Cross-State Variations and time Trends in Opioid use Disorder among a Privately Insured Nonelderly Population in the United States.
Article Information
Bibo Jiang1*, Li Wang1, Douglas Leslie1
1Department of Public Health Sciences, College of Medicine, The Pennsylvania State University, Hershey, PA, 17033.
*Corresponding Author: Bibo Jiang, Department of Public Health Sciences, College of Medicine, The Pennsylvania State University, Hershey, PA, 17033.
Received: 01 July 2023; Accepted: 08 July 2023; Published: 30 August 2023
Citation: Bibo Jiang, Li Wang, Douglas Leslie. Cross-State Variations and time Trends in Opioid use Disorder among a Privately Insured Nonelderly Population in the United States. Journal of Psychiatry and Psychiatric Disorders. 7 (2023): 138-146.
View / Download Pdf Share at FacebookAbstract
Objectives: To describe cross-state variations and time trends in Opioid Use Disorder (OUD) among privately insured individuals in the U.S. from 2005-2015 and investigate the demographic differences between OUD patients in states most affected by the epidemic compared to the remaining states.
Methods: The MarketScan® Commercial Claims and Encounters database was used to calculate the state-level prevalence of OUD. We analyzed the level and time change of OUD prevalence in each state from 2005 to 2015. A one-sided exact Fisher test was used to analyze the demographic differences between OUD patients in states most affected by the epidemic and the remaining states.
Results: Cross-state variations of the opioid epidemic among the privately insured population were substantial. Demographic patterns of the epidemic were similar across states. The 18-34 age group was the most affected group with the highest prevalence. The 55-64 age group experienced the most rapid increase of OUD prevalence, especially in states that were most affected by the epidemic.
Conclusions: The alarming increase in OUD prevalence among the 55-64 age group might indicate the need to improve prescription drug monitoring programs for this subpopulation, especially in those harder-hit states.
Keywords
Opioid epidemic, Opioid use disorder, Cross-state variations, Demographic difference, Privately insured population, Time trends
Article Details
1. Introduction
Over the past two decades, the opioid overdose epidemic has been one of the most pressing public health issues in the United States. Drug overdose deaths nearly tripled from 1999 to 2014, with over half of the drug overdose deaths in 2014 involving an opioid [1-5]. Recent statistics reveal a worsening of the opioid overdose epidemic. Opioid involved overdose death rates further increased by 15.6% from 2014 to 2015 [3,6] and 27.9% from 2015 to 2016 [6], resulting in 42,249 deaths (13.3 per 100,000 population) in 20166. In addition to the rising rate of opioid-involved mortality, the economic burden associated with opioid overdose, misuse and dependence is also increasing, reaching $78.5 billion in 2013 [7].
Although the opioid epidemic is nationwide, previous studies have documented geographic imbalances of the epidemic based on opioid-involved mortality rates across states, with the largest rates and increases concentrated in the eastern states [8-11]. A recent report released by the State Health Access Data Assistance Center confirmed that substantial differences in the opioid epidemic exist across states based on both non-heroin opioid death rates and heroin death rates. More specifically, in 2015, non-heroin opioid death rates ranged from 2.8 to 29.4 (per 100,000) and heroin death rates ranged from 0.7 to 13.3 (per 100,000) across states. [12] Although geographic patterns in death rates associated with drug poisoning have largely been unexplored9, some empirical studies have suggested that the increase in death rates associated with drug poisoning is greater for nonmetropolitan or rural areas of the U.S. compared to metropolitan areas [13,14]. Moreover, variation in the availability of opioid analgesics was found to be related to the difference in drug poisoning mortality by state [10,15].
Understanding variations in the opioid epidemic across states can assist state governments in designing localized interventions to more effectively address the epidemic. While previous studies have investigated demographic characteristics of the opioid epidemic in general, little is known about these patterns in privately insured populations. Since it has been suggested that a major cause of the epidemic is increased access to opioid pain medications in insured populations [16], examining these patterns in the privately insured population is important. Moreover, previous studies on prevalence of the opioid epidemic were mainly focused on opioid overdose death rates using mortality data from death certificates, such as the studies conducted by the Centers for Disease Control and Prevention (CDC) [2,6]. However, due to increasing clinical and economic burdens associated with OUD and its morbidities, it is also important to study the prevalence of OUD in claims data to better understand the epidemic and assist federal and state governments with allocating medical resources to effectively treat OUD and lower drug overdose death rates.
