Consensus Statement on the Diagnosis and Management of Functional Abdominal Pain (FAP) and Related Disorders in Children
Article Information
Bhaswati Acharyya1, Sanjeev Joshi2, Sanjay Wazir3, A.G. Karthikeyan4, Vyankatesh M. Chavan5, I. Shrikanth Rao6, Chaitanya Balloji7, Neha8, Krishna Chaitanya Veligandla8, Rahul Rathod8, Bhavesh Kotak8, Aditi Upadhayay9, Monjori Mitra1*
1Institute of Child Health, Kolkata, West Bengal, India
2Chirayu Criticare and Joshi Bal Rugnalay. Yavatmal, Maharashtra, India
3Neonatology at Cloud Nine Hospital, Gurgaon, India
4Sai Mother and Child Health Care, Royapettah, Chennai, India
5Bhagwaan Mahaveer Jain Hospital, Vasanthanagar, Bangalore, India
6Chetana Hospital, Puttur, Udupi, India
7Chaitanya Balloji Clinic in Ramachandra Rao Pet, West Godavari, India
8Dr. Reddy's Laboratories Ltd., Hyderabad, India
9Medclin Research Pvt. Ltd., Kolkata, West Bengal, India
*Corresponding Author: Monjori Mitra, Professor, Department of Pediatrics, Institute of Child Health, 11 Biresh Guha Street Kolkata, West Bengal, India
Received: 28 September 2023; Accepted: 20 October 2023; Published: 20 November 2023
Citation: Bhaswati Acharyya, Sanjeev Joshi, Sanjay Wazir, A.G. Karthikeyan, Vyankatesh M. Chavan, I. Shrikanth Rao, Chaitanya Balloji, Neha, Krishna Chaitanya Veligandla, Rahul Rathod, Bhavesh Kotak, Aditi Upadhayay, Monjori Mitra. Consensus Statement on the Diagnosis and Management of Functional Abdominal Pain (FAP) and Related Disorders in Children. Journal of Pediatrics, Perinatology and Child Health. 7 (2023): 218-228.
View / Download Pdf Share at FacebookAbstract
Functional Abdominal Pain (FAP) related to Functional Gastrointestinal Disorders (FGIDs) pose a common yet underdiagnosed challenge in paediatric healthcare, which can exert a detrimental toll on children's mental well-being. Unfortunately, these disorders often go unrecognized, leading to a lack of appropriate diagnostic testing and suboptimal management and follow-up. Expert consultations and existing evidence were utilised to formulate consensus guidelines for the holistic management of paediatric functional gastrointestinal disorders. FGIDs warrant significant attention in the medical community due to their prevalence and profound impact on the quality of life of the children. Diagnosis, investigation, management, and ongoing monitoring are critical aspects of addressing FGIDs effectively. By nurturing a strong patient-physician relationship, considering a range of biological and psychosocial interventions, parental counselling, physicians can offer a more holistic approach to managing FGIDs in paediatric patients. This consensus strategy on diagnosis and management of FAP can help alleviate symptoms, improve outcomes, and ultimately enhance the overall well-being of affected children.
Keywords
Functional abdominal pain; Functional Gastrointestinal disorders; Irritable bowel syndrome; Abdominal migraine; Functional dyspepsia; Cognitive behaviour therapy; ROME criteria; Limosilactobacillus reuteri
Functional abdominal pain articles Functional abdominal pain Research articles Functional abdominal pain review articles Functional abdominal pain PubMed articles Functional abdominal pain PubMed Central articles Functional abdominal pain 2023 articles Functional abdominal pain 2024 articles Functional abdominal pain Scopus articles Functional abdominal pain impact factor journals Functional abdominal pain Scopus journals Functional abdominal pain PubMed journals Functional abdominal pain medical journals Functional abdominal pain free journals Functional abdominal pain best journals Functional abdominal pain top journals Functional abdominal pain free medical journals Functional abdominal pain famous journals Functional abdominal pain Google Scholar indexed journals Child health articles Child health Research articles Child health review articles Child health PubMed articles Child health PubMed Central articles Child health 2023 articles Child health 2024 articles Child health Scopus articles Child health impact factor journals Child health Scopus journals Child health PubMed journals Child health medical journals Child health free journals Child health best journals Child health top journals Child health free medical journals Child health famous journals Child health Google Scholar indexed journals Infants articles Infants Research articles Infants review articles Infants PubMed articles Infants PubMed Central articles Infants 2023 articles Infants 2024 articles Infants Scopus articles Infants impact factor journals Infants Scopus journals Infants PubMed journals Infants medical journals Infants free journals Infants best journals Infants top journals Infants free medical journals Infants famous journals Infants Google Scholar indexed journals Gastrointestinal disorders articles Gastrointestinal disorders Research articles Gastrointestinal disorders review articles Gastrointestinal disorders PubMed articles Gastrointestinal disorders PubMed Central articles Gastrointestinal disorders 2023 articles Gastrointestinal disorders 2024 articles Gastrointestinal disorders Scopus articles Gastrointestinal disorders impact factor journals Gastrointestinal disorders Scopus journals Gastrointestinal disorders PubMed journals Gastrointestinal disorders medical journals Gastrointestinal disorders free journals Gastrointestinal disorders best journals Gastrointestinal disorders top journals Gastrointestinal disorders free medical journals Gastrointestinal disorders famous journals Gastrointestinal disorders Google Scholar indexed journals Central nervous system articles Central nervous system Research articles Central nervous system review articles Central nervous system PubMed articles Central nervous system PubMed Central articles Central nervous system 2023 articles Central nervous system 2024 articles Central nervous system Scopus articles Central nervous system impact factor journals Central nervous system Scopus journals Central nervous system PubMed journals Central nervous system medical journals Central nervous system free journals Central nervous system best journals Central nervous system top journals Central nervous system free medical journals Central nervous system famous journals Central nervous system Google Scholar indexed journals Visceral hypersensitivity articles Visceral hypersensitivity Research articles Visceral hypersensitivity review articles Visceral hypersensitivity PubMed articles Visceral hypersensitivity PubMed Central articles Visceral hypersensitivity 2023 articles Visceral hypersensitivity 2024 articles Visceral hypersensitivity Scopus articles Visceral hypersensitivity impact factor journals Visceral hypersensitivity Scopus journals Visceral hypersensitivity PubMed journals Visceral hypersensitivity medical journals Visceral hypersensitivity free journals Visceral hypersensitivity best journals Visceral hypersensitivity top journals Visceral hypersensitivity free medical journals Visceral hypersensitivity famous journals Visceral hypersensitivity Google Scholar indexed journals Postnatal life articles Postnatal life Research articles Postnatal life review articles Postnatal life PubMed