Depression: The Fourth Pillar of Classifying Risk of Diabetes-Related Amputation in Veterans
Article Information
Brandon M. Brooks1*, Jaminelli Banks2, Allison S. Arp3, Vilayvanh Saysoukha4, Bradley M. Brooks5, Brady M. Brooks6, Nichol L. Salvo7, Alton R. Johnson8, Donya A. Rabadi9, Ashley M. Nettles10, David G. Armstrong11, Lee C. Rogers12
1Brandon M. Brooks, DPM, MPH; Columbia VA Health Care System, South Carolina, USA*
2Jaminelli Banks, DPM; Center for Limb Preservation Advanced Wound Care, California, USA
3Allison S. Arp, MS; Independent Researcher, Wyoming, USA
4Vilayvanh Saysoukha, DPM, MS; Premier Foot and Ankle Centers of TN, Tennessee, USA
5Bradley M. Brooks, DO; Altapointe Health, Alabama, USA
6Brady M. Brooks, DO; University of Kentucky College of Medicine, Kentucky, USA
7Nichol L. Salvo, DPM; Atlanta VA Health Care System, Georgia, USA
8Alton R. Johnson Jr., DPM, University of Michigan, Michigan, USA
9Donya A. Rabadi, BS, Western University College of Podiatric Medicine, California, USA
10Ashley M. Nettles, DPM; Columbia VA Health Care System, South Carolina, USA
11David G. Armstrong, DPM, MD, PhD; Keck School of Medicine of USC; California, USA
12Lee C. Rogers, DPM; UT Health San Antonio, Texas, USA
*Corresponding Author: Brandon M. Brooks, Columbia VA Health Care System, 6439 Garners Ferry Rd, Columbia, South Carolina, USA.
Received: 26 October 2023; Accepted: 03 November 2023; Published: 22 November 2023
Citation: Brandon M. Brooks, Jaminelli Banks, Allison S. Arp, Vilayvanh Saysoukha, Bradley M. Brooks, Brady M. Brooks, Nichol L. Salvo, Alton R. Johnson, Donya A. Rabadi, Ashley M. Nettles, David G. Armstrong, Lee C. Rogers. Depression: The Fourth Pillar of Classifying Risk of Diabetes-Related Amputation in Veterans. Journal of Psychiatry and Psychiatric Disorders. 7 (2023): 201-209
View / Download Pdf Share at FacebookAbstract
Background: Over half of the 100,000 lower extremity amputations in the United States every year are related to complications of diabetes mellitus, yet mental health and/or depression are not routinely addressed as an underlying contributor. To prevent amputations, the Veterans Health Administration (VHA) utilizes the PAVE program which classifies risk (FRS) as normal(0), low(1), moderate(2) or high risk(3) for amputation. We hypothesized that PAVE FRS 2 and 3 Veterans would have a higher prevalence of depression compared to PAVE FRS 0 Veterans.
Methods: We conducted a retrospective cohort study involving Veterans with type 2 diabetes mellitus. We developed logistic regression models with several explanatory variables (age, race, sex, BMI, A1c, PAVE FRS) and a diagnosis of depression as the outcome.
Results: 148 patients met our inclusion criteria. Among the explanatory variables, only PAVE FRS 2 (OR 5.07;p=0.001; 95%CI 1.87,13.72) and PAVE FRS 3 (OR 9.85;p=0.002;95% CI 2.25,43.18) were significant. Of note, the PAVE FRS 2 includes Veterans with a foot deformity and/or neuropathy but not a history of a DFU or amputation.
Conclusions: PAVE FRS 2 and 3 Veterans had greater odds of having a documented diagnosis of depression. There was no significant difference in the prevalence of depression between PAVE FRS 2 (no DFU or amputation) and PAVE FRS 3 Veterans (DFU, amputation). Given that depression is among the most treatable mental disorders and can occur prior to a DFU and/or amputation, we proposed a modified threatened limb classification system that accounts for depression in the Veteran population (WIfI’D)
Keywords
Depression; Diabetic Foot Ulcers; Amputation; WIFI; WIFID; Classification systems; Mental Health; Diabetes Mellitus; Veterans; Polyvagal Theory; Major depressive disorder; Wound Healing
Depression articles; Diabetic Foot Ulcers articles; Amputation articles; WIFI articles; WIFID articles; Classification systems articles; Mental Health articles; Diabetes Mellitus articles; Veterans articles; Polyvagal Theory articles; Major depressive disorder articles; Wound Healing articles
Depression articles Depression Research articles Depression review articles Depression PubMed articles Depression PubMed Central articles Depression 2023 articles Depression 2024 articles Depression Scopus articles Depression impact factor journals Depression Scopus journals Depression PubMed journals Depression medical journals Depression free journals Depression best journals Depression top journals Depression free medical journals Depression famous journals Depression Google Scholar indexed journals Diabetic Foot Ulcers articles Diabetic Foot Ulcers Research articles Diabetic Foot Ulcers review articles Diabetic Foot Ulcers PubMed articles Diabetic Foot Ulcers PubMed Central articles Diabetic Foot Ulcers 2023 articles Diabetic Foot Ulcers 2024 articles Diabetic Foot Ulcers Scopus articles Diabetic Foot Ulcers impact factor journals Diabetic Foot Ulcers Scopus journals Diabetic Foot Ulcers PubMed journals Diabetic Foot Ulcers medical journals Diabetic Foot Ulcers free journals Diabetic Foot Ulcers best journals Diabetic Foot Ulcers top journals Diabetic Foot Ulcers free medical journals Diabetic Foot Ulcers famous journals Diabetic Foot Ulcers Google Scholar indexed journals Amputation articles Amputation Research articles Amputation review articles Amputation PubMed articles Amputation PubMed Central articles Amputation 2023 articles Amputation 2024 articles Amputation Scopus articles Amputation impact factor journals Amputation Scopus journals Amputation PubMed journals Amputation medical journals Amputation free journals Amputation best journals Amputation top journals Amputation free