strategies of coordination as opposed to other traditional strategies not including Vojta therapy [19]. Other innovative treatment methods that are described within the present rehabilitation plan are:
- Motor imagery and action observation, consisting in the mental planning of the execution of a movement (motor imagery) while the patient is physically seeing the execution of that movement (action observation), without any overt movement or peripheral muscle activation. This is supposed to lead to the activation of the same brain areas of actual movement [20] and is considered to improve the motor performance of the patient by developing a brain plasticity into the premotor cortex and parietal lobule, which should enhance the global motor function [21].
- Virtual reality, as a technological tool that helps motor skills learning through multimodal sensory information. It has been extensively used in neurological rehabilitation to improve motor skills of patients by providing an individualized and interactive environment that may increase the motivation of the patient when performing motor tasks [22]. In the same way that virtual reality has shown improvements in rehabilitation outcomes of neurological disorders such as Parkinsons’ Disease [23] or spinal cord injury [24], when comparing to traditional rehabilitation methods, the authors of the present work have used this innovative tool to promote a greater motor control by pursuing a neurological training.
- Balance training using a stabilometric force platform including visual biofeedback task-specific balance training: this method of balance training has been successfully demonstrated as optimal when compared with traditional stand-alone gait training methods, in other disorders in which the balance of the patient is altered, as in spinal cord injuries [25]. Because of the need of balance training due to the lack of proprioception in a quadruple amputee patient, this approach suits the present treatment plan accordingly.
This study tries to show the approach of the authors to an innovative management of the rehabilitation training of a complex amputee that combines the new options available thanks to the development of new technological rehabilitation tools with a specific neurological focus training, leaving behind the classical ideas of pursuing an early ambulation as the main principle goal of these patients, as well as changing dominant hand and avoiding the use of a wheelchair for bilateral transfemoral amputees, or using body-powered prostheses for an early upper limb training, as the described tools will provide physicians with new approaches for better outcomes. The pioneering TASKA TD applied to the myoelectric prosthesis on the upper limb transradial amputation of the patient had an important role as the central axis for success on gaining independence. It was also determinant to overcome some other difficulties, namely economical, psychological and further medical complications secondary to the sepsis.
2. Case Report
2.1 Patient Description
54-year-old Caucasian female, with unremarkable medical history, admitted to the Intensive Care Unit of the Hospital Universitario Fundación Jiménez Díaz on November 22nd, 2018 due to septic shock with multiple organ failure (hemodynamic, kidney, hepatic and respiratory failure). She required invasive mechanical ventilation and support with vasoactive drugs. Afterwards, she suffered from toxic shock with extensive epidermolysis and ischemia of the four limbs, as well as nasal ischemia, requiring bilateral above-knee amputation on December 17th, 2018. Later on, due to irreversible ischemia (Figure 1), a transradial amputation of the right upper limb, as well as partial amputation of the left hand (distal phalanx of first finger and distal and middle phalanges of 2nd, 3rd, 4th and 5th fingers) had to be performed on February 4th, 2019. Secondary complications included intensive anaemia that required transfusions; percutaneous tracheostomy on December 4th due to the collapse of the left and right lower pulmonary lung lobe, weakness of the right hemidiaphragm, which required respiratory rehabilitation techniques; reactive depression; hepatic failure finally solved; bilateral kidneys cortical necrosis causing an important renal insufficiency which initially required haemodialysis; initial isolation because of multiresistant bacterias; and strong phantom limb pain at every stump.

Figure 1: Amputation levels: a) and b) left partial hand amputation, c) right transradial upper limb amputation, d) bilateral above knee amputation.
2.2 Rehabilitation Training Program
2.2.1 Therapy Goals and Intervention: The patient rehabilitation program included 2,5 hours of physical therapy and 2 hours of occupational therapy every day. The patient was admitted at the hospital for 11 months (Table 1). The authors provided the patient with an informed consent document in order to be able to show the main aspects of this work in depth. The therapy goals and interventions are summarized in Table 2
|
Nov-18 |
Septic shock |
|
Dec-18 |
Bilateral above knee amputations |
|
Feb-19 |
Bilateral upper limb amputations |
|
Feb-19 |
Pre-prosthetic phase started |
|
May-19 |
Lower limb prosthetic phase started |
|
Nov-19 |
Upper limb prosthetic phase started |
Table 1: Case Timeline.