Medicaid plays a major role in financing treatment for opioid use disorder [17]; given its role as a safety net for individuals with OUD, this is not surprising. However, state variations in OUD prevalence among the privately insured population, which is a component of the entire population, are also important but not well understood. This study aims to fill the existing gap by investigating state-level OUD prevalence from 2005–2015 using data from the MarketScan® Commercial Claims and Encounters database.
2. Methods
2.1 Data Source
Data from the MarketScan® Commercial Claims and Encounters database (MarketScan), which includes claims information from various payers, and describes the healthcare service use and expenditures for covered employees and family members, were used for this study. The database contains subsections including inpatient claims, outpatient claims, outpatient prescription drug claims, and enrollment information. Claims data in each of the subsections contain a unique encrypted patient identifier and information on patient age, sex, geographic location (e.g., state), etc. This unique encrypted patient identifier, which is not available in admission-based data systems such as the Treatment Episode Data Set (TEDS), makes it feasible to count the number of OUD patients in each state for a given year.
2.2 Study Sample
Table 1: Demographic statistics of enrollments in the MarketScan database
The MarketScan data used in this study covers the period from January 2005 through December 2015 for all 50 states and contains healthcare service information for tens of millions of privately insured individuals each year (varying from year to year). The study sample is not nationally representative and the demographic characteristics of the sample are presented in Table 1. Table 1 shows that the sample does not contain any individuals aged 65 and older. Therefore, the derived prevalence rate is for a privately insured non-elderly (aged 64 and younger) cohort. In addition, Table 1 shows that the demographic characteristics remain relatively stable over this period. Institutional review board approval was obtained prior to the implementation of the study.
2.3 Study Measures
Opioid use disorder is a diagnosis introduced in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). It combines two disorders, Opioid Dependence and Opioid Abuse, from the previous edition of the Diagnostic and Statistical Manual, the DSM-IV-TR, and incorporates a wide range of illicit and prescription drugs from the opioid class. Following previous studies [18], we identified patients with OUD as those with an inpatient or outpatient claim with a primary ICD-9 diagnosis code of 304.0x, 304.7x, 305.5x, 965.0x , E850.0 – E850.2, or E935.0 – E935.2 and excluded those with a diagnosis of self-inflicted poisoning (E950.0 – E950.5) and assault by poisoning (E962.0x). Beginning in October 2015, ICD-10 diagnosis codes were used instead of ICD-9 diagnosis codes. Accordingly, for claims occurring in October 2015 onward, we used ICD-10 code F11.xx and T40.0 – T40.6 to identify OUD patients, and excluded those with a diagnosis of self-poisoning (T40.0X2, T40.1X2, T40.2X2, T40.3X2, T40.4X2, T40.5X2 and T40.6X2) and assault-by-poisoning (T40.0X3, T40.1X3, T40.2X3, T40.3X3, T40.4X3, T40.5X3 and T40.6X3).
State-level OUD prevalence rates were calculated using the total number of OUD patients divided by the total number of enrolled individuals[1] for that year in each state. Because there are no enrolled individuals aged 65 and older, the OUD prevalence rate is essentially for a non-elderly cohort (aged 64 or younger) only. OUD prevalence in 2015, the ending year of the sample period was investigated to study same-year cross-state variations. Moreover, absolute and relative changes in prevalence rates[2] between 2005 and 2015 were also calculated to study different time trends of the epidemic across states.
