Cutaneous Rosai-Dorfman Disease Showing Pruritic Macules
Article Information
Mayumi Ota, MD, Yoshimasa Nobeyama, MD*, and Akihiko Asahina, MD
Department of Dermatology, The Jikei University School of Medicine, Tokyo, Japan
*Corresponding Author: Yoshimasa Nobeyama, Department of Dermatology, The Jikei University School of Medicine, 25-8, Nishi-Shimbashi 3-chome, Minato-ku, Tokyo 105-8461, Japan
Received: 03 May 2021; Accepted: 14 May 2021; Published: 20 May 2021
Citation: Mayumi Ota, Yoshimasa Nobeyama, Akihiko Asahina. Cutaneous Rosai-Dorfman Disease Showing Pruritic Macules. Archives of Clinical and Medical Case Reports 5 (2021): 434-439.
View / Download Pdf Share at FacebookAbstract
Cutaneous Rosai-Dorfman disease (CRDD) is a rare skin-limited form of Rosai-Dorfman disease, a benign histiocytic proliferative disorder commonly affecting lymph nodes. Here, we report a case of CRDD characterized by pruritic reddish-brown macules, which we initially misdiagnosed as post-inflammatory pigmentation due to uremic dermatitis. A 64-year-old Japanese man was referred to us with an 8-month history of pruritic eruption located in the trunk and limbs. He had been receiving dialysis for chronic renal failure for 24 years. Physical examination revealed multiple reddish-brown macules measuring 1–10 cm in diameter with scratch marks irregularly distributed on the trunk and limbs. Pruritic score on the Numeric Rating Scale (NRS) was 9 out of 10. The patient displayed no extracutaneous involvements such as lymphadenopathy, fever or weight loss. Histopathological examination of the reddish-brown macules showed dense infiltration of histiocytes with lymphocytes and plasma cells in the dermis covered by epidermis with a faintly pigmented basal layer. Some histiocytes had taken in red blood cells, representing so-called emperipolesis. Immunohistochemical analyses of histiocytes showed reactivity to anti-S-100 protein antibodies and anti-CD68 antibodies, but not to anti-CD1a antibodies. Based on these findings, CRDD was diagnosed. This case suggests that CRDD may present with: i) macular lesions in the active phase; and ii) severe pruritus.
Keywords
Rosai-Dorfman disease; Pruritus; Macule; Emperipolesis; Histiocytosis
Rosai-Dorfman disease articles; Pruritus articles; Macule articles; Emperipolesis articles; Histiocytosis articles
Rosai-Dorfman disease articles Rosai-Dorfman disease Research articles Rosai-Dorfman disease review articles Rosai-Dorfman disease PubMed articles Rosai-Dorfman disease PubMed Central articles Rosai-Dorfman disease 2023 articles Rosai-Dorfman disease 2024 articles Rosai-Dorfman disease Scopus articles Rosai-Dorfman disease impact factor journals Rosai-Dorfman disease Scopus journals Rosai-Dorfman disease PubMed journals Rosai-Dorfman disease medical journals Rosai-Dorfman disease free journals Rosai-Dorfman disease best journals Rosai-Dorfman disease top journals Rosai-Dorfman disease free medical journals Rosai-Dorfman disease famous journals Rosai-Dorfman disease Google Scholar indexed journals Pruritus articles Pruritus Research articles Pruritus review articles Pruritus PubMed articles Pruritus PubMed Central articles Pruritus 2023 articles Pruritus 2024 articles Pruritus Scopus articles Pruritus impact factor journals Pruritus Scopus journals Pruritus PubMed journals Pruritus medical journals Pruritus free journals Pruritus best journals Pruritus top journals Pruritus free medical journals Pruritus famous journals Pruritus Google Scholar indexed journals Macule articles Macule Research articles Macule review articles Macule PubMed articles Macule PubMed Central articles Macule 2023 articles Macule 2024 articles Macule Scopus articles Macule impact factor journals Macule Scopus journals Macule PubMed journals Macule medical journals Macule free journals Macule best journals Macule top journals Macule free medical journals Macule famous journals Macule Google Scholar indexed journals Emperipolesis articles Emperipolesis Research articles Emperipolesis review articles