medical journals Amputation famous journals Amputation Google Scholar indexed journals WIFI articles WIFI Research articles WIFI review articles WIFI PubMed articles WIFI PubMed Central articles WIFI 2023 articles WIFI 2024 articles WIFI Scopus articles WIFI impact factor journals WIFI Scopus journals WIFI PubMed journals WIFI medical journals WIFI free journals WIFI best journals WIFI top journals WIFI free medical journals WIFI famous journals WIFI Google Scholar indexed journals WIFID articles WIFID Research articles WIFID review articles WIFID PubMed articles WIFID PubMed Central articles WIFID 2023 articles WIFID 2024 articles WIFID Scopus articles WIFID impact factor journals WIFID Scopus journals WIFID PubMed journals WIFID medical journals WIFID free journals WIFID best journals WIFID top journals WIFID free medical journals WIFID famous journals WIFID Google Scholar indexed journals Classification systems articles Classification systems Research articles Classification systems review articles Classification systems PubMed articles Classification systems PubMed Central articles Classification systems 2023 articles Classification systems 2024 articles Classification systems Scopus articles Classification systems impact factor journals Classification systems Scopus journals Classification systems PubMed journals Classification systems medical journals Classification systems free journals Classification systems best journals Classification systems top journals Classification systems free medical journals Classification systems famous journals Classification systems Google Scholar indexed journals Mental Health articles Mental Health Research articles Mental Health review articles Mental Health PubMed articles Mental Health PubMed Central articles Mental Health 2023 articles Mental Health 2024 articles Mental Health Scopus articles Mental Health impact factor journals Mental Health Scopus journals Mental Health PubMed journals Mental Health medical journals Mental Health free journals Mental Health best journals Mental Health top journals Mental Health free medical journals Mental Health famous journals Mental Health Google Scholar indexed journals Diabetes Mellitus articles Diabetes Mellitus Research articles Diabetes Mellitus review articles Diabetes Mellitus PubMed articles Diabetes Mellitus PubMed Central articles Diabetes Mellitus 2023 articles Diabetes Mellitus 2024 articles Diabetes Mellitus Scopus articles Diabetes Mellitus impact factor journals Diabetes Mellitus Scopus journals Diabetes Mellitus PubMed journals Diabetes Mellitus medical journals Diabetes Mellitus free journals Diabetes Mellitus best journals Diabetes Mellitus top journals Diabetes Mellitus free medical journals Diabetes Mellitus famous journals Diabetes Mellitus Google Scholar indexed journals Veterans articles Veterans Research articles Veterans review articles Veterans PubMed articles Veterans PubMed Central articles Veterans 2023 articles Veterans 2024 articles Veterans Scopus articles Veterans impact factor journals Veterans Scopus journals Veterans PubMed journals Veterans medical journals Veterans free journals Veterans best journals Veterans top journals Veterans free medical journals Veterans famous journals Veterans Google Scholar indexed journals Polyvagal Theory articles Polyvagal Theory Research articles Polyvagal Theory review articles Polyvagal Theory PubMed articles Polyvagal Theory PubMed Central articles Polyvagal Theory 2023 articles Polyvagal Theory 2024 articles Polyvagal Theory Scopus articles Polyvagal Theory impact factor journals Polyvagal Theory Scopus journals Polyvagal Theory PubMed journals Polyvagal Theory medical journals Polyvagal Theory free journals Polyvagal Theory best journals Polyvagal Theory top journals Polyvagal Theory free medical journals Polyvagal Theory famous journals Polyvagal Theory Google Scholar indexed journals
Article Details
1. Introduction
At least 15% of patients with diabetes mellitus will develop a foot ulcer during their lifetime. [1] Over half of the 100,000 annual major amputations in the United States are related to complications of diabetes mellitus. [2] Type 2 diabetes mellitus is a pandemic. [3,4] More curiously, despite the large health care costs associated with these wounds and subsequent amputations, preventive care is often an afterthought. [3,5,6] Further, specific populations may benefit from targeted measures. Prevention of Amputation in Veterans Everywhere (PAVE) is a program born of the Veterans Health Administration (VHA). The PAVE program is a directive that was originally developed in 1993. The directive has had seven iterations since then, with each one building on the experiences and improvements of the program. It has been wildly successful as over the course of three decades, the amputation rates among Veterans have decreased significantly. PAVE outlines the scope of care provided to Veteran patients who are at risk for limb loss and includes an amputation risk score classification system and a care referral pathway. [7] The risk score, otherwise known as foot risk score (FRS), is determined by screening diabetic Veterans for loss of protective sensation, lower extremity ischemia, foot ulceration (or history of ulceration), end stage renal disease, physical deformities, and other comorbidities. [8] Veterans are scored by risk stratification for amputation as normal (FRS 0), low (FRS 1), moderate (FRS 2) or high risk (FRS 3). Additionally, the program mandates a timely referral to a foot care specialist when the patient is found to be at increased risk for