Complex Surgical Treatment in A Patient with Locally Extended Rinosinusal Cancer - Case Report
Article Information
Mihai Dumitru Tudosie1,2*, Gloria Simona Bertesteanu1,2, Bianca Petra Taher1,2, Simona Andreea Rujan1,2, Alexandru Gabriel Enea1,2, Elena Teodora Diaconu1,2, Serban Vifor Gabriel Bertesteanu1,2, Raluca Grigore1,2
1University of Medicine and Pharmacy “Carol Davila”, Bucharest, Romania
2“Coltea” Clinical Hospital - Department of ENT, Bucharest, Romania
*Corresponding Author: Mihai-Dumitru TUDOSIE, University of Medicine and Pharmacy “Carol Davila”, Bucharest, Romania
Received: 05 December 2023; Accepted: 18 December 2023; Published: 26 December 2023
Citation:
Mihai-Dumitru TUDOSIE, Serban Vifor Gabriel BERTESTEANU, Raluca Grigore. Complex Surgical Treatment in A Patient with Locally Extended Rinosinusal Cancer - Case Report. Archives of Clinical and Medical Case Reports. 7 (2023): 433-436.
View / Download Pdf Share at FacebookAbstract
Introduction: Sinonasal malignancies are one of the rarest pathologies encountered in the ENT clinical field, less than 5% of all head and neck cancers. Endoscopic approach for all types of surgical pathologies has become the preferred method however, the external or combined approach is still necessary in selected cases. Surgical approach of the mid-structure of the face should always be performed with a reconstructive plan in mind. As presented in a multitude of studies, head and neck cancer survivors, especially the ones that underwent surgery, have a difficult time adjusting to their new condition, rejoin society, return to work and overall have a lower quality of life.
Material and method: This case report was based on following a patient admitted in the ENT Clinic of “Coltea” Clinical Hospital, from diagnosis to treatment and follow-up. Patient consent was taken for all photographs and imaging used in this article.
Results: Patient presented in the clinic with a tumoral growth on the right part of the nose, complaining of nasal obstruction, facial deformity and a few episodes of anterior epistaxis that stopped spontaneously. A tumour resection was performed but the disease reappeared in 6 months, requiring re-intervention of a greater calibre, with a complex reconstruction of the maxillo-facial structures.
Conclusion:
1. Rinosinusal carcinoma is a rare condition, <5% of all head and neck cancers, with a wide variety of histopathological types and subtypes.
2. Due to rarity, rinosinusal carcinoma can be misdiagnosed and mistreated, resulting in progression of the disease that increases the risks and costs of treatment.
3. Endoscopic surgery has become the rule of thumb for rinosinusal pathology but the combined or external approach still holds an important role in selected cases.
4. Oncologic surgery requires knowledge in reconstructive techniques and usually a multidisciplinary approach is needed.
5. Facial surgery is a high-risk surgery, that can profoundly alter the quality of life in patients affected by such procedures.
Keywords
Cancer; Rinosinusal; Reconstruction; Surgery; Head and neck
Cancer articles; Rinosinusal articles; Reconstruction articles; Surgery articles; Head and neck articles
Rinosinusal articles Rinosinusal Research articles Rinosinusal review articles Rinosinusal PubMed articles Rinosinusal PubMed Central articles Rinosinusal 2023 articles Rinosinusal 2024 articles Rinosinusal Scopus articles Rinosinusal impact factor journals Rinosinusal Scopus journals Rinosinusal PubMed journals Rinosinusal medical journals Rinosinusal free journals Rinosinusal best journals Rinosinusal top journals Rinosinusal free medical journals Rinosinusal famous journals Rinosinusal Google Scholar indexed journals Surgery articles Surgery Research articles Surgery review articles Surgery PubMed articles Surgery PubMed Central articles Surgery 2023 articles Surgery 2024 articles Surgery Scopus articles Surgery impact factor journals Surgery Scopus journals Surgery PubMed journals Surgery medical journals Surgery free journals Surgery best journals Surgery top journals Surgery free medical journals Surgery famous journals Surgery Google Scholar indexed journals Cancer articles Cancer Research articles Cancer review articles Cancer PubMed articles Cancer PubMed Central articles Cancer 2023 articles Cancer 2024 articles Cancer Scopus articles Cancer impact factor journals Cancer Scopus journals Cancer PubMed journals Cancer medical journals Cancer free journals Cancer best journals Cancer top journals Cancer free