articles Postnatal life PubMed Central articles Postnatal life 2023 articles Postnatal life 2024 articles Postnatal life Scopus articles Postnatal life impact factor journals Postnatal life Scopus journals Postnatal life PubMed journals Postnatal life medical journals Postnatal life free journals Postnatal life best journals Postnatal life top journals Postnatal life free medical journals Postnatal life famous journals Postnatal life Google Scholar indexed journals Sex hormones articles Sex hormones Research articles Sex hormones review articles Sex hormones PubMed articles Sex hormones PubMed Central articles Sex hormones 2023 articles Sex hormones 2024 articles Sex hormones Scopus articles Sex hormones impact factor journals Sex hormones Scopus journals Sex hormones PubMed journals Sex hormones medical journals Sex hormones free journals Sex hormones best journals Sex hormones top journals Sex hormones free medical journals Sex hormones famous journals Sex hormones Google Scholar indexed journals Neurotransmitters articles Neurotransmitters Research articles Neurotransmitters review articles Neurotransmitters PubMed articles Neurotransmitters PubMed Central articles Neurotransmitters 2023 articles Neurotransmitters 2024 articles Neurotransmitters Scopus articles Neurotransmitters impact factor journals Neurotransmitters Scopus journals Neurotransmitters PubMed journals Neurotransmitters medical journals Neurotransmitters free journals Neurotransmitters best journals Neurotransmitters top journals Neurotransmitters free medical journals Neurotransmitters famous journals Neurotransmitters Google Scholar indexed journals Anxiety and Depression articles Anxiety and Depression Research articles Anxiety and Depression review articles Anxiety and Depression PubMed articles Anxiety and Depression PubMed Central articles Anxiety and Depression 2023 articles Anxiety and Depression 2024 articles Anxiety and Depression Scopus articles Anxiety and Depression impact factor journals Anxiety and Depression Scopus journals Anxiety and Depression PubMed journals Anxiety and Depression medical journals Anxiety and Depression free journals Anxiety and Depression best journals Anxiety and Depression top journals Anxiety and Depression free medical journals Anxiety and Depression famous journals Anxiety and Depression Google Scholar indexed journals Irritable bowel syndrome articles Irritable bowel syndrome Research articles Irritable bowel syndrome review articles Irritable bowel syndrome PubMed articles Irritable bowel syndrome PubMed Central articles Irritable bowel syndrome 2023 articles Irritable bowel syndrome 2024 articles Irritable bowel syndrome Scopus articles Irritable bowel syndrome impact factor journals Irritable bowel syndrome Scopus journals Irritable bowel syndrome PubMed journals Irritable bowel syndrome medical journals Irritable bowel syndrome free journals Irritable bowel syndrome best journals Irritable bowel syndrome top journals Irritable bowel syndrome free medical journals Irritable bowel syndrome famous journals Irritable bowel syndrome Google Scholar indexed journals Abdominal migraine articles Abdominal migraine Research articles Abdominal migraine review articles Abdominal migraine PubMed articles Abdominal migraine PubMed Central articles Abdominal migraine 2023 articles Abdominal migraine 2024 articles Abdominal migraine Scopus articles Abdominal migraine impact factor journals Abdominal migraine Scopus journals Abdominal migraine PubMed journals Abdominal migraine medical journals Abdominal migraine free journals Abdominal migraine best journals Abdominal migraine top journals Abdominal migraine free medical journals Abdominal migraine famous journals Abdominal migraine Google Scholar indexed journals Paediatricians articles Paediatricians Research articles Paediatricians review articles Paediatricians PubMed articles Paediatricians PubMed Central articles Paediatricians 2023 articles Paediatricians 2024 articles Paediatricians Scopus articles Paediatricians impact factor journals Paediatricians Scopus journals Paediatricians PubMed journals Paediatricians medical journals Paediatricians free journals Paediatricians best journals Paediatricians top journals Paediatricians free medical journals Paediatricians famous journals Paediatricians Google Scholar indexed journals Peptic ulcer disease articles Peptic ulcer disease Research articles Peptic ulcer disease review articles Peptic ulcer disease PubMed articles Peptic ulcer disease PubMed Central articles Peptic ulcer disease 2023 articles Peptic ulcer disease 2024 articles Peptic ulcer disease Scopus articles Peptic ulcer disease impact factor journals Peptic ulcer disease Scopus journals Peptic ulcer disease PubMed journals Peptic ulcer disease medical journals Peptic ulcer disease free journals Peptic ulcer disease best journals Peptic ulcer disease top journals Peptic ulcer disease free medical journals Peptic ulcer disease famous journals Peptic ulcer disease Google Scholar indexed journals Functional dyspepsia articles Functional dyspepsia Research articles Functional dyspepsia review articles Functional dyspepsia PubMed articles Functional dyspepsia PubMed Central articles Functional dyspepsia 2023 articles Functional dyspepsia 2024 articles Functional dyspepsia Scopus articles Functional dyspepsia impact factor journals Functional dyspepsia Scopus journals Functional dyspepsia PubMed journals Functional dyspepsia medical journals Functional dyspepsia free journals Functional dyspepsia best journals Functional dyspepsia top journals Functional dyspepsia free medical journals Functional dyspepsia famous journals Functional dyspepsia Google Scholar indexed journals
Article Details
1. Introduction
Functional abdominal pain (FAP) is common, affecting up to a quarter of all children and infants worldwide [1]. FAP is part of a broader spectrum of gastrointestinal disorders, Functional Gastrointestinal Disorders (FGIDs); defined by morphological and physiological aberrations whose underlying aetiology is an alteration of the interaction between gut mucosa, microbiome, immune function and or central nervous system processing bringing dysmotility and or visceral hypersensitivity [2]. The pathophysiology of Functional Gastrointestinal Disorders (FGIDs) is best comprehended through a biopsychosocial model, which also plays a crucial role in shaping their management. These conditions, often called "disorders of gut-brain interaction," are believed to stem from a complex interplay of genetic factors and precipitating psychosocial or medical events, typically occurring early in postnatal life [3]. The initial disturbances do not present symptoms immediately; instead, a second "hit" is theorized to be necessary. This second hit could involve factors such as the influence of sex hormones, alterations in the hypothalamic-adrenal-pituitary axis, or even changes in brain structure and function [3]. These factors disrupt the microbiota-gut-brain axis, resulting in several critical consequences:
Visceral Hypersensitivity: This refers to increased gut sensitivity, where even minor stimuli can trigger sensations like pain and distension.
