Consulting Readings of Home Blood Pressure Monitoring With Doctor Increases the Effectiveness of Antihypertensive Therapy in Daily Clinical Practice
Article Information
Jerzy Chudek1*, Aleksander Jerzy Owczarek2, Magdalena Olszanecka-Glinianowicz3, Agnieszka Almgren-Rachtan4
1 Department of Internal Medicine and Oncological Chemotherapy, Medical Faculty in Katowice, Medical University of Silesia, Katowice, Poland
2 Department of Statistics, Department of Instrumental Analysis, School of Pharmacy and Laboratory Medicine in Sosnowiec, Medical University of Silesia, Katowice, Poland
3 Health Promotion and Obesity Management Unit, Department of Pathophysiology, Medical Faculty in Katowice, Medical University of Silesia, Katowice, Poland
4 Department of Pharmacovigilance, Europharma Rachtan Co. Ltd., Katowice, Poland
*Corresponding author: Jerzy Chudek, Department of Internal Medicine and Oncological Chemotherapy, Medical Faculty in Katowice, Medical University of Silesia, Katowice, Poland
Received: 12 August 2019;Accepted: 22 August 2019;Published: 04 September 2019
Citation: Jerzy Chudek, Aleksander Jerzy Owczarek, Magdalena Olszanecka-Glinianowicz, Agnieszka Almgren-Rachtan. Consulting Readings of Home Blood Pressure Monitoring With Doctor Increases the Effectiveness of Antihypertensive Therapy in Daily Clinical Practice. Cardiology and Cardiovascular Medicine 3 (2019): 290-302.
View / Download Pdf Share at FacebookAbstract
Background: The routine home blood pressure monitoring (HBPM) is strongly recommended for management of hypertension, however the evidence concerning the improvement of blood pressure (BP) control related to self-measurement of BP is weak. The aim of this study was to assess the efficacy of antihypertensive therapy in relation to the consulting of HBPM readings with physicians in daily clinical practice.
Patients & methods: The survey was conducted by 627 physicians among 21,940 hypertensive patients, of whom 17,143 (8,972 women and 8,171 men; mean age of 63 ± 12 years) were receiving antihypertensive medication for at least 6 months. BP control was scored based on two office BP measurements (< 140/90 mmHg).
Results: Among patients declaring performing HBPM (N = 14,524), 86.6% were consulting the readings with physicians. Patients consulting the readings had lower systolic (by 6.4 mmHg) and diastolic (by 3.4 mmHg) BP than those not consulting their HBPM results, and by 5.3 and 4.5 mmHg than those not measuring BP at home. Patients consulting the HBPM results were obtaining more frequently recommended BP control (54.2%). BP control was similar in patients performing but not consulting HBPH readings and not doing HBPM (35.8 and 35.7%, respectively).
Conclusion: The benefits of home blood pressure monitoring are restricted to patients consulting the readings with physicians.
Keywords
Hypertension, home blood pressure monitoring, efficacy of hypertensive therapy, therapeutic goals, daily clinical practice; blood pressure control; consulting BP results; BP records
Article Details
Abbreviations
ACE-I - Angiotensin converting enzyme inhibitor ABPM - Ambulatory blood pressure monitoring ANOVA - Analysis of variance
ARB - Angiotensin II receptor antagonist BP - Blood pressure
C - Consulting the results CAD - Coronary artery disease
CCB - Calcium channel blocker CKD - Chronic kidney disease CI – Confidence interval
CRAN - Comprehensive R Archive Network CVD - Cerebrovascular disease
ESC - European Society of Cardiology ESH - European Society of Hypertension HBPM - Home blood pressure monitoring NC - Not consulting the results
NHANES - National Health and Nutrition Examination Survey OBPM - Office blood pressure monitoring
OR – Odds ratio
p - Value, probability
SPRINT - The Systolic Blood Pressure Intervention Trial TIA - Transient ischemic attack
WHO – World Health Organization VIF - The variance inflation factor
1. Introduction
In the beginning of this decade, high blood pressure (7% of global estimated deaths and disability-adjusted life years), tobacco smoking including second-hand smoke (6.3%) and alcohol abuse (5.5%) were identified as the three leading risk factors for global disease burden [1]. Despite the substantial improvements in awareness and efficacy in the treatment of hypertension, half of the patients did not reach the recommended blood pressure (BP) targets in the US [2] and Europe [3]. A population based study among older Poles performed in years 2007-2012 revealed that more than 60% of treated hypertensive patients had not met the recommended BP goals [4]. The recently performed SPRINT study showed that hypertensive, nondiabetic patients with increased cardiovascular risk may benefit from the reduction of systolic BP even below 120 mmHg, obtaining lower mortality rates [5].