medical journals Cancer famous journals Cancer Google Scholar indexed journals Aflibercept articles Aflibercept Research articles Aflibercept review articles Aflibercept PubMed articles Aflibercept PubMed Central articles Aflibercept 2023 articles Aflibercept 2024 articles Aflibercept Scopus articles Aflibercept impact factor journals Aflibercept Scopus journals Aflibercept PubMed journals Aflibercept medical journals Aflibercept free journals Aflibercept best journals Aflibercept top journals Aflibercept free medical journals Aflibercept famous journals Aflibercept Google Scholar indexed journals Ultrasound articles Ultrasound Research articles Ultrasound review articles Ultrasound PubMed articles Ultrasound PubMed Central articles Ultrasound 2023 articles Ultrasound 2024 articles Ultrasound Scopus articles Ultrasound impact factor journals Ultrasound Scopus journals Ultrasound PubMed journals Ultrasound medical journals Ultrasound free journals Ultrasound best journals Ultrasound top journals Ultrasound free medical journals Ultrasound famous journals Ultrasound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals subretinal hemorrhage articles subretinal hemorrhage Research articles subretinal hemorrhage review articles subretinal hemorrhage PubMed articles subretinal hemorrhage PubMed Central articles subretinal hemorrhage 2023 articles subretinal hemorrhage 2024 articles subretinal hemorrhage Scopus articles subretinal hemorrhage impact factor journals subretinal hemorrhage Scopus journals subretinal hemorrhage PubMed journals subretinal hemorrhage medical journals subretinal hemorrhage free journals subretinal hemorrhage best journals subretinal hemorrhage top journals subretinal hemorrhage free medical journals subretinal hemorrhage famous journals subretinal hemorrhage Google Scholar indexed journals subretinal injection articles subretinal injection Research articles subretinal injection review articles subretinal injection PubMed articles subretinal injection PubMed Central articles subretinal injection 2023 articles subretinal injection 2024 articles subretinal injection Scopus articles subretinal injection impact factor journals subretinal injection Scopus journals subretinal injection PubMed journals subretinal injection medical journals subretinal injection free journals subretinal injection best journals subretinal injection top journals subretinal injection free medical journals subretinal injection famous journals subretinal injection Google Scholar indexed journals Pediatric articles Pediatric Research articles Pediatric review articles Pediatric PubMed articles Pediatric PubMed Central articles Pediatric 2023 articles Pediatric 2024 articles Pediatric Scopus articles Pediatric impact factor journals Pediatric Scopus journals Pediatric PubMed journals Pediatric medical journals Pediatric free journals Pediatric best journals Pediatric top journals Pediatric free medical journals Pediatric famous journals Pediatric Google Scholar indexed journals
Article Details
1. Introduction
Sinonasal malignancies are one of the rarest pathologies encountered in the ENT clinical field, less than 5% of all head and neck cancers [1]. Endoscopic approach for all types of surgical pathologies has become the preferred method however, the external or combined approach is still necessary in selected cases. Such cases include the extension of the tumor in adjacent regions, such as the orbit, the bony structures, skull base and pterigo-maxillary fossa [2-5]. Surgical approach of the mid-structure of the face should be performed keeping in mind that it is an exposed region with many components that define the human being. Altering its aspect can have tremendous impact on a patient’s quality of life and therefore, before attempting any invasive manoeuvres, a reconstructive technique should be considered. In head and neck surgery, the pectoral flap is the workhorse in reconstructions but it is not the
only option to have in mind, especially in difficult cases [6]. As presented in a multitude of studies, head and neck cancer survivors, especially the ones that underwent surgery, have a difficult time adjusting to their new condition, rejoin society, return to work and overall have a lower quality of life [7, 8].
2. Material and Method
This case report was based on following a patient admitted in the ENT Clinic of “Coltea” Clinical Hospital, from diagnosis to treatment and follow-up. Patient consent was taken for all photographs and imaging used in this article.