2.2.2 Pre-prosthetic Phase: The first main treatment consisted on respiratory rehabilitation techniques aimed to restore the respiratory function. Then, physical therapy with reflex locomotion therapy from Vojta technique was proven useful to activate motor function and to initiate the body trunk straightening using proprioceptive stimuli [18,19,26]. This therapy helped her to improve the awareness of her body, facilitating body balance and getting used to her new body dimensions. This technique was especially useful for improving her diaphragmatic activity at the beginning, using the pectoral point as a triggering area of proprioceptive stimulus. This technique has also been adjuvant for decreasing low back pain [27]. Immediately after that, the therapy swifted to the mobilization of the four stumps and the design of a training plan to start rehabilitation in the patient’s bed. For this purposes, the Motor Imagery (MI) and Action Observation (AO) training techniques were applied. This allowed the pursuing of the activation of mirror neurons in response to auditory stimulation and emotional expressions [28-31], in order to achieve the construction of motor memory [32]. The reason for combining MI and AO instead of using AO alone was to achieve a greater activation of the parietal cortex, the supplementary motor area, the caudate nucleus and the cerebellum [33,34]. For this purpose, a 360º camera and a mobile phone were used to record video exercises, along with virtual reality glasses (VG) as well as an iPod, to make the recording available for the patient (Figure 2). Those videos had a double function: first, to apply the MI/AO technique in order to allow the patient to achieve a faster aesthetical acceptance of her current condition. The focus of the videos was on the simulation of amputated limbs, for the movements to be used as OA with the addition of mental practice (MI) [35-38]. The second function was to advance the strengthening, since the sooner the patient was trained, the better practice of the exercises of action execution (AE). The patient practiced, in her bedroom, 10 repetitions of each exercise 2 times a day each morning and 2 times a day each afternoon. During the stump remodeling with bandages, the patient presented an allergic reaction to the material of the bandages, so the stump care had to be swifted in order to determine her sensitivity to different textures such as electric toothbrush sensation, requiring the use of hypoallergenic bandages for the stumps. Along with this, she required massage therapy in order to activate circulation, recover sensitivity, and start the motor function of the upper limb stumps. Afterwards, the patient started to develop body trunk control and was prepared to start training at the main rehabilitation area outside her room, with isolation measures (given her multiresistant bacteria colonization) at first. At the rehabilitation gym, the training started with verticalization in an adapted inclined plane with the addition of wedges at the bottom to maintain the correct body positioning. Before applying any other physical therapies, the treatment focused on Vojta techniques in order to activate the body muscles to facilitate the action of the stabilizing muscles, which are necessary to reach a correct posture control of the body trunk, while other muscles accomplished a directed task. The goal of this technique was to improve the proprioceptive sensation of her new body condition to easily achieve self-movement for transfers. Those exercises were designed to achieve pelvic, trunk and scapular muscle straightening. Before next phase, she also trained creep and turns to learn transfers to decubitus, as well as body balance during sitting, and strategies to transfer supports. Then, she trained standing on the stumps with the use of vestibular training whilst keeping balance on an unstable surface with open and closed eyes (static balance). Lastly, the training included motor control with virtual glasses, also walking on a stretcher with the use of an overhead crane and harness. These combined activities (Figure 3) helped her to learn how to move independently without prosthetics at this stage. In addition to all of the above, the training included exercises of therapeutic Pilates. From the beginning (bedding phase) through the pre-prosthetic phase, including the adaptation to her new body image (Figure 4a), until the prosthetic phase (Figure 4b), the patient carried out activities that include the vestibular system and proprioception. The vestibular training included a MI training achieved with the VG which provide virtual scenarios consisting of car and bus sitting rides and standing and walking on the beach. It was also important not to forget to train the motor skills of the upper limbs, which enabled the patient to be successful through the next phases. Five months before starting the prosthetic right upper limb training, the therapy was completed with the use of the Mio boy training system, a motor sensor program designed to activate and train the muscles that would be on charge of controlling TASKA TD right upper myoelectric prosthetic movements, simulating movements of wrist bending and extension, hand opening and closing, and clamp function. For this purpose, the VG training was particularly useful to simulate a prosthetic hand while she trained the muscle activation (Figure 2).
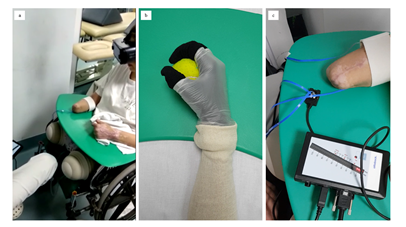
Figure 2: Rehabilitation training for the right upper limb pre-prosthetic phase with the synchronized combination of motor imagery and action observation: a) motor imagery with virtual glasses which allows the b) action observation of the virtual movement of the hand, and at the same time, c) the trainer controlled the correct action execution with the Mio boy motor sensor system which identified the activation of the muscles that synchronously corresponded to her hand observed virtually image movement.

Figure 3: Combined activities at strengthen training program.
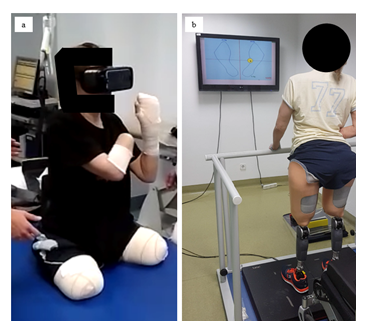
Figure 4: Vestibular and proprioceptive rehabilitation training program: a) Virtual reality at pre-prosthetic phase, b) Training dynamic balance with a stabilometric balance platform at prosthetic phase.
