Cyclops Lesion of Non-Operated Knees — A Case Report
Article Information
Atef Ibrahim Awad1*, Ibrahim el sebaei2, Khalid Ayed3
Affiliation:
1Consultant Orthopedic Surgeon, AFHSR Hospital, Saudi Arabia
2Consultant Orthopedic Surgeon, Faculty of Medicine, Orthopedic Department, Azahar University, Cairo, Egypt
3Senior Specialist Orthopedics, AFHSR Hospital Saudi Arabia
*Corresponding author: Atef Ibrahim Awad, Consultant Orthopedic Surgeon, AFHSR Hospital, Saudi Arabia.
Citation: Atef Ibrahim Awad, Ibrahim el sebaei, Khalid Ayed. Cyclops Lesion of Non-Operated Knees — A Case Report. Journal of Orthopedics and Sports Medicine 4 (2022): 199-202.
Received: July 08, 2022; Accepted: July 15, 2022; Published: July 19, 2022
Citation: Atef Ibrahim Awad, Ibrahim el sebaei, Khalid Ayed. Cyclops Lesion of Non-Operated Knees — A Case Report. Journal of Orthopedics and Sports Medicine 4 (2022): 199-202.
View / Download Pdf Share at FacebookAbstract
Cyclops lesions had been commonly reported after anterior cruciate ligament reconstructive surgeries due to many causes, mostly ACL graft tear or impingements, but the incidence of development of such lesions in non-operated knees of the native ACL, is not clearly described in the literature, this case study presents a Cyclops lesion after partial tear of anterior cruciate ligament in non-operated knee, causing loss of full knee extension with giving way.
Keywords
Cyclops lesions; Knee; Arthrofibrosis
Article Details
Introduction
Cyclops lesion, also known as localized anterior arthrofibrosis, was first described by Jackson and Schaefer [1]. It is a fibrous nodule of granulation tissue that is located anteriorly along the graft after an Anterior Cruciate Ligament Reconstruction (ACLR). A cyclops lesion with loss of extension of the knee with or without an audible or palpable clunk in terminal extension constitutes the cyclops syndrome. The incidence of cyclops syndrome has been reported to be between 1% and 10% of all ACLRs, whereas Magnetic Resonance Imaging (MRI) studies have reported an incidence of 25% to 47% for cyclops lesions. The incidence of all types of cyclops progressively increases with time. It was described clearly in the literature after ACLR surgeries but on the other hand not clearly reported in non- operated knees especially after partial tear of the ACL. The purpose of this report is to highlight the existence of cyclops lesions in non-operated knees after partial anterior cruciate ligament tears.
Case Presentation
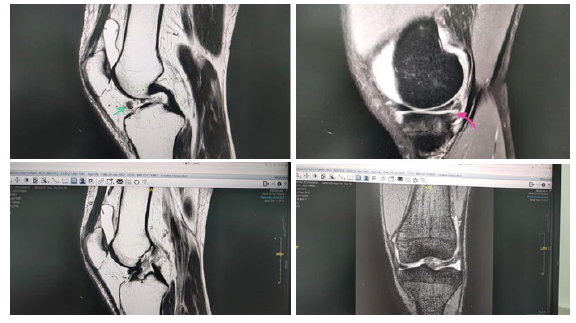
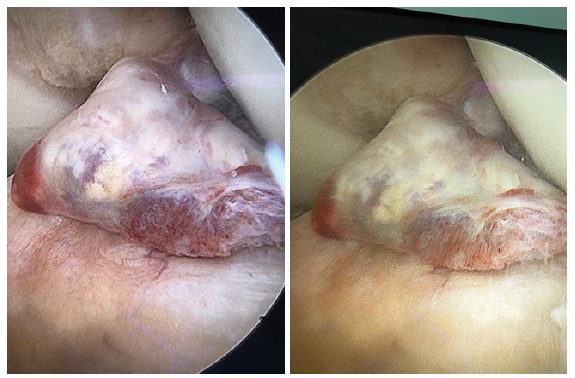
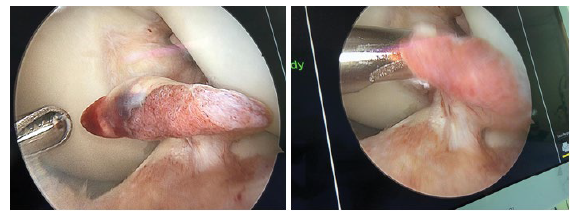
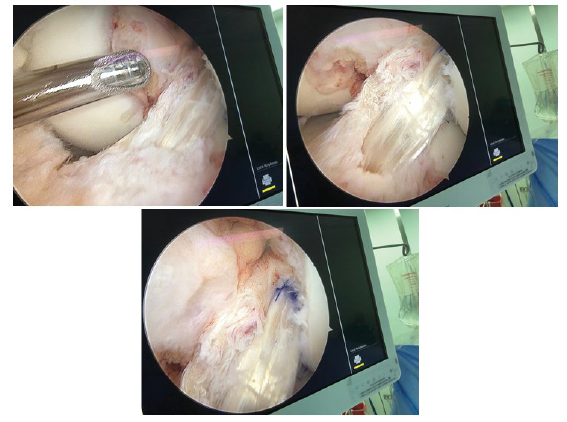