Due to the diagnosis codes changing from ICD-9 to ICD-10 in October 2015, the prevalence rates calculated for 2015 are not directly comparable to the prevalence rates calculated for 2005. To adjust for the effect of changing diagnosis codes, we assumed that the number of OUD patients identified in the first three quarters was a fixed fraction of the total number of OUD patients identified throughout the year. The data largely supports this assumption since the fraction was 84.4% in 2013 and 84.7% in 2014. However, this fraction became 81.2% in 2015, which indicated that the fraction of OUD patients identified in the fourth quarter of 2015 was higher than in previous years. This was likely due to the changing of diagnosis codes. Based on this assumption, we have:
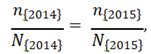
where n{2014} and n{2015} denote the number of OUD patients identified in the first three quarters of 2014 and 2015 respectively, and N{2014} and N{2015} denote the total number of OUD patients identified in the corresponding years. Therefore, we calculated the adjusted number of OUD patients in 2015 using the following formula:
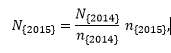
and calculated the adjusted OUD prevalence rate for 2015 using the adjusted number of OUD patients and the total number of enrollments in 2015. In the following analysis, all OUD prevalence rates in 2015 were adjusted using this method.
2.4 Data Analysis
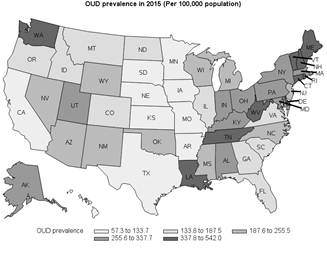
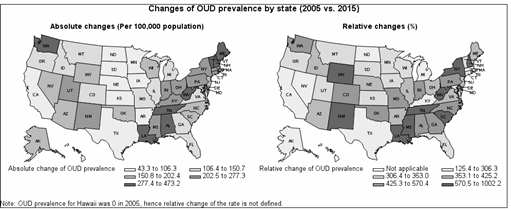
Figure 1 and Figure 2 utilize maps of the U.S. to show variations in the opioid epidemic across states. Figure 1 shows the variation in OUD prevalence across states in 2015. The OUD prevalence rates for the 50 states were categorized into 5 ranges such that each range contained 10 states. Figure 2 depicts the trends of change for the epidemic across states by showing the absolute and relative changes in OUD prevalence rates from 2005 to 2015.
To gain additional insight on the opioid epidemic in the states most affected by the epidemic, we classified the 50 states into two groups based on OUD prevalence rates in 2015. The 10 states with the highest OUD prevalence in 2015 were classified as the state group experiencing a relatively severe opioid epidemic, and the remaining states were used as a comparison group. To investigate contributing subpopulations to the relatively high OUD prevalence rates in these 10 states, we calculated the OUD prevalence in subpopulations identified by age group and sex, and compared those with their corresponding counterparts in the remaining states where the opioid epidemic was less severe. The relative change in the prevalence between 2005 and 2015 was also calculated for each group in each state to identify different rates of increase. Five age groups were considered as follows: 0-17, 18-35, 35- 44, 45-54, and 55-64.
We applied a one-sided Fisher exact test on OUD prevalence to compare demographic differences between the 10 states with more severe opioid epidemics and the remaining states. OUD patients were extracted using SAS software version 9.4 and an analysis of demographic difference was conducted using Stata software version 11.
3. Results
3.1 The Opioid Epidemic Across States
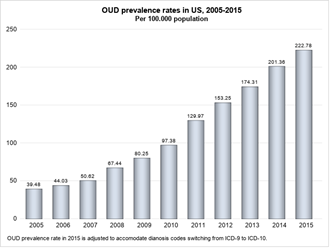
As shown in Figure 3, the national level of OUD prevalence monotonically increased from 2005 to 2015. It reached 222.78 per 100,000 population in 2015, which was more than 5 times the level in 2005 (39.48 per 100,000). Virtually all states experienced a dramatic increase in OUD prevalence during this period. In 2005, the median OUD prevalence in the 50 states was 40.4 (per 100,000) and all states except Michigan (112 per 100,000) had OUD prevalence rates below 100 per 100,000. However, in 2015 only four states, including South Dakota, Nebraska, Iowa and Hawaii had OUD prevalence rates below 100 per 100,000 population. The median OUD prevalence rate for the 50 states reached 239.3 (per 100,000), which was almost 6 times the median level in 2005.