amputation (which equates to an FRS 2 or 3) and timely referral to a mental health team to provide support to patients. The causes of diabetic foot ulcers (DFUs) in Veterans are multifactorial. [9] In many cases, the complications of type 2 diabetes mellitus are preventable. [4,5,10] While poor diet and lack of exercise are common culprits, depression is associated with emotional eating/poor diet, lack of compliance, self-isolation, poor sleep, lack of exercise, and substance abuse. [11–19] Many of these depression-related associations can result in diabetic foot complications. [11–19] The diabetic foot – pain – depression cycle (also called the Saint Mariam Baouardy Cycle), was first described by Brooks et al at the 19th Annual Desert Foot Limb Salvage Conference in 2022 as an underlying causal mechanism between these variables; further, this cycle illustrates how depression and pain can contribute to diabetic foot complications. [20] Despite numerous wound classification systems existing in the literature, depression and overall mental health status is not addressed as an underlying contributor to threatened limbs, diabetic foot ulcers, and other diabetic foot complications. [21] As healthcare continues to shift in the United States to more population-specific and customized preventive measures, [22] it is unknown if DFU and other wound classification systems should as well. The Veteran population has unique comorbid, socioeconomic, and psychosocial challenges, including mental health issues secondary to traumatic experiences. [23,24] These traumatic experiences can impact Veterans for months, years, decades, and sometimes their entire lives. [23,24] In this study, we aim to determine associations between a diagnosis of depression and the PAVE FRS among the Veteran population. Secondarily, we aim to produce a Veteran-specific threatened limb classification system for this population. We hypothesize that Veterans with a PAVE FRS 2 (moderate risk of amputation but no DFU history or prior amputation) and PAVE FRS 3 (DFU history, ESRD, Charcot neuroarthropathy, or amputation level of the lower extremity) will have greater odds of a diagnosis of depression compared to the PAVE FRS 0 (normal risk). Further, we hypothesize that there will be no statistically significant difference between PAVE FRS 2 and PAVE FRS 3 Veterans in terms of the prevalence of depression.
2. Methods
2.1 Research Design
We obtained expedited approval from the Dorn VA Medical Center’s Institutional Review Board for retrospective cohort study design. We reviewed all charts of patients who required the PAVE screening seen in the podiatry clinic of the primary author in April of 2023. Patients without a diagnosis of type 2 diabetes mellitus were excluded. Our goal a priori was to review at least 140 charts. The outcome of interest is a documented diagnosis of depression. Our explanatory variables were PAVE FRS score (0,1,2,3), BMI (Obese [BMI 30+] or not obese [BMI <30]), age (65+ or younger than 65), HbA1c (Less than 6.5%, 6.5% to 8%, above 8%), sex, and race.
2.2 Statistical Analysis
We developed simple logistic regression models to identify the odds of a PAVE patient having a diagnosis of depression. To adjust for confounding, we aimed to develop a multiple logistic regression model that included explanatory variables that achieved p<0.1 with simple logistic regression. Further, we used Fisher’s Exact Test to determine if there was a significant difference between the prevalence of depression between PAVE FRS 2 and PAVE FRS 3 Veterans. We analyzed the data using STATA v15.1 (College Station, TX). In the multivariate model, statistical significance was pre-defined at p<0.05.
3. Results
Descriptive Results
One-hundred forty-eight Veterans’ charts were reviewed from the month of April 2023. The outcome of interest, specifically depression, was broken down by the PAVE FRS in Figure 1. Twenty-eight Veterans were classified as PAVE FRS 0, fifty-two as PAVE FRS 1, fifty-one as PAVE FRS 2, and seventeen as PAVE FRS 3. Ninety-eight patients were Black or African American, forty-eight were White, and two “preferred not to say.” Twelve were female while 136 were male. Fifty-two patients were under the age of 65 while ninety-six were seniors (age 65+). Sixty patients had a BMI less than 30 while 88 were obese. Eighty-three patients had a diagnosis of depression listed in their chart while 65 did not.
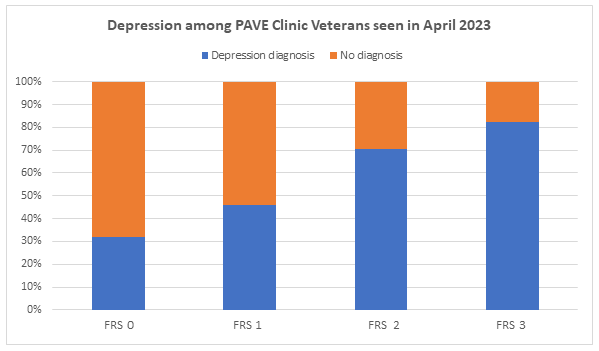
Figure 1: Percentage of VA PAVE patients with a Depression Diagnosis by PAVE Foot Risk Score (FRS)
|
Pave Score |
No diagnosis |
Depression diagnosis |
Total |
|
0 |
19 |
9 |
28 |
|
1 |
28 |
24 |
52 |
|
2 |
15 |
36 |
51 |
|
3 |
3 |
14 |
17 |
|
Total |
65 |
83 |
148 |
3.1 Statistical Results
The only explanatory variable in the univariate analysis with p<0.1 was the “PAVE foot risk score.” In the logistic regression model, PAVE FRS 0 (normal risk) was used as the referent group. The Pseudo R-square was 0.0906 in the logistic regression model. Veterans with a PAVE FRS 1(low risk) did not have a statistically significant difference (p=0.227) in having a diagnosis of depression compared to Veterans with a PAVE FRS 0; however, Veterans with a PAVE FRS 2 (moderate risk) had greater odds (OR 5.07; p=0.001; 95% CI 1.87, 13.72) of having a diagnosis of depression in their medical record compared to Veterans with a PAVE FRS 0. Further, Veterans with a PAVE FRS 3 (high risk) had even greater odds (OR 9.85; p=0.002; 95% CI 2.25, 43.18) of having a diagnosis of depression in their medical record compared to Veterans with a PAVE FRS 0.