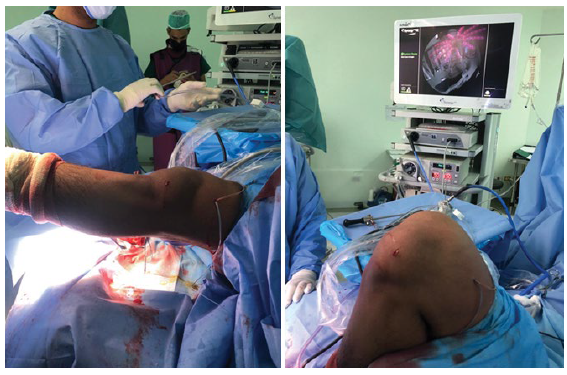
37 yrs. old male complained of pain and giving way of his left knee, with history of twisting left knee injury 6 months prior presentation during football playing. On examination wasted quadriceps, loss of active full extension (20° extension lag), tender medial joint line with positive anterior drawer and Lachman tests with endpoint; pivot shift test was done intra operatively with grade 2. MRI study showed partial tear of the ACL with cyclops lesion occupying the anterior knee compartment. Diagnostic arthroscopy reveals tear of the postrerolateral bundle of the ACL that formed a cyclops lesion. Arthroscopic removal of the cyclops with immediate full extension was achieved with ACL augmentation. Histopathological examination of the removed tissues excluded other pathological natures. Full ROM ESPECIALLY extension was achieved intraoperatively and post operatively with the patient follow up (Figures 1-6).
Discussion
Cyclops lesions are not commonly described in the literature to develop in non- operated knees that originate from the native ACL as consequence of its partial tear. The cyclops lesion is a pedunculated or nonpedunculated nodule of fibrovascular tissue. The arthroscopic appearance with its overlying blood vessels gives the appearance of a “cyclops”. The most common site is the anterolateral aspect of the tibial insertion site of the ACL graft [1]. With a high incidence of ACL tears
(250,000 per year in the United States [2]), an incidence of 1% to 10% for cyclops lesions after ACLR can mean a huge burden to health care. However, no large series of cyclops lesions have been reported in the literature. It may be assumed that a large number of cyclops or cyclopoid lesions are asymptomatic and undiagnosed or that the incidence is declining because of improvements in ACLR techniques [2]. In typical cyclops lesions after partial ACL tears, the nodule will be found adherent to the anterolateral part of the ACL [3].
Variants of cyclops lesions
Inverted cyclops lesion has been described as a fibrous nodule arising from the femoral notch instead of the tibia. Only 5 reports
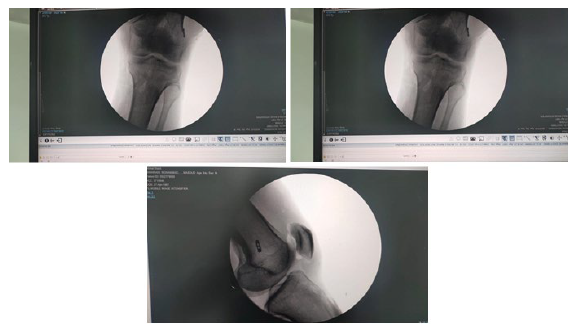
Figure 6: Showing post op X-rays demonstrating ACL tunnels with tightrope femoral fixation. of this lesion have been published, and it has been associated with T-shaped intercondylar fracture of the femur [4], autologous ACLR using Bone–Patellar Tendon–Bone (BPTB) graft [5], 4-strand hamstring grafts, or has occurred after supracondylar nailing of the femur [6,7]. The lesion may have a stalk leading to the femoral tunnel [5] or may occur without any connection to the femoral tunnel [7].
