Comparison of the Effect of Modified Ward’s and Triangular Flap Design on Periodontium of the Second Molar after Surgical Removal of Mandibular Impacted Third Molar
Article Information
Viral Patel1, Anil Managutti2*, Arvind Agrawal3, Shailesh Menat4, Khyati Mahida5, Dr. Jigar Patel6, Dr. Sunita Managutti7
1Private Practitioner, Ahmedabad, India
2Professor and HOD, Departmentof OMFS, Narsinhbhai Patel Dental College and Hospital, Sakalchand Patel University, Visnagar, India
3Consulting Oral and Maxillofacial Surgeon, Ahmedabad, India
4Professor, Department of OMFS, Narsinhbhai Patel Dental College and Hospital, Sakalchand Patel University, Visnagar, India
5Department of Orthodontics, Narsinhbhai Patel Dental College and Hospital, Sakalchand Patel University, Visnagar, India
6Senior Lecturer, Department of OMFS, Narsinhbhai Patel Dental College and Hospital, Sakalchand Patel University, Visnagar, India
7Reader, Department of Oral and maxillofacial pathology, Narsinhbhai Patel Dental College and Hospital, Sakalchand Patel University, Visnagar, India
*Corresponding Author: Dr. Anil Managutti, Professor and HOD, Departmentof OMFS, Narsinhbhai Patel Dental College and Hospital, Sakalchand Patel University, Visnagar, India
Received: 11 April 2020; Accepted: 24 April 2020; Published: 18 May 2020
Citation: Viral Patel, Anil Managutti, Arvind Agrawal, Shailesh Menat, Khyati Mahida, Dr. Jigar Patel, Dr. Sunita Managutti. Comparison of the Effect of Modified Ward’s and Triangular Flap Design on Periodontium of the Second Molar after Surgical Removal of Mandibular Impacted Third Molar. Archives of Clinical and Medical Case Reports 4 (2020): 459-470.
View / Download Pdf Share at FacebookAbstract
Background and Objectives: Impacted lower third molar is found in 90% of the general population. Impacted lower third molar surgery may result in complication like pain, swelling, trismus and periodontal health on the distal surface of the adjacent second molar. The aim of this study was to evaluate the effect of flap design on the pain, swelling, trismus, and periodontal health status adjacent to second molar after lower third molar surgery.
Materials and Methods: Sixty patients, with an age range of 18-25 years, participated in the present study. They were divided in two groups, each group comprised of 30 patients. In group one triangular flap was used and in group two modified Ward’s flap was used. Post-operatively pain, swelling, trismus was measured on 1st day, 3rd day, and 7th day and periodontal status at 15th days, 1st month, 3rd month and 6th month.
Results: No statistically significant differences were found in comparing of pain, swelling, trismus and periodontal status for the between both type of flap design used.
Conclusion: It was concluded that the design of mucoperiosteal flap used in surgical removal of impacted mandibular third molar have no effect on the degree of pain, swelling, trismus and periodontal health of adjacent second molar.
