Comparison with 2019 of breast surgery activity and breast cancer prognostic factors in a French cancer center during the first 6 months of the COVID-19 pandemic
Article Information
Casto Elilindia Mlay*, Mubashir Alavi Jusabani, Tumaini Fedrick Minja, Elvin James Meshack, Rogers Joackim Temu
Department of Orthopaedics and Trauma, Kilimanjaro Christian Medical Centre, Moshi, United Republic of Tanzania
*Corresponding Author: Dr. Casto Elilindia Mlay, Department of Orthopaedics and Trauma, Kilimanjaro Christian Medical Centre, Moshi, United Republic of Tanzania
Received: 03 December 2020; Accepted: 09 December 2020; Published: 28 April 2021
Citation: Navid Mokarram Dorri, Monique Cohen, Sophie Knight, Laura Sabiani, Julien Barrou, Sandrine Rua, Camille Jauffret, Guillaume Blache, Eric Lambaudie, Marie Bannier, Gilles Houvenaeghel. Comparison with 2019 of breast surgery activity and breast cancer prognostic factors in a French cancer center during the first 6 months of the COVID-19 pandemic. Journal of Surgery and Research 4 (2021): 218-228.
View / Download Pdf Share at FacebookAbstract
Introduction
The rapid spread of the COVID-19 pandemic left departments of surgery, especially in oncology unprepared. The diagnostic and therapeutic management of breast cancer in Paoli Calmettes Institute cancer center underwent a major reorganization.
Methods
This study aimed to describe whether there was a change in the rate of surgical activity and type of tumors treated since the beginning of the outbreak (year 2020 was divided into 3 periods: before March the 17th = P1, between March the 17th and May the 11th = P2, from May the 11th to July 31st = P3) and compared to 2019.
Results
Over the three periods, a 12.71% decrease in the overall breast cancer surgery activity (n = 967 vs 1062) and a 18.05% decrease in new breast cancer surgery (n = 709 vs 581) was observed. The second period (P2) was the most critical one in both situations. During P2 a higher rate of large tumors, grade SBR 3 and negative endocrine receptor tumors were observed, there was also fewer Luminal A-like histological type diagnosed , during P3 fewer cT0 tumors and finally during both P2 and P3 there was a higher rate of neo-adjuvant chemotherapy.
Conclusion
This challenging period led to the diagnosis of higher stage and more aggressive histological types of breast cancers subsequently leading to more aggressive treatments.
Keywords
COVID-19, Breast, Surgery, Reconstruction, Cancer
COVID-19 articles; Breast articles; Surgery articles; Reconstruction articles; Cancer articles
COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals breast surgery activity articles breast surgery activity Research articles breast surgery activity review articles breast surgery activity PubMed articles breast surgery activity PubMed Central articles breast surgery activity 2023 articles breast surgery activity 2024 articles breast surgery activity Scopus articles breast surgery activity impact factor journals breast surgery activity Scopus journals breast surgery activity PubMed journals breast surgery activity medical journals breast surgery activity free journals breast surgery activity best journals breast surgery activity top journals breast surgery activity free medical journals breast surgery activity famous journals breast surgery activity Google Scholar indexed journals Surgery articles Surgery Research articles Surgery review articles Surgery PubMed articles Surgery PubMed Central articles Surgery 2023 articles Surgery 2024 articles Surgery Scopus articles Surgery impact factor journals Surgery Scopus journals Surgery PubMed journals Surgery medical journals Surgery free journals Surgery best journals Surgery top journals Surgery free medical journals Surgery famous journals Surgery Google Scholar indexed journals Reconstruction articles Reconstruction Research articles Reconstruction review articles Reconstruction PubMed articles Reconstruction PubMed Central articles Reconstruction 2023 articles Reconstruction 2024 articles Reconstruction Scopus articles Reconstruction impact factor journals Reconstruction Scopus journals Reconstruction PubMed journals Reconstruction medical journals Reconstruction free journals Reconstruction best journals Reconstruction top journals Reconstruction free medical journals Reconstruction famous journals Reconstruction Google Scholar indexed journals Cancer articles Cancer Research articles Cancer review articles Cancer PubMed articles