Cyclopoid lesions were first described by Muellner et al. [8] as fibroproliferative nodules without cartilage or bone and hence softer than the classic cyclops lesion. Because cyclopoid lesions are soft, they do not restrict terminal extension, may be asymptomatic, and are detected only as incidental findings on MRI scans or during arthroscopy. If flexion is also restricted in patients, the cyclopoid lesion probably represents a general tendency toward fibrotic healing and is not due to evolution into a true Cyclops [8]. Pseudocyclops lesions mimic cyclops lesions clinically and sometimes on imaging but do not have pathological features of cyclops. These are very rare lesions. Cyclops-like presentation has other causes. Gouty tophus has been reported as a cause of loss of extension and cyclops-like appearance during arthroscopy [9]. And the most common location is the infrapatellar fat pad region [9]. Other potential causes include space-occupying lesions, such as ganglia and pigmented villonodular synovitis, but these have not been reported in the setting of trauma to the knee or ACLR and hence may be incidental occurrences. They can be differentiated according to their typical histological features [10]. Cyclops lesion has been reported with both complete tear and partial tears of the native ACL. The cause of the nodule in ACL ruptures was thought to be avulsion of pieces of bone from the tibial attachment site of the ACL [11].
Cyclops lesion has also been reported after partial avulsion of small bone pieces from proximal attachment on the femur [12]. Persistent loss of knee extension for more than 2 months even after aggressive rehabilitation after ACL rupture should raise suspicion of a cyclops lesion [13]. Microtrauma was thought to lead to granulation tissue, which leads to formation of the nodule creating the cyclops [14]. No difference has been noted in the location, histologic features, or amount of loss of extension between cyclops lesion after rupture of the native ACL and that after ACLR [13]. Cyclops lesion has been reported with different types of ACL grafts and repair and reconstruction methods [15].
Diagnosis
Most cyclops lesions are asymptomatic and are found incidentally on postoperative MRI scans. Only 2% to 10% of all cyclops lesions are symptomatic [16]. These patients often present with loss of terminal extension of the knee, discomfort on walking or running or when laying supine [3], and an audible or palpable clunk during terminal extension [1]. Other reported causes for loss of terminal extension were suprapatellar, intercondylar, or capsular adhesions; fibrosis; and entrapment of the patella [17]. Clinical symptoms and signs have included pain at terminal extension, crepitus, painful cracking [18], rubbery endpoint to extension with a palpable pop [19], stiffness, and residual laxity [20].
Grinding with attempted extension beyond a patient’s limit, joint line pain and tenderness, locking of the knee, and discomfort with climbing stairs [21]. Tonin et al. [22] reported good results after excision of the lesion if ne within 12 weeks of presentation and did not report any recurrence after successful surgical excision, although recurrence is common for the other causes of loss of knee extension [22].
We are presenting male 37 years with history of twisting injury 6 months ago, no history of surgery before, who complained of left knee pain giving way and loss of full extension (extension lag 20°). On clinical examination, wasted left quadriceps muscle with loss of active last 20° of extension, positive anterior drawer and Lachman tests with endpoints, and tender medial joint line. MRI showed partial tear of the native ACL mostly the PL bundle, grade 3 tear of the posterior horn of the medial meniscus. Through diagnostic arthroscopy was done that confirmed the presentation of a hypervascular Cyclops lesion and confirmed its origin to be the PL bundle of the native ACL. Histopathological examination was done for this hyper vascular lesion to exclude other causes of Cyclops lesions (i.e., PVN). Complete arthroscopic shaving of the lesion with reconstruction of the PL bundle of the ACL with preservation of the intact AM bundle. Full extension was obtained intraoperative and after PL bundle reconstruction.
Conclusion
Cyclops lesion is a common complication after ACLR. But it can develop in non-operated knees as sequelae of partial tear of the native ACL, It is important to distinguish between a cyclops lesion and cyclops syndrome because management is needed only for the symptomatic lesion. Confirmatory diagnosis is made using MRI, and surgical excision is the management of choice for symptomatic lesions followed by ACL reconstruction or augmentation. Outcomes after excision are very good, and lesions almost never recur after excision.