3.2 Prevalence of Depression between PAVE foot risk scores (FRS) 2 and 3 Veterans
The Fisher’s Exact Test statistic value was 0.527, indicating the prevalence of a diagnosis of depression between PAVE FRS 2 (no DFU history) and PAVE FRS 3 (DFU history, amputation, etc.) was not significantly different between the two groups.
4. Discussion
Our retrospective cohort study of 148 Veterans treated in a VHA podiatry clinic found that Veterans with PAVE FRS 2 and 3 had increased odds, statistically significant and clinically meaningful, of having a diagnosis of depression compared to Veterans with a PAVE FRS 0 designation. Patients with a PAVE FRS 3 have either had a history of a DFU, an amputation, severe peripheral arterial disease with loss of protective sensation, Charcot disease with a lasting foot deformity, or chronic kidney disease stage 4 or 5. Patients with a PAVE FRS 2 have decreased (or absent, in some cases) protective sensation, no severe peripheral arterial disease, no ulceration, and no severe chronic kidney disease (chronic kidney disease less than stage 4). Most patients with diabetic neuropathy without ulceration fall into the PAVE FRS 2 category; many of these patients routinely see podiatric physicians for preventative foot care. Further, there was no significant difference between the PAVE FRS 2 and PAVE FRS 3 Veterans in terms of the prevalence of depression. The WHO has acknowledged depression as a leading cause of global disease burden. [25] It currently affects approximately 280 million people, [26] costing $326.2 billion in 2018 for adults in the US alone, [27] and continues to increase in prevalence over time on a global scale. [28] Known depression symptoms such as decreased physical activity are known to contribute to subsequently higher incidence of comorbidities such as metabolic syndrome and cardiovascular disease, [29, 30] physical health multimorbidity, [31] and diabetes. [18] Additional behavioral contributors to high physical comorbidities with depression may include stress, lack of hygiene, and poor nutrition. [32,33] These are behaviors also known to impact wound healing [32,34-38] and to increase the risk of adverse events in diabetic populations. [19] Various treatment options are recommended to manage depression, with options multifaceted and mechanistically diverse. [11,39,40] Certain treatments are known to convey physical benefits that may allay mechanisms by which depression affects wound healing. [41, 42] Importantly, multiple forms of depression treatment have been shown to be cost-effective, and while a combination of psychotherapy and pharmacotherapy has been shown to be a superior treatment option, either treatment alone can also be effective. [43-45] Efficacy of treatment options for the management of depression may be influenced by comorbidities and vice versa, rendering a comprehensive approach to treatment necessary to optimize care. [46]. The number of Veterans seeking mental health care is growing, and depression, accounting for 9% of all ambulatory military health network appointments, [24] remains one of the most prominent mental health conditions in the military. Not only can military-service in and of itself contribute to the incidence of depression, but deployment and combat are both also associated with increased risk of depression. [24] While older populations of Veterans may not be at greater risk of depression compared to non-veterans, [23] depression among the Veteran population and Veterans’ access to mental health clinicians remains a public health concern. For example, studies conducted by the Department of Veteran Affairs (VA) using Veteran data have found that Veterans with depression have a 40% higher risk of heart attack. [47] Additionally, many Veterans with depression may have unrecognized psychological comorbidities [12] and a higher risk of a myriad of physical comorbidities. [12] Multiple treatment options for depression in Veterans are also recommended by the VA or used at VA facilities. [48-50] Diabetes prevalence among Veterans is also of great concern; according to the VA Office of Research and Development, nearly 25% of VA patients have diabetes,51 far higher than the prevalence seen in the general population. [9] Notably, risk of multimorbidity increases each year after the age of 25 in Veterans with the greatest disparity between Veterans and non-Veterans occurring from ages 35-44, during which the former cohort is 50% more likely to report multimorbidity. [52] Multimorbidity is known to follow an S-shape pattern with aging. [53,54] Further, there is specific imperative to address multimorbidity in Veterans because multimorbidity has also been identified as a global health burden and a priority for health research. [55] VA initiatives such as the Translating Initiatives for Depression into Effective Solutions (TIDES) project emphasize the value of utilizing collaborative, evidence-based approaches to depression management and provide guidelines for collaboration between primary care and mental health specialists. [56] Early recognition and comprehensive treatment in cases of multimorbidity is essential. [56,57] Although comprehensive classification tools have been successfully implemented to enable earlier recognition in a variety of healthcare contexts, there is currently no comprehensive classification tool for diabetic wounds that incorporates the influence of depression. [58–60] Due to the multifaceted mechanisms by which depression influences wound healing, [18] mediating mechanisms such as comprehensive approaches to classification and treatment of wounds given comorbid depression are not only recommended, [32,46] but may offer a plethora of benefits to patients, care providers, and insurance providers alike: earlier and more accurate recognition of impaired wound healing or potential for impaired wound healing, [61] prevention of adverse outcomes, [62] subsequently lowered treatment burden and cost of care, [57] and improved clinical outcomes. [62–64] Additionally, utilizing a wound classification tool that incorporates depression may allow providers to recognize and more effectively address depression-related treatment plan non-adherence, a key problem in diabetic wound care. [61,64-66] Comprehensive foot care and patient education to treat foot ulcers is known to be a cost-saving intervention, and multi-component interventions are known to be very cost-effective. [67] Both interventions may be more effectively implemented by providers given the insight from a comprehensive wound classification tool. In patients with multimorbidity, combined interventions incorporating patient-level and provider-level components have been shown to not only be cost-effective, but to also promote beneficial physical conditions and outcomes. [68] Thus, beyond cost-savings, improved classification tools may allow for both improvement of current interventions and development of new interventions at multiple levels of care to improve outcomes.