Reduced Sensory Threshold: A lowered threshold for sensory inputs, makes the gut more responsive to various stimuli, including pain and distension.
Central Hypervigilance: The central nervous system becomes hypersensitive, amplifying neural signalling. This heightened sensitivity contributes to the perception of pain, often triggered by neurotransmitters produced by the microbes residing in the gut [3,4].
Increased severity of symptoms along with prolonged disease course is seen with concomitant psychological problems, including anxiety and depression, whose origins may be linked to the immune response generated in the brain secondary to the circulating pro-inflammatory cytokines [5,6].
The diagnosis of FAP hinges on assessing symptoms against the ROME IV criteria. These criteria help categorize FAP into subtypes, including irritable bowel syndrome (IBS), functional dyspepsia (FD), abdominal migraine, and Functional Abdominal Pain-Not Otherwise Specified (FAP-NOS), based on specific clinical characteristics. However, it is important to note that the universal adoption of these criteria is not widespread, which can hinder the accurate diagnosis of these disorders [6]. Furthermore, the low referral rate to specialists leads to incorrect or redundant ordering of tests, often guided by parental anxieties, and ineffective therapies lacking evidence backing [7]. The lack of an integrated approach to managing these disorders, often is accompanied informed by a lack of set guidelines and recommendations, leading to subpar treatment. Clinicians often fail to recognize the role of psychological factors in predisposing and perpetuating the condition. The results in omitting the role of psychological approach in the management of FAP, ultimately contributing to its chronicity [8].
It is important to highlight that there is currently no well-defined guideline for the diagnosis and management of FAP in children in India. Paediatricians frequently encounter difficulties when dealing with this condition, underscoring the pressing need for a standardized guideline. This consensus statement has been developed in response to this imperative need, aiming to provide clarity and guidance for healthcare professionals navigating the challenges of diagnosing and managing FAP in children in India. The purpose of this consensus statement is threefold:
- To establish clear guidelines for the diagnosis, investigative procedures, multidisciplinary approaches, management, and follow-up of patients with Functional Abdominal Pain (FAP).
- To facilitate the dissemination of knowledge about FAP among medical practitioners and healthcare professionals thus improving awareness and understanding improving awareness and understanding of FAP.
- To promote and support ongoing research endeavours focused on advancing our understanding of FAP.
2. Methods
The consensus study was conducted through literature review of publicly available sources and the consultation of specialists in various fields. Furthermore, the opinion and contribution of advisors, themselves experts in their fields, was sought. An advisory board meeting was convened and attended virtually by eight experts in the field across India. During this meeting, each of the eight members was assigned specific questions related to FAP. They were asked to respond with evidence-based arguments, referencing both previous research and their own clinical experience. Their responses to the supplementary questions were then summarized with the reason and judgements provided by the experts. The summary was circulated back to the experts in view of revising the previous responses. The final responses were then collated to construct a consensus statement following guidelines for the diagnosis and management of FAP.
3. The Consensus Statements
Five items were identified as priority for inclusion in the consensus statement (1) Diagnosis of Functional Gastrointestinal Disorders. (2) Clinical evaluation of suspected Functional Gastrointestinal Disorders. (3) Role of cross-speciality in the management of Functional Gastrointestinal Disorders. (4) Management of Functional Gastrointestinal Disorders (5) Measurement of efficacy of therapies.
3.1 Diagnosis of Functional abdominal Pain
The diagnosis of functional abdominal pain is anchored on the patient history, which should capture the characteristics of the pain, more so site, onset, character, severity, exacerbating and relieving factors, and its association with meals [3]. Of note, the nature of pain is necessary to elicit in the history, as night pain that wakes the patient is unlikely to be functional, pointing more to peptic ulcer disease [7]. The classic presentation of a child with Functional Abdominal pain is constant periumbilical pain [3]. The red flag signs as elaborated in Table 1 likely point to a more sinister pathology, and ought to be elicited in the history. The history of presenting illness should probe for a possible trigger event, which may be biological, such as infection, or psychosocial, such as the beginning a school year [3]. This also necessitates a complete psychological history, and an extensive family-social history, as children with Functional Gastrointestinal Disorders, including Functional abdominal Pain – Not otherwise specified, may present with co-morbid Anxiety or mood disorders [3,5,6]. A physical examination should include distraction, as pain that is alleviated by the aforementioned is more consistent with Functional Abdominal Pain [3]. The integration of the findings from the history and physical examination should be examined against the Rome IV criteria, to arrive at a suitable diagnosis [6] Table 1. It should be noted that the coexistence of syndromes does not exist, there may be an overlap of symptoms; Functional Abdominal Pain may coexist with irritable bowel syndrome, with the association of pain with feeding and bowel habits being the main distinguishing factor, the latter showing a strong correlation [6]. Adoption of the Rome IV criteria enables clear distinction between the syndromes improving the diagnostic process [8]. This was validated by a factor analysis study conducted globally across geographical regions in 26 countries, by sex, and by age groups. 49 ordinal variables were analysed through exploratory factor analysis (EFA) to identify interrelated factors. Revealing that all pre-specified factors with close correspondence to a Rome IV criteria diagnosis had loading of ≥0.4 solidifying the criteria’s validity [9]. As presented in Table 1, certain signs should be regarded as red flags that are contrary with the presentation of Functional Gastrointestinal Disorders.