Office blood pressure monitoring (OBPM) remains the usual care and a gold standard for hypertension management [6]. However, the values of OBPM are usually higher than home BP values and ambulatory BP monitoring (ABPM), as the result of ‘white coat effect’ [7]. It was shown that incidence of cardiovascular disease with reference to OBPM values corresponded to that of a 5 mmHg lower value of ABPM in a meta- analysis [8] and this difference is reflected in most guidelines.
The routine HBPM is strongly recommended not only for diagnosis but also for management of hypertension [5]. Weak evidence supporting the reduction in BP related to HBPM is coming from systematic reviews and meta-analyses [9, 10]. An analysis of 52 prospective comparative studies of HBPM with or without additional support in relation to usual care showed 3.9 and 2.4 mmHg benefit in systolic BP and diastolic BP, respectively after 6 months, but the effect disappeared after 12 months [9]. The effect only persisted after 12 months in studies combining HBPM with additional support (education, pharmacist intervention), accounting for a 3.4 – 8.9 mmHg reduction in systolic BP and a 1.9 – 4.4 mmHg reduction in diastolic BP [9]. More recent meta-analysis of 25 randomized controlled trials reveled a 6.1 mmHg reduction in systolic BP, but only when monitoring was combined with intensive support (patients counseling, telemonitoring, pharmacist intervention). Self-monitoring of HBPM alone was completely ineffective [10]. This casts doubts whether HBPM improves adherence to treatment as was shown by Ogedegbe et al. [11].
The availability of good quality BP monitors increases their use in daily clinical practice. They are increasingly perceived as necessary for daily use both by physicians and their patients, similarly as glucose monitoring in diabetics. Frequently, self-monitoring is performed as a protective tool against the fear of a silent but serious clinical condition [12]. However, there is the lack of data on how HBPM affects the efficacy of BP control in daily clinical practice.
The aim of this study was to assess the efficacy of antihypertensive therapy in relation to consulting of HBPM readings with physicians in daily clinical practice.
2. Materials and Methods
The survey was carried out by 627 family doctors, internal medicine doctors and cardiologists as well as doctors during specialization, on a group of 21,940 outpatients pharmacologically treated for hypertension for at least 6 months. There were no other inclusion criteria with the exception of the agreement to participate in the survey. The exclusion criterion was the inability to obtain answers to questions in the questionnaire. The study did not meet the criterion of a medical experiment and did not require the approval of the Bioethical `Committee. The study organizer (Europharma) did not process patients' personal data.
3. Survey procedures
The study questionnaire was filled out by the physicians participating in the survey based on an interview and data from the medical history.
The questionnaire included data concerning: patients age, gender, selected anthropometric measures (body mass, height, waist circumference), two attended office blood pressure measurements (OBPM), period of treatment for hypertension, pharmacotherapy of hypertension in the last months (monotherapy / polytherapy / current medications), the highest recorded blood pressure before initiation of treatment, severity of hypertension, comorbidities, carrying out and recording home blood pressure measurements (HBPM), and whether the patient is bringing the recorded HBPM values on control visits. Finally, the physician was scoring the recorded HBPM measurements if most of them were < 135/85 mmHg.
4. Data analysis
The blood pressure control was assessed on the basis of the mean values of systolic and diastolic BP of two OBPMs. The values of less than 140/90 mmHg were scored as good BP control in accordance with the recommendations of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) [6].
Coronary artery disease (CAD) was defined as history of acute myocardial infarction, percutaneous coronary intervention, coronary artery bypass graft, or the occurrence of symptoms of angina pectoris.
Cerebrovascular disease (CVD) was defined as history of ischemic stroke or intracerebral hemorrhage or transient ischemic attack (TIA).
Heart failure was diagnosed based on clinical sign and symptoms and included patients with preserved ejection fraction of the left ventricle.