Although all 50 states experienced a rapid increase in OUD prevalence, we can tell from Figure 1 that the level of prevalence rates varied substantially across states. The prevalence rates across the 50 states were categorized into 5 quintiles, with the highest range being 337.8 to 542.0 per 100,000, and the lowest range being 57.3 to 133.7 per 100,000. The eastern United States was most affected by the opioid epidemic in 2015 while the central United States had relatively low OUD prevalence rates. West Virginia, Rhode Island, Tennessee, Maine, Delaware, Washinton State, New Hampshire, Vermont, Connecticut and Louisiana were the 10 states with the highest OUD prevalence rates in 2015. Prevalence rates for these 10 states varied from 337.8 to 542.0 per 100,000 population, which was much higher than states in the central United States, such as South Dakota (57.3), Nebraska (84.8), Iowa (85.7), Hawaii (98.6), Minnesota (105.9) and Kansas (111.9). The epidemic in the western United States, in general, was not as severe as in the eastern United States. However, Washington State (386.4), Utah (276.7) and Alaska (271.3) were the three states in this region that had OUD prevalence rates in the top 20 states.
To study the time trends of the epidemic across the 50 states, Figure 2 presents the absolute change[3] and relative change[4] of state-level OUD prevalence rates during the 11-year timeframe. From the map of “absolute changes,” we can see that, in general, those states more affected by the epidemic in 2015 were also the ones that had large absolute changes in prevalence rates from 2005 to 2015. Most of the eastern United States had OUD prevalence rates increase by 227.4 to 473.2 per 100,000 population, while the increase in the central United States mainly ranged from 43.3 to 150.7 per 100,000. On the other hand, the map of “relative changes” showed cross-state variation in the percentage change of the prevalence rate during this period. The eastern United States again showed higher increasing rates than the majority of states in other regions. To summarize, the majority of states most impacted by the epidemic in 2015 showed a rapid increase in their prevalence rates both in terms of absolute and relative changes. Another finding worth noting is that Wyoming and New Mexico had the most rapid increase in terms of relative change, with Wyoming increasing by 1002% (from 17.8 to 188.3 per 100,000) and New Mexico increasing by 984.5% (from 21.21 to 230.1 per 100,000). Although the high relative changes in the prevalence rates in these two states were partially attributable to their low prevalence rates in 2005, the rates of increase were still astonishing. Some other states in the same region, such as Oklahoma, Colorado and Missouri, also had rapid increases in OUD prevalence, with their rates being 546.2%, 477.9% and 453.9%, higher than the median increasing rate of 378.9%.
3.2 Opioid Epidemic Development in Hard-hit States
As mentioned in the previous section, West Virginia, Rhode Island, Tennessee, Maine, Delaware, Washinton State, New Hampshire, Vermont, Connecticut and Louisiana were the 10 states with the highest OUD prevalence rates in 2015, hereafter collectively referred to as the “T10” states. These states also experienced a faster increase in OUD prevalence rates than most other states did. Since the epidemic was more severe in these states, we further analyzed trends of change in these states by analyzing the level and change of OUD prevalence in subpopulations defined by gender and age.
Table 2: Historical Ranks of OUD Prevalence for T10 States
|
State Name |
2005 |
2006 |
2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
2013 |
2014 |
2015 |
|
West Virginia |
9 |
11 |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
2 |
1 |
|
Rhode Island |
11 |
9 |
6 |
2 |
2 |
2 |
2 |
2 |
2 |
1 |
2 |
|
Tennessee |
13 |
17 |
14 |
16 |
15 |
14 |
15 |
15 |
17 |
8 |
3 |
|
Delaware |
19 |
25 |
23 |
8 |
4 |
8 |
3 |
3 |
3 |
5 |
4 |
|
Maine |
6 |
8 |
10 |
10 |
11 |
5 |
5 |
5 |
5 |
7 |
5 |
|
Washington |
12 |
14 |
7 |
4 |
5 |
7 |
6 |
7 |
8 |
6 |
6 |
|
Vermont |
1 |
2 |
4 |
2 |
3 |
4 |
10 |
6 |
7 |
3 |
7 |
|
New Hampshire |
28 |
13 |
15 |
19 |
18 |
12 |
14 |
12 |
6 |
9 |
8 |
|
Connecticut |
3 |
3 |
3 |
5 |
7 |
4 |
10 |
6 |
7 |
3 |
9 |
|
Louisiana |
21 |
26 |
19 |
22 |
27 |
23 |
21 |
23 |
22 |
15 |
10 |
Table 2 ranks the T10 states based on their state-level OUD prevalence rates for each year. The majority of T10 states ranked high in OUD prevalence since 2005. With the exception of Louisiana, the T10 states remained within the top 20 states for OUD prevalence in most years during the 11-year timeframe. Louisiana, which was ranked the 10th highest for OUD prevalence in 2015, previously ranked within the 20-30 range from 2005 to 2013, but experienced a rapid increase in 2014 and 2015, resulting in its 10th position in 2015.