|
Consensus statements |
|
|
1.1 |
Pain is the most prominent presenting symptom in Functional Abdominal Pain- Not otherwise specified and needs to be elicited in the history [6]. |
|
1.2 |
Abdominal fullness, bloating, constipation, irregular bowel with intermittent diarrhoea and periodic pain with a family history of migraines ought to be elicited in the history, as they are typically absent in FAP-NOS [2,6]. |
|
1.3 |
Diagnosis of Functional Gastrointestinal Disorders is to be anchored on the Rome IV diagnostic criteria based on the predominant signs and symptoms: The Rome IV diagnostic criteria for the diagnosis of Functional Gastrointestinal Disorders [6]: 1.3.1. Irritable Bowel Syndrome [6] The criteria must be fulfilled for at least 2 months and include all of the following. · Abdominal pain at least 4 days per month associated with defaecation and/or a change in the frequency of stool and/or a change in the appearance of stool · Abdominal pain does not resolve with resolution of the constipation (children in whom the pain resolves have functional constipation, not irritable bowel syndrome) · After appropriate evaluation, the symptoms cannot be fully explained by another medical condition. 1.3.2. Functional dyspepsia [6] The criteria must be fulfilled for at least 2 months before diagnosis and must include one or more of the following bothersome symptoms at least 4 days per month. · Postprandial fullness · Early satiation · Epigastric pain or burning not associated with defaecation · After appropriate evaluation, the symptoms cannot be fully explained by another medical condition 1.3.3. Abdominal migraine[6] The criteria must be fulfilled for at least 6 months before diagnosis and include all of the following occurring at least twice. · Paroxysmal episodes of intense, acute periumbilical, midline or diffuse abdominal pain lasting 1 hour or more (should be the most severe and distressing symptom) · Episodes are separated by weeks to months; the pain is incapacitating and interferes with normal activities; stereotypical pattern and symptoms in the individual patient · The pain is associated with two or more of the following: anorexia, nausea, vomiting, headache, photophobia or pallor · After appropriate evaluation, the symptoms cannot be fully explained by another medical condition 1.3.3. Functional abdominal pain not otherwise specified[6] The criterial must be fulfilled for at least 2 months before diagnosis and at least four times per month and include all of the following. · Episodic or continuous abdominal pain that does not occur solely during physiological events (for example, eating and menses) · Insufficient criteria for irritable bowel syndrome, functional dyspepsia or abdominal migraine · After appropriate evaluation, the abdominal pain cannot be fully explained by another medical condition |
|
1.4 |
Functional Abdominal pain is unlikely to be associated with night time pain that wakes the child, or pain that only occurs at night; Peptic ulcer Disease or inflammatory bowel disease should be ruled out [7]. |
|
1.5 |
Persistent localisation of pain is a red flag, and its characterisation is necessary to rule out the presence of an acute abdomen or other organic causes. This also includes localised abdominal tenderness [7]. 1.5.1 Pain not located in the periumbilical area [3,7]. 1.5.2 Persistent epigastric or lower chest pain may be suggestive of common bile duct obstruction, or gastritis. 1.5.3 Pain in both the loins may be suggestive of ureteric calculi. 1.5.4 Persistent pain and tenderness in the right iliac fossa might suggest appendicular infection |
|
1.6 |
Bilious Vomiting is a red flag, usually indicative of bowel obstruction or malrotation, warrants immediate investigation [7]. |
|
1.7 |
Hematemesis and blood in the stool are red flags, and should be investigated for possible bleeding disorder, infection, or ulceration in gastrointestinal tract [7]. |
|
1.8 |
Unintentional weight loss or poor growth is a red flag likely pointing to malabsorption or chronic inflammation of the gastrointestinal tract [7]. |
|
1.9 |
Fever is a red flag, typically pointing to infection or inflammation within the Gastrointestinal Tract [7]. |
Table 1: Summarises the consensus statements for the diagnosis of Functional abdominal pain and the related disorders.
3.2 Clinical evaluation of suspected Functional abdominal Pain
The following tests are recommended for children presenting with chronic pain to include (or exclude) a diagnosis of functional abdominal pain. These are listed in the order of importance.
- Complete blood count/peripheral smear, C-Reactive Protein levels (CRP), Erythrocyte Sedimentation Rate (ESR), liver function test. Elevated Erythrocyte Sedimentation Rate is a red flag, likely pointing to inflammatory bowel disease [7].
- Coeliac screening, thyroid function test, fasting blood sugar/random blood sugar.
- The serological testing of coeliac disease by measurement of serum tissue transglutaminase and the total IgA levels derives evidence from a study done in Italy revealing a 4% prevalence of coeliac disease in children with Irritable Bowel disease, and another showing a fourfold increase in the risk of Functional Abdominal Disorders in children with coeliac disease [10,11]. The utility of this is more so to children with Inflammatory Bowel disease with diarrhoea.
- Serum lipase/amylase, calcium, and creatinine – These rule out pancreatic disease; acute pancreatitis is an emergency requiring immediate care.
- Urine routine to rule out urinary tract infection.
- Stool routine: parasites, occult blood – Faecal occult blood is a red flag and likely points to inflammatory bowel disease or infection in the gastrointestinal tract [7,12].
- Fasting ultrasound of the abdomen, that reveals any pathological condition within the abdomen
- Faecal calprotectin – Elevated levels of faecal calprotectin help rule out Functional Gastrointestinal disorders (More so Irritable Bowel disease) in favour of inflammatory bowel diseases [7,13]. Further investigations such as Endoscopy, CT or MRI should be ordered, based on the symptomatology. Figure 1: Explains the algorithm to diagnose functional abdominal pain in children.
