Comparison of the Radiological and Functional Outcome of Proximal Femoral Nail with Helical Blade versus Lag Screw in Intertrochanteric Fractures
Article Information
Kamaldeep Singh, Raj Kumar Aggarwal, Aarti Dewan and Chandan Jasrotia*
Department of Orthopaedics, Sri Guru Ram Das Institute of Medical Sciences and Research, Sri Amritsar, India
*Corresponding Author: Chandan Jasrotia, Department of Orthopaedics, Sri Guru Ram Das Institute of Medical Sciences and Research, Sri Amritsar, India.
Received: 28 January 2023; Accepted: 07 February 2023; Published: 10 February 2023
Citation:
Kamaldeep Singh, Raj Kumar Aggarwal, Aarti Dewan, Chandan Jasrotia. Comparison of the Radiological and Functional Outcome of Proximal Femoral Nail with Helical Blade versus Lag Screw in Intertrochanteric Fractures. Journal of Orthopedics and Sports Medicine 5 (2023): 47-55.
View / Download Pdf Share at FacebookAbstract
Introduction: Intertrochanteric fractures are defined as extracapsular fractures of the proximal femur that occur between the greater and lesser trochanter. These fractures occur both in the elderly and the young, but they are more common in the elderly population with osteoporosis due to a low energy mechanism. The female to male ration is between 2:1 and 8:1. Operative management of these fractures is considered urgent, not emergent. This allows the many comorbidities with which patients often present to be optimized preoperatively, to reduce morbidity and mortality.
Aim and objectives: Aim of the study is to compare the radiological and functional outcome of proximal femoral nail with helical blade vs. proximal femoral nail with lag screw in intertrochanteric fractures.
Materials and methods: Patients fulfilling the inclusion criteria were included in the study and randomly allocated in two groups. Group patients with intertrochanteric fracture were operated with proximal femoral nail using lag screw and group B patients were operated with proximal femoral nail using helical blade.
Keywords
Intertrochanteric fractures; Femoral nail; Osteoporoti
Orthopaedics articles Orthopaedics Research articles Orthopaedics review articles Orthopaedics PubMed articles Orthopaedics PubMed Central articles Orthopaedics 2023 articles Orthopaedics 2024 articles Orthopaedics Scopus articles Orthopaedics impact factor journals Orthopaedics Scopus journals Orthopaedics PubMed journals Orthopaedics medical journals Orthopaedics free journals Orthopaedics best journals Orthopaedics top journals Orthopaedics free medical journals Orthopaedics famous journals Orthopaedics Google Scholar indexed journals Intertrochanteric fractures articles Intertrochanteric fractures Research articles Intertrochanteric fractures review articles Intertrochanteric fractures PubMed articles Intertrochanteric fractures PubMed Central articles Intertrochanteric fractures 2023 articles Intertrochanteric fractures 2024 articles Intertrochanteric fractures Scopus articles Intertrochanteric fractures impact factor journals Intertrochanteric fractures Scopus journals Intertrochanteric fractures PubMed journals Intertrochanteric fractures medical journals Intertrochanteric fractures free journals Intertrochanteric fractures best journals Intertrochanteric fractures top journals Intertrochanteric fractures free medical journals Intertrochanteric fractures famous journals Intertrochanteric fractures Google Scholar indexed journals Osteoporotic articles Osteoporotic Research articles Osteoporotic review articles Osteoporotic PubMed articles Osteoporotic PubMed Central articles Osteoporotic 2023 articles Osteoporotic 2024 articles Osteoporotic Scopus articles Osteoporotic impact factor journals Osteoporotic Scopus journals Osteoporotic PubMed journals Osteoporotic medical journals Osteoporotic free journals Osteoporotic best journals Osteoporotic top journals Osteoporotic free medical journals Osteoporotic famous journals Osteoporotic Google Scholar indexed journals Hip fracture articles Hip fracture Research articles Hip fracture review articles Hip fracture PubMed articles Hip fracture PubMed Central articles Hip fracture 2023 articles Hip fracture 2024 articles Hip fracture Scopus articles Hip fracture impact factor journals Hip fracture Scopus journals Hip fracture PubMed journals Hip fracture medical journals Hip fracture free journals Hip fracture best journals Hip fracture top journals Hip fracture free medical journals Hip fracture famous journals Hip fracture Google Scholar indexed journals Stable fractures articles Stable fractures Research articles Stable fractures review articles Stable fractures PubMed articles Stable fractures PubMed Central articles Stable fractures 2023 articles Stable fractures 2024 articles Stable fractures Scopus articles Stable fractures impact factor journals Stable fractures Scopus journals Stable fractures PubMed journals Stable fractures medical journals Stable fractures free journals Stable fractures best journals Stable fractures top journals Stable fractures free medical journals Stable fractures famous journals Stable fractures Google Scholar indexed journals Helical blade articles Helical blade Research articles Helical blade review articles Helical blade PubMed articles Helical blade PubMed Central articles Helical blade 2023 articles Helical blade 2024 articles Helical blade Scopus articles Helical blade impact factor journals Helical blade Scopus journals Helical blade PubMed journals Helical blade medical journals Helical blade free journals Helical blade best journals Helical blade top journals Helical blade free medical journals Helical blade famous journals Helical blade Google Scholar indexed journals Trochanteric fractures articles Trochanteric fractures Research articles Trochanteric fractures review articles Trochanteric fractures PubMed articles Trochanteric fractures PubMed Central articles Trochanteric fractures 2023 articles Trochanteric fractures 2024 articles Trochanteric fractures Scopus articles Trochanteric fractures impact factor journals Trochanteric