4.1 WIfI’D: A Population-specific Classification System for Veterans
Despite Cole-King and Harding establishing the link between depression and wound-healing in 2001, many wound and threatened limb classification systems do not adequately recognize the importance of wellbeing and mental health. [21,69] Therefore, we propose “WIfI’D,” a mind-body approach to the classification of threatened limbs in the Veteran population; it is a modified version of The Society for Vascular Surgery’s WIfI (Wound, Ischemia, Foot Infection) Threatened Limb Classification System. [70] WIfI is used by clinicians to predict the risk of amputation at one year and to determine the need for limb revascularization. In this modified classification system, the four pillars of risk stratification for multidisciplinary amputation prevention and wound healing are: Wound, Ischemia, foot Infection, and Depression (Figure 2).
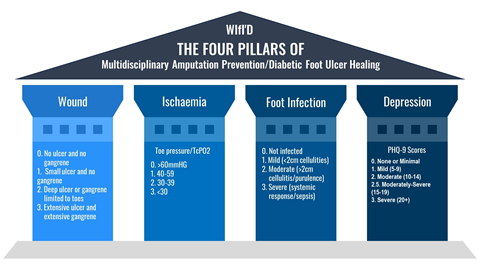
Figure 2: The Four Pillars of Multidisciplinary Amputation Prevention and the proposed WIfI’D classification system
4.2 Overcoming Schemata: Normalizing Depression Screening
We recommend that all patients with a diabetic foot ulcer should also be concomitantly screened for depression. The Merit-based Incentive Payment System (MIPS) outlines screening for depression as quality measure #134 given its potential benefits and low cost. [71] The Patient Health Questionnaire-9 (PHQ-9) is a nine-question self-reporting tool used to screen for depression; [72,73] Traditionally, PHQ-9 scores of 5, 10, 15, and 20 represented mild, moderate, moderately severe, and severe depression, respectively; [73] Podiatric physicians and surgeons are qualified to screen for depression and ensure a timely referral when necessary. [20] The appropriate referral will often be to a mental health provider such as a psychiatrist or clinical psychologist; however, certain patients may prefer discussing their mental health with their established primary care provider (i.e., primary care physician, physician assistant, nurse practitioner) as it may be easier for them to “open up” to a provider who already has their trust. [74] Every VA hospital can devise referral strategies best suited to serve its Veteran population; of note, the PAVE program is often the first step in the development of a multidisciplinary case management system for diabetic foot complications. [75] We recommend that multidisciplinary amputation prevention/limb salvage teams have a mental health provider, such as psychiatrist or clinical psychologist, as a team member. There have been numerous studies demonstrating the effectiveness of a multidisciplinary approach to the diabetic foot.
4.3 Applying Polyvagal Theory to Wound Healing
While vagus nerve stimulation has been utilized to treat depression, polyvagal theory takes it a step further with an innovative scientific perspective in studying neurophysiology. [76,77,78,79,80] First proposed by Stephen Porges, the polyvagal theory acknowledges that feelings of safety emerge from internal physiological states regulated by the autonomic nervous system. [76,77] Feelings of safety reflect a core fundamental process; by respecting human need to feel safe as a biological imperative linked to survival, we respect our phylogenetic heritage. [76,77] When there is no threat of perceived-danger, humans can remain in a state of social engagement, calmness, mindfulness, and trust. [76,77] Of note, “Building Trust” is an initiative of the ABIM Foundation which notes that “trust” is associated good health-related outcomes (and mistrust is associated with poor outcomes). [74,81] Further, when the autonomic nervous system is in a state of safety, humans have increased resistance to infection, better immune response, rest, and circulation to non-vital organs including the skin and the lower extremity. [77, 81] In summation, this is the ideal physiological state for patients with DFUs to be in as opposed to a state of perceived danger (i.e., fight or flight) which can result in increases in blood pressure, heart rate, and adrenaline. [77,81] Further, humans in this state can experience decreases in insulin activity, digestion, and immune response. [77,81] Limberg et al in 2022 further highlighted the dynamic interplay between central and peripheral mechanisms during hyperinsulinemia to increase sympathetic nervous system activity and maintain blood pressure in insulin-sensitive adults. [82,83]
4.4 Limitations
The Veteran population in one state may not be reflective of the entire American Veteran population. Further, our sample size (n=148) limits the generalizability of our results. Additional research into polyvagal theory and its implications for wound healing and amputation prevention are warranted. Further studies are needed to validate the inclusion of depression/mental health in the WIfI Classification System; however, we believe that multidisciplinary intervention and management of diabetic foot complications based on the effective and systematic combination of these components will contribute to the prevention and treatment of this patient population and improve their prognosis.