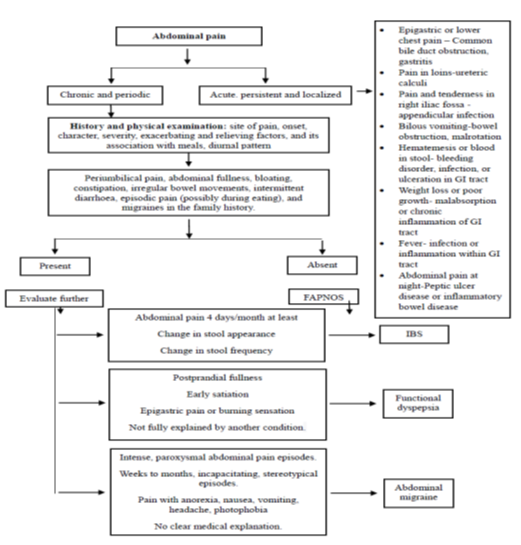
Figure 1: The algorithm to diagnose functional abdominal pain in children.
Of note is that laboratory testing should be targeted to avoid the escalation of costs and dwelling on minor findings whose significance is little at best. This is supported by the evidence of no changes in prognosis between children with Functional Abdominal Pain who underwent endoscopic evaluation and those who were not endoscopically tested [14]. The routine requesting of such investigations is therefore not recommended unless there is a strong indication for the same. In children presenting classically, without alarming signs, the evidence points to faecal calprotectin and the serological testing for coeliac disease as the most cost-effective laboratory tests [3]. The fact that negative test results (Which are expected, as organic disease is absent) may exacerbate parental anxiety should be recognised by the clinicians and addressed adequately with counselling [15]. With correct diagnosis, guided by appropriate investigations, the chances of early resolution increases [16].
3.3 Role of cross-speciality in Functional abdominal Pain in children
A multidisciplinary approach is recommended for the management of Functional Abdominal pain in children. The alarmingly low referral rate of referral amongst clinicians’ guides cripples effective diagnosis, management and follow-up, and guides these recommendations. The major downturn of the involvement of specialists in the management of Functional Abdominal Pain and related disorders is the escalation of the cost of management, which may expand up to fivefold [17]. Future policies are needed to enable the affordability of multidisciplinary care in Functional Gastrointestinal disorders. The following are to be involved in the management of Functional Abdominal Pain in Children:
Paediatric Gastroenterologist: Their primary role is to exclude alternative diagnoses, especially organic sources of abdominal pain, while also recommending medications or dietary modifications to alleviate symptoms and ensuring ongoing care and surveillance. –Their involvement may however lead to invasive procedures such as endoscopy or colonoscopy, increased cost of management, or unnecessary testing, and side effects from multiple prescribed medication [17].
Psychologist: They will provide important services focused on improving coping skills, reducing stress and anxiety, enhancing quality of life, and decreasing pain perception and disability, and facilitating psychosocial interventions such as Cognitive behavior therapy and hypnotherapy. Their involvement may lead to stigma, increased cost of treatment, or lack of adherence to treatment, which may stem from poor accessibility or increased costs [18]. With this, there is potential for virtual psychological interventions, which have been shown to be just as effective [18,19].
Pain specialist: The benefits of seeing a pain specialist may include reducing pain intensity and frequency, improving function and sleep. Research into the role of electrical stimulation methods such as percutaneous electrical nerve field stimulation (PENFS) in pain management shows significant reduction in pain and disability in children with Functional Abdominal Pain, with results sustained over time [20]. The risks of involving a pain specialist may include side effects of medications, invasive procedures such as nerve blocks or electrical stimulation [20].
3.4 Management of Functional Abdominal Pain and other Functional Gastrointestinal disorders in children
Based on the evidence reviewed, management of children with Functional Gastrointestinal Disorders, including Functional Abdominal Pain is to take a biopsychosocial approach. An important biologic intervention is the administration of probiotics, which have been shown to reduce the intensity of pain and increase the number of pain free days [21]. This is particularly for L. reuteri and lactobacillus probiotics [22,11]. The role of psychological treatments in the management of functional gastrointestinal disorders has been studied extensively revealing efficacy in relieving somatic symptoms [23-26].
Prokinetics such as domperidone find an important niche in the management of Functional Dyspepsia of all types, with a systematic review and meta-analysis revealing a statistically significant effect of treatment with prokinetics treatment and the reduction of all the symptoms of Functional Dyspepsia [27]. Of note is that the quality of evidence was very low, and the higher quality randomised control trials are needed to solidify this association [27]. Constipation, a feature of irritable bowel disease and an identified subtype may be amenable to laxatives, and is endorsed in the Rome 1V guidelines [28]. The conflicting results on the use of dietary fibre is a point of concern; studies in adults with irritable bowel syndrome show increased risk of pain and bloating, others show no benefit of addition of dietary fibre in the reduction of pain [29,30]. The prescription of the same should therefore be on a case-by-case basis, based on the indication. The psychological component of these disorders should guide clinicians as to whether antidepressants are required. The efficacy of amitriptyline in the management of functional abdominal pain is shown in an open-label trial where children diagnosed as Functional Abdominal Pain disorders were randomized to amitriptyline or placebo for 12 weeks, revealing reduction of in pain in 76% of those in the treatment group compared to 14.9% in the placebo group (P < 0.001) [31]. The potential side effects of amitriptyline, including anticholinergic effects, should be weighed against their benefits in functional gastrointestinal disorders, and weighed on a case-by-case basis.
The overgrowth of bacteria in the small intestines, particularly in irritable bowel disease, has been linked to some of the symptoms observed, including diarrhoea, bloating, abdominal pain and constipation [32]. Their presence is detected by a positive breath test, based on the principle that these bacteria ferment ingested carbohydrates (glucose or lactose) and produce gases in quantities different from those produced by human metabolism [33]. This suggests a role for inclusion of antibiotics in the treatment regime; patients with a positive breath test must be advised Rifamixin (antibiotic), that remains poorly absorbed in the gut and show improvement of symptoms over time [32-34].
