Delayed Postoperative Pneumothorax and Pneumomediastinum Following Orthognatic Surgery; a Rare Case Report and Literature Review
Article Information
Mirochnik R1, Joachim M2, Araidy S3, Barak M4*, Abu El-Naaj I5
1Roman Mirochnik DMD, Resident, Department of Oral and Maxillofacial Surgery, the Baruch Padeh Medical Center, Poriya, Israel
2Michael Joachim, DMD, M.Sc., Resident, Department of Oral and Maxillofacial Surgery, the Baruch Padeh Medical Center, Poriya, Israel
3Shareef Araidy, DMD, Attending, Department of Oral and Maxillofacial Surgery, the Baruch Padeh Medical Center, Poriya, Israel
4Michal Barak, MD, Senior Anesthesiologist, Department of Anesthesiology, Rambam Health Care Campus and the Rappaport Faculty of Medicine, Technion - Israel Institute of Technology, Haifa, Israel
5Imad Abu El-Naaj, DMD, Head, Department of Oral and Maxillofacial Surgery, The Baruch Padeh Medical Center, Poriya, Israel and Azrieli Faculty of Medicine, Bar-Ilan University, Safed, Israel
*Corresponding Author: Dr. Michal Barak, Department of Anesthesiology, Rambam Health Care Campus, POB 9602, Haifa 31096 Israel
Received: 10 June 2019; Accepted: 25 June 2019; Published: 19 August 2019
Citation: Mirochnik R, Joachim M, Araidy S, Barak M, Abu El-Naaj I. Delayed Postoperative Pneumothorax and Pneumomediastinum Following Orthognatic Surgery; a Rare Case Report and Literature Review. Archives of Clinical and Medical Case Reports 3 (2019): 199-205.
View / Download Pdf Share at FacebookAbstract
Pneumomediastinum and pneumothorax are potentially life-threatening complications, yet are extremely rare following maxillo-facial surgery. We report a case of a 20-year-old female patient who underwent bilateral sagittal split ramus osteotomy and genioplasty under general anesthesia. Several hours after the completion of the operation, she became extremely dyspneic and was re-intubated in the ward. Chest x-ray and CT exams revealed pneumothorax and pneumomediastinum. A chest drain was introduced and the patient recovered gradually. Here we review the literature and discuss this complication.
Keywords
Orthognathic surgery, Pneumothorax, Pneumomediastinum
Orthognathic surgery articles Orthognathic surgery Research articles Orthognathic surgery review articles Orthognathic surgery PubMed articles Orthognathic surgery PubMed Central articles Orthognathic surgery 2023 articles Orthognathic surgery 2024 articles Orthognathic surgery Scopus articles Orthognathic surgery impact factor journals Orthognathic surgery Scopus journals Orthognathic surgery PubMed journals Orthognathic surgery medical journals Orthognathic surgery free journals Orthognathic surgery best journals Orthognathic surgery top journals Orthognathic surgery free medical journals Orthognathic surgery famous journals Orthognathic surgery Google Scholar indexed journals Pneumothorax articles Pneumothorax Research articles Pneumothorax review articles Pneumothorax PubMed articles Pneumothorax PubMed Central articles Pneumothorax 2023 articles Pneumothorax 2024 articles Pneumothorax Scopus articles Pneumothorax impact factor journals Pneumothorax Scopus journals Pneumothorax PubMed journals Pneumothorax medical journals Pneumothorax free journals Pneumothorax best journals Pneumothorax top journals Pneumothorax free medical journals Pneumothorax famous journals Pneumothorax Google Scholar indexed journals Pneumomediastinum articles Pneumomediastinum Research articles Pneumomediastinum review articles Pneumomediastinum PubMed articles Pneumomediastinum PubMed Central articles Pneumomediastinum 2023 articles Pneumomediastinum 2024 articles Pneumomediastinum Scopus articles Pneumomediastinum impact factor journals Pneumomediastinum Scopus journals Pneumomediastinum PubMed journals Pneumomediastinum medical journals Pneumomediastinum free journals Pneumomediastinum best journals Pneumomediastinum top journals Pneumomediastinum free medical journals Pneumomediastinum famous journals Pneumomediastinum Google Scholar indexed journals health articles health Research articles health review articles health PubMed articles health PubMed Central articles health 2023 articles health 2024 articles health Scopus articles health impact factor journals health Scopus journals health PubMed journals health medical journals health free journals health best journals health top journals health free medical journals health famous journals health Google Scholar indexed journals pneumothorax articles pneumothorax Research articles pneumothorax review articles pneumothorax PubMed articles pneumothorax PubMed Central articles pneumothorax 2023 articles pneumothorax 