3. Result
Patient N.B., 56 years old, presented in the clinic with a tumoral growth on the right part of the nose, complaining of nasal obstruction, facial deformity and a few episodes of anterior epistaxis that stopped spontaneously. The patient is admitted for evaluation and treatment. From patient history we learned that he was diagnosed with squamous cell carcinoma of the nasal mucosa for which he underwent radiotherapy (Total Dose=70Gy) and chemotherapy (Cisplatin+5-FU - 6 cycles), but the outcome was progression of the disease. Also, he underwent surgery for a tumor on the right auricular lobe for which he had no documentation. Upon clinical examination, we found a tumoral growth that involved the right side of the nose and completely obstructed the right nasal fossa, with involvement of the nasal septum (Figure 1 and 2).

Figure 1 Figure 2
Computed tomography (CT) showed invasion of the nasal septum, right nasal fossa and the medial wall of the right maxillary sinus. After preoperative preparation, we performed resection of the tumour, en bloc with the nose, anterior part of the septum and anterior part of the medial wall of the right maxillary sinus (Figure 3-7).
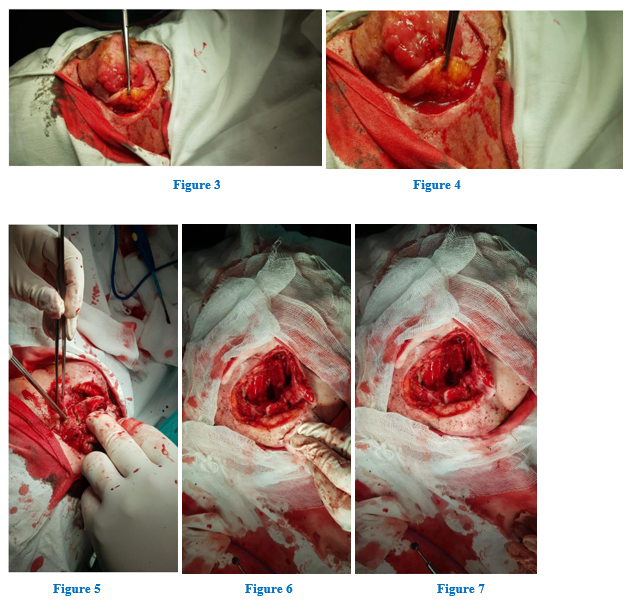
Figure 3 Figure 4
Figure 5 Figure 6 Figure 7
After the ablative process, primary reconstruction was needed. In order to cover the medio-facial defect, we used a regional flap from the forehead, as seen in Figure 8-9. Furthermore, to cover the remaining defect after flap prelevation, we used a free-skin graft (Figure 10) from the patient’s right forearm to cover the frontal area. Finally, a feeding tube was placed through the left nasal fossa.
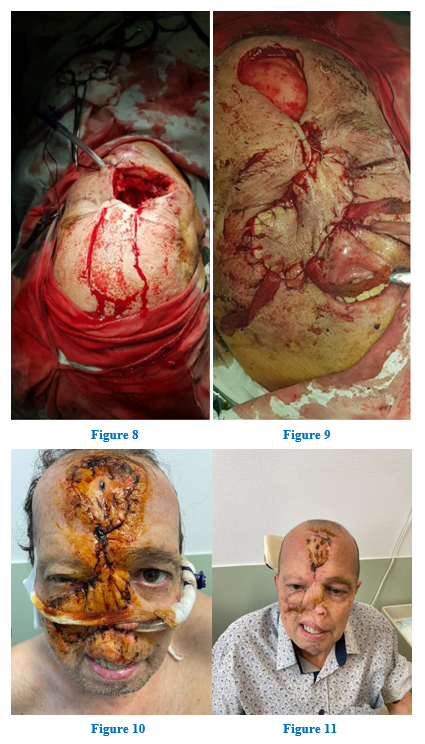
Figure 8 Figure 9
Figure 10 Figure 11
Postoperative care included daily wound dressing, antibiotic therapy and local vasodilators. After 14 days the sutures were removed and the patient was discharged. Follow-up schedule involved a visit every two months with the surgeon and the oncologist. After 2 months, the patient presented with a good postoperative aspect, no complications and the feeding tube was removed (Figure 11).