Cancer PubMed Central articles Cancer 2023 articles Cancer 2024 articles Cancer Scopus articles Cancer impact factor journals Cancer Scopus journals Cancer PubMed journals Cancer medical journals Cancer free journals Cancer best journals Cancer top journals Cancer free medical journals Cancer famous journals Cancer Google Scholar indexed journals prognostic factors articles prognostic factors Research articles prognostic factors review articles prognostic factors PubMed articles prognostic factors PubMed Central articles prognostic factors 2023 articles prognostic factors 2024 articles prognostic factors Scopus articles prognostic factors impact factor journals prognostic factors Scopus journals prognostic factors PubMed journals prognostic factors medical journals prognostic factors free journals prognostic factors best journals prognostic factors top journals prognostic factors free medical journals prognostic factors famous journals prognostic factors Google Scholar indexed journals French cancer center articles French cancer center Research articles French cancer center review articles French cancer center PubMed articles French cancer center PubMed Central articles French cancer center 2023 articles French cancer center 2024 articles French cancer center Scopus articles French cancer center impact factor journals French cancer center Scopus journals French cancer center PubMed journals French cancer center medical journals French cancer center free journals French cancer center best journals French cancer center top journals French cancer center free medical journals French cancer center famous journals French cancer center Google Scholar indexed journals Orthopaedics and Trauma articles Orthopaedics and Trauma Research articles Orthopaedics and Trauma review articles Orthopaedics and Trauma PubMed articles Orthopaedics and Trauma PubMed Central articles Orthopaedics and Trauma 2023 articles Orthopaedics and Trauma 2024 articles Orthopaedics and Trauma Scopus articles Orthopaedics and Trauma impact factor journals Orthopaedics and Trauma Scopus journals Orthopaedics and Trauma PubMed journals Orthopaedics and Trauma medical journals Orthopaedics and Trauma free journals Orthopaedics and Trauma best journals Orthopaedics and Trauma top journals Orthopaedics and Trauma free medical journals Orthopaedics and Trauma famous journals Orthopaedics and Trauma Google Scholar indexed journals
Article Details
1. Introduction
As we write this article there has currently been over five hundred thousand people diagnosed with COVID-19 in France [1]. It will soon be a year since the COVID-19 pandemic began and we are now able to begin assessing the sanitary consequences of the pandemic and the lockdown on breast cancer treatment. The French Society of Surgical Oncology provided recommendations on how to prioritize surgical care delivery [2]. The aim was to avoid contamination by COVID-19 of patients at higher risk of complication and mortality by performing surgery [3]. Guidelines on re-organization of the management of breast cancer were also issued during this period: organized screening programs were suspended, the access to MRI was limited, patients with positive endocrine receptors (ER) invasive cancer and severe comorbidities were treated with neo-adjuvant endocrine therapy, in order to delay surgery [4]. Recent publications suggest that this strategy in postmenopausal patients with low risk tumors (ER positive, Her2 negative, Ki67 < 10/15%) was effective [5].
In a previous publication we reported over the same period a description of our surgical activity including breast cancer surgery, however breast cancer characteristics were not reported and activity was not analyzed in terms periods of interest during year 2020 [6]. This study focuses on evaluating to what extent patient care adaptations during this period could have impacted efficacy and quality of surgical management of breast cancer.
2. Methods
The department of surgical oncology 2 in Paoli Calmettes Institute, a French cancer center located in Marseille, is dedicated to breast, gynaecologic and urologic cancers. During COVID-19 pandemic, the hospital remained free of patients with COVID-19 infection and patients with a positive COVID-19 RT-PCR were referred to Infectious Hospital Unit of Marseille. The first wave of COVID-19 epidemic began in France in March and latest until May 2020. The first lockdown began on March the 17th and ended on May the 11th.