Apart from being historically high, OUD prevalence in the T10 states generally increased more rapidly when compared to the remaining states[5], hereafter collectively referred as the “RM” states. The increasing rates of OUD prevalence in eight of the T10 states were above the median of 387%. Among them, seven exceeded 500%. Maine and Connecticut were the only two T10 states that had increasing rates, 307.9% and 302.6% respectively, lower than the median increasing rate. However, the relatively lower increasing rates in the two states are partially attributable to their high prevalence rates in 2015. The prevalence rates for Vermont and Connecticut were the 2nd and 3rd highest in 2015. The absolute changes of OUD prevalence in these two states were 288.3 and 265.3 per 100,000 population, which were much higher than the median level of 174.1 per 100,000 population. Therefore, it is reasonable to conclude that the 10 states most affected by the epidemic in 2015 also experienced rapid increases in OUD prevalence during the 11-year timeframe.
3.3 Demographic Difference of the Opioid Epidemic Between Two State Groups
To further examine the rapid spread of the opioid crisis within the T10 states, we investigated the level and change of OUD prevalence in various subpopulations within these states. In particular, we analyzed OUD prevalence in subpopulations classified by gender and age groups. Table 3 lists the OUD prevalence by gender and age groups for the T10 states in 2005 and 2015. As a comparison, the corresponding prevalence rates for the RM states are also shown. To test whether the OUD prevalence rate for each subpopulation in the T10 states was significantly higher compared to the corresponding subpopulations in the RM states, we applied the one-sided exact fisher test and presented the p-values in Table 3.
Table 3: OUD Prevalence (per 100,000) of Subpopulations and Relative Change of OUD Prevalence from 2005 to 2015
|
2005 |
2015 |
% change |
||||||
|
T10 |
RM |
p-value |
T10 |
RM |
p-value |
T10 |
RM |
|
|
Age group |
||||||||
|
0-17 |
13.9 |
10.3 |
0.01 |
17.3 |
13.1 |
0.002 |
24.5 |
27.2 |
|
18-34 |
112.9 |
64.7 |
<0.001 |
636.5 |
365.4 |
<0.001 |
463.7 |
464.8 |
|
35-44 |
82.3 |
60.2 |
<0.001 |
527 |
263.4 |
<0.001 |
540.3 |
337.5 |
|
45-54 |
72.7 |
66.8 |
0.09 |
409 |
207.5 |
<0.001 |
462.6 |
210.6 |
|
55-64 |
36.6 |
33.3 |
0.183 |
327.2 |
179.7 |
<0.001 |
794 |
439.6 |
|
Sex |
||||||||
|
Male |
73.3 |
51.3 |
<0.001 |
454 |
252.6 |
<0.001 |
519.4 |
392.4 |
|
Female |
53.3 |
39 |
<0.001 |
308.9 |
158.7 |
<0.001 |
479.5 |
306.9 |
As seen in Table 3, OUD prevalence patterns across subpopulations were similar in the T10 and RM state groups. From 2005 to 2015, both state groups experienced a dramatic increase in OUD prevalence for all age groups, with the exception of the 0-17 age group. Younger groups (except for the 0-17 age group) generally had higher OUD prevalence rates than older groups, with the peak prevalence appearing in the 18-34 age group. In 2005, the OUD prevalence rate for the 45-54 age group in the RM states was the highest across all age groups; however, in 2015, it was lower than the 18-34 and 35-44 age groups, indicating that the epidemic in the two younger groups deteriorated much faster than the 45-54 age group. Although the patterns of OUD prevalence across different subpopulations were similar, the difference between the two state groups was apparent. The OUD prevalence level for each subpopulation was generally much higher in the T10 states than in the RM states for both years. An exception to this is seen in the 45-54 and 55-64 age groups in both state groups, where the difference in prevalence rates was either marginally (p-value = 0.090) or not (p-value= 0.183) significant in 2005. However, the difference between the prevalence rates in these two age groups within the two state groups became statistically significant in 2015.