Figure 12 Figure 13 Figure 14
Unfortunately, after 6 months, the patient returned accusing a tumoral growth on the surgical site, associating right side diplopia, an important decrease in visual acuity of the right eye and minor bleeding from the area(fig 12-14). The patient underwent a CT-scan that showed a tumoral growth involving the flap, with implication of the remaining right maxillary sinus, the left orbit and the eyeball, the hard palate and the gingival mucosa of the upper right side dental arch. A second biopsy was prelevated and the result was low grade epidermoid-cell carcinoma. Patient was presented with the choices, either salvage surgery with important disfigurement, oncological treatment or palliative care. The patient opted for surgery. An ophthalmologic consult reported back that the right eye has no vision at all.
Surgery began with a delimitation of the affected area and a zone of healthy tissue, to ensure free margins. As seen from fig 15, the whole right maxillary bone was affected and it required removal of the hard palate, nasal septum in its entirety and left orbital exenteration.
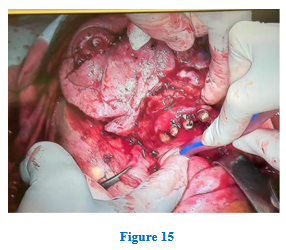
Figure 15
Removal of the tumour left an enormous defect that involved a massive reconstruction effort. Two major challenges emerged. One was the reconstruction of the hard palate and the other was the obliteration of the superior part of the defect. A complex technique was used, involving 2 different flaps. First, a regional flap from the right pectoralis major muscle was prelevated. Dividing the skin on the flap on its midline provided coverage for the hard palate and the inferior part of the face defect. Unfortunately, a pectoral flap cannot be pulled upwards beyond the zygomatic line. Therefore, a local temporal flap was used to cover the orbital part of the defect and the remaining area of the temporal region was covered with a split-skin graft prelevated from the right forearm (Figure 16-17). A tracheostomy tube was placed in order to protect the airway from any complications that may appear and to ensure fast airway control in case surgical re-entry was needed. The patient had favourable postoperative evolution and the regular follow-ups show the absence of the disease (Figure 18).

Figure 16 Figure 17 Figure 18
Next step in the patients treatment is discussing an alternative solution to the feeding tube, such as a gastrostomy, referral to a plastic surgeon for estetic re-intervention on the flaps and referral to an maxillofacial prosthodontist for an individualised prosthesis. Also, psychotherapy and counselling for him and the family was recommended.
Conclusion
- Rinosinusal carcinoma is a rare condition, <5% of all head and neck cancers, with a wide variety of histopathological types and subtypes.
- Due to rarity, rinosinusal carcinoma can be misdiagnosed and mistreated, resulting in progression of the disease that increases the risks and costs of treatment.
- Endoscopic surgery has become the rule of thumb for rinosinusal pathology but the combined or external approach still holds an important role in selected cases.
- Oncologic surgery requires knowledge in reconstructive techniques and usually a multidisciplinary approach is needed.
- Facial surgery is a high-risk surgery that can profoundly alter the quality of life in patients affected by such procedures.
References
- Thawani R, Kim MS, Arastu A, et al. The contemporary management of cancers of the sinonasal tract in adults. CA Cancer J Clin 73 (2023): 72-112.
- Konstantinidis I, Constantinidis J. Indications for open procedures in the endoscopic era. Curr Opin Otolaryngol Head Neck Surg 24 (2016): 50-56.
- Peter-John Wormald - Endoscopic Sinus Surgery; Anatomy, Three-Dimensional Reconstruction, and Surgical Tehnique, Fourth Edition ISBN 978-1-62623-469-7.
- Daniel Simmen, Nick Jones - Manual of Endoscopic Sinus Surgery and its extended Applications ISBN 3-13-130971-7.
- John S. Schneider, Andrew Day, Matthew Clavenna, Paul T. Russell, James Duncavage - Early Practice: External Sinus Surgery and Procedures and Complications, Otolaryngologic Clinics of North America 48 (2015): 839-850.
- Soler-Presas F, Cuesta-Gil M, Borja-Morant A, et al. Midface soft tissue reconstruction with the facio-cervico-pectoral flap. J Craniomaxillofac Surg 25 (1997): 39-45.
- Margalit DN, Salz T, Venchiarutti R, et al. Interventions for head and neck cancer survivors: Systematic review. Head Neck 44 (2022): 2579-2599.
- Yu J, Smith J, Marwah R, Edkins O. Return to work in patients with head and neck cancer: Systematic review and meta-analysis. Head Neck 44 (2022): 2904-2924.