Since the 1st of April 2020, all patients that should undergo general anesthesia had to perform a COVID-19 RT-PCR two or three days prior to surgery and provide a negative result when admitted to hospital. They were also asked to fill in a questionnaire during the 7 days before surgery in order to confirm the absence of any clinical symptom of COVID-19 (fever, cough, anosmia, ageusia, headache).
Breast surgery activity from January 2020 to July 2020 was analyzed. Comparisons of breast surgery activity and ambulatory hospitalization were performed between each month of 2019 and 2020. The following breast cancers characteristics were analysed: clinical T-stage, clinical N-stage, age, menopausal status, axillary surgery, tumor SBR grade, endocrine receptors status, tumor subtypes (molecular-like subtypes), chemotherapy and type of breast surgery. Breast cancers characteristics were compared between 2019 and 2020, three periods were individualized: before March the 17th (P1), from March the 17th to May the 11th (P2), from May the 11th to the July 31st (P3) and after July the 31st.
Statistics: Rate comparisons were performed using Chi-2 or Fisher tests. A p-value <0.05 was considered statistically significant. Statistical analysis was performed using SPSS 16.0.
3. Results
Breast surgeries
Breast surgeries included mastectomies, lumpectomies for breast cancer or borderline breast lesions, axillary surgery and re-operations for non in-sano margins after first resection. Between January and July 2020, 927 breast surgeries were performed in comparison with 1062 breast surgeries during the same period in 2019, with a decrease of 12.71%. A large decrease was observed during April, May and June (48.3%, 41.9% and 26.3% respectively) (Figure 1). Ambulatory hospitalization rate decreased in 2020 in comparison with 2019 (58.90% versus 64.41%: p<0.02), mainly during March and April (Figure 2): 12.47% and 16.01% respectively.
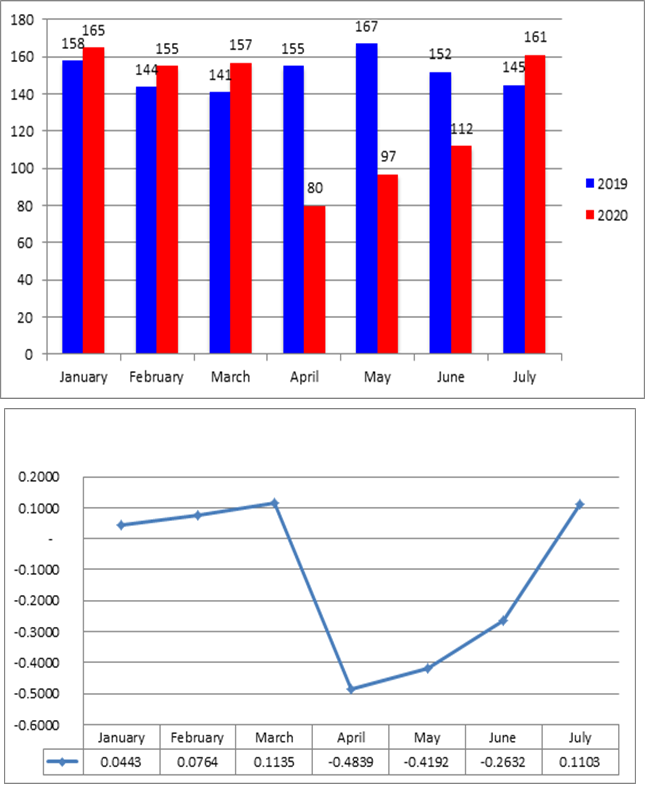
Figure 1: Breast surgery: number of patients and activity rates from January to July during year 2020 in comparison with year 2019.