Chronic kidney disease was defined as the occurrence of estimated glomerular filtration rate below 30 ml/min/1.73m2 and/or proteinuria over 300 mg/24 hrs.
5. Statistical analysis
There were 18,357 questionnaires completed by the physicians. However, 1214 of them did not meet the inclusion criteria (6-month period of treatment for hypertension) or were incomplete and were excluded from the analysis. Therefor the final analysis was included questionnaires of 17,143 patients. Statistical analysis was performed using the STATISTICA 10.0 PL (Tibco Software Inc, Palo Albo, USA), StataSE 12.0 (StataCorp LP, TX, U.S.) and R software (CRAN). Statistical significance was set at a p-value below 0.05. All tests were two-tailed. Imputations were not done for missing data. Nominal and ordinal data were expressed as percentages, while interval data were expressed as mean value ± standard deviation in the case of a normal distribution or as the median and interquartile range in the case of data with skewed or non-normal distribution. Distribution of variables was evaluated by the Shapiro- Wilk test and the Cullen-Frey graph. Homogeneity of variances was assessed by the Fisher-Snedecor test. For comparison of data, the one-way ANOVA analysis was used with RIR Tukey posthoc test. Categorical variables were compared using χ2 tests. The stepwise backward multivariable logistic regression was used to assess factors affecting BP control (results were presented with odds ratio with a 95% confidence interval and corresponding p-value), while stepwise backward linear regression was used to assess factors affecting systolic and diastolic blood pressure. The variance inflation factor (VIF) was used to assess the multicollinearity, and to eliminate co-linear variables.
6. Results
Study groupThe group covered by this analysis included 17,143 patients with hypertension: 8,972 women and 8,171 men. The mean age was 63 ± 12 years. Stage III hypertension was diagnosed in less than one fifth of patients. More than half of patients were treated for at least 5 years. Overweight or obesity, according to WHO criteria, was diagnosed in 80.3% of patients. Other comorbidities are presented in the Table 1.
Table 1: Comparison of hypertensive patients performing or not performing home blood pressure monitoring and those consulting and not consulting the results with physicians on control visits.
ACE-I - angiotensin converting enzyme inhibitor, ARB - Angiotensin II receptor antagonist; BP – blood pressure, C - Consulting the results, CAD - coronary artery disease, CCB - calcium channel blocker, CKD – chronic kidney disease, CVD -cerebrovascular disease, NC - not consulting the results, HBPM - Home blood pressure monitoring, OBPM - Office blood pressure monitoring.
HBPM was carried out by 89.8% of women and 79.1% of men. Among those, 90.0% of women and 82.2% of men carrying out the measurements were presenting the reading during control visits.
In the whole group, mean systolic and diastolic BP (OBPM) were 141.0 ±14.6 and 84.7 ± 10.0 mmHg, respectively. According to the assessment of home measurements, hypertension was successfully treated in 46.1% of the study group (Table 1).
Pharmacotherapy of hypertensionAmong the study group 19.6% of patients were treated with monotherapy and 80.4% with polytherapy, receiving 3.1 ± 1.0 drugs on average. Angiotensin converting enzyme inhibitors, β-adrenolytic and dihydropyridine calcium channel blockers were the most commonly used antihypertensive drugs (Tab. 1). One-third of the patients were treated with thiazide or thiazide-like diuretics. Loop diuretics were less frequently used.
Efficacy of antihypertensive therapy in relation to HBPM and its results consulting with physicianAmong patients declaring conducting HBPM (N = 14,524), 86.6% (N = 12,572) were consulting the results with physicians. Patients consulting the HBPM readings had lower systolic and diastolic BP, by 6.4 and 3.4 mmHg respectively, than those performing but not consulting HBPM results, and by 5.3 and 4.5 mmHg respectively, than those not measuring BP at home (Tab. 1). In parallel, the patients consulting the HBPM results more frequently obtained the recommended BP control: 54.2% vs 35.8 and 35.7%, respectively (Tab. 1). Of note, the percentage of patients obtaining the recommended BP control was similar in patients performing but not consulting HBPM readings and not doing HBPM.
There were substantial differences between the study subgroups. There were least men, smokers and obese and treated with monotherapy among patients conducting and consulting HBPM readings with physician on the control visits (Table 1).