2024 articles pneumothorax Scopus articles pneumothorax impact factor journals pneumothorax Scopus journals pneumothorax PubMed journals pneumothorax medical journals pneumothorax free journals pneumothorax best journals pneumothorax top journals pneumothorax free medical journals pneumothorax famous journals pneumothorax Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals diagnosis articles diagnosis Research articles diagnosis review articles diagnosis PubMed articles diagnosis PubMed Central articles diagnosis 2023 articles diagnosis 2024 articles diagnosis Scopus articles diagnosis impact factor journals diagnosis Scopus journals diagnosis PubMed journals diagnosis medical journals diagnosis free journals diagnosis best journals diagnosis top journals diagnosis free medical journals diagnosis famous journals diagnosis Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals disease articles disease Research articles disease review articles disease PubMed articles disease PubMed Central articles disease 2023 articles disease 2024 articles disease Scopus articles disease impact factor journals disease Scopus journals disease PubMed journals disease medical journals disease free journals disease best journals disease top journals disease free medical journals disease famous journals disease Google Scholar indexed journals MRI articles MRI Research articles MRI review articles MRI PubMed articles MRI PubMed Central articles MRI 2023 articles MRI 2024 articles MRI Scopus articles MRI impact factor journals MRI Scopus journals MRI PubMed journals MRI medical journals MRI free journals MRI best journals MRI top journals MRI free medical journals MRI famous journals MRI Google Scholar indexed journals
Article Details
1. Introduction
Pneumomediastinum and pneumothorax are potentially life-threatening complications, yet are relatively rare in maxillo-facial surgical practice. Only 5 cases were reported in the literature, in which pneumothorax and pneumomediastinum were associated with orthognathic surgery [1-5]. Early detection and treatment are crucial in such an occurrence. Ten percent of pneumothoraxes are asymptomatic, the rest of the patients often complain of acute chest pain and difficulty breathing. There is a reduction in vital capacity, tachycardia, tachypnoea, and hypoxemia [3,6]. In this case report we describe a 20 year old otherwise healthy female patient who had a unilateral pneumothorax and pneumomediastinum following a mandibular bilateral sagittal split osteotomy and advancement genioplasty. Possible causes, diagnosis and management are discussed.
2. Case Report
A 20-year old female 161 cm height, 52 kg weight (BMI 20), otherwise healthy, diagnosed with a skeletal class II malocclusion, was electively admitted for mandibular advancement by bilateral sagittal split ramus osteotomy and advancement genioplasty. Physical examination and preliminary laboratory work including a chest X-ray were normal.
In the operating room the patient was monitored with the standard monitors and IV line was established. General anesthesia was induced using i.v. propofol 150 mg, fentanyl 0.2 mg midazolam 3mg, and rocuronium 50 mg was used for muscle relaxation. Naso-tracheal intubation was performed without any complication, and bilateral ventilation was verified by auscultation. The patient was ventilated using volume-control ventilation with a tidal volume of 450 ml and respiratory rate 9-10/min. Peak airway pressure was maintained below 20 cmH2O, and the end-tidal carbon dioxide was 35-37 mmHg. Isoflurane was used for the maintenance of anesthesia. The operation took 4 hours, in which the patient was stable and vital signs were normal. Intermaxillary fixation was performed after oro-pharyngeal packing was removed. After the patient gained conciseness and her spontaneous breathing was effective, she was extubated and transferred to the recovery room. The patient stayed 2 hours in the recovery room, where her vital signs were stable and her oxygen saturation was 96-99% without supplemental oxygen, than she was transferred to the Department of Maxillofacial Surgery for further care. About ½ hour later, the patient suddenly became tachypneic and dyspneic, her oxygen saturation was noticed to decrease to 50-70%, nasal cannula with supplement oxygen with 6 L/min showed no benefit, breath sounds were weak and shallow, the patient was urgently delivered to the OR, there intermaxillary fixation removed and she was re-intubated orally. A chest X-ray at that time demonstrated scattered shadows in the lower lobe of the right lung, compatible with a suspected aspiration (Figure 1).