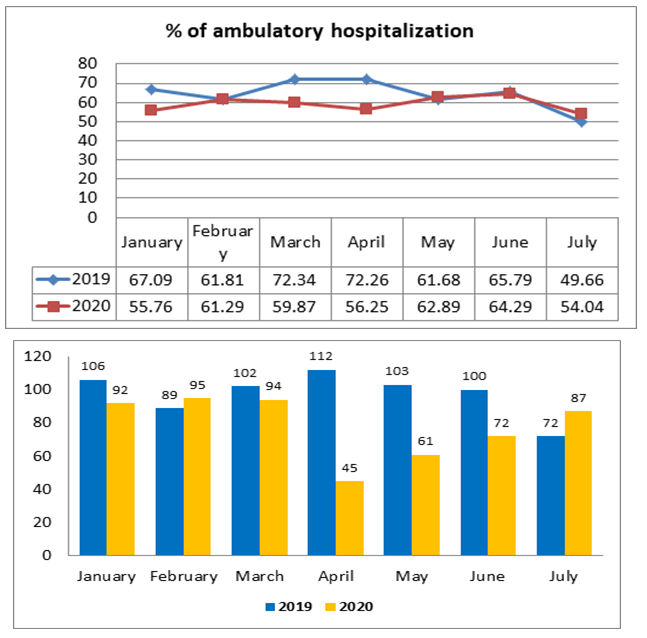
Figure 2: Ambulatory hospitalization: number of patients and ambulatory rates from January to July 2020 in comparison with year 2019.
The rate of immediate breast reconstruction after mastectomy was not significantly different between 2020 and 2019: 27.1% (48/177) in 2020 and 28.8% (66/229) in 2019 (Table 1).
|
2020 |
2019 |
||||
|
Nb |
% |
Nb |
% |
||
|
≤ March 17th |
without IBR |
41 |
32.8 |
56 |
32.5 |
|
IBR |
20 |
27 |
|||
|
>March 17 to May 11th |
without IBR |
19 |
5 |
41 |
26.8 |
|
IBR |
1 |
15 |
|||
|
> May 11th to July 31st |
without IBR |
69 |
28.1 |
66 |
26.7 |
|
IBR |
27 |
24 |
|||
|
Total |
without IBR |
129 |
27.1 |
163 |
28.82 |
|
IBR |
48 |
66 |
|||
Table 1: Comparison between 2019 and 2020 of immediate breast reconstruction (IBR) after mastectomy according the three periods: before, during and after the first lockdown.
Newly diagnosed breast cancers
Breast surgery for breast cancers decreased from 709 in 2019 to 581 in 2020 during the three periods between January and July (-18.05%). A major decrease was observed during the second period (-63.78%) (Figure 3). The number of surgeries per week according the three periods of 2019 and 2020 were calculated (11 weeks during P1, 8 weeks during P2, 11 weeks during P3 and 22 weeks after July 31 for year 2019). Number of breast surgeries per week decreased drastically during P2 (Figure 4): 8 in 2020 and 23 in 2019 (-65.2%).
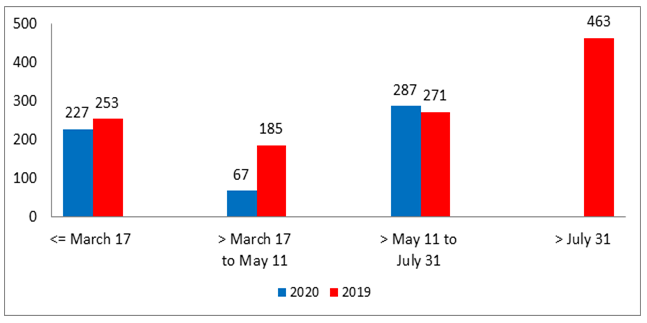
Figure 3: Number of patients operated for breast cancer according to periods and years 2019-2020.
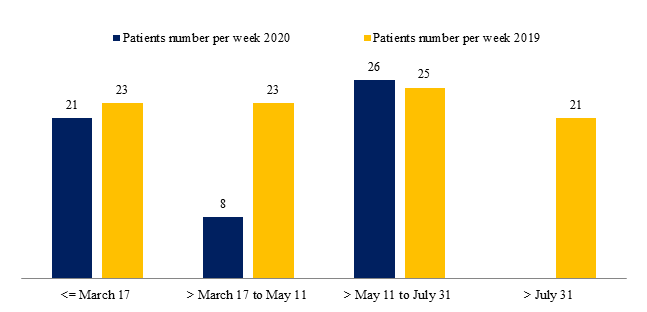
Figure 4: Number of patients per week operated for breast cancer according to periods and years 2019-2020.