5. Conclusion
Veterans with PAVE FRS of 2 and 3 had greater odds of having a diagnosis of depression compared to Veterans with a PAVE FRS of 0 (“normal risk”). There was no statistical difference in the prevalence of depression in PAVE FRS 2 patients (no ulceration and no amputation) and the PAVE FRS 3 Veterans (i.e., amputation, history of ulceration, and/or current ulcer). The gap between the need for treatment for mental disorders and its provision is wide all over the world. Mental disorders remain an area of concern because of their high prevalence. Given that depression is among the most treatable mental disorders with some of the most deleterious effects, early recognition is critical. Depression has been associated with a lack of compliance, self-isolation, failure to keep appointments, and hopelessness - and none of these associations are conducive to the prevention of amputations in Veterans everywhere (PAVE) and wound-healing. We therefore recommend that all Veterans with DFUs be screened for depression. Should this screening be positive, then consideration should be made to refer the patient for a mental health assessment for possible treatment. In addition, we propose a modified WIfI classification system which can help Veterans and clinicians overcome the schemata associated with the depression diagnosis and screening, and ultimately optimize their clinical management.
Funding Statement:
None
Acknowledgements
This material is the result of work supported with resources and the use of facilities at the William Jennings Bryan Dorn VA Medical Center in Columbia, South Carolina, USA. The first author was inspired to include depression as pillar of multidisciplinary amputation prevention after reflecting upon the life of Saint Dymphna; subsequently, he prefers to refer to the inclusion of depression into existing wound/threatened limb classification systems as the “Saint Dymphna modification;” Saint Dymphna is the patron saint of depression.
References
- Yazdanpanah L, Shahbazian H, Nazari I, et al. Incidence and Risk Factors of Diabetic Foot Ulcer: A Population-Based Diabetic Foot Cohort (ADFC Study)—Two-Year Follow-Up Study. Int J Endocrinol. 39 (2018): 1-9
- Barnes JA, Eid MA, Creager MA, et al. Epidemiology and Risk of Amputation in Patients With Diabetes Mellitus and Peripheral Artery Disease. Arterioscler Thromb Vasc Biol. 40 (2020): 1808-1817.
- Armstrong DG, Wrobel J, Robbins JM. Guest editorial: Are diabetes-related wounds and amputations worse than cancer? Int Wound J. 4 (2007): 286-287
- Robbins JM, Strauss G, Aron D, et al. Mortality rates and diabetic foot ulcers: is it time to communicate mortality risk to patients with diabetic foot ulceration? J Am Podiatr Med Assoc. 98 (2008):489-493.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. New England Journal of Medicine. 376 (2017): 2367-2375.
- Barshes NR, Sigireddi M, Wrobel JS, et al. The system of care for the diabetic foot: Objectives, outcomes, and opportunities. Diabet Foot Ankle. 2013
- Sibona A, Bianchi C, Leong B, et al. A single center’s 15-year experience with palliative limb care for chronic limb threatening ischemia in frail patients. J Vasc Surg. 75 (2022): 1014-1020..
- Prevention of Amputation In Veterans Everywhere | VA North Texas Health Care | Veterans Affairs. 2023.
- Liu Y, Sayam S, Shao X, et al. Prevalence of and Trends in Diabetes Among Veterans, United States, 2005-2014. Prev Chronic Dis. 14 (2017).
- Frykberg RG, Zgonis T, Armstrong DG, et al. DIABETIC FOOT DISORDERS: A CLINICAL PRACTICE GUIDELINE (2006 revision). Journal of Foot and Ankle Surgery. 2006.
- Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 21 (2001): 33-61.
- Nichter B, Norman S, Haller M, et al. Psychological burden of PTSD, depression, and their comorbidity in the U.S. veteran population: Suicidality, functioning, and service utilization. J Affect Disord. 256 (2019): 633-640.
- Gore M, Brandenburg NA, Dukes E, et al. Pain Severity in Diabetic Peripheral Neuropathy is Associated with Patient Functioning, Symptom Levels of Anxiety and Depression, and Sleep. J Pain Symptom Manage. 2005;30 (2005): 374-385.
- Badescu S V., Tataru C, Kobylinska L, et al. The association between Diabetes mellitus and Depression. J Med Life. 9 (2016): 120-125.
- Roy T, Lloyd CE. Epidemiology of depression and diabetes: A systematic review. J Affect Disord. 2012;142( 2012): S8-S21.
- De Groot M, Anderson R, Freedland KE, et al. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 63 (2001): 619-630.
- Semenkovich K, Brown ME, Svrakic DM, et al. Depression in type 2 diabetes mellitus: prevalence, impact, and treatment. Drugs. 75 (2015): 577-587.
- Habib S, Sangaraju SL, Yepez D, et al. The Nexus Between Diabetes and Depression: A Narrative Review. Cureus. 14 (2022).
- Holt RIG, De Groot M, Golden SH. Diabetes and depression. Curr Diab Rep. 14 (2014).
- Brooks BM, Shih CD, Brooks BM, et al. The Diabetic Foot-Pain-Depression Cycle. J Am Podiatr Med Assoc. 113 (2023).
- Jeon BJ, Choi HJ, Kang JS, et al. Comparison of five systems of classification of diabetic foot ulcers and predictive factors for amputation. Int Wound J. 14 (2017): 537.