Multivariate regression analysis modelsFollowing factors were included in multivariable models: age, gender, hypertension stage and its treatment time above 5 years, smoking, nutritional status (overweight and obesity), occurrence of diabetes, CAD/CVD, heart failure, CKD as well as hypertensive
polytherapy. Factors increasing BP control were CAD/CVD, consulting the HBPM readings, and to less extent performing but not consulting HBPM readings. While decreased BP control were observed in the elder, smokers, overweigh and obese patients, suffering from more severe stages of hypertension, and with heart failure, and CKD (Table 2).
|
Variable |
OR |
-95% CI |
+95% CI |
p |
|
Age [years] |
0.978 |
0.976 |
0.982 |
< 0.001 |
|
Smoking (yes vs. no) |
0.662 |
0.615 |
0.712 |
< 0.001 |
|
Overweight vs normal weight |
0.790 |
0.719 |
0.868 |
< 0.001 |
|
Obesity vs normal weight |
0.456 |
0.415 |
0.502 |
< 0.001 |
|
CAD + CVD (yes vs. no) |
1.330 |
1.223 |
1.446 |
< 0.001 |
|
Heart failure (yes vs. no) |
0.638 |
0.579 |
0.704 |
< 0.001 |
|
CKD (yes vs. no) |
0.641 |
0.551 |
0.745 |
< 0.001 |
|
Hypertension stage II vs. I |
0.739 |
0.684 |
0.799 |
< 0.001 |
|
Hypertension stage III vs. I |
0.485 |
0.439 |
0.537 |
< 0.001 |
|
HBPM Non-consulting vs. No |
1.133 |
0.985 |
1.304 |
0.08 |
|
HBPM Consulting vs. No |
2.714 |
2.455 |
3.000 |
< 0.001 |
Table 2: Results of stepwise backward logistic regression analysis concerning factors associated with blood pressure control.
CAD - Coronary artery disease, CKD - Chronic kidney disease, CI – confidence interval, CVD - Cerebrovascular disease, HBPM - Home blood pressure monitoring, OR – odds ratio, p - Value, probability
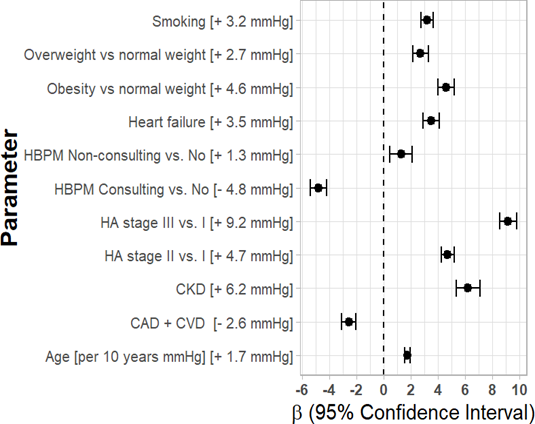
Mean systolic OBPM were diminished in subjects with CAD/CVD (by 2.6 mmHg) and in patients consulting the HBPM results (by 4.8 mmHg), while smoking, overweight and obesity, more severe stages of hypertension, heart failure, CKD, older age and non-consulting HBPM readings were factors increasing the OBPM values (Figure 1).
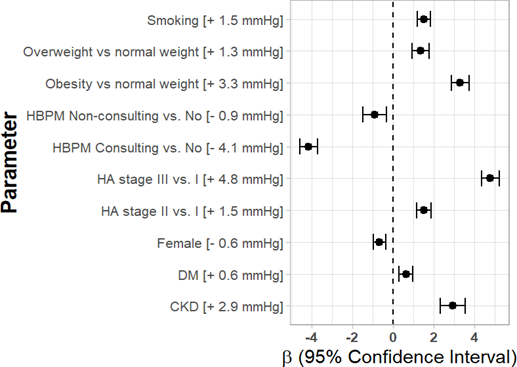
Mean diastolic OBPM were slightly diminished in patients non-consulting HBPM readings (by 0.9 mmHg), and much more in those consulting the readings (by 4.1 mmHg). What is more, they were increased in smokers, higher stages of hypertension, overweight, obese, with diabetes and with CKD (Figure 2).