Keywords
Third molar surgery; Two flap design; Post-operative complication
Third molar surgery articles, Two flap design articles, Post-operative complication articles
Third molar surgery articles Third molar surgery Research articles Third molar surgery review articles Third molar surgery PubMed articles Third molar surgery PubMed Central articles Third molar surgery 2023 articles Third molar surgery 2024 articles Third molar surgery Scopus articles Third molar surgery impact factor journals Third molar surgery Scopus journals Third molar surgery PubMed journals Third molar surgery medical journals Third molar surgery free journals Third molar surgery best journals Third molar surgery top journals Third molar surgery free medical journals Third molar surgery famous journals Third molar surgery Google Scholar indexed journals Two flap design articles Two flap design Research articles Two flap design review articles Two flap design PubMed articles Two flap design PubMed Central articles Two flap design 2023 articles Two flap design 2024 articles Two flap design Scopus articles Two flap design impact factor journals Two flap design Scopus journals Two flap design PubMed journals Two flap design medical journals Two flap design free journals Two flap design best journals Two flap design top journals Two flap design free medical journals Two flap design famous journals Two flap design Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Post-operative complication articles Post-operative complication Research articles Post-operative complication review articles Post-operative complication PubMed articles Post-operative complication PubMed Central articles Post-operative complication 2023 articles Post-operative complication 2024 articles Post-operative complication Scopus articles Post-operative complication impact factor journals Post-operative complication Scopus journals Post-operative complication PubMed journals Post-operative complication medical journals Post-operative complication free journals Post-operative complication best journals Post-operative complication top journals Post-operative complication free medical journals Post-operative complication famous journals Post-operative complication Google Scholar indexed journals prophylactic articles prophylactic Research articles prophylactic review articles prophylactic PubMed articles prophylactic PubMed Central articles prophylactic 2023 articles prophylactic 2024 articles prophylactic Scopus articles prophylactic impact factor journals prophylactic Scopus journals prophylactic PubMed journals prophylactic medical journals prophylactic free journals prophylactic best journals prophylactic top journals prophylactic free medical journals prophylactic famous journals prophylactic Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals pericoronitis articles pericoronitis Research articles pericoronitis review articles pericoronitis PubMed articles pericoronitis PubMed Central articles pericoronitis 2023 articles pericoronitis 2024 articles pericoronitis Scopus articles pericoronitis impact factor journals pericoronitis Scopus journals pericoronitis PubMed journals pericoronitis medical journals pericoronitis free journals pericoronitis best journals pericoronitis top journals pericoronitis free medical journals pericoronitis famous journals pericoronitis Google Scholar indexed journals CT scan articles CT scan Research articles CT scan review articles CT scan PubMed articles CT scan PubMed Central articles CT scan 2023 articles CT scan 2024 articles CT scan Scopus articles CT scan impact factor journals CT scan Scopus journals CT scan PubMed journals CT scan medical journals CT scan free journals CT scan best journals CT scan top journals CT scan free medical journals CT scan famous journals CT scan Google Scholar indexed journals pathology articles pathology Research articles pathology review articles pathology PubMed articles pathology PubMed Central articles pathology 2023 articles pathology 2024 articles pathology Scopus articles pathology impact factor journals pathology Scopus journals pathology PubMed journals pathology medical journals pathology free journals pathology best journals pathology top journals pathology free medical journals pathology famous journals pathology Google Scholar indexed journals MRI articles MRI Research articles MRI review articles MRI PubMed articles MRI PubMed Central articles MRI 2023 articles MRI 2024 articles MRI Scopus articles MRI impact factor journals MRI Scopus journals MRI PubMed journals MRI medical journals MRI free journals MRI best journals MRI top journals MRI free medical journals MRI famous journals MRI Google Scholar indexed journals
Article Details
1. Introduction
A tooth which is completely or partially unerupted beyond its chronologic age and is position against another tooth, bone and soft tissue, so that further eruption is not possible is known as impaction. Third molar impaction surgery is a common dental procedure that requires a sound understanding and surgical principles and patient management skills [1]. Mandibular third molars are found in 90% of the general population, with 33% of the people having at least one impacted molar [2-5]. The high prevalence of impaction might be attributed to both genetic and environmental factors [2]. Third molars are situated in the area of oral cavity which is less accessible for cleaning and is frequently assaulted by microorganisms from both the oral and pharyngeal areas. So, the impacted mandibular third molar may cause pain, pericoronitis, caries, periapical pathosis, pathological resorption, increased risk of angle fracture. The removal of impacted mandibular third molar is often advocated for a variety of reasons, At the recent National Institutes of health consensus Development Conference on removal of third molars, it was agreed that impaction or malposition of a third molar was an abnormal state and might justify its removal. Such treatment was not considered to be “prophylactic,” and thus removal of impacted third molar is the most frequently performed surgical procedure in many oral and maxillofacial surgical practices [5].