- Health Care - Healthy People 2030 | health.gov. 2023.
- Gould CE, Rideaux T, Spira AP, et al. Depression and anxiety symptoms in male veterans and non-veterans: the Health and Retirement Study. Int J Geriatr Psychiatry. 30 (2015): 623-630
- Inoue C, Shawler E, Jordan CH, et al. Veteran and Military Mental Health Issues. StatPearls. May 2022.
- Moussavi S, Chatterji S, Verdes E, et al. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 370 (2007): 851-858.
- Depressive disorder (depression).2023.
- Greenberg PE, Fournier AA, Sisitsky T, et al. The Economic Burden of Adults with Major Depressive Disorder in the United States (2010 and 2018). Pharmacoeconomics. 39 (2021): 653-665.
- Moreno-Agostino D, Wu YT, Daskalopoulou C, et al. Global trends in the prevalence and incidence of depression:a systematic review and meta-analysis. J Affect Disord. 281 (2021): 235-243.
- Vancampfort D, Koyanagi A, Ward PB, et al. Chronic physical conditions, multimorbidity and physical activity across 46 low- and middle-income countries. Int J Behav Nutr Phys Act. 14 (2017).
- Kerling A, Tegtbur U, Gützlaff E, et al. Effects of adjunctive exercise on physiological and psychological parameters in depression: a randomized pilot trial. J Affect Disord. 177 (2015): 1-6.
- Stubbs B, Vancampfort D, Veronese N, et al. Depression and physical health multimorbidity: primary data and country-wide meta-analysis of population data from 190 593 people across 43 low- and middle-income countries. Psychol Med. 47 (2017): 2107-2117.
- Walburn J, Vedhara K, Hankins M, et al. Psychological stress and wound healing in humans: a systematic review and meta-analysis. J Psychosom Res. 67 (2009): 253-271.
- Otte C, Gold SM, Penninx BW, et al. Major depressive disorder. Nat Rev Dis Primers. 2 (2016).
- Stechmiller JK. Understanding the role of nutrition and wound healing. Nutr Clin Pract. 25 (2010): 61-68.
- Wild T, Rahbarnia A, Kellner M, et al. Basics in nutrition and wound healing. Nutrition. 26 (2010): 862-866.
- Christian LM, Graham JE, Padgett DA, et al. Stress and Wound Healing. Neuroimmunomodulation. 13 (2006): 337.
- Gouin JP, Kiecolt-Glaser JK. The Impact of Psychological Stress on Wound Healing: Methods and Mechanisms. Crit Care Nurs Clin North Am. 24 (2012): 201.
- Ebrecht M, Hextall J, Kirtley LG, et al. Perceived stress and cortisol levels predict speed of wound healing in healthy male adults. Psychoneuroendocrinology. 29 (2004): 798-809.
- Slattery DA, Hudson AL, Nutt DJ. Invited review: The evolution of antidepressant mechanisms. Fundam Clin Pharmacol.18 (2004): 1-21.
- Souter MA, Miller MD. Do animal-assisted activities effectively treat depression? a meta-analysis. Anthrozoos. 20 (2007):167-180.
- Noordali F, Cumming J, Thompson JL. Effectiveness of Mindfulness-based interventions on physiological and psychological complications in adults with diabetes: A systematic review. J Health Psychol. 22 (2017): 965-983.
- Esterling BA, L’Abate L, Murray EJ, et al. Empirical foundations for writing in prevention and psychotherapy: Mental and physical health outcomes. Clin Psychol Rev. 19 (1999):79-96.
- Barth J, Munder T, Gerger H, et al. Comparative efficacy of seven psychotherapeutic interventions for patients with depression: a network meta-analysis. PLoS Med. 10 (2013).
- Kamenov K, Twomey C, Cabello M, et al. The efficacy of psychotherapy, pharmacotherapy and their combination on functioning and quality of life in depression: a meta-analysis. Psychol Med. 47 (2017): 414-425.
- Ross EL, Vijan S, Miller EM, et al. The Cost-Effectiveness of Cognitive Behavioral Therapy Versus Second-Generation Antidepressants for Initial Treatment of Major Depressive Disorder in the United States: A Decision Analytic Model. Ann Intern Med. 171 (2019): 785-795.
- Gold SM, Köhler-Forsberg O, Moss-Morris R, et al. Comorbid depression in medical diseases. Nat Rev Dis Primers. 6 (2020).
- Scherrer JF, Chrusciel T, Zeringue A, et al. Anxiety disorders increase risk for incident myocardial infarction in depressed and nondepressed Veterans Administration patients. Am Heart J. 159 (2010): 772-779.
- Egede LE, Acierno R, Knapp RG, et al. Psychotherapy for depression in older veterans via telemedicine: a randomised, open-label, non-inferiority trial. Lancet Psychiatry. 2 (2015): 693-701.
- The Effectiveness of rTMS in Depressed VA Patients - Full Text View - ClinicalTrials.gov. 2023.
- VA Augmentation and Switching Treatments for Improving Depression Outcomes - Full Text View - 2023.
- US Department of Veterans Affairs Office of Research and Development.2023.
- Bloeser K, Lipkowitz-Eaton J. Disproportionate multimorbidity among veterans in middle age. J Public Health (Oxf). 44 (2022): 28-35.