Although Table 3 shows that the 18-34 age group had the highest OUD prevalence rate across all age groups in the T10 states for both years, the 55-64 age group had the largest increasing rate of OUD prevalence from 2005 to 2015, with a percentage change of 794%. Although the same age group in the RM states also experienced a dramatic increase (439.5%) in OUD prevalence, the increasing rate was much lower than in the T10 states. In fact, the relative changes of OUD prevalence for the 45-54 and 55-65 age groups in the T10 states were about twice of those for the same age groups in the RM states. These differences were much larger than observed in the other age groups. In addition, Table 3 also shows that the change of OUD prevalence was drastic for both males and females in both state groups. Prevalence rates were much higher in males compared to females, suggesting that males are likely more vulnerable to this disease than females.
As seen in Table 3, OUD prevalence patterns across subpopulations were similar in the T10 and RM state groups. From 2005 to 2015, both state groups experienced a dramatic increase in OUD prevalence for all age groups, with the exception of the 0-17 age group. Younger groups (except for the 0-17 age group) generally had higher OUD prevalence rates than older groups, with the peak prevalence appearing in the 18-34 age group. In 2005, the OUD prevalence rate for the 45-54 age group in the RM states was the highest across all age groups; however, in 2015, it was lower than the 18-34 and 35-44 age groups, indicating that the epidemic in the two younger groups deteriorated much faster than the 45-54 age group.
Although the patterns of OUD prevalence across different subpopulations were similar, the difference between the two state groups was apparent. The OUD prevalence level for each subpopulation was generally much higher in the T10 states than in the RM states for both years. An exception to this is seen in the 45-54 and 55-64 age groups in both state groups, where the difference in prevalence rates was either marginally (p-value = 0.090) or not (p-value= 0.183) significant in 2005. However, the difference between the prevalence rates in these two age groups within the two state groups became statistically significant in 2015. Although Table 3 shows that the 18-34 age group had the highest OUD prevalence rate across all age groups in the T10 states for both years, the 55-64 age group had the largest increasing rate of OUD prevalence from 2005 to 2015, with a percentage change of 794%. Although the same age group in the RM states also experienced a dramatic increase (439.5%) in OUD prevalence, the increasing rate was much lower than in the T10 states. In fact, the relative changes of OUD prevalence for the 45-54 and 55-65 age groups in the T10 states were about twice of those for the same age groups in the RM states. These differences were much larger than observed in the other age groups.
In addition, Table 3 also shows that the change in OUD prevalence was drastic for both males and females in both state groups. Prevalence rates were much higher in males compared to females, suggesting that males are likely more vulnerable to this disease than females.
4. Discussion
Although a rapid increase in OUD prevalence is seen nationwide, there is a significant difference in the OUD epidemic across states. The results of this analysis show that the eastern United States was most affected by the epidemic in 2015. These findings are largely consistent with the CDC findings on rates of drug overdose death by state in 2015 [19]. In 2015, West Virginia had the highest overdose death rate (41.5 per 100,000 population) followed by New Hampshire (34.3 per 100,000). The overdose death rates for Rhode Island, Tennessee, Connecticut, Delaware and Maine varied from 21.2 to 28.2 per 100,000, which were higher than the median overdose death rate of 16.1 per 100,000 for all 50 states. It is worth noting that the overdose death rate for Utah and New Mexico was 23.4 and 25.3 per 100,000, respectively, ranking among the top 10 according to the CDC report. However, these two states ranked 17 and 24 out of 50 for OUD prevalence rates based on the results of our analysis. On the other hand, Washington State, which had the 6th highest OUD prevalence rate in 2015 based on our results, had an overdose death rate of 14.7 per100, 000, which was lower than the median death rate among the 50 states. The differences between our results and the death rates in the CDC report might be due to different research populations. Our study sample was from a privately insured population, while the CDC report was based on death certificates that were drawn from the entire population. Differences in the effectiveness of OUD treatment programs between states might also be a contributing factor. States with the same OUD prevalence rate but more effective treatment programs are likely to have lower overdose death rates.