The surgical removal of impacted third molar is indicated in some situation like infection, caries, pathology, prosthetic consideration and orthodontic consideration. The decision to remove the impacted third molar must be made with due consideration to the patient’s overall health status and potential risk of complication. Surgical removal of impacted mandibular third molar requires raising a mucoperiosteal flap, osteotomy and odontomy. This common procedure carries well known potential complications. One often overlooked complication is compromised periodontal status of the adjacent second molar. Different flap designs have been suggested for the surgical removal of mandibular 3rd molar to minimize the patients’ discomfort and to prevent periodontal complications [3]. The different flap designs suggested by various authors are envelope flap, ward’s flap, modified ward’s flap, S-shaped flap, Szmyd flap, triangular flap, vestibular tongue-shape flap, 3-cornered flap, modified triangular flap, marginal flap, para marginal flap, and comma shaped flap. The most common postoperative complaints including pain, trismus, swelling and wound dehiscence that influence the patient’s quality of life in the week following surgery. Intraoral suture and flap techniques affect these postoperative complications [6].
The need for this study is to understand and investigate the effect of different flap designs accessibility, post-operative pain, swelling, and trismus, periodontal health status of mandibular second molar after the impacted third molar extraction.
2. Materials and Methods
60 out patients aged between 18 and 25 years of age who were attending Oral and Maxillofacial Surgery Department, Narsinhbhai patel dental College and hospital, who required surgical removal of impacted mandibular third molar teeth and good oral hygiene were eligible for inclusion in this study. Before participation in this study, full medical histories were obtained from all patients, those with systemic diseases were excluded from the study. Women patients were excluded if they were pregnant or lactating.
60 patients were divided in two groups; in group 1, 30 impacted teeth were removed using triangular flap, in which the anterior incision curves forwards from the distobuccal corner of the crown of the second molar and ends alongside the mesiobuccal cusp of that tooth. Distally the horizontal incision was extended with the buccal side of the tooth to the external oblique ridge (Figure 1A). Whereas in group 2, modified Ward’s flap was used for the removal of 30 impacted teeth. In this type of flap design, the anterior vertical incision is commenced at the distobuccal corner of the crown of the lower first molar and extended forwards alongside that tooth. A horizontal incision is made in the buccal gingival crevice of the second molar and then the incision is extended along the buccal side of the tooth to the external oblique ridge (Figure 1B) [13].
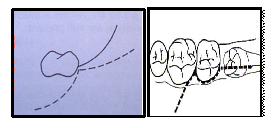
Figure 1: Tooth incisions made in the buccal gingival crevice.
All surgical procedure carried out by same surgeon. After positioning the patient in dental chair, painting and draping was done. Local anesthesia using 2% lignocaine HCL with 1:1, 80,000 adrenaline (Lignoter manufactured by: - Carewin Pharmaceutical Pvt. Ltd) was administered. In all patients inferior alveolar nerve block, lingual nerve block along with long buccal nerve block was given to the operating site depending on the procedure. After the effect of local anesthesia was achieved, surgery was started under all aseptic precautions. Surgical procedure for the impacted third molar was performed as follows. During the surgery, a verbal communication made with the patient at all time. An incision was made with Bard Parker no 15 blade and no. 3 handle. Group 1 – Triangular incision was used and group 2 –Modified Ward’s incision was used. Full thickness mucoperiosteal flap was reflected using a periosteal elevator. Bone removal was done for all impacted teeth using round No.8 and straight fissure carbide bur (no. 703). Odontomy was done using same bur. Sectioned wise tooth removal was done. After removal of tooth the socket was inspected for root fragments, loose bony fragments, and attached dental follicle sac were curetted if necessary. Through inspection for fracture of the lingual plate or exposure of the inferior alveolar nerve was done. Through curettage of the socket was done. Through inspection of distal aspect of 2nd moral was done for any caries and bone loss. Wound debridement was done with betadine and normal saline. Closure was done using 3-0 silk suture (3 simple interrupted suture). All patients were given Amoxycillincapsules (as antibacterial agent) 500 mg TID and diclofenac sodium tablets (as analgesic) 500 mg BID for 5 days post–operatively.