fractures Scopus journals Trochanteric fractures PubMed journals Trochanteric fractures medical journals Trochanteric fractures free journals Trochanteric fractures best journals Trochanteric fractures top journals Trochanteric fractures free medical journals Trochanteric fractures famous journals Trochanteric fractures Google Scholar indexed journals Proximal femoral articles Proximal femoral Research articles Proximal femoral review articles Proximal femoral PubMed articles Proximal femoral PubMed Central articles Proximal femoral 2023 articles Proximal femoral 2024 articles Proximal femoral Scopus articles Proximal femoral impact factor journals Proximal femoral Scopus journals Proximal femoral PubMed journals Proximal femoral medical journals Proximal femoral free journals Proximal femoral best journals Proximal femoral top journals Proximal femoral free medical journals Proximal femoral famous journals Proximal femoral Google Scholar indexed journals Femur fractures articles Femur fractures Research articles Femur fractures review articles Femur fractures PubMed articles Femur fractures PubMed Central articles Femur fractures 2023 articles Femur fractures 2024 articles Femur fractures Scopus articles Femur fractures impact factor journals Femur fractures Scopus journals Femur fractures PubMed journals Femur fractures medical journals Femur fractures free journals Femur fractures best journals Femur fractures top journals Femur fractures free medical journals Femur fractures famous journals Femur fractures Google Scholar indexed journals Valgus alignment articles Valgus alignment Research articles Valgus alignment review articles Valgus alignment PubMed articles Valgus alignment PubMed Central articles Valgus alignment 2023 articles Valgus alignment 2024 articles Valgus alignment Scopus articles Valgus alignment impact factor journals Valgus alignment Scopus journals Valgus alignment PubMed journals Valgus alignment medical journals Valgus alignment free journals Valgus alignment best journals Valgus alignment top journals Valgus alignment free medical journals Valgus alignment famous journals Valgus alignment Google Scholar indexed journals Femoral neck shaft angle articles Femoral neck shaft angle Research articles Femoral neck shaft angle review articles Femoral neck shaft angle PubMed articles Femoral neck shaft angle PubMed Central articles Femoral neck shaft angle 2023 articles Femoral neck shaft angle 2024 articles Femoral neck shaft angle Scopus articles Femoral neck shaft angle impact factor journals Femoral neck shaft angle Scopus journals Femoral neck shaft angle PubMed journals Femoral neck shaft angle medical journals Femoral neck shaft angle free journals Femoral neck shaft angle best journals Femoral neck shaft angle top journals Femoral neck shaft angle free medical journals Femoral neck shaft angle famous journals Femoral neck shaft angle Google Scholar indexed journals Cephalo-medullary nails articles Cephalo-medullary nails Research articles Cephalo-medullary nails review articles Cephalo-medullary nails PubMed articles Cephalo-medullary nails PubMed Central articles Cephalo-medullary nails 2023 articles Cephalo-medullary nails 2024 articles Cephalo-medullary nails Scopus articles Cephalo-medullary nails impact factor journals Cephalo-medullary nails Scopus journals Cephalo-medullary nails PubMed journals Cephalo-medullary nails medical journals Cephalo-medullary nails free journals Cephalo-medullary nails best journals Cephalo-medullary nails top journals Cephalo-medullary nails free medical journals Cephalo-medullary nails famous journals Cephalo-medullary nails Google Scholar indexed journals Femur surgery articles Femur surgery Research articles Femur surgery review articles Femur surgery PubMed articles Femur surgery PubMed Central articles Femur surgery 2023 articles Femur surgery 2024 articles Femur surgery Scopus articles Femur surgery impact factor journals Femur surgery Scopus journals Femur surgery PubMed journals Femur surgery medical journals Femur surgery free journals Femur surgery best journals Femur surgery top journals Femur surgery free medical journals Femur surgery famous journals Femur surgery Google Scholar indexed journals Sliding hip screws articles Sliding hip screws Research articles Sliding hip screws review articles Sliding hip screws PubMed articles Sliding hip screws PubMed Central articles Sliding hip screws 2023 articles Sliding hip screws 2024 articles Sliding hip screws Scopus articles Sliding hip screws impact factor journals Sliding hip screws Scopus journals Sliding hip screws PubMed journals Sliding hip screws medical journals Sliding hip screws free journals Sliding hip screws best journals Sliding hip screws top journals Sliding hip screws free medical journals Sliding hip screws famous journals Sliding hip screws Google Scholar indexed journals Medial fracture segment articles Medial fracture segment Research articles Medial fracture segment review articles Medial fracture segment PubMed articles Medial fracture segment PubMed Central articles Medial fracture segment 2023 articles Medial fracture segment 2024 articles Medial fracture segment Scopus articles Medial fracture segment impact factor journals Medial fracture segment Scopus journals Medial fracture segment PubMed journals Medial fracture segment medical journals Medial fracture segment free journals Medial fracture segment best journals Medial fracture segment top journals Medial fracture segment free medical journals Medial fracture segment famous journals Medial fracture segment Google Scholar indexed journals
Article Details
1. Introduction
Intertrochanteric fractures are defined as extracapsular fractures of the proximal femur that occur between the greater and lesser trochanter and are extremely common fractures occurring in elderly osteoporotic individuals [1]. Recumbence following a hip fracture is known to be associated with increased mortality in this group of patients. The female to male ratio is between 2:1 and 8:1 [2].