The malabsorption of fermentable carbohydrates in functional gastrointestinal disorders is thought to cause an osmotic diarrhoea, as well as provide substrates for fermentation by colonic bacteria, resulting in the production of gas and bloating [35,36]. This is demonstrated by a study where administration of fructose for a fructose breath test caused nausea, bloating and abdominal pain, with elevated breath hydrogen levels above baseline [35]. The restriction of the same was associated with significant improvement in symptoms overtime, more so abdominal pain and bloating (p < 0.05) [35]. It is therefore recommended that children with functional gastrointestinal disorders maintain a low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) diet [35,36].
A study done by Levy et al. [37] demonstrated that children undergoing cognitive behaviour therapy (CBT) showed greater decreases in pain and gastrointestinal symptom severity (as reported by parents) than children in the comparison group (time × treatment interaction, p < 0.01), cementing our recommendation that CBT is incorporated in the management of functional gastrointestinal disorders [37]. These improvements are shown to be durable as well [38]. The aims of CBT include learning better coping and problem-solving skills, identification of triggers and reduction of maladaptive reactions to them. This is achieved by techniques such as keeping a diary of symptoms, feelings, thoughts and behaviours, adopting relaxation and distraction strategies, using positive and negative reinforcement for behaviour modification, confronting assumptions or beliefs that may be unhelpful and gradually facing activities that may have been avoided.
Other psychosocial interventions include hypnotherapy, which has been shown to significantly reduce the frequency of pain and the intensity of the same, and achieve high rates of remission. Vlieger et al. [39] showed that 85% of those in the treatment group (received hypnotherapy) in a randomised control study with 53 paediatric patients had achieved clinical remission at the end of 1 year, compared with 25% in the comparator group who received standard medical therapy (p < 0.001) [39]. These outcomes are comparable to self-hypnosis techniques, as demonstrated by Anbar et al. [40]. Guided imagery has also yielded commendable outcomes; guided imagery techniques with progressive muscle relaxation have demonstrated significant reduction in pain frequency [41]. These are therefore, when possible and available, to be incorporated in the management of functional gastrointestinal disorders. The inclusion of the family in the psychologic treatment by way of parental counselling and family therapy is integral as it lowers anxiety within the family and reduces the number of unnecessary investigations ordered [42]. It therefore requires that strong physician-parent and patient relationships are cultivated, all for the benefit of the child.
The utility of alterative and complementary medicine such as acupuncture in the management of functional gastrointestinal disorders is unsupported by current evidence: trials in adult did not find evidence supporting the superiority of acupuncture when compared to sham acupuncture (the comparator group) in the treatment of IBS [43,44]. There omission from this statement is therefore to eliminate the inclusion of unsupported modalities of therapy, which may inflate the cost of management. The consensus statement on management of FAP is summarised in Error! Reference source not found.. Figure 2 explains the algorithm to manage functional abdominal pain.
|
Consensus statements |
|
|
Biological Interventions |
|
|
2.1 |
Limosilactobacillus reuteri DSM 17938, a probiotic, is recommended and approved for use in Functional Gastrointestinal disorders, including FAP and IBS [21]. |
|
2.2 |
The duration of treatment with Limosilactobacillus reuteri DSM 17938 should be for a minimum of 6 weeks and up to 8 weeks [21]. |
|
2.3 |
Probiotics containing lactobacillus are approved for the management of Functional Gastrointestinal disorders [22]. |
|
2.4 |
Prokinetics should be considered in children with Functional Dyspepsia [27]. |
|
2.5 |
Laxatives are to be prescribed as a part of initial therapy for children with Irritable bowel syndrome – Constipation (IBS-C) [28] |
|
2.6 |
Use of bulking agents or dietary fibre in the management of Functional Gastrointestinal Disorders should be approached with caution. Empiric trial is recommended with close monitoring of symptom progression, which will guide further prescription [29]. |
|
2.7 |
Amitriptyline is to be prescribed for children with Anxitey [31]. |
|
2.8 |
For a positive Hydrogen Breath test, Rifamixin is advised [32-34]. |
|
2.9 |
Dietary modification, more so a low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) diet is recommended for the management of Functional Gastrointestinal Disorders [35]. |
|
Psychosocial interventions |
|
|
2.1 |
Cognitive Behaviour therapy recommended as a psychological intervention for the management of Functional Gastrointestinal disorders in children, alone or in combination with other biological and psychological interventions[37,38]. |
|
2.11 |
Hypnotherapy is approved for the management of Functional Gastrointestinal Disorders in children, alone or in combination with other psychological approaches [39,40]. |
|
2.12 |
Guided imagery is approved in the treatment of Functional Gastrointestinal Disorders [41]. |
|
2.13 |
Family therapy and parental counselling is recommended as a way of reducing parental anxiety [42]. |
|
2.14 |
Not much evidence or studies are conducted which supports acupuncture and other complementary and alternative therapies as management of FAP and related disorders [43,44] |
|
2.15 |
A strong patient physician relationship is linked to better outcomes in Functional Gastrointestinal Disorders and ought to be cultivated. |
Table 2: Summarizes statements for management of Functional abdominal pain.
3.5 Outcome measurements in the evaluation of the effect of therapy
The efficacy of the therapy should be assessed using a few efficient markers. The markers used to assess the efficacy of the treatments are summarised in Table 3.
|
Markers of effective therapy(ies) [45] |
|
|
3.1 |
Improved school attendance |
|
3.2 |
Reduced pain intensity as described by the patient or the parents |
|
3.3 |
Reduced frequency of pain. |
|
3.4 |
Improved quality of life, as reported by the child, the parents, teachers, or psychologist. |
|
3.5 |
Reduced anxiety and depression reported by the child, the parents, teachers, or psychologist. |
|
3.6 |
Improvement in defecation pattern. |
Table 3: summarises the measures of evaluating efficacy of therapy in children with Functional Gastrointestinal Disorders.
The potential subjectivity of these measures is a potential area of study, the goal of which would be to produce a universally accepted standardised measure of therapy efficacy, even in clinical trials. In the past, various measures have been used to gauge the efficacy of medication in trials, often relying on the pain (As this is the most crucial symptom); these are often individualised to the study, and little has been done to generate a reference to be used by all clinicians. [46,47].