|
Phases |
Exercises |
Goals |
|
|
Pre-prosthetic phase |
First phase (March 2019) |
- Exercises to maintain proper joint’s range of motion. (sets: 4; repetitions: 10; once a day) - Exercises to strengthen the muscle chains, with the aid of Vojta therapy, Motor Imagery, Action Obsevation and Action Execution. (Figure 2). (Vojta Therapy: sets: 1; 3 times per week) (Motor Imagery, Action Observation and Action Execution: sets: 2; repetitions: 10, 4 times per week) - Strategies to work transfers. - Verticalization. - Stumps’ care measures: to promote wound healing, to avoid pain, to ensure a proper blood supply, to mold the stump. |
- To restore the respiratory function. - To start activating muscle chains at supine and lateral decubitus position. - To achieve aesthetical acceptance to current body appearance. |
|
Second phase (April 2019 - May 2019) |
- Exercises to progressively strengthen the pelvic, trunk and scapular muscle chains, with previous training with Vojta techniques. (sets: 4; repetitions: 10; once a day) - Creep and turns exercises and combined activities. (Figure 3). (1 time per day, 3 days per week). - Body balance exercises during sitting position and exercises to train strategies to transfer supports. (Figure 4a). (1 time per day, 3 days per week). - Body balance standing on the stumps with the use of vestibular training keeping balance on an unstable surface with open and closed eyes (static balance), and motor control with virtual glasses, also walking on a stretcher with the use of an overhead crane and harness. - Therapeutic Pilates. (sets: 2; repetitions: 10; twice a week) - Exercises with Mio boy training system, to activate and train the muscles that would be on charge of controlling TASKA TD right upper myoelectric prosthetic movements, with the aid of VG training. (sets: 2; repetitions: 15; three days per week) |
- To improve the proprioceptive sensation of her new body condition to easily achieve self-movement for transfers. - To learn transfers to decubitus. - To train balance prior to prepare for gait training. - To move independently at home without prostheses. - To prepare right upper limb for prosthetic phase. |
|
|
Prosthetic phase |
Third phase (June 2019 - December 2019) |
- Gait training with lower limb prosthesis: · Firstly, training started with her knees blocked in extension to work on a static balance performing a postural control and learning to change charges from one side to another. · One week later, she trained with a slight bending of the knees to start learning how to get sit and up and we started her first steps at parallels. (repetitive activities [squats, supports on a step...] were performed to reach an increasingly slow and subtle movement which was recorded by the MPKs) · To walk out of parallels with the help of two crutches, (right crutch adapted for forearm). · To work on steps, how to get off the ground, and walking on a treadmill hung on harness. - Balance training exercises using the stabilometric balance platform. (Figure 4b). |
- To prevent from fallings. - To walk short distances independently. - To correct step length and to remove technical aids. - To achieve autonomous transfers. - To train dynamic balance. |
|
Fourth phase (January 2020 - February 2020) |
- To train the use of every prostheses at the same time. - To train activities of daily life. - To train activities with Taska TD (writing, dressing, bimanual tasks…). |
- To achieve bimanual tasks reaching independence in activities of daily life. - To get used to wear every prostheses. |
|
Table 2: Rehabilitation program timeline.
2.2.3 Prosthetic Phase: For the prosthetic legs, prosthetic phase began 5 months after lower limbs amputations. For the prosthetic arm, it began 9 months after upper limb amputations. The goals of this phase were to facilitate the achievement of independence and autonomy in activities of daily life. The features of the prostheses are summarized in Table 3.
|
LIMB |
PROSTHESIS |
TYPE OF SOCKET |
INTERFACE MATERIAL |
SUSPENSION |
LENGTH (limb +fitted prosthesis) |
|
RUL |
TASKA TD |
Munster |
silicone |
vacuum suspension |
73 cm |
|
LUL |
No Prosthesis |
- |
- |
- |
64 cm |
|
RLL |
Rheo MPK + Avalon K2 foot |
quadrangular |
silicone |
vacuum suspension with hypobaric membrane |
95 cm |
|
LLL |
Rheo MPK + Avalon K2 foot |
quadrangular |
silicone |
vacuum suspension with hypobaric membrane |
95 cm |
Table 3: Prostheses features.
RUL- Right Upper Limb; LUL- Left Upper Limb; RLL- Right Lower Limb; LLL- Left Lower Limb; MPK- Microprocessor Knee; TD- Terminal Device.
2.2.4 Bilateral above Knee Lower Limb Prostheses. Rheo MPK with Avalon K2 Feet: The standing and gait stability training was started using her definitive prosthesis. The choice for the knee joints was two Rheo MPK with stance control for safety, as it has been proven that is a superior system when compared with non-microprocessor-controlled (mechanical) knee joints (NMPK); for MPK reduces the number and frequency of stumbles and falls, especially for bilateral amputees. The choice for the feet was two Avalon K2 feet, with a hydraulic design that allows the adaptation to inclinations by its self-aligning, designed to secure the knee prostheses’ joints, providing good posture and joint position. Those feet allowed to enhance stability and a balanced limb loading while walking. The TASKA TD was not implemented until 9 months after upper limb amputation, therefore at the very beginning the patient required help for the donning of her lower limb prostheses. The training started with the knees blocked in extension to work on a static balance performing a postural control and learning to change charges from one side to another. One week later, a slight bending on the knees was introduced in order for the patient to start learning how to sit down and stand up; this is the moment when the patient began her first steps at parallels. The learning process in the use of these MPKs consisted on performing repetitive activities (squats, supports on a step...) to reach an increasingly slow and subtle movement which was recorded by the MPKs. This process allowed the patient to develop a suitable time of reaction to prevent from fallings. Once this was achieved, the gait training was taken out from the parallels with the aid of two crutches, including a right crutch adapted for forearm support. Working on a stabilometric balance platform was helpful to achieve dynamic balance (Figure 4b). The training then focused on steps, how to get off the ground, and walking on a treadmill with harness support to correct step length. At this stage, the removal of one crutch was attained. At the end of this stage, the patient achieved an independent walking with two crutches, as well as autonomous transfers for sitting down and standing up.