These fractures are usually a result of a ground-level fall in the elderly population and are classified as either stable or unstable. Determination of stability is important as it helps determine the type of fixation required for stability. Stable fractures have an intact posteromedial cortex and will resist compressive loads once reduced. Examples of unstable fractures include: comminution of the posteromedial cortex, fractures extending up to lateral wall, displaced lesser trochanter fracture, subtrochanteric extension and reverse obliquity pattern [3].
Intertrochanteric fractures are extra capsular and have a much more robust osseous blood supply, and therefore are much less likely to result in chronic complications such as AVN or nonunion. Thus, the primary concerns of inadequate treatment of trochanteric fractures are related to the risks of acute instability and possible nonunion/malunion with post injury deformity. Nonoperative treatment is rarely indicated and should only be considered for non-ambulatory patients and patients with a high risk of perioperative mortality [4].
Although there are multiple studies comparing PFN with other intra-medullary devices like Gamma nail, PFNA, limited studies are available which compares treatment outcomes of proximal femoral nail with lag screw and proximal femoral nail with helical blade. In view of the extremely limited literature available, we conducted this study to compare the clinical, radiological and functional outcomes of PFN with lag screw and helical blade PFN in management of intertrochanteric fracture.
2. Aim and Objectives
Aim of the present study is to compare the radiological and functional outcome of proximal femoral nail with helical blade vs. proximal femoral nail with lag screw in intertrochanteric fractures. Objective of the study Radiological outcome were compared between two groups with respect to Femoral Neck shaft angle, Horizontal Femoral offset, Total femoral length, Tip apex distance and Union at 3 months. Functional outcome was compared between of the two groups using Harris Hip Scoring system (HHS).
3. Material and Methods
The Randomized comparative interventional study was conducted in department of orthopedics SGRDIMSAR Sri Amritsar from 1st April 2021 to 31st July 2022, in which patients fulfilling the inclusion criteria were be randomly divided in two groups.
Helical blade group: Patients with intertrochanteric fracture operated using proximal femoral nail with helical blade.
3.2 Lag screw group: Patients with intertrochanteric fracture operated using proximal femoral nail with lag screw.
3.3 Randomization: All Patients having age 30 years and above with fracture intertrochanteric femur (AO/OTA classification).were included in the study after obtaining informed written consent for both the treatments i.e. proximal femoral nail with helical blade and lag screw. To avoid the selection bias computer generated random numbers were obtained and sealed in an envelope. The slip was then taken out by office clerk not involved in the study and whether to put helical blade or lag screw was then decided according to the coded slip. The patients and the operating surgeon were blinded in the present study till the insertion of column screw. Patients were followed up at 3 months after discharge.
3.4 Exclusion criteria:
- Patients with previous ipsilateral hip or femur surgery.
- Patients with pathological fractures.
- Fractures extension into subtrochanteric region.
As per new AO/ OTA classification and fracture pattern, cases from both the groups were classified further into stable and unstable and various radiological and functional parameters were assessed accordingly.
3.5 Operative protocol:
All patients with trochanteric fractures which were operated by two surgeons of our unit were taken on radiolucent table with traction applied on injured limb. In all patient attempt of closed reduction was given on traction table and in fractures where closed reduction was not achieved then fractures were reduced with mini open or percutaneous methods. All cases were provisionally fixed with K wires out of the path of the nail and these k wires were maintained until the nail insertion.
After Palpating the greater trochanter, around 5 cm incision was given proximal to the tip of greater trochanter. Entry was made just medial to the tip of the greater trochanter and was confirmed on image intensifier in both AP and roll over lateral view, in lateral view the entry point was in line with the axis of the intramedullary canal of shaft and femoral neck.
Then guide wire was inserted, femur canal was opened with solid cannulated reamer of appropriate size. Medullary canal was not reamed during the surgery. In our study, after estimating the nail size and diameter preoperatively using image meter pro and confirming it on image intensifier intraoperative, guide wire for both cervical screws was inserted in dead center of femoral head and neck on roll over lateral view and slightly inferior or in center on AP view on image intensifier.