References
- Jackson DW, Schaefer RK. Cyclops syndrome: loss of extension following intra-articular anterior cruciate ligament reconstruction. Arthroscopy 6 (1990): 171-178.
- Marrale J, Morrissey MC, Haddad FS. A literature review of autograft and allograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 15 (2007): 690-704.
- Veselko M, Rotter A, Tonin M. Cyclops syndrome occurring after partial rupture of the anterior cruciate ligament not treated by surgical reconstruction. Arthroscopy 16 (2000): 328-331.
- Hart AJ, Eastwood DM, Dowd GSE. Fixed flexion deformity of the knee following femoral physeal fracture: the inverted cyclops lesion. Injury 35 (2004): 1330-1333.
- Rubin LE, Yeh PC, Medvecky MJ. Extension loss secondary to femoral-sided inverted cyclops lesion after anterior cruciate ligament reconstruction. J Knee Surg 22 (2009): 360-363.
- Kambhampati S, Shanmugasundaram S. Inverted cyclops lesion of the knee associated with a supracondylar femoral nail: a case report. Cureus 11 (2019):
- Kambhampati S, Ware H. Inverted cyclops lesion after anterior cruciate ligament Ann R Coll Surg Engl 94 (2012): e99-e100.
- Muellner T, Kdolsky R, Grossschmidt K, et al. Cyclops and cyclopoid formation after anterior cruciate ligament reconstruction: clinical and histomorphological differences. Knee Surg Sports Traumatol Arthrosc 7 (1999): 284-289.
- Doany M, Lopez N, Rokito A. Knee extension loss secondary to a “cyclops-like” gouty tophus: a case report and literature review. Bull Hosp Jt Dis 75 (2017): 213-216.
- Simpfendorfer C, Miniaci A, Subhas N, et al. Pseudocyclops: two cases of ACL graft partial tears mimicking cyclops lesions on Skelet Radiol 44 (2015): 1169-1173.
- Nagira K, Enokida M, Hayashi I, et A simple method to reduce the incidence of cyclops lesion after anterior cruciate ligament reconstruction. J Knee Surg (2019).
- Tanabe Y, Yasuda K, Kondo E, et al. Clinical results of anterior cruciate ligament reconstruction with ligament remnant tissue preservation: a systematic review. Asia Pac J Sports Med Arthrosc Rehabil Technol 4 (2016): 1-8.
- McMahon PJ, Dettling JR, Yocum LA, et The cyclops lesion: a cause of diminished knee extension after rupture of the anterior cruciate ligament. Arthroscopy 15 (1999): 757-761.
- Delcogliano A, Franzese S, Branca A, et Light and scan electron microscopic analysis of cyclops syndrome: etiopathogenic hypothesis and technical solutions. Knee Surg Sports Traumatol Arthrosc 4 (1996): 194-199. Kim S-JJ, Jeong J-HH, Ko Y-GG. Synovitic cyclops syndrome caused by a Kennedy ligament augmentation device. Arthroscopy 19 (2003): e38.
- Noailles T, Chalopin A, Boissard M, et al. Incidence and risk factors for cyclops syndrome after anterior cruciate ligament reconstruction: a systematic literature review. Orthop Traumatol Surg Res 105 (2019): 1401-1405.
- Recht MP, Piraino DW, Cohen MA, et al. Localized anterior arthrofibrosis (cyclops lesion) after reconstruction of the anterior cruciate ligament: MR imaging findings. Am J Roentgenol 165 (1995): 383-385.
- Balcarek P, Sawallich T, Losch A, et al. Delayed cyclops syndrome: symptomatic extension block four years after anterior cruciate ligament reconstruction. Acta Orthop Belg 74 (2008): 261-265.`
- Bradley DM, Bergman AG, Dillingham MR imaging of cyclops lesions. Am J Roentgenol. 174 (2000): 719-726.
- Delincé P, Krallis P, Descamps PY, et al. Different aspects of the cyclops lesion following anterior cruciate ligament reconstruction: a multifactorial Arthroscopy 14 (1998): 869-876.
- Marzo JM, Bowen MK, Warren RF, et al. Intraarticular fibrous nodule as a cause of loss of extension following anterior cruciate ligament reconstruction. Arthroscopy 8 (1992): 10-18.
- Tonin M, Saciri V, Veselko M, et al. Progressive loss of knee extension after injury: cyclops syndrome due to a lesion of the anterior cruciate ligament. Am J Sports Med 29 (2001): 545-549.