2.2.5 Right Upper Limb Prosthesis. Myoelectric Prosthesis with an Innovative TASKA TD: A TASKA TD was chosen for her right myoelectric prosthesis. The TASKA TD, recently launched in the Spanish market, allows for an almost ‘plug and play’ fitting with easy access to 7 different grip patterns, even with non-power users. The programming settings allow for both one and two electrodes’ commands, signal gain and smoothing, toggle between grips with EMG pattern signals, direct grip access through dorsal buttons with a total of 14 possible grip patterns out of a total of 23 grip patterns available. Apart from all these functionalities, it can empower the patient with personalized grip patterns, programmed by the user him or herself, with the possibility of sharing it at an online TASKA user’s community, using the built-in Bluetooth connection to download the data to a smartphone, tablet or PC. Each user can select and test different grips with a ‘drag and drop’ functionality and select the order in which these come to use while toggling through in an alternating manner (Figure 5). As her dominant arm was the left one, the main goal of this right upper limb was to be integrated into her daily activities in order to achieve bimanual tasks for her independence in activities of daily life: cutting food with a knife (Figure 6d), hold things like a bottle of water while opening it (Figure 6f). It needed to be able to perform delicate tasks such as moving an egg to a bowl (Figure 6b), type on a computer (Figure 6g), handwriting (Figure 6h), among others; but also, was required to be able to manipulate heavy things such as an iron (Figure 6i). At the time, this hand TD was the only one which was waterproof so it could be used for cooking or cleaning tasks without risk of damage (Figure 7a). Another important feature was the protection of the fingers with a resistant knuckle cover which could support her weight to stand up making a grip without the risk of damaging fingers (Figure 7b). This TD was also very important to achieve her independence in donning and doffing her leg prostheses by herself, and walking alone (Figure 6k and 6l).
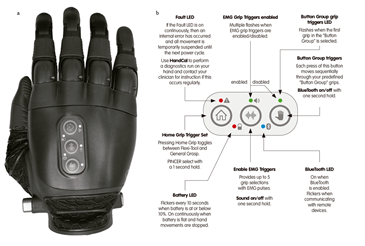
Figure 5: TASKA programming. a) TASKA TD, b) quick map of buttons and light-emitting diodes (LEDs).
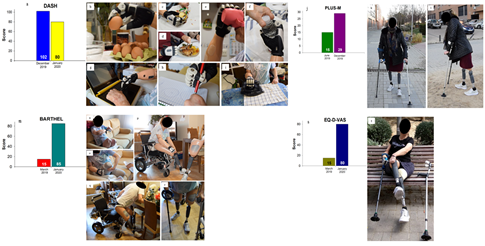
Figure 6: Assessment Scales and functional outcomes: a) Decrease of difficulties in upper limb tasks measured by DASH Scale. Bimanual tasks permitted due to features of TASKA TD: b) dextrous, c) flexible, d) and e) practical, f) and g) useful, h) and i) device. j) Improvement in mobility measured by PLUS-M Scale. Independence outdoors: k) Walking with two crutches for short distances, l) walking through irregular surfaces. m) Increase of independence measured by Barthel Scale. Independence indoors and donning prostheses independently: n) donning her myoelectric prosthesis and turning on her TASKA TD, o) donning her liners bimanually, p) donning her lower limb prostheses, q) standing up, r) walking with two crutches indoors. Increase of perception of quality of life and health measured by EQ-D-VAS Scale. t) Independence.
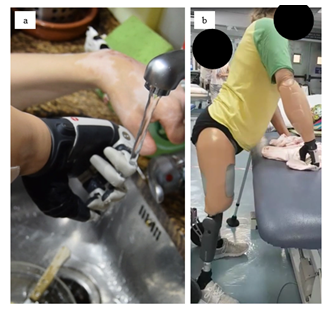
Figure 7: Special features of TASKA TD: a) waterproofness, b) resistant knuckle cover.
2.2.6 Left Partial Hand Amputation. No Prosthesis: No prostheses were needed to left partial hand amputation. Once she accepted her new situation psychologically, she started accomplishing tasks without prosthetics. At the beginning, the offer of a cosmetic glove was pondered as she was very concerned about her self-image. However, in this case, it was agreed that the gloves would not help her functionally because of the loss of sensory feedback, which becomes vital to accomplishing tasks without prosthetics. A dynamic prosthetic was also unnecessary, because she quickly learned to use that partial hand dextrously for every task.
2.2.7 Outcome Results: The prosthetic chosen options and the physical treatment plan resulted in a useful and aesthetically acceptable option for this quadruple amputee young woman patient. In order to measure the motor capacity and degree of mobility permitted due to her lower limb prosthetics, the system used was PLUS MOBILITY Score [39]. At the end of the first month, the patient attained a raw score of 15 which represents a 1,6% of mobility. By the end of the seventh month of training with the help of two crutches, the raw score raised up to 29, which represents a 16,6% of mobility. This numbers show that mobility improved a 15% during these months (Figure 6j). The evaluation of the upper limbs was carried out using the Disabilities of the Arm, Shoulder and Hand Questionnaire (DASH) [40]. The score without TASKA TD was of 102 points, which represents a 68% of difficulties for upper limb tasks; with TASKA TD, the patient obtained a score of 80 points at the end of the training program, which represents a 53,3% of difficulties in doing upper limb tasks. The difficulties in doing upper limb tasks decreased a 14,7% in one month using her myoelectric prosthesis with TASKA TD (Figure 6a). This improvement was especially remarkable at bimanual tasks such as opening a bottle, cooking, eating, or carrying things while walking (Figure 6b-i). Her level of independence was assessed using the Barthel Index [41], which increased from 15 points (total dependence) at the starting point without prostheses up to 85 points (moderate dependence) at the end of the training. Her level of independence increased a 70% (Figure 6m). The measurement of her perception of quality of life and health was assessed using the EQ-D-VAS Scale [42], which increased from 15 points at the start without prostheses, up to 80 points at the end of the trainee. Her own perception of quality of life and health increased a 65% (Figure 6s).