Assessment of Post–operative Pain The pain was evaluated subjectively according to the following criteria
0=No pain, 1=Mild pain: It is easily tolerated, 2=Moderate pain: It is causing discomfort, but bearable, 3=Severe pain: It is causing discomfort, hardly tolerated and unbearable. Assessment of the post–operative swelling was assessed subjectively by criteria developed by Sabur [1] as follows: Grade 0=No swelling, Grade 1=Oedema that involves the alveolar mucosa buccally and/or lingually (intraorally). Grade 2=Oedema that involves the alveolar mucosa buccally and/or lingually, and involves the cheek (extraorally) to the lower border of the mandible, Grade 3=Oedema that involves the alveolar mucosa buccally and/or lingually, and involves the cheek (extraorally) below the lower border of the mandible.
Further patients were evaluated for postoperative trismus after 1st day, 3rd days, 7th day. Trismus was measured by mouth opening in m.m. between maxillary central incisor and mandibular central incisor. All patients were evaluated for postoperative probing depth and alveolar bone height (distal to second molar) was measured with William’s probe in m.m. after 7th days, 15th days, 1 month, 3 months, 6 months.
3. Result
Out of 60, 23 patients were female and 37 were male patients with age from 18-25 year. Patients were randomly selected for each flap designs. Concerning group 1, there were 17 male and 13 female patients. The age range was 18-25 years with mean age 22 years. However in group 2 there were 17 male and 13 female patients. The age range from 18-25 years with mean age of 22 years (Table 1).
|
Group |
Type of flap |
Sex |
Total |
Age range (years) |
Mean Age (years) |
|
|
Male |
Female |
|||||
|
1 |
Triangular flap |
17 |
13 |
30 |
18-25 |
22.2 |
|
2 |
Modified Ward’s flap |
18 |
12 |
30 |
18-25 |
22.6 |
Table 1: Sex distribution and mean age of patients in relation to treatment group.
|
Severity of pain |
1st day |
3rd day |
7th day |
||||||
|
G1 |
G2 |
T |
G1 |
G2 |
T |
G1 |
G2 |
T |
|
|
No pain(0) |
0 |
0 |
0 |
7 |
7 |
14 |
27 |
27 |
54 |
|
Mild Pain(1) |
3 |
8 |
11 |
14 |
19 |
33 |
3 |
3 |
6 |
|
Moderate pain(2) |
19 |
16 |
35 |
9 |
4 |
13 |
0 |
0 |
0 |
|
Severe Pain (3) |
8 |
6 |
14 |
0 |
0 |
0 |
0 |
0 |
0 |
|
p-value |
0.245 |
0.262 |
1.00 |
||||||
Table 2: Patients expression of pain.
Concerning day 1 interval, all patients had a pain, but the majority of patients were suffering from moderate pain. Only 11 patient’s recorded mild pain and 14 patients showed severe pain. No statistically significant difference (p ≤ 0.005) was observed among both groups. For the 3rd day 14 patients recorded no pain, 33 patients having mild pain and 13 patients suffering from the moderate pain. Over the next seventh day, the pain levels were dramatically decreased. The majority of patients recorded no pain and only 6 patients stated mild pain. But again, no statistically significant difference was observed as shown in Table 2.
|
Severity of swelling |
1st day |
3rd day |
7th day |
||||||
|
G1 |
G2 |
T |
G1 |
G2 |
T |
G1 |
G2 |
T |
|
|
No swelling (0) |
0 |
2 |
2 |
7 |
15 |
22 |
30 |
29 |
59 |
|
Mild swelling (1) |
7 |
14 |
21 |
19 |
10 |
29 |
0 |
1 |
1 |
|
Moderate swelling(2) |
16 |
9 |
25 |
4 |
5 |
9 |
0 |
0 |
0 |
|
Severe swelling (3) |
7 |
5 |
12 |
4 |
5 |
9 |
0 |
0 |
0 |
|
p-value |
0.085 |
0.055 |
0.313 |
||||||
Table 3: Result of Swelling.