Patient, tumors and treatment characteristics for all three periods are reported in Table 2.
Before March 17 (P1) a significant difference between 2020 and 2019 was observed for chemotherapy, with less adjuvant chemotherapy in 2020.
Table 2: Patients, tumors and treatments characteristics according to the three periods: before, during and after the first lockdown.
During the second period (P2), several differences were observed between 2020 and 2019: a higher rate of large tumors (cT2-4) in 2020 (38.5% versus 21.4% in 2019: p<0.01), higher rate of SBR grade 3 tumors in 2020 (33.9% versus 19.0%: Grade 3 versus Grades 1-2, p=0.03), higher rate of negative ER tumors in 2020 (19.7% versus 9.3%: p=0.040), fewer Luminal A-like tumors (ER+ Her2-, Grade SBR 1-2) (55.0% versus 74.1%: p=0.01 for Luminal A versus others subtypes), higher rate of neo-adjuvant chemotherapy in 2020 (19.4% versus 10.3%). A lower median age was observed during 2020 (57 in 2020 versus 62 in 2019), the difference was not significant.
During the third period (P3) of 2020, we reported a lower rate of cT0 tumors (31.8% versus 36.8%), of cN0 tumors (82.4% versus 87.2%, non-significant), a significantly higher rate of non-menopausal patients (35.4% versus 28.0%, p=0.037), a lower rate of sentinel lymph node biopsy (SLNB) alone (60.6% versus 68.6%, non-significant among patients with axillary surgery) and a higher rate of neo-adjuvant chemotherapy (24.7% versus 15.5%).
Comparison between P1 and P2 during year 2020 showed significant difference for SBR tumor grade (p=0.045) with a higher rate of grade 3 tumors during P2 (35% grade 3 for P2 versus 20.4% for P1: 21/60 versus 40/196). Comparisons between P2 and P3 during year 2020 showed significant difference (p=0.001) with a lower rate of adjuvant chemotherapy during P2 (2.9% for P2 versus 19.3% for P3: 2/68 versus 53/275). Higher rates of neo-adjuvant chemotherapy were observed for P2 and P3-2020 in comparison with P1-2020 (17.6% in P1: 40/227, 22.1% in P2: 15/68 and 24.7% in P3: 68/275).
Similar results were observed when comparing P2-2020 with all patients of year 2019: higher rate of grade 3 tumors during P2-2020 in comparison with year-2019 (33.9% grade 3 tumors in P2-2020 versus 21.6% in year-2019: 20/59 versus 223/1034; p<0.05), higher rate of absence of chemotherapy in P2-2020 in comparison with year-2019 (76.1% in P2-2020 versus 62.9% in year-2019: 51/68 versus 737/1172) and a lower rate of adjuvant chemotherapy in P2-2020 in comparison with year-2019 (2.9% for P2 versus 22.3% in year-2019: 2/68 versus 261/1172) (p=0.002).
4. Discussion
The overall breast cancer surgery activity decreased during the beginning of the 2020, particularly during the first lockdown (P2). Immediate breast reconstruction after mastectomy continued to be performed. During the second period, tumors were more frequently diagnosed at an advanced stage (cT2-4, grade SBR III) and with a poorer prognosis (fewer luminal A-like tumors, more neo-adjuvant chemotherapy). After the first lockdown (P3), fewer cT0 cancer were diagnosed and we observed a more frequent resort to neo-adjuvant chemotherapy compared to 2019.
Indeed more aggressive and larger size tumors were diagnosed during P2 as well as less infra-clinical tumors during P3, this could be attributed to the fact that screening program were suspended. This fact is also directly linked with the increase in neo-adjuvant chemotherapy during the third period. A statistical trend in favor of more luminal A-like tumors operated during P3 (without being significant) can be explained by the postponement of these less aggressive types of cancer.