4. Conclusion
In conclusion, this consensus statement strives to enhance the management of FAP by providing a comprehensive definition, guiding investigations, and outlining the involvement of specialists across different cross disciplines. Our strategy, based on the Rome IV criteria and the biopsychosocial model, emphasizes early multidisciplinary collaboration and accurate diagnosis. We advocate the use of Prokinetics, laxatives, probiotics, and antidepressants, complemented by psychological interventions like Cognitive Behaviour Therapy and parental counselling. We discourage practices like acupuncture due to limited evidence of efficacy. Furthermore, we recommend the provision of a patient information leaflet with all the information regarding disease cause, general course and the signs to observe in children in whom there is suspicion of alarming disease as is done in the United Kingdom to manage these diseases better. Furthermore, we propose the development of a standardized guideline for measuring improvement, benefiting both researchers and clinicians. While our recommendations provide a solid foundation, ongoing research efforts are essential to refine our approach and advance the management of these complex disorders, ultimately reducing the burden of morbidity associated with FAP.
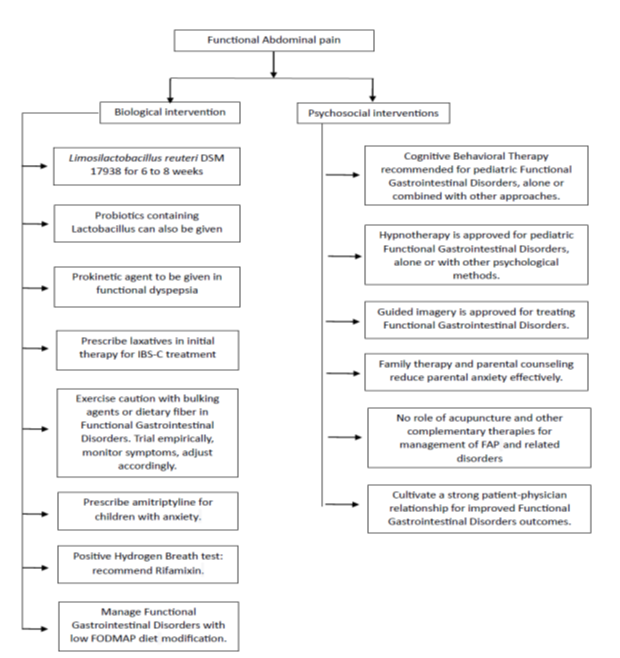
Figure 2: The algorithm to manage functional abdominal pain.
Acknowledgement
The authors would like to acknowledge support of Medclin Research. Funding for this study was provided by Dr. Reddy's Laboratories Ltd.
Conflict of interest
N, KCV, RR, and BK are employees of Dr. Reddy's Laboratories Ltd. AU is an employee of Medclin Research. The other authors declare no conflict of interest.
References
- Robin SG, Keller C, Zwiener R, et al. Prevalence of pediatric functional gastrointestinal disorders utilizing the Rome IV criteria. The Journal of Pediatrics 195 (2018): 134-139.
- Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology 19 2016: S0016-5085(16)00223-7.
- Thapar N, Benninga MA, Crowell MD, et al. Paediatric functional abdominal pain disorders. Nat Rev Dis Primers 89 (2020).
- Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain 152 (2011): S2-15.
- Dinan TG, Cryan JF. The microbiome-gut-brain axis in health and disease. Gastroenterology Clinics. 46 (2017): 77-89.
- Hyams JS, Di Lorenzo C, Saps M, et al. Functional Disorders: Children and Adolescents. Gastroenterology (2016): 00181-5.
- Motamed F, Mohsenipour R, Seifirad S, et al. Red flags of organic recurrent abdominal pain in children: study on 100 subjects. Iran J Pediatr 22 (2012): 457-462.
- Zeevenhooven J, Koppen IJ, Benninga MA. The New Rome IV Criteria for Functional Gastrointestinal Disorders in Infants and Toddlers. Pediatr Gastroenterol Hepatol Nutr 20 (2017): 1-13.
- Hreinsson JP, Törnblom H, Tack J, et al. Factor Analysis of the Rome IV Criteria for Major Disorders of Gut-Brain Interaction (DGBI) Globally and Across Geographical, Sex, and Age Groups. Gastroenterology 164 (2023): 1211-1222.
- Turco R, Boccia G, Miele E, et al. The association of coeliac disease in childhood with functional gastrointestinal disorders: a prospective study in patients fulfilling Rome III criteria. Alimentary Pharmacology and Therapeutics 34 (2011): 783-789.
- Saps M, Sansotta N, Bingham S, et al. Abdominal pain-associated functional gastrointestinal disorder prevalence in children and adolescents with celiac disease on gluten-free diet: a multinational study. The Journal of pediatrics 182 (2017): 150-154.
- Wakid MH. Fecal occult blood test and gastrointestinal parasitic infection. J Parasitol Res 2010 (2010): 434801.
- Pathirana WGW, Chubb SP, Gillett MJ, et al. Faecal Calprotectin. Clin Biochem Rev 39 (2018): 77-90.
- Bonilla S, Wang D, Saps M. The prognostic value of obtaining a negative endoscopy in children with functional gastrointestinal disorders. Clinical pediatrics 50 (2011): 396-401.
- Trivic I, Hojsak I. Initial diagnosis of functional gastrointestinal disorders in children increases a chance for resolution of symptoms. Pediatric Gastroenterology, Hepatology and Nutrition 21 (2018): 264-270.
- van Tilburg MA, Venepalli N, Ulshen M, et al. Parents' worries about recurrent abdominal pain in children. Gastroenterology Nursing 29 (2006): 50-55,
- Lane MM, Weidler EM, Czyzewski DI, et al. Pain symptoms and stooling patterns do not drive diagnostic costs for children with functional abdominal pain and irritable bowel syndrome in primary or tertiary care. Pediatrics 123 (2009): 758-764.