3.5.1 Proximal locking with helical blade: Select the appropriate length helical blade as measured. Align the back end of the helical blade with the impactor. Thread the connecting screw into the helical blade and finger-tighten the assembly. Hold the handle of the inserter and advance the blade as far as possible by hand. Use light hammer blows on the back of the connecting screw to seat the helical blade. Insert to the stop. The blade is fully inserted when the helical blade impactor comes to a stop at the back of the blade guide sleeve.
3.5.2 Proximal locking with lag screw: After selecting appropriate length lag screw, pass the screw insertion assembly over the guide wire, through the blade guide sleeve and through the nail. Advance the screw by turning the inserter clock- wise until the mark on the inserter meets the flange surface of the blade guide sleeve.
Both the type of column screws were locked in static mode using a set screw.
The result of this surgical procedure was analyzed on the basis of various radiological and functional parameters. Follow up was done at third month. At each visit clinical, various radiological parameters and along with this function outcome was assessed using Harris hip score [5].
4. Analysis of Data
The data from the present study was systematically collected, compiled and statistically analyzed to draw relevant conclusions using SPSS Statistics-26 version. The observations were tabulated in the form of mean Standard Deviation (SD) and Number with percentage. In parametric data, unpaired student t test was used. Quantitative variables were correlated using chi square test. The data was analyzed and level of significance was determined as its ‘p’ value with p<0.05 as significant and p<0.001 as highly significant.
5. Results
The comparative interventional randomized study comprising of 29 patients of trochanteric femur fractures treated either with Proximal femoral nail with helical blade (n = 17) and proximal femoral nail with lag screw (n = 12). Patients were admitted in Department of Orthopaedics at Sri Guru Ram Das Institute of medical Sciences and Research, Amritsar between April 2021 to July 2022. This study was performed under the approval of our institution’s ethical review board (Document number: Ant/85/2021). Informed consent was obtained from each participant. Out of 29 patients, 2 patients were lost to follow up. A single case of helical blade cut through was observed at 3rd week follow up due to unprotected weight bearing. The final outcome of 26 cases on the basis of radiological and functional parameters were assessed and is hereunder:
5.1 Baseline characteristics
Majority of patients belonged to age group of more than 65 years contributing 72 percent to the present study with minimum age of 25 years and maximum age of 89 years and the mean age of 68.76 ± 13.51 in helical group and mean age of 65.08 ± 14.40 in lag screw group. Out of 29 patients, 14 were male and 15 were female (Table 1).
|
Age Group |
Number |
Percentage |
|
<65 Years |
8 |
27.59 |
|
≥65 Years |
21 |
72.41 |
|
Gender |
||
|
Female |
15 |
51.72 |
|
Male |
14 |
48.28 |
|
Stability |
||
|
Stable |
17 |
58.62 |
|
Unstable |
12 |
41.38 |
Table 1: Demographic data related to the present study.
As per AO/OTA guidelines, out of 29 intertrochanteric fractures, 19 were of stable fracture pattern and 10 were of unstable fracture pattern. Further, it was observed that in helical blade group, 9 cases (53%) were of stable fracture pattern (AO31A1) and 8 cases (47%) were of unstable fracture pattern (AO31A2 and AO31A3). In lag screw group, 8 cases (67%) belonged to stable fracture pattern (AO31A1) and 4 cases (33%) belonged to unstable fracture pattern (AO31A2 and AO31A3). There was no statistically significant difference (P=0.174) in the proportion of fractures that were unstable or stable between the helical blade and lag screw group. The baseline characteristics demonstrated no statistically significant differences between the groups.
6. Radiological Analysis
6.1 Femoral Neck shaft angle:
6.1.1 Helical blade group: There was an overall average increase in femoral neck shaft angle at 3rd month from 129.13 ± 3.42 degrees (uninjured side) to 130.27 ± 3.84 degrees (operated side) (p = 0.059) irrespective of fracture pattern. We tried to achieve positive cortical reduction intra-operatively which led to valgus alignment of the neck shaft angle. On subgroup analysis on basis of fracture pattern: Among the unstable fracture pattern (n = 7), there was an average increase in neck shaft angle at 3rd month from 127.57 ± 2.64 degrees (uninjured side) to 128.71 ± 1.98 degrees (operated side) (p = 0.231). In stable fracture pattern (n = 8), there was an average increase in neck shaft angle at 3rd month from 130.5 ± 3.59 degrees (uninjured side) to 131.63 ± 4.66 degrees (operated side) (p = 0.185).