The arterial blood gas analysis showed: PO2 75 mmHg, pH 7.36, PCO2 38 mmHg, and HCO3 21.5 mmol/L. After stabilizing the patient, and ventilating by positive pressure, chest CT scan was performed, demonstrating pneumomediastinum and pneumothorax in the right upper lung (Figure 2 and 3).
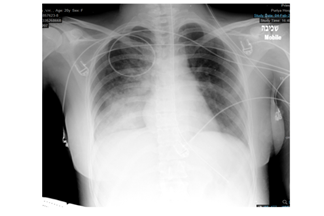
Figure 1: Chest X-ray following re-intubation shows scattered shadows in the lower lobe of the right lung.
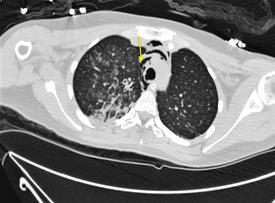
Figure 2: Chest CT scan. Arrow shows air in the mediastinum.
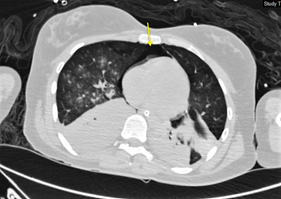
Figure 3: Chest CT scan. Arrow shows air in the mediastinum.
An intercostal drain was positioned (Pleurevac) on the right 5th intercostal space. The patient was mechanically ventilated during the following day, with progressive improvement in her vital signs, blood gas exams and follow-up radiographies. The patient was extubated on 2nd day and the intercostal drain was removed on the 3rd day. The intermaxillary fixation was reestablished on day 5th post-op day when the chest X-ray confirmed full recovery (Figure 4). The patient was discharged from hospital on the next day.
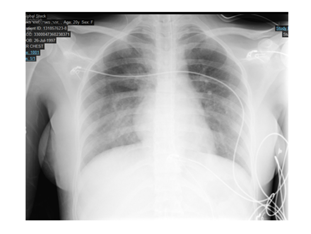
Figure 4: Chest X-ray on 5th post-op day, after clinical recovery.
3. Discussion
Pneumomediastinum and pneumothorax are defined as air presence in the mediastinum or pleural space, respectably. Primary pneumothorax occurs with no underlying lung disease usually in people aged 18–40 years with an incidence of 7.4–18 cases/ 100,000/ year for men, and 1.2–6 cases/ 100,000/ year for women. Secondary pneumothorax usually occurs in older adults with underlying disease such as COPD and collagen vascular diseases including Marfan syndrome [3,6]. While pneumothorax may occur spontaneously, in patients with or without lung disease, pneumomediastinum however, is not a spontaneously occurring event.
In our case, it is likely that the cause for pneumothorax and pneumomediastinum was the introduction of air into the mediastinum and pleural cavity from alveolar rupture by increased intra-alveolar pressure, possibly induced by choking, coughing, and mucous plugging, or by vigorous ventilatory support with mechanical ventilation [1,7]. Macklin was the first to describe the process of air entering into the mediastinum through perforation of the pulmonary interstitium by alveolar rupture [8]. When the intra-alveolar air pressure increases rapidly, air released from the ruptured alveoli causes pulmonary interstitial emphysema, dissects along the broncho-vascular sheath to the mediastinum, and causes pneumomediastinum. Another explanation for the pneumothorax was positive pressure ventilation. This is a well-known cause for pneumothorax, and our patient was ventilated with a tidal volume of 450 ml (more than 8 ml/kg), which may cause barotrauma.
As there is just a handful amount of reported cases, it is unfeasible to find a significant common variable. Data is gathered in Table 1.