3. Discussion
This study presents a thorough description of the innovative prosthetic options and the physical treatment plan chosen for a quadruple amputee young female after sepsis to achieve the restoration of her function, independence and mobility. The authors have found a need to develop tools to help physicians to make the right decisions choosing the best prosthetic options and to sort the steps of rehabilitation training programs in order to achieve the best results that would allow complex amputee patients to recover a successful independence and return to activities of daily life. With this challenging patient example, the authors pretend bring forth every cosmetic and functional aspects to choose the best prosthetic or even no-prosthetic option for an optimal functional recovery. For the upper limb loss, without a careful study to select prostheses, patients may experience or manifest rejection due to multiple reasons. There are studies stating an overall mean rejection rate of 23% from 22 studies of patients wearing a myoelectric prosthesis, and a rate of 26% from 11 studies of patients wearing body-powered prosthesis [43]. Though alternative techniques, such as osseointegration [44] or the promising development of multiple degrees of freedom electromyogram pattern recognition-based prostheses, are currently taking place to solve these amputee troubles [45,46], body-powered and myoelectric prosthesis are the predominant prosthetic options for people with upper limb amputations. However, there is a lack of empirical evidence regarding functional differences in upper limb prostheses. It is also unclear whether is better to choose hook terminal devices (TDs), popular for their functionality, durability, low mass and improved visual access to objects of interest during manipulation, against hand TDs, which are better aesthetically accepted although their slower movements, the increase in mass and their decrease visual access to the objects [47]. Passive prostheses have received very little attention in prosthetic research and in the literature, probably because of the poor functional value which is attributed to passive hand prosthesis when compared to active ones [48]. Nevertheless, this type of prostheses, or even not wearing a prosthesis, may be considered since they might play an important role for one of the amputated limbs of a complex amputee patient, because this patient will need to experiment with many prostheses at different limb levels, and also because prosthetic fitting after upper limb loss arranges the patient to lose sensory perception feedback which becomes vital to accomplish tasks without prosthetics [49].
For the objective of achieving strong function restoration in the quadruple amputee patient of this study, the training program needs to begin with the right upper limb. It was crucial for the patient not to forget to use this limb until she received her definitive myoelectric right upper limb prosthesis later on the training period, as this limb was responsible for successfully dealing with bimanual tasks allowing her to resume her activities of daily life, and also to achieve the independence at donning her lower limbs prostheses. To achieve this goal, the main importance laid on the initial training program with strengthening exercises, and MI with OA for the later adaptation of her new self-image using VG. As her right upper limb was affected at a medium level (transradial amputation) the authors think it was truly important for this particular type of training to maintain the activation of her motor cortex brain which is responsible to make the motor function of the hand. The authors support this idea because it has been the experience of this rehabilitation team that usually when amputees are not wearing an upper limb prosthesis for a period of one year, they get used to develop their daily routines not wearing it, and it becomes very difficult, and even impossible in many cases, to accomplish the integration of wearing the upper limb prosthesis once that period of one year of time has passed. This may occur because the cessation of motor activity makes plasticity disappear in a cortical area [50]. This was avoided in this case by using motor imagery in order to make the patient to include prostheses in her body image and being able to success in all the praxias that allowed her to develop motor activities and executive tasks. This training technique allowed us to solve the trouble of 9 months since upper limb amputations, of waiting to obtain the TASKA TD. As she was concerned with her body image and cosmetics, the team successfully trained her in the use of a myoelectric upper limb with a novel dextrous TASKA TD. The mastering of her right upper limb prosthesis has helped her with the donning and doffing of her lower limb prostheses (Figure 6n-r). In this way, the innovative TASKA TD as her myoelectric prosthesis for the upper limb transradial amputation took an important role as the central axis to success for gaining independence. The authors observed a slight improvement on the DASH scale after one month of training with TASKA TD, but it is expected to find a significant high increase on this scale after 2 more months of training, as she is being able to integrate this limb in every daily task, with a special improvement in those which need to involve both upper limbs such as firmly holding a knife to cut a thick juicy steak, doing the laundry, washing the dishes, clicking a computer mouse (Figure 6b-i), or even more important, dressing up her microprocessor knees for her bilateral lower above knee amputations independently (Figure 6n-r). It seems reasonable to associate the fast patient’s improvement in developing upper limb tasks with the special features of this TASKA TD (robustness, waterproofness, and fewer tendency to get damaged in addition to a great functionality allowed for manual tasks). There are some examples in the literature fitting every amputated limb in a complex amputee [51], with the best prosthetic option, but it is not a common practice to find not to wear a prosthesis as the best option because of the tendency to think that wearing a prosthetic device will always increase functionality. Nevertheless, to choose between wearing or not wearing a prosthesis is not as simple, and many psychological and functional aspects will be needed to be considered to make the best decision. For our patient, it is important to note that no prosthetic for left partial amputated hand was needed due to her level of left amputation but especially due to her dominance, and also it permitted her not to lose sensory perception feedback. For the lower extremities of a bilateral transfemoral amputee patient, from a cardiovascular stand point, it is challenging, especially in our case, because of the kidney disease secondary to the sepsis, and it is known that the level of mobility and the independence in the activity of daily life among patients with chronic kidney disease tends to decrease without an appropriate rehabilitation program [52]. However, given the fall risk as a quadruple amputee, microprocessor knees (MPK) with stance control for safety have demonstrated to be superior when compared with non-microprocessor-controlled (mechanical) knee joints (NMPK), because MPK reduce the number and frequency of stumbles and falls of up to 80% [5-9]. At the end of the trainee program, she was able to walk with two crutches for short distances (Figure 6k) and irregular surfaces (Figure 6l). For long distances, she needed an electric wheelchair. The strengthening training program has played an essential role to overcome the necessary spending of energy to achieve prostheses motion. Vojta therapy has also been very useful at the beginning of the therapy to regain her strength and obtain the proprioception of her new body condition.