Models were designed in order to estimate worldwide cancellation rate of elective surgery during the outbreak; for cancer surgery 37.7% operations would be cancelled [7]. Thus, this prediction is much more optimistic than what was experienced in our practice during P2 (-63.78%). In Lombardy, the prevalence of Covid-19 cases was similar to the prevalence in Marseille, the breast unit of IRCCS Maugeri had almost as many cases as we do in usual times [8]. However, they experienced a lower decrease during the peak of the outbreak, around -32% (63 in March-April 2020 versus 93 in March-April 2019).
The decrease in surgical activity during the lockdown in our cancer center is substantial, however it most likely is not as important as that of other institutions in the PACA region (southeast of France) that had to reduce activity in order to treat COVID-19 infected patients. In the opposite way, the increase of activity through P3 reaches past year score. Meanwhile the increase in activity observed during P3 did not exceed the increase in activity of 2019. An explanation could be the delayed diagnoses due to the suspension of screening program and postponement of consultations or biopsies. This phenomenon shall probably persist until the end of the pandemic and lead to more advanced clinical stages and a delay in histological diagnosis.
The main limitation of this study lies in its unicentric character: there is a lack of data regarding other hospitals in Marseille and its surroundings. In order to fully measure the consequences of the outbreak on the management of breast cancer it will be necessary to evaluate the number of patients and types of breast cancer treated throughout the COVID-19 pandemic.
5. Conclusion
During the first lockdown we observed an increase in breast cancer surgery for patients with poorer prognostic factors however surgeries for high-risk breast cancer did not appear to reduce after the first lockdown. The results of this study highlight he fact that there is an urgent need to restore routine gynaecological follow-up. Especially since the COVID-19 pandemic shall probably last for a significant length of time.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Author Contributions
All authors were responsible for data collection.
Authors responsible of data analysis, interpretation of the results, and writing the manuscript: Gilles Houvenaeghel, Navid Mokarram Dorri and Sophie Knight.
All authors have seen and approved either the primary submission or any revisions and the manuscript is not in press or submitted for consideration of publication elsewhere currently.
All authors approve final version of paper for submission.
Funding
No funding
Acknowledgments
None
Data Availability Statement
All data generated or analyzed during this study are included in this published article.
References
- The World Health Organization. Weekly Epidemiological Update Coronavirus disease 2019 (COVID-19) 28 September 2020.
- Jean-Marc Classe, Gilles Dolivet, Serge Evrard, Gwenael Ferron, Fabrice Lécuru, et al. French Society for Surgical Oncology (SFCO) guidelines for the management of surgical oncology in the pandemic context of COVID 19.
- Yong Liu, Jiaming Wang, Yi Tang, Rong Su, Qianwen Yang. Surgical Management Strategy for Breast Cancer Patients During the COVID-19 Outbreak.
- Daraï E, Mathelin C, Gligorov J. Breast Cancer Management during the COVID 19 Pandemic: French Guidelines. Eur J Breast Health (2020).
- Dowsett M, Ellis MJ, Dixon JM. Evidence-based guidelines for managing patients with primary ER+ HER2− breast cancer deferred from surgery due to the COVID-19 pandemic. npj Breast Cancer 6 (2020).
- Houvenaeghel G, Barrou J, Sabiani L, Blache G, Cohen M, et al. Surgical Oncologic Activity Before, During and after Pandemic COVID-19 Period in a French Cancer Center. J Surg Res. 3 (2020): 370-381.
- Aneel Bhangu. Elective surgery cancellations due to the COVID-19 pandemic : global predictive modelling to inform surgical recovery plans.
- Corsi F, Caruso A, Albasini S. Management of breast cancer in an EUSOMA-accredited Breast Unit in Lombardy, Italy, during the COVID-19 pandemic. Breast J. (2020): 1-2.