7. Discussion
The implementation of HBPM in daily clinical practice in Poland, as in the other countries, is growing even without reimbursement of the purchase of BP meters by the national health systems. HBPM gives patients a more active role in the management of hypertension, may improve adherence to the therapy and the quality of care. In this study HBPM was carried out by 89.8% of hypertensive women and 79.1% of men. In comparison, in France a survey performed by 500 general practitioners revealed that the percentage of HBPM users increased from 70% in 2004 to 92% in 2009, with one-fifth using this method nearly systematically [13]. The benefits related to the use of HBPM, raised by physicians in this survey, included among other: therapeutic adaptation, and better adherence to the treatment [13]. Another advantage related to consultation of HBPM readings with a physician is an enhanced doctor-patient therapeutic relationship [14] that may increase adherence to antihypertensive therapy and its effectiveness. Nevertheless, HBPM protocol is troublesome to incorporate into daily schedule for professionally active people [15] and may also create confusion in some patients with regard to the BP target and lead to making their own decisions (restriction of pharmacotherapy) based on their own standards [14]. Therefore, HBPM has to be combined with patient education, at least concerning the protocol of BP measurement to obtain accurate results, readings timing, and the specific, lower for HBPM than OBPM targets [16, 17]. In addition, the patient should be informed about self-management of abnormal BP values.
Little is known about patients’ behaviors related to the nonuse of owned BP monitors, and the lack of adherence concerning bringing BP records (dairies). In our study this subgroup of patients included more men, and those diagnosed with obesity and heart failure. Thus, we suggested that the perception of hypertension as a chronic disease and the attention to their own health in these patients differ, however these aspects were not studied. We can say a little bit more about patients not performing HBPM. This subgroup was the youngest, and included the highest percentage of men, much more smokers – disregarding health, but less patients with diabetes, who are used to self-management. Health attitudes seems to explain the differences in HBPM implementation and not bringing BP records to the control visits, and in consequence a lower adherence to antihypertensive therapy. In NHANES study, HBPM was more frequently performed by the older adults, diabetics and obese, subjects with middle-income level, higher healthcare utilization, health insurance, and with well-controlled hypertension [18]. Of note, in our study, the number of antihypertensive drugs used in polytherapy did not differ markedly between the study subgroups, therefore the differences in BP control cannot be explained, but may reflect better adherence to medication. This important issue necessitates further research.
The main study finding is the evidence that patients consulting the HBPM records had lower systolic (by 6.4 and 5.3 mmHg) and diastolic (by 3.4 and 4.5 mmHg) BP, and more frequently obtained recommended BP values in OBPM than those performing but not consulting HBPM readings, and those not measuring BP at home, in a large unselected cohort in a daily clinical practice. Of note, the difference was independent of clinically important confounding factors such as severity of hypertension, time of treatment, gender, smoking status, co-morbidities (obesity, diabetes, CAD and CVD, heart failure, CKD). In the multivariate regression analysis patients consulting HBPM readings with physicians had lower systolic and diastolic BP by and 4.1 mmHg, independent from confounding factors such as: severity of hypertension, age, gender, hypertension treatment time > 5 years, smoking, overweight and obesity, diabetes, CAD/CVD, heart failure, CKD as well as This group of patients also more frequently obtained the recommended BP control.
The observed difference in BP control related to the consulting of HBPM readings is slightly smaller than demonstrated in already mentioned meta-analysis of randomized control trials, showing 6.1 mmHg decline in systolic BP when HBPM was combined with intensive support [10].
Abbreviations: CAD - Coronary artery disease; CKD - Chronic kidney disease; CVD - Cerebrovascular disease; HA – Hypertension; HBPM - Home blood pressure monitoring
Abbreviations: CKD - Chronic kidney disease; DM – Diabetes; HA – Hypertension; HBPM - Home blood pressure monitoring
This study has some limitations related to the study design. OBPM was performed with various BP monitors. Performance of HBPM, and not bringing the BP diaries was declared by the patients, therefore we cannot be sure that patients were performing the BP measurements at home. In addition, we neither assessed factors affecting the adherence to HBPM, nor the adherence to pharmacotherapy. Furthermore, the group of patients with better adherence to HBPM could include more frequent users of healthcare service, and therefore were overrepresented in the study cohort.
Conclusion
The benefits of home blood pressure monitoring are restricted to patients consulting the readings with physicians.