Another important technological tool that played an important role is virtual reality provided by VG. In this case, this useful and motivational device has let the patient to immerse in a virtual scenario very similar to the situations of daily life, which has facilitated the interaction and training for real situations without real risks. This tool has been adapted depending on the stage of recovery. The achievement of the vividness of the actions [20-24, 28-38] made possible to transfer her virtual learning to her daily life which was very useful for carrying out her activities of daily life. The results of this study state a clear improvement in every assessment scale. There was an improvement of a 15% in mobility walking with two crutches on the PLUS-M scale after 6 months of trainee (Figure 6j). It was initially expected to achieve a faster recover, but it happened slower probably because of the later delivery of the TASKA TD. With the training of the right upper limb, authors expect to achieve independent walking without crutches. It was also observed a slight decrease of 14,7% in difficulties in upper limb tasks on the DASH Scale after one month wearing her right upper limb prosthesis, especially notable at bimanual tasks (Figure 6a). This improvement is also expected to become higher with a longer training period of time, but authors find truly interesting to show these results at this short period of time, to further proof the importance of the initial therapy with Vojta and virtual reality therapy to prepare her brain to train her current myoelectric prosthesis in order to achieve these successful results. As the time lapse between the upper limb amputation and the fitting of the TASKA terminal device was rather long, the authors think that other traditional physical therapies would have failed. Her level of independence also increased a 70% starting from a level of a total dependence, moving to a level of moderate dependence (Figure 6m). The team has not yet achieved a total independence on the Barthel Index, since the patient needs to train on stars and needs help with small buttons of clothes, but she is completely independent for feeding, transfer between chair and bed, doing shower, use the toilet, walking and get dressed. Her own perception of quality of life and health has successfully increased a 65% going from 15 points on the EQ-D-VAS Scale at the beginning of the trainee period, to 80 points at the end (Figure 6s). She has been treated with a selective serotonin reuptake inhibitor (SSRI) since the beginning of the amputations were done, so this perception may be partially due to the effects of this drug. Serotonin receptors are widely expressed in human brain and SSRIs inhibit serotonin's transporter, which cause increased extracellular serotonin concentrations [53]. It is well known that brain serotonin transmission modulates anxiety and stress, promoting patience and coping, and moreover, brain serotonine is thought to participate in generating brain plasticity to achieve a greater adaptation to new circumstances, so chronic treatment with SSRIs could be associated not only with regulating mood, but also with improvements in learning and cognition [54]. For this reason, this drug may have contributed to help her to be successful on therapy, especially during the prosthetic fitting progress, which has provided her with the increased success that is evident from the results of the other scales. The improvement on the Barthel Index Scale, which shows her global dependence function, resembles higher than the improvement on the PLUS-M or DASH Scale, which are focused on the assessment of particular tasks: walking and bimanual tasks, respectively. These different results may be explained by the big improvement of her own perception of quality of life and health, which probably is conditioning her global function. For this case, it was also determinant to overcome some other difficulties such as economical coverage, psychological deterrence and other medical complications secondary to the sepsis. Many national health care systems, and in this case the National Healthcare system of Spain, will not cover the price of this type of prostheses, even though there are studies which suggest that these MPK provides substantial additional health benefits for these patients compared with NMPK, and also that is likely to be cost-effective in above knee amputees with and without cardiovascular risks such as diabetes mellitus at a ICER threshold of 40.000 Euro per QALY gained [55]. A multidisplinary team (physiotherapists, orthopedic technicians, medical doctors from other specialties…) coordinated by physiatrists has been the key to achieve successful development of patient’s independence (Figure 6t).
4. Conclusions
Even when the rehabilitation process of this patient has not yet concluded, the authors regard the publication of this case and its development as of great interest, as it showcases the training choices and technological keys to restore function in a quadruple amputee patient. For this particular case, it was important to start the training program with the right upper limb. As she was concerned with her body image and cosmetics, the team successfully trained her to use a myoelectric prosthesis with a novel dextrous TASKA terminal device, which was the central axis to recover her independence. No prosthetic for left partial amputated hand was needed due to her dominance, and it permitted her not to lose sensory perception feedback which is vital to accomplish tasks without prosthetics. As for the lower extremities, from a cardiovascular stand point, it was challenging, but given the fall risk as a quadruple amputee, microprocessor knees with stance control for safety have demonstrated to be the most appropriate.
Disclosure Statement
No funding was secured for this work. All authors declare that they have nonfinancial interests that might be relevant to the submitted work.
Acknowledgements
The prosthetic fitting of the patient was funded by the Fundación Renal of Íñigo Álvarez de Toledo. The language editing of the present work was supported by Luis Jaen.
Contributors’ Statement
All authors approved the final manuscript as submitted and agreed to be accountable for all.