6.1.2 Lag screw group: There was an overall average increase in femoral neck shaft angle at 3rd month from (127.63 ± 3.80) degrees (uninjured side) to (128.36 ± 4.76) degrees (operated side) (p = 0.363) irrespective of fracture pattern. On subgroup analysis on the basis of fracture pattern: Among the unstable fracture pattern (n = 3) there was an average increase in neck shaft angle in at 3rd month from 127.57 ± 2.63 degrees (uninjured side) to 128.71 ± 1.96 degrees (operated side) (p = 0.321). On further analysis, amongst the stable fracture pattern (n = 8) fixed with lag screw, we observed an insignificant average decrease of neck shaft angle from (128.00 ± 3.891) degrees (uninjured side) to (127.78 ± 4.44) degrees (operated side) (p = 0.785) as one case was erroneously fixed in slight varus neck shaft angle intra-operatively which led to relative decrease in neck shaft angle degrees and affecting the outcome of this specific group but there was no further varus collapse i.e. the neck shaft angle was maintained at 3rd month follow up in this case. The patient achieved radiological union at 3 months and functional outcome was good. If we tend to exclude this case from our analysis, the results will be same as in other groups irrespective of fracture pattern or type of implant used. The average change in neck shaft angle of both the groups irrespective of fracture pattern was statistically insignificant (p = 0.270) (Figure 1).
6.2 Horizontal femoral offset (Neck length):
6.2.1 Helical blade group: There was an overall average decrease in horizontal femoral offset at 3rd month from 39.73 ± 4.35 mm (uninjured side) to 38.60 ± 4.56 mm (operated side) (p = 0.055) irrespective of fracture pattern. On subgroup analysis on basis of fracture pattern: Among the unstable fracture pattern (n =7), there was an average decrease in horizontal femoral offset at 3rd month from 42.14 ± 3.62 mm (uninjured side) to 41.43 ± 3.45 mm (operated side) (p = 0.441). Among the stable fracture pattern (n = 8) fixed with helical blade, there was an average decrease in horizontal femoral offset at 3rd month from 37.63 mm ± 3.96 mm (uninjured side) to 36.13 ± 4.05 mm (operated side) (p = 0.072).
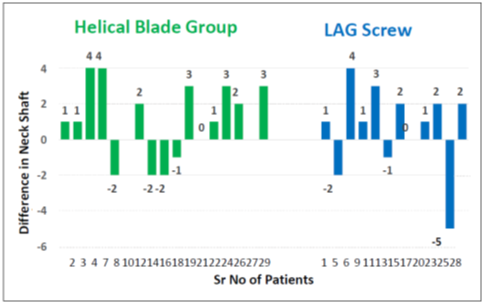
Figure 1: Difference of neck shaft angle at 3rd month with uninjured side in both groups.
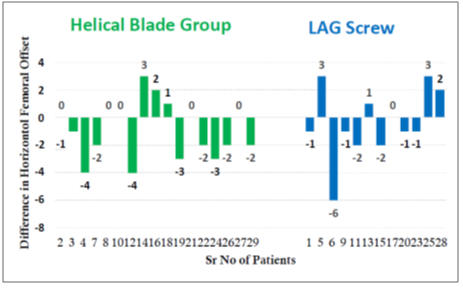
Figure 2: Difference of horizontal offset (mm) change at 3rd month with uninjured side in both groups.
6.2.2 Lag screw group: There was an overall average decrease in horizontal femoral offset at 3rd month from 42.09 ± 5.394 mm (uninjured side) to 41.63 ± 5.163 (operated side) (p = 0.578) irrespective of fracture pattern. On subgroup analysis, among the unstable fracture pattern (n = 3), there was an average decrease in horizontal femoral offset at 3rd month from 48.00 ± 5.292 mm (uninjured side) to 45.67 ± 6.65 mm (operated side) (p = 0.369). In stable fracture pattern (n = 8), there was an insignificant average increase in horizontal femoral offset at 3rd month from 39.875 ± 3.60 mm (uninjured side) to 40.12 ±3.98 mm (operated side) (p = 0.741). The variability in this group can be attributed to the case discussed above which led to an average increase in this subgroup. Both the outcomes in comparison were statistically insignificant (p = 0.126). Both the types of collum screws were statically locked with set screw to prevent any significant collapse irrespective of fracture pattern and type of implant used. (Figure 2).
6.3 Total femoral length:
6.3.1 Helical blade group: There was an overall average increase in total femoral length at 3rd month from 391.67 ± 40.039 mm (uninjured side) to 394.27 ± 40.704 mm (operated side) (p = 0.238) irrespective of fracture pattern. On sub group analysis, among the unstable fracture pattern, there was an average increase in total femoral length at 3rd month from 388.57 ± 37.79 mm to 392 ± 38.82 mm (p = 0.268) and an average increase in total femoral length at 3rd month from 394.38 ± 44.32 mm to 396.25 ± 44.86 mm (p = 0.583) in the stable fracture pattern.
6.3.2 Lag screw group: There was an overall average increase in total femoral length (Figure 3) at 3rd month from 391.364 ± 16.170 mm (uninjured side) to 392.091 ± 12.888 mm (operated side) (p = 0.744). On further analysis, among the unstable fracture pattern, there was an average increase in total femoral length at 3rd month from 391.67 ± 22.59 mm (uninjured side) to 393.67 ± 18.82 mm (operated side) (p = 0.713). In stable fracture pattern, there was average increase of total femoral length at 3rd month from 391.250 ±15.08 mm (uninjured side) to 391.500 ± 11.60 mm (operated side). Both the outcomes in comparison were statistically insignificant (p = 0.866).