On 1st day, the majority of patients recorded grade 2 swelling. Only two patients from group 2 had no swelling (grade 0) and 12 patients had grade 3 swelling and remaining 21 patients had grade 1 swelling. At the third day, 29 patients showed grade 1 swelling and 22 patients had no swelling (grade 0). However 9 patient showed grade 2 and 9 patients showed grade 3 swelling. On 7th day 59 patients showed no swelling and only 1 patient had grade 1 swelling and that was from group 2. Statistically analysis showed no significant differences among treatment groups concerning swelling.
|
Group |
N |
Mean |
Std. Deviation |
95% Confidence Interval of the Difference |
p-value |
||
|
Lower |
Upper |
||||||
|
1st day |
1 |
30 |
23.33 |
7.107 |
-5.735 |
1.669 |
0.276 |
|
2 |
30 |
25.37 |
7.218 |
-5.735 |
1.669 |
0.276 |
|
|
3rd day |
1 |
30 |
28.43 |
5.500 |
-5.111 |
0.177 |
0.067 |
|
2 |
30 |
30.90 |
4.700 |
-5.112 |
0.179 |
0.067 |
|
|
7th day |
1 |
30 |
34.37 |
4.846 |
-3.073 |
1.273 |
0.410 |
|
2 |
30 |
35.27 |
3.443 |
-3.078 |
1.278 |
0.411 |
|
Table 4: Mouth opening in mm.
The interincisal mouth opening was measured preoperatively and postoperatively on 1st day, 3rd day, and 7th day in both groups. The mean preoperative mouth opening in triangular flap group was 39.103 mm and in modified ward’s flap group was 37.833 mm. On the 1st day, it was 23.33 ± 7.107 mm mouth opening in triangular group whereas 25.37 ± 7.218 mm in modified ward’s group. On 3rd day again we measured mouth opening, in triangular group 28.43 ± 5.50 mm and in modified ward’s group 30.90 ± 4.70 mm. After 7th day, mouth opening in group 1 was 34.37 ± 4.846 and in group 2 was 35.27 ± 3.443 mm. However, no significant difference was observed as shown in Table 4.
|
Group |
N |
Mean |
Std. Deviation |
95% Confidence Interval of the Difference |
p-value |
||
|
Lower |
Upper |
||||||
|
7th day |
1 |
30 |
8.53 |
1.613 |
-0.680 |
1.080 |
0.651 |
|
2 |
30 |
8.33 |
1.788 |
-0.680 |
1.080 |
0.651 |
|
|
15th day |
1 |
30 |
6.03 |
1.189 |
-0.748 |
0.681 |
0.926 |
|
2 |
30 |
6.07 |
1.552 |
-0.749 |
0.682 |
0.926 |
|
|
1st month |
1 |
30 |
3.73 |
0.980 |
-0.690 |
0.424 |
0.634 |
|
2 |
30 |
3.87 |
1.167 |
-0.691 |
0.424 |
0.634 |
|
|
3rd month |
1 |
30 |
2.90 |
0.305 |
-0.274 |
0.207 |
0.782 |
|
2 |
30 |
2.93 |
0.583 |
-0.276 |
0.209 |
0.783 |
|
|
6th month |
1 |
30 |
2.70 |
0.466 |
-0.118 |
0.384 |
0.292 |
|
2 |
30 |
2.57 |
0.504 |
-0.118 |
0.384 |
0.292 |
|
Table 5: Probing depth in mm.