References
- Abbott H, Capellini A, Carroll K, et al. First Step. A guide for adapting to limb loss. Amputee Coallition 7 (2017): 11-14.
- Durmus D, Safaz I, Adigüzel E, et al. Psychiatric symptoms in male traumatic lower limb amputees: associations with neuropathic pain, locomotor capabilities, and perception of body image. J. Mood Disord 5 (2015): 164-172.
- Zidarov D, Swaine B, Gauthier-Gagnon C. Quality of life of persons with lower-limb amputation during rehabilitation and at 3-month follow-up. Arch Phys Med Rehabil 90 (2009): 634-645.
- Rodríguez-Piñero Durán M, Rodríguez-Piñero Bravo-Ferrer M. Rodillas protésicas. Clasificación e indicaciones clínicas. Rehabilitación (Madr) 37 (2003): 207-214.
- Hahn A, Lang M. Effects of mobility grade, age, and etiology on functional benefit and safety of subjects evaluated in more than 1200 C-Leg trial fittings in Germany. Prosthet. Orthot 27 (2015): 86-94.
- Dite W, Connor HJ, Curtis HC. Clinical identification of multiple fall risk early after unilateral transtibial amputation. Arch. Phys. Med. Rehabil 88 (2007): 109-114.
- Highsmith MJ, Kahle JT, Bongiorni DR, et al. Safety, energy efficiency, and cost efficacy of the C-Leg for transfemoral amputees. A review of the literature. Prosthet. Orthot. Int 34 (2010): 362-377.
- Hafner BJ, Smith DG. Differences in function and safety between medicare functional classification Level-2 and -3 transfemoral amputees and influence of prosthetic knee joint control. J. Rehabil. Res. Dev 46 (2009): 417-433.
- Kahle JT, Highsmith MJ, Hubbard SL. Comparison of nonmicroprocessor knee mechanism versus C-Leg on prosthesis evaluation questionnaire, stumbles, falls, walking tests, stair descent, and knee preference. Rehabil. Res. Dev 45 (2008): 1-14.
- Stevens PM, Rheinstein J, Wurdeman SR. Prosthetic Foot Selection for Individuals with Lower-Limb Amputation: A Clinical Practice Guideline. J Prosthet Orthot 30 (2018): 175-180.
- Kuiken TA, Barlow AK, Hargrove L, et al. Targeted Muscle Reinnervation for the Upper and Lower Extremity. Tech Orthop 32 (2017): 109-116.
- Vadalà G, Di Pino G, Ambrosio L, et al. Targeted muscle reinnervation for improved control of myoelectric upper limb prostheses. J Biol Regul Homeost Agents 31 (2017): 183-189.
- Noce E, Dellacasa Bellingegni A, Ciancio AL, et al. EMG and ENG-envelope pattern recognition for prosthetic hand control. J Neurosci Methods 311 (2019): 38-46.
- http://www.ottobock.es/protesica/miembro-superior/sistemas-de-brazo-y-mano/myo-plus/
- Brinton MR, Barcikowski E, Davis T, et al. Portable Take-Home System Enables Proportional Control and High-Resolution Data Logging With a Multi-Degree-of-Freedom Bionic Arm. Frontiers in Robotics and AI 7 (2020): 133.
- George JA, Davis TS, Brinton MR, et al. Intuitive neuromyoelectric control of a dexterous bionic arm using a modified Kalman filter. J Neurosci Methods 330 (2020): 108462.
- Davidson JH, Jones LE, Cornet J, et al. Management of the multiple limb amputee. Disabil Rehabil 24 (2002): 688-699.
- Bauer H, Appaji G, Mundt D. VOJTA neurophysiologic therapy. Indian J Pediatr 59 (1992): 37-51.
- Sanz-Esteban I, Calvo-Lobo C, Ríos-Lago M, et al. Mapping the human brain during a specific Vojta's tactile input: the ipsilateral putamen's role. Medicine (Baltimore) 97 (2018): e0253.
- Mulder T. Motor imagery and action observation: cognitive tools for rehabilitation. J Neural Transm (Vienna) 114 (2007): 1265-1278.
- Mizuguchi N, Kanosue K. Changes in brain activity during action observation and motor imagery: Their relationship with motor learning. Prog Brain Res 234 (2017): 189-204.
- Ferreira Dos Santos L, Christ O, Mate K, et al. Movement visualisation in virtual reality rehabilitation of the lower limb: a systematic review. Biomed Eng Online 15 (2016): 144.
- Lei C, Sunzi K, Dai F, et al. Effects of virtual reality rehabilitation training on gait and balance in patients with Parkinson's disease: A systematic review. PLoS One 14 (2019): e0224819.
- De Araújo AVL, Neiva JFO, Monteiro CBM, et al. Efficacy of Virtual Reality Rehabilitation after Spinal Cord Injury: A Systematic Review. Biomed Res Int 2019 (2019): 7106951.
- Tamburella F, Scivoletto G, Molinari M. Balance training improves static stability and gait in chronic incomplete spinal cord injury subjects: a pilot study. Eur J Phys Rehabil Med 49 (2013): 353-364.
- Vojta V. Alteraciones motoras cerebrales infantiles. Diagnóstico y tratamiento precoz. 2ª ed. Madrid. Ediciones Morata 1 (2004): 31.
- Juárez-Albuixech ML, Redondo-González OR, Tello I, et al. Vojta Therapy versus transcutaneous electrical nerve stimulation for lumbosciatica syndrome: A quasi-experimental pilot study. Journal of Bodywork and Movement Therapies 24 (2020): 39-46.