Moreover, our results showed a staggering increase in OUD prevalence rates in the eastern states, most of which were historically harder-hit states as well. The rapid deterioration of the epidemic in these states indicates that the epidemic is showing no signs of slowing down. More effective interventions are needed in these states to curb the epidemic. In addition, our results also show a skyrocketing rate of increase in some Midwest states. This suggests that the OUD epidemic could be spreading to regions previously less impacted. More active and effective interventions should be taken in those states to prevent the rapid spread of the epidemic.
Previous studies found that the opioid epidemic did not conform to the stereotypical boundaries of age, gender, and geography [20]. The young males had been the most affected group [15,20]. Our study, based on data from a privately insured population, confirmed that almost every subgroup was affected by the OUD epidemic, with the 18-34 age group appearing to be the most vulnerable having the highest OUD prevalence across all age groups. In addition, we found that after the mid-30s, increasing age was associated with a decrease in OUD prevalence. This is consistent with the previous finding that OUD prevalence peaks among those between 18 and 29 years of age and then decreases as age increases [21] This might partly be due to early mortality or remission of symptoms after reaching age 40 [22]. It is also worth noting that although our findings show that the prevalence of the disorder was highest in the 18-34 age group, OUD prevalence for the 55-64 age group increased most rapidly, especially in the T10 states. More specifically, from 2005 to 2015, OUD prevalence increased by 794.0% in the T10 states and 439.6% in the RM states for this age group. This drastic increase in OUD prevalence in the 55-64 age group was likely caused by the dramatic increase in prescription opioids during this period, since this age group, in general, is more likely to use opioid-involved pain medications than other groups. The fact that the prevalence rate was much higher in the T10 states might suggest more aggressive opioid prescribing activities in those states. A multifaceted approach, including educating health professionals and the public about the appropriate use of opioids, implementing prescription drug monitoring programs, enhancing accessibility to non-opioid pain medications, etc., should be taken to battle the disorder.
4.1 Limitations
The findings of this research are subject to the following limitations. First, the data used in this study cover the period from 2005 to 2015, which does not capture recent trends of change in the OUD epidemic. Analysis of more recent data would be meaningful to catch recent changes in the trends. Second, the identification of OUD patients in this study was based on OUD-related diagnosis codes from outpatient and inpatient claims. Since drug claims do not contain diagnosis codes, we were not able to identify those patients who only had claims for medications used to treat OUD (e.g., buprenorphine) for the entire year. From this point of view, the OUD prevalence calculated in this study might be underestimated. However, we believe that the bias may be minimal since clinical guidelines state that patients on OUD pharmacotherapy should be monitored regularly and receive psychosocial treatment [23], which would result in inpatient or outpatient claims. Moreover, like all studies based on claims data, our study was not able to capture those OUD patients who never seek treatment. This is another possible factor causing an underestimation of OUD prevalence in the commercially insured population. In addition, due to diagnosis codes changing from ICD-9 to ICD-10 in October 2015 and the fact that no one-on-one mapping exists between the two sets of codes, the classification of OUD patients might not be fully consistent. Although we have made reasonable adjustments on OUD prevalence in 2015, the estimation of OUD prevalence in 2015 and the change of prevalence from 2005 to 2015 can still be affected by the change in diagnosis codes.