On the 7th day, probing depth distal to second molar was measured. It was 8.53 ± 1.613mm in group 1 and 8.33 ± 1.788 mm in group 2. On 15th day again we measured probing depth at same site, in group 1 it was 6.03 ± 1.189 mm and in group 2 it was 6.07 ± 1.55 mm. After one month the probing depth in group 1 was 3.73 ± 0.980 and in group 2 was 3.87 ± 1.167 mm. After 3 month in group 1 we noticed 2.90 ± 0.305 mm and in group 2 probing depth was 2.93 ± 0.583 mm. At the end of six month we found probing depth in group 1 was 2.70 ± 0.466 mm and in group 2 was 2.57 ± 0.466 mm. That was statistically not significant.
4. Discussion
Pain, trismus and facial swelling after surgical removal of a third molar tooth are routine sequlae due to inflammation as a result of surgery. A major cause of third molar surgical trauma occurs when raising a mucoperiosteal flap to adequately visualize and gain access to the tooth [10]. The design of the flaps used to expose impacted mandibular third molar has been the subject of textbook and various articles in recent years. Several different flap techniques have been developed, compared and discussed to minimize the potential periodontal complications adjacent to second molar or improve surgical access [5].
In present study, two flap designs were assessed clinically on the most common post-operative sequalae pain, swelling, trismus and periodontal health status of the mandibular second molar after the extraction of impacted third molar. Pain is not generated due to the incision itself (whatever the type of incision) but due to the release of endogenous mediator such as bradykinin, serotonine and certain type of prostaglandin. Besides that raising in tissue tension within the inflamed area is another cause. Various authors stated that types of incision had no influence on severity of pain [1]. Pain can be evaluated subjectively by using VAS (visual analogues scale) or verbal scale. In our study, we measured pain by giving score 0 to 3.0 scale: - where there is no pain, 1 scale means mild pain, scale 2 means moderated pain and scale 3 means severe pain.
In present study, pain was severe to moderate 1stand 3rdpost-operative day in triangular group than modified ward’s flap group. There was no difference at the 7th day in pain score in both groups. But this difference was not statistically significant in both group at 1st, 3rd, and 7th day. The result of this study are in accordance with Mohammad SS1who revealed no significant difference regarding pain among envelope flap, standard flap, modified standard flap and S- shaped flap group at 1st day, 3rd days and 7th days post-operatively. The results are also in accordance with Baquin ZH et al. and Maria MS et al., who conducted study on various flap design technique.
A surgical trauma in the oral cavity always causes tissue injury characterized by hyperemia, vasodilatation, increased capillary permeability with liquid accumulation in the interstitial space and granulocyte and monocyte migration, due to the increased osmotic pressure in capillaries (Starling law). Swelling is the expression of exudates or transudation, and in surgery, probably both the events occur. Transudation in fact is secondary to blood flow slowing (i.e. hyperemia, vasodilatation, stenosis, etc.), while a superimposed infection is responsible for exudates [31]. In present study more number of patients recorded with moderate to mild swelling in triangular flap on 1st and 3rd post-operative day than that of modified ward’s flap. On 7th day both groups showed no swelling. The results of our study are in accordance with Mohammad SS, Baquin ZH, Kirk DG and Koyuncu BO. Where they have evaluated various flap design effects on swelling and found no statistical significant difference.
Trismus after third molar surgery is usually caused by inflammation of the muscles of mastication leading to spasm secondary to raising of a mucoperiosteal flap. Other possible causes include TMJ trauma, direct needle trauma to the medial pterygoid after the placement of an inferior alveolar nerve block and rarely infection [10]. It has been suggested that triangular mucoperiosteal flap induce inflammation in the muscles of mastication and it is possible that muscle irritation induced by heamatoma forming when the periosteam is incised for the anterior releasing component, is more likely with this flap design [3].
In present study, post-operative mouth opening was better in modified ward’s flap than the triangular flap. This results showed no statistically significant differences for trismus. The result of present study are in accordance with Kirk et al. [10] and Maria MS [9]. But study done by Baqain et al. [3] observed significantly greater reduction in maximum interincisal mouth opening on 7th and 14th post-operative day with triangular flap design compared to envelop flap. Mohammad SS [1] stated that trismus was reduced as a result of reduction of pain and swelling at 3rd and 7th day intervals.