- Bonnert M, Olén O, Lalouni M, et al. Internet-delivered cognitive behavior therapy for adolescents with irritable bowel syndrome: a randomized controlled trial. Official journal of the American College of Gastroenterology ACG 112 (2017): 152-162.
- Sampaio F, Bonnert M, Olén O, et al. Cost-effectiveness of internet-delivered cognitive–behavioural therapy for adolescents with irritable bowel syndrome. BMJ Open 9 (2019): e023881.
- Kovacic K, Hainsworth K, Sood M, et al. Neurostimulation for abdominal pain-related functional gastrointestinal disorders in adolescents: a randomised, double-blind, sham-controlled trial. The lancet Gastroenterology and hepatology 2 (2017): 727-737.
- Jadrešin O, Sila S, Trivic I, et al. Lactobacillus reuteri DSM 17938 is effective in the treatment of functional abdominal pain in children: Results of the double-blind randomized study. Clin Nutr 39 (2020): 3645-3651.
- Gawronska A, Dziechciarz P, Horvath A, et al. A randomized double-blind placebo-controlled trial of Lactobacillus GG for abdominal pain disorders in children. Aliment Pharmacol Ther 25 (2007): 177-184.
- Walker LS, Williams SE, Smith CA, et al. Parent attention versus distraction: impact on symptom complaints by children with and without chronic functional abdominal pain. Pain 122 (2006): 43-52.
- Newton E, Schosheim A, Patel S, et al. The role of psychological factors in pediatric functional abdominal pain disorders. Neurogastroenterology and Motility 31 (2019): e13538.
- Lackner JM, Mesmer C, Morley S, et al. Psychological treatments for irritable bowel syndrome: a systematic review and meta-analysis. J Consult Clin Psychol 72 (2004): 1100-1113.
- Huertas-Ceballos A, Logan S, Bennett C, et al. Psychosocial interventions for recurrent abdominal pain (RAP) and irritable bowel syndrome (IBS) in childhood. Cochrane Database Syst Rev 23 (2008): CD003014.
- Pittayanon R, Yuan Y, Bollegala NP, et al. Prokinetics for Functional Dyspepsia: A Systematic Review and Meta-Analysis of Randomized Control Trials. Am J Gastroenterol 114 (2019): 233-243.
- Rome Foundation. GI genius interactive clinical decision toolkit. Rome Foundation https://romeonline.org/product/rome-iv-interactive-clinical-decision-toolkit-logicnets (2020).
- Hebden JM, Blackshaw E, D’Amato M, et al. Abnormalities of GI transit in bloated irritable bowel syndrome: effect of bran on transit and symptoms. Am J Gastroenterol 97 (2002): 2315-2320.
- Christensen M. Recurrent abdominal pain and dietary fiber. Am J Dis Child 140 (1986): 738-739.
- Seetharaman J, Poddar U, Yachha SK, et al. Efficacy of amitriptyline in pediatric functional abdominal pain disorders: A randomized placebo-controlled trial. J Gastroenterol Hepatol 37 (2022): 685-691.
- Quigley E, Quera R. Small intestinal bacterial overgrowth: roles of antibiotics, prebiotics, and probiotics. Gastroenterology 130 ((2006)): S78-S90.
- Saadi M, McCallum RW. Rifaximin in irritable bowel syndrome: rationale, evidence and clinical use. Ther Adv Chronic Dis 4 (2013): 71-75.
- Pimentel M, Lezcano S. Irritable bowel syndrome: bacterial overgrowth—what’s known and what to do. Current treatment options in gastroenterology 10 (2007): 328-337.
- Gomara RE, Halata MS, Newman LJ, et al. Fructose intolerance in children presenting with abdominal pain. J Pediatr Gastroenterol Nutr 47 (2008): 303-308.
- Chumpitazi BP, McMeans AR, Vaughan A, et al. Fructans exacerbate symptoms in a subset of children with irritable bowel syndrome. Clinical Gastroenterology and Hepatology 16 (2018): 219-225.
- Levy RL, Langer SL, Walker LS, et al. Cognitive-behavioral therapy for children with functional abdominal pain and their parents decreases pain and other symptoms. Am J Gastroenterol 105 (2010): 946-956.
- Lackner JM, Jaccard J, Radziwon CD, et al. Durability and decay of treatment benefit of cognitive behavioral therapy for irritable bowel syndrome: 12-month follow-up. The American Journal of Gastroenterology 114 (2019): 330.
- Vlieger AM, Menko-Frankenhuis C, Wolfkamp SC, et al. Hypnotherapy for children with functional abdominal pain or irritable bowel syndrome: a randomized controlled trial. Gastroenterology 133 (2007): 1430-1436.
- Anbar RD. Self-hypnosis for the treatment of functional abdominal pain in childhood. Clin Pediatr (Phila) 40 (2001): 447-451.
- Weydert JA, Shapiro DE, Acra SA, et al. Evaluation of guided imagery as treatment for recurrent abdominal pain in children: a randomized controlled trial. BMC Pediatr 6 (2006): 29.
- Salvatore S, Abkari A, Cai W, et al. Review shows that parental reassurance and nutritional advice help to optimise the management of functional gastrointestinal disorders in infants. Acta Paediatr 107 (2018): 1512-1520.
- Lembo AJ, Conboy L, Kelley JM, et al. A treatment trial of acupuncture in IBS patients. Am J Gastroenterol 104 (2009): 1489-1497.
- Schneider A, Enck P, Streitberger K, et al. Acupuncture treatment in irritable bowel syndrome. Gut 55 (2006): 649-654.
- Camilleri M, Chang L. Challenges to the therapeutic pipeline for irritable bowel syndrome: end points and regulatory hurdles. Gastroenterology 135 (2008): 1877-1891.
- Fehnel S, Johnston J, Kurtz C, et al. Assessing global change and symptom severity in subjects with IBS: qualitative item testing. Am J Gastroenterol 101 (2006): S483.
- Gordon S, Ameen V, Bagby B, et al. Validation of IBS global improvement scale. Dig Dis Sci 48 (2003): 1317-1323.