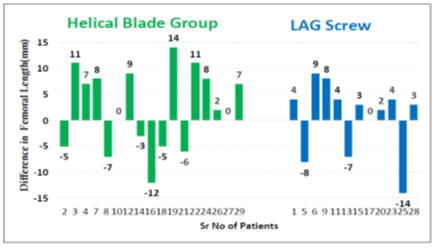
Figure 3: Difference of femoral length (mm) change at 3rd month with uninjured side in both groups.
6.4 Tip apex distance:
6.4.1 Helical blade group: The mean tip apex distance post operatively in this group was 21.67 ± 2.13.
6.4.2 Lag screw group: The mean tip apex distance post operatively in this group was 21.27 ± 1.74
6.4.3 Union: Radiological Union at 3 months was achieved in 24 cases in total. Two cases had delayed radiological union each belonging to either group (unstable fracture pattern in helical group and stable fracture pattern in lag screw group) (Figure 4).

Figure 4: comparison of patients as per the union of fracture in both the groups.
6.5 Functional Outcome:
Functional outcome at 3rd month which was assessed using Harris hip score showed statistically insignificant difference between the two comparison groups irrespective of fracture pattern and type of implant used (p = 0.967) (Figure 5).
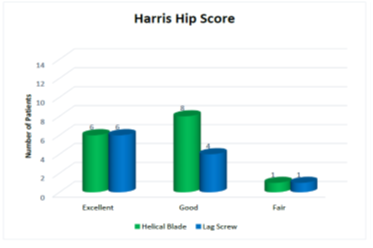
Figure 5: Harris hip score in both groups at three months.
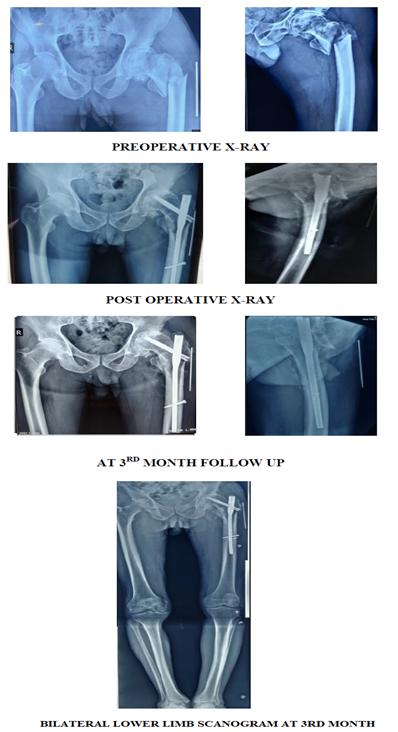
7. Case scenario 1:
A 75 year old male with unstable intertrochanteric fracture fixed with PFN with lag screw.
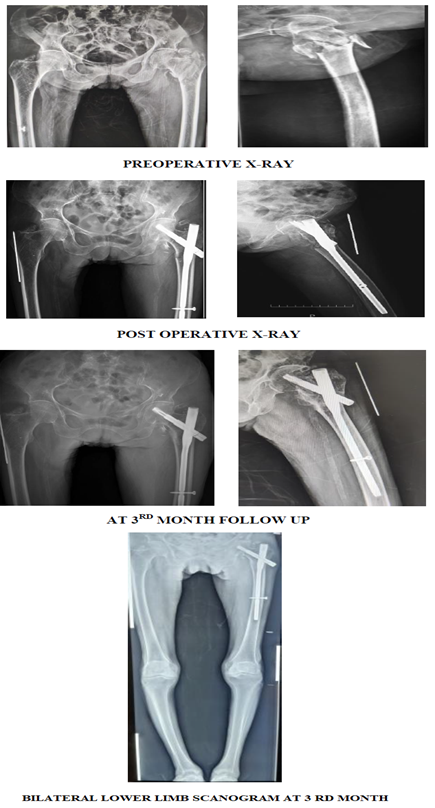
8. Case scenario 2:
9. Discussion
With the increase in elderly population, the incidence of intertrochanteric fractures has increased year by year. Patients suffering from intertrochanteric fractures have a high incidence of morbidity and mortality. An early surgical procedure is now considered as preferred option for the treatment of intertrochanteric fractures providing an opportunity for early and full weight bearing mobilization. Surgical delay is associated with a significant increase in the risk of death and pressure sores [6].
Surgical implants employed to fix intertrochanteric fractures are dichotomized into being either intramedullary (cephalo-medullary nails) or extra-medullary (sliding hip screws). There is an increasing trend towards the use of intramedullary devices for the fixation of intertrochanteric fractures due to superior biomechanics and minimally invasive surgery particularly in unstable fracture patterns which enables immediate rehabilitation of the patient after surgery [7]. These devices allow controlled collapse at the fracture site.