5. Conclusion
By investigating state-level OUD prevalence from 2005 to 2015 using data from the MarketScan database, we found that although most states experienced drastic increases in OUD prevalence nationwide, cross-state variations were also substantial both in terms of severity and acceleration of the epidemic. The sharp increase in OUD prevalence and variations across states indicate that more effective and localized interventions are needed to curb the epidemic. The alarming increase in OUD prevalence among the 55-64 age group might indicate the need for improved prescription drug monitoring programs, especially in states more affected by the epidemic. Our study provides a valuable reference for policy makers when designing targeted clinical and policy interventions and guidelines to address the opioid epidemic in the United States.
Conflict of Interest:
The authors report no conflicts of interest.
References
- Bachhuber MA, Mehta PK, Faherty LJ, et al. Medicaid Coverage of Methadone Maintenance and the Use of Opioid Agonist Therapy Among Pregnant Women in Specialty Med Care 55 (2017): 985-990.
- Drug Poisoning Mortality: United States, 1999-2015. NCHS Data (2017).
- Rudd RA, Seth P, David F, et al. Increases in Drug and Opioid-Involved Overdose Deaths – United States, 2010-2015. MMWR Morb Mortal Wkly Rep 65 (2016): 1445-
- Rudd RA, Aleshire N, Zibbell JE, et al. Increases in Drug and Opioid Overdose Deaths-- United States, 2000-2014. MMWR Morb Mortal Wkly Rep 64 (2016): 1378-
- Prevention Increases in Drug and Opioid-Involved Overdose Deaths — United States, 2010–2015.: Morbidity and Mortality Weekly Report (2016).
- Overdose Deaths Involving Opioids, Cocaine, and Psychostimulants — United States, 2015–2016. Morbidity and Mortality Weekly Report (MMWR) 67 (2018): 10.
- Florence CS, Zhou C, Luo F, et al. The Economic Burden of Prescription Opioid Overdose, Abuse, and Dependence in the United States, Med Care 54 (2016): 901-906.
- Warner M, Chen LH, Makuc DM, et al. Drug poisoning deaths in the United States, 1980-2008. NCHS Data Brief 81 (2011): 1-
- Rossen LM, Khan D, Warner Trends and geographic patterns in drug-poisoning death rates in the U.S., 1999-2009. Am J Prev Med 45 (2013): 19-25.
- Paulozzi LJ, Ryan Opioid analgesics and rates of fatal drug poisoning in the United States. Am J Prev Med. 31 (2006): 506-511.
- Seth P, Scholl L, Rudd RA, et al. Overdose Deaths Involving Opioids, Cocaine, and Psychostimulants - United States, 2015-2016. MMWR Morb Mortal Wkly Rep 67 (2018): 349-
- Planalp CaL, The Opioid Epidemic: State Trends in Opioid-Related Overdose Deaths from 2000 to 2015. 10 (2017).
- McDonald DC, Carlson K, Izrael Geographic variation in opioid prescribing in the U.S. J Pain 13 (2013): 988-996.
- Centers for Disease C, CDC grand rounds: prescription drug overdoses - a U.S. epidemic. MMWR Morb Mortal Wkly Rep 61 (2012): 10-13.
- Vital Signs: Overdoses of prescription opioid pain relievers - United States, 1999-2008. MMWR Morb Mortal Wkly Rep 60 (2011): 6.
- Kounang 41 state attorneys general subpoena opioid manufacturers. CNN (2017).
- Becker WC, Fiellin DA, Merrill JO, et Opioid use disorder in the United States: insurance status and treatment access. Drug Alcohol Depend 94 (2008): 207-213.
- Naeger S, Mutter R, Ali MM, et al. Post-Discharge Treatment Engagement Among Patients with an Opioid-Use J Subst Abuse Treat 69 (2016): 64-71.
- Drug Overdose Death (2018).
- Health An Assessment of Fatal and Nonfatal Opioid Overdoses in Massachusetts (2011 -2015). 54 (2017).
- Wu LT WG, Yang C, Blazer How do prescription opioid users differ from users of heroin or other drugs in psychopathology: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Addict Med 5 (2020): 8.
- Gnanavel S, Robert Diagnostic and statistical manual of mental disorders, fifth edition, and the impact of events scale-revised. Chest 144 (2013): 1974.
- Medicine The National Practice Guideline: For the Use of Medications in the Treatment of Addiction Involving Opioid Use. (2015).