Emperipolesis PubMed articles Emperipolesis PubMed Central articles Emperipolesis 2023 articles Emperipolesis 2024 articles Emperipolesis Scopus articles Emperipolesis impact factor journals Emperipolesis Scopus journals Emperipolesis PubMed journals Emperipolesis medical journals Emperipolesis free journals Emperipolesis best journals Emperipolesis top journals Emperipolesis free medical journals Emperipolesis famous journals Emperipolesis Google Scholar indexed journals Histiocytosis articles Histiocytosis Research articles Histiocytosis review articles Histiocytosis PubMed articles Histiocytosis PubMed Central articles Histiocytosis 2023 articles Histiocytosis 2024 articles Histiocytosis Scopus articles Histiocytosis impact factor journals Histiocytosis Scopus journals Histiocytosis PubMed journals Histiocytosis medical journals Histiocytosis free journals Histiocytosis best journals Histiocytosis top journals Histiocytosis free medical journals Histiocytosis famous journals Histiocytosis Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Case Report articles Case Report Research articles Case Report review articles Case Report PubMed articles Case Report PubMed Central articles Case Report 2023 articles Case Report 2024 articles Case Report Scopus articles Case Report impact factor journals Case Report Scopus journals Case Report PubMed journals Case Report medical journals Case Report free journals Case Report best journals Case Report top journals Case Report free medical journals Case Report famous journals Case Report Google Scholar indexed journals Cancer articles Cancer Research articles Cancer review articles Cancer PubMed articles Cancer PubMed Central articles Cancer 2023 articles Cancer 2024 articles Cancer Scopus articles Cancer impact factor journals Cancer Scopus journals Cancer PubMed journals Cancer medical journals Cancer free journals Cancer best journals Cancer top journals Cancer free medical journals Cancer famous journals Cancer Google Scholar indexed journals lymphadenopathy articles lymphadenopathy Research articles lymphadenopathy review articles lymphadenopathy PubMed articles lymphadenopathy PubMed Central articles lymphadenopathy 2023 articles lymphadenopathy 2024 articles lymphadenopathy Scopus articles lymphadenopathy impact factor journals lymphadenopathy Scopus journals lymphadenopathy PubMed journals lymphadenopathy medical journals lymphadenopathy free journals lymphadenopathy best journals lymphadenopathy top journals lymphadenopathy free medical journals lymphadenopathy famous journals lymphadenopathy Google Scholar indexed journals
Article Details
1. Introduction
Rosai-Dorfman disease (RDD) is a rare, benign histiocytic proliferative disorder that frequently involves lymphadenopathy [1] and extranodal involvements such as pyrexia, polyclonal gammopathy and neutrophilia with a medium frequency. Indeed, Foucar et al. reported that the extranodal organs were affected in approximately 40% of cases, with the skin as one of the most commonly affected extranodal organs [2]. Cutaneous manifestations of RDD include papules, nodules, plaques, masses and ulcers, which may be located in any region [2-4]. Because of the wide variety of clinical manifestations, the diagnosis must be made based on histopathological and immunohistochemical findings of dense infiltration of histiocytes with positive reactivity to anti-S-100 protein along with anti-CD68 antibodies and negative reactivity to anti-CD1a antibodies [3-5]. The diagnosis is further confirmed through the detection of emperipolesis, representing histiocytes that have taken in lymphocytes, plasma cells, neutrophils and red blood cells.
Cutaneous RDD (CRDD) is a subtype of RDD in which the lesions are localized in skin tissue without any extracutaneous symptoms such as lymphadenopathy. This subtype accounts for only 3% of all RDD cases [6]. Here, we report a case of CRDD characterized by pruritic reddish-brown macules, which we initially misdiagnosed as post-inflammatory pigmentation due to uremic dermatitis.