Currently two different types of collum implants are available for proximal fixation, a traditional lag screw and a helical blade. Several randomized controlled trials and studies comparing helical blade with the lag screw in intramedullary fixations have demonstrated greatly different outcomes compared with published data and theoretical concepts. The optimal choice between the helical blade and lag screw is still controversial.
We conducted this randomized comparative study of 29 patients with intertrochanteric fracture, majority of patients belonging to age group of more than 65 years, which were randomized in two groups i.e. helical blade group (n =17) and lag screw group (n =12). All the patients were followed up for a time period of 3 months. Out of these, two patients were lost to follow up.
The aim of our randomized study was to assess if there were any differences in various radiological parameters and functional outcomes of patients with intertrochanteric fracture fixed with proximal femoral nail with helical blade and a proximal femoral nail with lag screw.
To avoid further bias in study, both the helical blade and lag screw were statically locked proximally to prevent undue collapse at fracture site.
Among the radiological parameters, an overall average increase of neck shaft angle at 3rd month was achieved irrespective of the fracture pattern and type of implant used. This average increase of neck shaft angle at 3rd month was statistically insignificant in comparison of both the groups (p = 0.270). We tried to maintain positive cortical reduction intra-operatively which led to valgus alignment of the neck shaft angle except in one case as discussed below. The average increase in neck shaft angle led to an overall average increase in total femoral length at 3rd month irrespective of fracture pattern and type of implant used. This average increase of total femoral length at 3rd month was statistically insignificant in comparison of both the groups (p = 0.866).
There was an insignificant average decrease in horizontal femoral offset irrespective of fracture pattern and type of implant used. This average decrease in horizontal femoral offset at 3rd month was statistically insignificant in comparison as well (p = 0.126). On subgroup analysis, the variability i.e. an insignificant increase in horizontal femoral offset among stable fracture pattern group fixed with lag screw was observed due to a single case as discussed below.
We calculated the Tip apex distance on immediate post-operative x-ray. Average Tip apex distance (TAD) was within 10-25 mm in both the comparison groups. Radiological union at 3 months was achieved in 24 cases in total. 2 cases had delayed radiological union each belonging to either group. There was no statistical significant difference between the functional outcome of two comparison groups as measured by Harris Hip Score (HHS) at 3rd month follow up (p = 0.967)
One case was erroneously fixed in slight varus neck shaft angle intra-operatively (Figure 6), which led to insignificant relative decrease in neck shaft angle degrees and insignificant relative increase in horizontal femoral offset among the stable fracture pattern group fixed with lag screw. But there was no further varus collapse i.e the neck shaft angle was maintained at 3rd month follow up in this case. The patient achieved radiological union at 3 months and functional outcome was good. If we tend to exclude this case from our analysis, the results will be same as in other groups irrespective of fracture pattern or type of implant used.
We also observed a single case of cut-through which was fixed with helical blade PFN at 3rd week follow up. Reason for which can be attributed to unprotected weight bearing.
A comparative study done by Talia chapman et al. [8] in 2018 on 126 patients treated with Trochanteric Fixation Nail (TFN; Synthes) with either a helical blade (71 [56.3%]) or screw (55 [43.7%]) concluded in their study that 7 failures of fixation (5.6%) occurred, all of which used a helical blade. 5 failures resulted from medial migration of the helical blade through the femoral head, while 2 resulted from typical supero-lateral cutout and varus collapse. There was no difference in average Tip Apex Distance (TAD) between the cases using blade versus screw fixation or between failures and the remainder of the cohort. This study showed a higher failure rate with use of the blade and supports the use of screw fixation in such fractures.
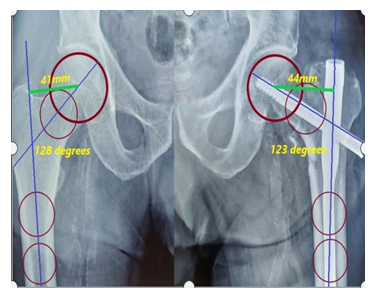
Figure 6: X-Ray radiograph of Pelvis (AP view) showing varus fixation of fracture.
A Systematic Review and Meta-Analysis conducted by Kim et al. [9] in 2021 compared fixation failure between helical blade-type and lag screw-type CMNs with cut-out and cut-through rates as primary outcomes and degree of sliding length, time to union, and non-union rate as secondary outcomes. They concluded in their study that fixation failure (OR = 1.88, 95% CI: 1.09-3.23, P = 0.02), especially cut-through (OR = 5.33; 95% CI, 2.09-13.56; P < 0.01), was more common with helical blades than with lag screws, although the cut-out rate was not significantly different between both the comparison groups (OR = 0.87, 95% CI: 0.38-1.96, P = 0.73). In our study, we have observed a single case of cut through of helical blade as discussed earlier.