- Xu X, Mishra GD, Jones M. Evidence on multimorbidity from definition to intervention: An overview of systematic reviews. Ageing Res Rev. 37 (2017): 53-68.
- Profile of Veterans: 2017. Prepared by the National Center for Veterans Analysis and Statistics. 2023.
- Multiple Long-Term Conditions (Multimorbidity): a priority for global health research | The Academy of Medical Sciences., 2023.
- Luck J, Hagigi F, Parker LE, et al. A social marketing approach to implementing evidence-based practice in VHA QUERI: the TIDES depression collaborative care model. Implement Sci.4 (2009): 64.
- Skou ST, Mair FS, Fortin M, et al. Multimorbidity. Nat Rev Dis Primers. 8 (2022)
- AbuRuz SM, Bulatova NR, Yousef AM. Validation of a comprehensive classification tool for treatment-related problems. Pharmacy World and Science.28 (2006): 222-232.
- Runciman WB, Williamson JAH, Deakin A, et al. An integrated framework for safety, quality and risk management: an information and incident management system based on a universal patient safety classification. Qual Saf Health Care. 15 (2006).
- DiLosa K, Brown C, Rajasekar G, et al. Provider ankle brachial index and wound classification teaching as part of a comprehensive limb preservation outreach program. J Vasc Surg. 77 (2023).
- van Netten JJ, Seng L, Lazzarini PA, et al. Reasons for (non-)adherence to self-care in people with a diabetic foot ulcer. Wound Repair Regen. 27 (2019): 530-539.
- Diniz BS, Reynolds CF, Butters MA, et al. The effect of gender, age, and symptom severity in late-life depression on the risk of all-cause mortality: the Bambuí Cohort Study of Aging. Depress Anxiety. 31 (2014): 787-795.
- Stubbs B, Vancampfort D, Veronese N, et al. Depression and pain: primary data and meta-analysis among 237 952 people across 47 low- and middle-income countries. Psychol Med. 47 (2017): 2906-2917.
- Gatwood JD, Chisholm-Burns M, Davis R, et al. Differences in health outcomes associated with initial adherence to oral antidiabetes medications among veterans with uncomplicated Type 2 diabetes: a 5-year survival analysis. Diabet Med. 35 (2018): 1571-1579.
- Khalil H, Cullen M, Chambers H, et al. Elements affecting wound healing time: An evidence based analysis. Wound Repair Regen. =23 (2015): 550-556.
- Koyanagi A, Oh H, Stubbs B et al. Epidemiology of depression with psychotic experiences and its association with chronic physical conditions in 47 low- and middle-income countries. Psychol Med. 47 (2017): 531-542.
- Siegel KR, Ali MK, Zhou X, et al. Cost-effectiveness of Interventions to Manage Diabetes: Has the Evidence Changed Since 2008? Diabetes Care. 43 (2020): 1557-1592.
- Zhou Y, Dai X, Ni Y, et al. Interventions and management on multimorbidity: An overview of systematic reviews. Ageing Res Rev. 87 (2023).
- Cole-King A, Harding KG. Psychological factors and delayed healing in chronic wounds. Psychosom Med.63 (2001): 216-220.
- Mills JL, Conte MS, Armstrong DG, et al. The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: risk stratification based on wound, ischemia, and foot infection (WIfI). J Vasc Surg. 59 (2014).
- 2021 MIPS Measure #134: Preventive Care and Screening: Screening for Depression and Follow-Up Plan | MDinteractive. 2022.
- Levis B, Sun Y, He C, et al. Accuracy of the PHQ-2 Alone and in Combination With the PHQ-9 for Screening to Detect Major Depression: Systematic Review and Meta-analysis. JAMA. 2020;323 (2020): 2290-2300.
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a Brief Depression Severity Measure. J Gen Intern Med. 16 (2001): 606.
- Lynch TJ, Wolfson DB, Baron RJ. A Trust Initiative in Health Care: Why and Why Now? Acad Med. 94 (2019): 463-46
- Sibona A, Bianchi C, Leong B, et al. A single center’s 15-year experience with palliative limb care for chronic limb threatening ischemia in frail patients. J Vasc Surg.75 (2022)
- Porges SW. The polyvagal theory: New insights into adaptive reactions of the autonomic nervous system. Cleve Clin J Med. 76 (2009): S86.
- Hanazawa H. [Polyvagal Theory and Its Clinical Potential: An Overview]. Brain Nerve. 74 (2022): 1011-1016.
- Porges SW. The polyvagal theory: phylogenetic substrates of a social nervous system. Int J Psychophysiol. 42 (2001): 123-146.
- Ruby Jo Walker, LCSW | Southwest Trauma Training | Polyvagal Theory. 2023.
- Cooper CM, Farrand AQ, Andresen MC, et al. Vagus nerve stimulation activates nucleus of solitary tract neurons via supramedullary pathways. J Physiol. 599 (2021): 5261-5279.
- NYU’s Lauren Taylor Joins ABIM Foundation, AcademyHealth Effort to Mitigate Mistrust in Health Care - ABIM Foundation. 2023.
- Limberg JK, Soares RN, Padilla J. Role of the Autonomic Nervous System in the Hemodynamic Response to Hyperinsulinemia-Implications for Obesity and Insulin Resistance. Curr Diab Rep. 22 (2022): 169-175.
- PORGES SW. Orienting in a defensive world: mammalian modifications of our evolutionary heritage. A Polyvagal Theory. Psychophysiology. 32 (1995): 301-318.