Acknowledgment
This study and the associated article processing charges were funded by a scientific grant of Recordati Polska Co.Ltd. (RECO/NT/2018). Europharma Rachtan Co. Ltd. designed the study and is the copyright holder.
All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and the accuracy of the data analysis. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Conflict of interest
Aleksander Owczarek received honorarium for statistical analysis. Magdalena Olszanecka- Glinianowicz received honorarium for the project drafting. Agnieszka Almgren-Rachtan is employed by Europharma Rachtan Co. Ltd (Director of the Department of Pharmacovigilance). Jerzy Chudek received honorarium for data analysis and manuscript drafting.
Compliance with ethics guidelines
According to the Polish law, surveys are not medical experiments and as such do not require either Bioethical Committee approval or the need to obtain informed consent from the patients for inclusion.
References
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990- 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380 (2012): 2224-2260.
- Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA 303 (2010): 2043-2050.
- Borghi C, Tubach F, De Backer G, Dallongeville J, Guallar E, et al. Lack of control of hypertension in primary cardiovascular disease prevention in Europe: Results from the EURIKA Int J Cardiol 218 (2016): 83- 88.
- Zdrojewski T, Wizner B, Wi?cek A, ?lusarczyk P, Chudek J,et al. Prevalence, awareness, and control of hypertension in elderly and very elderly in Poland: results of a cross-sectional representative survey. J Hypertens 34 (2016):532-538.
- Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. SPRINT Research Group. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 373 (2015): 2103-2116.
- Williams B, Mancia G, Spiering W, AgabitiRosei E, Azizi M, Burnier M, et al. ESC ScientificDocumentGroup. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart 39 (2018): 3021- 3104.
- Pickering TG, Gerin W, Schwartz What is the white-coat effect and how should it be measured? Blood Press Monit. 7 (2002): 293- 300.
- Niiranen TJ, Asayama K, Thijs L, Johansson JK, Ohkubo T, Kikuya et al. International Database of Home blood pressure in relation to Cardiovascular Outcome Investigators. Outcomedriven thresholds for home blood pressure measurement: international database of home blood pressure in relation to cardiovascular outcome. Hypertension 61 (2013): 27–34.
- Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med 159(3) (2013): 185-194.
- Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, et al. Self-monitoring of blood pressure in hypertension: A systematic review and individual patient data meta-analysis. PLoS Med 14 (2017) e1002389.
- Ogedegbe GO, Boutin-Foster C, Wells MT, Allegrante JP, Isen AM, Jobe JB, Charlson A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive African Americans. Arch Intern Med. 172 (2012): 322-326.
- Grant S, Greenfield SM, Nouwen A, McManus Improving management and effectiveness of home blood pressure monitoring: a qualitative UK primary care study. Br J Gen Pract 65 (2015): e776-783.
- Boivin JM, Tsou-Gaillet TJ, Fay R, Dobre D, Rossignol P, Zannad F. Influence of the recommendations on the implementation of home blood pressure measurement by French general practitioners: a 2004-2009 longitudinal survey. J Hypertens 29 (2011): 2105-2115.
- Abdullah A, Othman The influence of self- owned home blood pressure monitoring (HBPM) on primary care patients with hypertension: a qualitative study. BMC Fam Pract 12 (2011): 143.
- Milot JP, Birnbaum L, Larochelle P, Wistaff R, Laskine M, Van Nguyen P, Lamarre-Cliche M. Unreliability of home blood pressure measurement and the effect of a patient-oriented intervention. Can J Cardiol 31 (2015): 658-663.
- Carter EJ, Moise N, Alcántara C, Sullivan AM, Kronish IM. Patient Barriers and Facilitators to Ambulatory and Home Blood Pressure Monitoring: A Qualitative Study. Am J Hypertens. 31 (2018): 919-927.
- Kronish IM, Kent S, Moise N, Shimbo D, Safford MM, Kynerd RE, O'Beirne R, Sullivan A, Muntner P. Barriers to conducting ambulatory and home blood pressure monitoring during hypertension screening in the United States. J Am Soc Hypertens 11 (2017): 573-580.
- Ostchega Y, Zhang G, Kit BK, Nwankwo Factors Associated With Home Blood Pressure Monitoring Among US Adults: National Health and Nutrition Examination Survey, 2011-2014. Am J Hypertens 30 (2017): 1126-1132.