Following are the results of a biomechanical study conducted by Sommers et al. [10] and Al-Munajjed et al. [11] comparing helical blade and lag screw showing improved resistance of helical blade fixation to varus collapse and rotational control of the medial fracture segment compared to screw fixation (i.e., lag screw). These studies concluded that the improved resistance of the helical blade to cut-out has been attributed to radial compaction of cancellous bone as the blade is inserted. Major drawback of this study is that it is an in vitro study, so these results are hard to extrapolate on real life patients.
A recent study conducted by B J Punt [12] in 2019, on 631 patients which were surgically treated for an intertrochanteric femur fracture. Of this group, 239 patients (37.9%) were treated with Trochanteric femoral nail with helical blade and 392 patients (62.1%) with a Trochanteric femoral nail with femoral neck screw. This study demonstrated no statistically significant differences in primary and secondary outcomes between the use of a TFN with helical blade and a TFN with femoral neck screw (lag screw) for the surgical treatment of intertrochanteric femur fractures. A major drawback of our study was less number of patients taken into account and limited time duration for follow up. Although they have not mentioned about the distribution of the patients, an advantage of our study is that it is a randomized comparative study so that any bias is prevented.
Although we were able to achieve satisfactory results in both the comparison groups, as per surgeon’s experience the operative technique for lag screw insertion was more technically complex as compared to helical blade insertion as the surgeon have to keep a check on rotation of femoral head segment while tightening the lag screw which may lead to loss of reduction intra-operatively. We have also used set screw to statically lock both helical blade and lag screw and have observed no case of non- union in any of our cases.
We acknowledge the limitations of the present study. Firstly our study group was small in number and we were unable to relate the age related osteoporosis with type of collum implant to be used as lack of availability of DEXA-CT scan at our institute.
10. Summary and Conclusion
So from current study comprising 26 patients of intertrochanteric fractures fixed with either Helical blade PFN or Lag screw PFN, we can conclude that Mean change in neck shaft angle and horizontal femoral offset at 3rd month was statistically insignificant irrespective of type of fracture pattern and type of implant used. Similarly mean change in total femoral length at 3rd month was statistically insignificant irrespective of type of fracture pattern and type of implant used. All the patients achieved radiological union. There was no case of non-union in any of the two comparison groups.
At the end we can conclude that good functional and radiological outcome in intertrochanteric fractures fixed with proximal femoral nail can be achieved with either of the collum implants as it depends upon the adequate reduction preferably positive in both the antero-posterior and lateral planes, proper placement of head neck implant with respect to Tip Apex Distance (TAD), statically locking both devices with set screw and quality of the bone and not on the type of implant used.
References
- Karakus O, Ozdemir G, Karaca S, et al. The relationship between the type of unstable intertrochanteric femur fracture and mobility in the J Orthop Surg Res 13 (2018): 207.
- Kani KK, Porrino JA, Mulcahy H, et al. Fragility fractures of the proximal femur: review and update for Skeletal Radiol 48 (2019): 29-45.
- Attum B, Pilson Intertrochanteric Femur Fracture. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2022).
- Parkkari J, Kannus P, Palvanen M, et al. Majority of hip fractures occur as a result of a fall and impact on the greater trochanter of the femur: a prospective controlled hip fracture study with 206 consecutive patients. Calcif Tissue Int 65 (1999): 183-187.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result J Bone Joint Surg Am 51 (1969): 737-755.
- Simunovic N, Devereaux PJ, Bhandari M. Surgery for hip fractures: Does surgical delay affect outcomes? Indian J Orthop 45 (2011): 27-32.
- Jegathesan T, Kwek EB. Are intertrochanteric fractures evolving? Trends in the elderly population over a 10-year period. Clinics in Orthopedic Surgery 14 (2022): 13-20.
- Chapman T, Zmistowski B, Krieg J, et al. Helical Blade Versus Screw Fixation in the Treatment of Hip Fractures With Cephalomedullary Devices: Incidence of Failure and Atypical "Medial Cutout". J Orthop Trauma 32 (2018): 397-402.
- Kim CH, Kim HS, Kim YC, et al. Does the Helical Blade Lead to Higher Rates of Fixation Failure as Compared to Lag Screw in the Cephalomedullary Nailing Treatment of Hip Fractures? A Systematic Review and Meta-Analysis. J Orthop Trauma 35 (2021): 401-407.
- Sommers MB, Roth C, Hall H, et al. A laboratory model to evaluate cutout resistance of implants for pertrochanteric fracture fixation. J Orthop Trauma 18 (2004): 361-368.
- Al-Munajjed AA, Hammer J, Mayr E, et al. Biomechanical characterisation of osteosyntheses for proximal femur fractures: helical blade versus Stud Health Technol Inform 133 (2008): 1-10.
- van Leur JPH, Jakma TSC, Willemsen SP, et al. Trochanteric Fixation Nail® with Helical Blade Compared with Femoral Neck Screw for Operative Treatment of Intertrochanteric Femoral Fractures. Hip Pelvis 31 (2019): 48-56.