2. Case Report
A 64-year-old Japanese man was referred to us with an 8-month history of pruritic eruption located in the trunk and limbs. The patient had been treated in another clinic with prednisolone at 0.5 mg/kg once or twice a week, nalfurafine hydrochloride at 2.5 µg/day, bepotastine besilate at 20 mg/day and topical betamethasone butyrate propionate, resulting in no response. He had been receiving dialysis for chronic renal failure for 24 years, and had undergone nephrectomy for left renal cell carcinoma 4 years before this presentation.
Physical examination revealed multiple reddish-brown macules measuring 1–10 cm in diameter with scratch marks irregularly distributed on the trunk and limbs (Figure 1). Pruritic score on the Numeric Rating Scale (NRS) was 9 out of 10. The patient displayed no extracutaneous involvements such as lymphadenopathy, fever or weight loss. Histopathological examination of the reddish-brown macules showed dense infiltration of histiocytes with lymphocytes and plasma cells in the dermis covered by epidermis with a faintly pigmented basal layer (Figure 2). Some histiocytes had taken in red blood cells, representing so-called emperipolesis (Figure 3). Immunohistochemical analyses of histiocytes showed reactivity to anti-S-100 protein antibodies (Agilent, Santa Clara, CA) and anti-CD68 antibodies (Agilent) (Figure 4 and 5), but not to anti-CD1a antibodies (Agilent). Based on these findings, CRDD was diagnosed. The patient was treated with prednisolone at 0.5 mg/kg/day and narrow-band ultraviolet B irradiation twice at a 2-week interval, and pruritic sensation was relieved (NRS, 0). Administration of prednisolone was ceased within 2 months after the first visit, by which time the eruptions had almost disappeared (Figure 6).
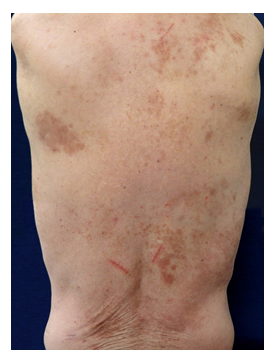
Figure 1: Clinical findings at the first visit. Multiple reddish-brown macules measuring 1–10 cm in diameter with scratch marks are irregularly distributed over the trunk.
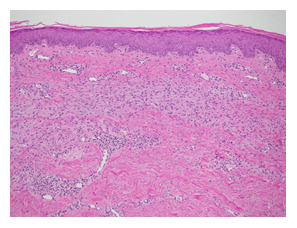
Figure 2: Histopathological findings (hematoxylin and eosin stain, ×100). Histiocytes show dense infiltration with lymphocytes and plasma cells into the dermis, covered by an epidermis with a faintly pigmented basal layer.
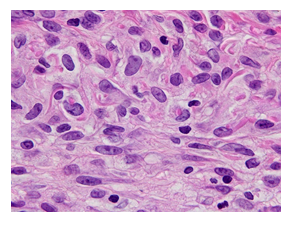
Figure 3: Histopathological findings (hematoxylin and eosin stain, ×1000). Some histiocytes show intake of red blood cells, representing emperipolesis.
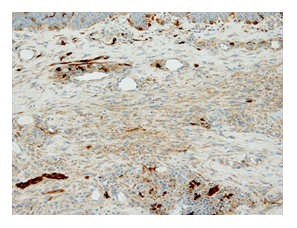
Figure 4: Immunohistochemical findings for S-100 protein (×200). Histiocytes show reactivity to anti-S-100 protein antibodies.
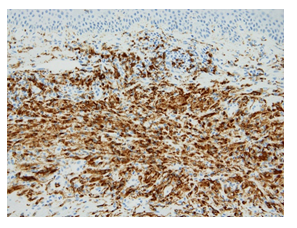
Figure 5: Immunohistochemical findings for CD68 (×200). Histiocytes show reactivity to anti-CD68 antibodies.