- Rizzolatti G, Fogassi L. The mirror mechanism: recent findings and perspectives. Philos Trans R Soc Lond B Biol Sci 369 (2014): 20130420.
- Buccino G, Vogt S, Ritzl A, et al. Neural circuits underlying imitation learning of hand actions: an event-related fMRI study. Neuron 42 (2004): 323-334.
- Kohler E, Keysers C, Umiltà MA, et al. Hearing sounds, understanding actions: action representation in mirror neurons. Science 297 (2002): 846-848.
- Carr L, Iacoboni M, Dubeau MC, et al. Neural mechanisms of empathy in humans: a relay from neural systems for imitation to limbic areas. Proc Natl Acad Sci U S A 100 (2003): 5497-5502.
- Buccino G. Action observation treatment: a novel tool in neurorehabilitation. Philos Trans R Soc Lond B Biol Sci 369 (2014): 20130185.
- Nedelko V, Hassa T, Hamzei F, et al. Action imagery combined with action observation activates more corticomotor regions than action observation alone. J Neurol Phys Ther 36 (2012): 182-188.
- Filgueiras A, Quintas Conde EF, Hall CR. The neural basis of kinesthetic and visual imagery in sports: an ALE meta - analysis. Brain Imaging and Behavior 12 (2018): 1513-1523.
- Cuenca-Martínez F, Suso-Martí L, Grande-Alonso M, et al. Combining motor imagery with action observation training does not lead to a greater autonomic nervous system response than motor imagery alone during simple and functional movements: a randomized controlled trial. PeerJ 6 (2018): e5142.
- Fink A, Graif B, Neubauer AC. Brain correlates underlying creative thinking: EEG alpha activity in professional vs. novice dancers. Neuroimage 46 (2009): 854-862.
- Wriessnegger SC, Kirchmeyr D, Bauernfeind G, et al. Force related hemodynamic responses during execution and imagery of a hand grip task: A functional near infrared spectroscopy study. Brain Cogn 117 (2017): 108-116.
- Decety J, Jeannerod M, Germain M, et al. Vegetative response during imagined movement is proportional to mental effort. Behavioural Brain Research 42 (1991): 1-5.
- Plus-m.org [Internet]. Washington (Seattle): 12-item Short Form 2 (2014).
- García González LA, Aguilar Sierra FJ, Moreno Serrano C, et al. Traducción, adaptación cultural y validación de una escala de función del miembro superior: DASH. REv Colomb Ortop y Traumatol (2017).
- Barreno Solis CL, García Arrioja S, Ojeda Manzano A. Índice Barthel (IB): Un instrumento esencial para la evaluación funcional y la rehabilitación. Plasticidad y Restauración Neurológica 4 (2005): 81-85.
- Cabasés JM. El EQ-5D como medida de resultados en salud [The EQ-5D as a measure of health outcomes]. Gac Sanit 29 (2015): 401-403.
- Biddiss EA, Chau TT. Upper limb prosthesis use and abandonment: A survey of the last 25 years. Prosthet Orthot Int 31 (2007): 236-257.
- Overmann AL, Aparicio C, Richards JT, et al. Orthopaedic osseointegration: Implantology and future directions. J Orthop Res (2019): 1-10.
- Asogbon MG, Samuel OW, Geng Y, et al. Towards resolving the co-existing impacts of multiple dynamic factors on the performance of EMG-pattern recognition based prostheses. Comput Methods Programs Biomed 184 (2019): 105278.
- Parajuli N, Sreenivasan N, Bifulco P, et al. Real-Time EMG Based Pattern Recognition Control for Hand Prostheses: A Review on Existing Methods, Challenges and Future Implementation. Sensors (Basel) 19 (2019): 4596.
- Carey SL, Lura DJ, Highsmith MJ. Differences in myoelectric and body-powered upper-limb prostheses: Systematic literature review. JRRD 52 (2015): 247-262.
- Maat B, Smit G, Plettenburg D, et al. Passive prosthetic hands and tools: A literature review. Prosthet Orthot Int 42 (2018): 66-74.
- Wilke M, Hartmann C, Schimpf F, et al. The interaction between feedback type and learning in routine grasping with myoelectric prostheses. IEEE Trans Haptics (2019): 1939-1412.
- Walker JR, Detloff MR. Plasticity in Cervical Motor Circuits following Spinal Cord Injury and Rehabilitation. Biology 10 (2021): 976.
- Monné Cuevas P, Borrás Correa A, Vidal Fortuny E, et al. Traumatic quadruple amputee rehabilitation: from amputation to prosthetic functionality: a case report. Disabil Rehabil Assist Technol 2 (2019): 1-7.
- Tsur A, Shakeer N, Geron R. Comparison of the Functional Outcomes of Lower Limb Amputees with or without End-Stage Renal Disease. Isr Med Assoc J 21 (2019): 585-588.
- Dankoski EC, Agster KL, Fox ME, et al. Facilitation of serotonin signaling by SSRIs is attenuated by social isolation. Neuropsychopharmacology 39 (2014): 2928-2937.
- Carhart-Harris RL, Nutt DJ. Serotonin and brain function: a tale of two receptors. J Psychopharmacol 31 (2017): 1091-1120.
- Kuhlmann A, Krüger H, Seidinger S, et al. Cost-effectiveness and budget impact of the microprocessor-controlled knee C-Leg in transfemoral amputees with and without diabetes mellitus. Eur J Health Econ (2020).