|
Author \ year |
Gender |
Age years |
Type of Surgery |
Background |
Pneumo-mediastinum |
Pneumothorax |
Side |
Imaging |
Treatment |
|
Piecuch 1979 [9] |
M |
24 |
LF1+BSSO+Iliac crest |
Asthma Recent flu |
Yes |
No |
- |
XR |
Observation |
|
Edwards 1986 [1] |
F |
16 |
LF1+genioplasty |
Yes |
Yes |
Left |
XR |
Observation |
|
|
F |
21 |
LF1+BSSO+genioplasly |
No |
Yes |
Left |
XR |
Observation |
||
|
St. Hilaire 2004 [7] |
M |
19 |
LF1+BSSO+genioplasly |
Myotonic Dystrophy |
Yes |
No |
- |
XR |
Observation |
|
Goodson 2009 [3] |
F |
18 |
LF1+BSSO |
No |
Yes |
Left |
XR+CT |
Chest Drain |
|
|
Kim 2010 [4] |
M |
23 |
BSSO+genioplasty |
Yes |
Yes |
Right |
XR+CT |
Chest Drain |
|
|
Chebel 2010 [2] |
F |
28 |
LF1 |
Yes |
Yes |
Both |
XR |
Observation |
|
|
Bertossi 2012 [10] |
F |
28 |
LF1+BSSO |
No |
Yes |
Both |
XR+CT |
Chest Drain |
|
|
Corega 2014 [11] |
F |
22 |
LF1+BSSO |
No |
Yes |
Right |
XR+CT |
Chest Drain |
Abbreviations: LF1 – Le-Fort 1 osteotomy, BSSO – Bilateral Sagittal Split Osteotomy, XR – X-Ray, CT – Computerized Tomography
Table 1: Previous reports on pneumothorax with or without pneumomediastinum following orthognatic surgery.
Post-operative pneumothorax and pneumomediastinum present a difficult diagnostic challenge to the physician. Many patients, who underwent maxillofacial operation, complain on breathing difficulties in the immediate post-operative setting, usually it is attributed to edema, irritation of the nasal mucous membrane, bleeding, secretions, clot formation, deviated septum and others. Inter-maxillary fixation often worsen the situation, since breathing difficulty is worse and we cannot assist the patient with clearing the secretion or blood from the mouth. Furthermore, when the patient tries to cough in order to clear the airways, the resistance of the closed mouth increases significantly and the intra- pleural pressure may be excessive. The risk of aspiration at that time is very high as well. Thus, various types of respiratory complications may occur.
We recommend that physicians will be familiar with the possibility of pneumothorax and pneumomediastinum, thus may be ahead in diagnosing the patient’s actual problem and give the proper treatment as soon as possible.
Acknowledgment
None
Conflict of Interest
None
Funding
None
Ethics Statement/Confirmation of Patient Permission
Ethics approval not required. Patient permission for publication was obtained.
References
- Edwards DB, Scheffer RB, Jackler I. Postoperative pneumomediastinum and pneumothorax following orthognathic surgery. J Oral Maxillofac Surg 44 (1986): 137-41.
- Chebel NA, Ziade D, Achkouty R. Bilateral pneumothorax and pneumomediastinum after treatment with continuous positive airway pressure after orthognathic surgery. Br J Oral Maxillofac Surg 48 (2010): e14-e15.
- Goodson ML, Manemi R, Paterson AW. Pneumothorax after orthognathic surgery. Br J Oral Maxillofac Surg 48 (2010): 180-181.
- Kim T, Kim J Y, Woo YC, et al. Pneumomediastinum and pneumothorax after orthognathic surgery -A case report- Korean J Anesthesiol59 (2010): S242-S245.
- Al Shetawi AH, Golden L, Turner M. Anesthetic Complication during Maxillofacial Trauma Surgery: A Case Report of Intraoperative Tension Pneumothorax. Craniomaxillofac Trauma Reconstr 9 (2016): 251-254.
- Baumann MH, Strange C, Heffner JE, et al. Management of Spontaneous Pneumothorax. Chest 119 (2001): 590-602.
- St-Hilaire H, Montazem AH, Diamond J. Pneumomediastinum after orthognathic surgery. J Oral Maxillofac Surg 62 (2004): 892-894.
- Macklin CC. Transport of Air along Sheaths of Pulmonic Blood Vessels from Alveoli to Mediastinum: Clinical Implications. Arch Intern Med 64 (1939): 913-926.
- Piecuch JF, West RA. Spontaneous pneumomediastinum associated with orthognathic surgery: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol 48 (1979): 506-508.
- Bertossi D, Malchiodi L, Turra M, et al. Bilateral pneumothorax after orthognatic surgery. Dent Res J (Isfahan) 9 (2012): S242-S245.
- Corega C, Vaida L, Festila D, et al. Bilateral pneumothorax and pneumomediastinum after orthognathic surgery. Chirurgia (Bucur) 109 (2014): 271-274.