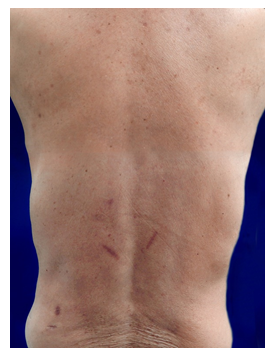
Figure 6: Clinical findings 2 months after the first visit. Eruptions show marked resolution.
3. Discussion
Because CRDD occasionally shows spontaneous regression and usually presents with nodules or plaques as the clinical manifestation [7], the macular lesions on the first visit in our case might be considered as simply a clinical manifestation in the regression process from plaque or nodular lesions. However, our case was strongly suggested to have presented with macular lesions in the active phase of the disease, because: i) the patient had not noticed the appearance of nodular or plaque lesions during the course of the disease in situations where the patient would have looked at and touched the lesions located on the trunk and limbs due to severe pruritus; ii) histopathological examination of the macular lesions showed massive histiocytic infiltration and many instances of emperipolesis, which is found only in recently developed lesions, and not in older lesions [3]; and iii) eruptions had almost disappeared within 2 months, in contrast with the fact that post-inflammatory pigmentation is more persistent.
Previous reports have described the ineffectiveness of various treatments for CRDD, including topical and systemic corticosteroids, radiation therapy and phototherapy, although surgical excision appears effective for solitary lesion [8]. In this context, no therapeutic strategy has been established for CRDD showing multiple lesions. Principally, therapy for CRDD may not be needed, because: i) the prognosis is good and most cases will show spontaneous regression over a period of months to years; and ii) no cases of cutaneous disease progressing to systemic disease have been reported [2,5]. However, our patient was in exceptional need of treatment because of the severe pruritus. Immediately after performing narrow-band ultraviolet B irradiation in combination with administering a medium dose of systemic corticosteroid in addition to an anti-histamine and a topical corticosteroid, the patient was very satisfied with the decrease in the pruritic sensation. We still lack evidence that narrow-band ultraviolet B irradiation in combination with systemic corticosteroid administration is effective against CRDD, considering that the disease can regress spontaneously.
In conclusion, CRDD may present with macular lesions in the active phase and severe pruritus. Further study is required to elucidate the clinical manifestations and pathogenesis of this disease.
References
- Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch Pathol 87 (1969): 63-70.
- Foucar E, Rosai J, Dorfman R. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): review of the entity. Semin Diagn Pathol 7 (1990): 19-73.
- Gameiro A, Gouveia M, Cardoso JC, et al. Histological variability and the importance of clinicopathological correlation in cutaneous Rosai-Dorfman disease. An Bras Dermatol 91 (2016): 634-637.
- Rubenstein MA, Farnsworth NN, Pielop JA, et al. Cutaneous Rosai-Dorfman disease. Dermatol Online J 12 (2006): 8.
- Brenn T, Calonje E, Granter SR, et al. Cutaneous rosai-dorfman disease is a distinct clinical entity. Am J Dermatopathol 24 (2002): 385-391.
- Wang KH, Chen WY, Liu HN, et al. Cutaneous Rosai-Dorfman disease: clinicopathological profiles, spectrum and evolution of 21 lesions in six patients. Br J Dermatol 154 (2006): 277-286.
- Kroumpouzos G, Demierre MF. Cutaneous Rosai-Dorfman disease: histopathological presentation as inflammatory pseudotumor. A literature review. Acta Derm Venereol 82 (2002): 292-296.
- Kong YY, Kong JC, Shi DR, et al. Cutaneous rosai-dorfman disease: a clinical and histopathologic study of 25 cases in China. Am J Surg Pathol 31 (2007): 341-350.