Regarding the periodontal health of the adjacent molar, Peng et al. demonstrate that mandibular third molar surgery may compromise periodontal health on distal surface of second molar [3]. Results of several studies have shown that flap design has no correlation with periodontal health status of the mandibular second molar after the extraction of the adjacent impacted third molar but different short and long-term results of these correlations have been reported [2]. Kirtiloglu et al. demonstrated that the mean probing depth (PD) at distal and buccal sites was significantly different between the flaps at 1-week, 2-week, and 4-week intervals postoperatively (p<0.05) [2]. There were no significant differences in preoperative and 1-year postoperative mean PD between the two flap designs (p>0.05). In addition, the modified Szmyd flap, which leaves intact gingiva around the second molar, has better primary periodontal healing than the 3-cornered flap after surgical removal of the fullyimpacted mandibular third molar. Rosa et al. did not demonstrate any statistically significant differences in measurements of probing depth, clinical attachment level, or bone level for the two types of flaps used or the two surfaces measured [4].
The result of present study and several other studies demonstrate no significant differences in probing depth between two flap designs. Jakse et al. [7] in evaluation of the two different flap designs, demonstrated that the Szmyd flap in lower third molar surgery considerably influences primary wound healing. The modified triangular flap is significantly less conducive to the development of wound dehiscence. In another study, Brabander et al. removed molars using a mucoperiosteal flap as described by Szmyd and analysis of variance indicated that there was no significant difference between the two types of wound closure. Karacaet et al. [5] demonstrated that selection of a flap design does not seem to have a lasting effect on the health of periodontal tissue. Results of the present study and several other studies demonstrate no significant differences in pocket depth between the two flap designs.
In the present study, all operations were performed by a single surgeon, using same instruments. Therefore, patient’s compliance bias was eliminated and all other possible factor and surgical procedures were kept as constant as possible, presenting flap design as the sole independent factor to determine the severity of outcome variables. Given the small sample size in these study it is not possible to investigate the influences of flap design that prissily.
5. Conclusion
The surgical removal of an impacted mandibular third molar may generally be associated with short-term pain, swelling, trismus and long-term periodontal problem. After the surgical removal of mandibular third molar, we found pain and swelling were less in modified ward’s flap group on the first day and third day post-operatively. But at the end of seventh day pain and swelling scale was similar in triangular flap group and modified ward’s flap group. There were no statistically significant difference found on first, third and seventh post-operative day for the trismus and periodontal probing depth in surgically removal of mandibular third molar in triangular flap design and modified ward’s flap design group.
References
- Sulieman MS. Clinical evaluation of the effect of four flap designs on the post-operative sequel (pain, swelling and trismus) following the lower third molar surgery. Rafidain Dent J 5 (2005): 24-32.
- Atra SA, Kheyradin RP, Mesgarzadeh AH, et al. Comparison of the two flap design on periodontal healing after surgical extraction of impacted third molars. J Dent Res Dent Clin Dent Prospects 5 (2011): 1-4.
- Baquin ZH, Shafii AA, Hamdan AA, et al. Flap design and mandibular third molar surgery: a split mouth randomized clinical study. Int. J. oral maxillofac. Surg 41 (2012): 1020-1024.
- Rosa AL, Lavrador MA, Novaes AB. Influence of flap design on periodontal healing of second molars after extraction of impacted mandibular third molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 93 (2002): 404-407.
- Kareca I, Simsek S, Ugar D, et al. Review of flap design influence on the health of the periodontium after mandibular third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104 (2007): 18-23.
- Koyungu BO, Zeytinoglu M, Cetingul E. Comparison of 2 different flap technique in the surgical removal of bilateral impacted mandibular third molars. Turk J Med Sci 43 (2013): 891-898.
- Jakse N, Bankaoglu V, Wimmer G, et al. Primary wound healing after lower third molar surgery: evaluation of 2 different flap designs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 93 (2002): 7-12.
- Briguglio F, Zenebio EG, Isola G, et al. Complications in surgical removal of impacted mandibular third molars in relation to flap design: clinical and statistical evaluations. Quintessence int 42 (2011): 445-453.
- Maria MS, Cunqueiro S, Gutwald R, et al. marginal flap versus paramarginal flap in impacted mandibular third molar surgery: A Prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 95 (2003): 403-408.
- Kirk GD, Tong DC, Love RM. Influence of two flap designs on incidence of pain, swelling, trismus and alveolar osteitis in the week following third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104 (2007): e1-e6.
- Koyungu BO, Cetingul E. Short-term clinical outcomes of two different flap techniques in impacted mandibular third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol 116 (2013): e179-w184.
- Comma incision for impacted mandibular third molars. J Oral Maxillofac Surg 60 (2002): 1506-1509.
- Yuasa H, Sugiura M. clinical postoperative finding after removal of impacted mandibular third molars: prediction of postoperative facial swelling and pain based on preoperative variables. Br J Oral Maxillofac Surg 42 (2004): 209-214.
- Ingibrorg S, Benediktsdottir, Wenzel A, et al. Mandibular third molar removal: risk indicators for extended operation time, postoperative pain, and complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97 (2004): 438-446.
- Garcia AG, Sampedro FG, Rey JG, et al. trismus and pain after removal of impacted lower third molars. J Oral Maxillofac surg 55 (1997): 1223-1226.
- Pasqualini D, Cocero N, Castella A, et al. Primary and secondary closure of the surgical wound after removal of impacted mandibular third molars: a comparative study. Int. J. Oral Maxillofac. Surg 34 (2005): 52-57.
- Cetinkaya BO, Sumer M, Tutkun F, et al. Influence of different suturing techniques on periodontal health of the adjacent second molars after extraction of impacted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108 (2009): 156-161.
- Hashemi HM, Beshkar M, Aghajani R. The effect of suturless wound closure on postoperative pain and swelling after impacted mandibular third molar surgery. Br J Oral Maxillofac Surg 50 (2012): 256-258.
- Ghoreshian M, Gheisari R, Fayazi M. Tissue adhesive and suturing for closure of the surgical wound after removal of impacted mandibular third molars: A Comparative study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108 (2009): e14-e16.
- Rakprasitkul S, Pairuehvej V. Mandibular third molar surgery with primary closure and tube drain. Int. J. Oral Maxillofac. Surg 26 (1997): 187-190.
- Krausz AA, Machtei EE, Peled M. Effect of lower third molar extraction on attachment level and alveolar bone height of the adjacent second molar. Int. J. Oral Maxillofac. Surg 34 (2005): 756-760.
- Peng KY, Tseng YC, Shen EC, et al. Mandibular second molar periodontal status after third molar extraction. J Periodontol 72 (2001): 1647-1651.
- Dodson TB. Management of mandibular third molar extraction site to prevent periodontal defect. J Oral Maxillofac Surg 62 (2004): 1213-1224.
- Yee WS, Rahman RA, Taib H. Effect of lower third molar removal on attachment level and alveolar bone height of the adjacent second molar. Archives of orofacial sciences 4 (2009): 36-40.
- Dodson TB. Reconstruction of alveolar bone defects after extraction of mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 82 (1996): 241-247.
- Monaco G, Daprile G, Tavernese L, et al. Mandibular third molar removal in young patients: an evaluation of 2 different flap designs. J Oral Maxillofac Surg 67 (2009): 15-21.
- Roode GJ, Butow K. An alternative surgical flap design for impacted third molars: A comparison of two different surgical techniques 65 (2010): 246-251.
- Kjolle GK, Bjorland T. Low risk of neurosensory dysfunction after mandibular third molar surgery in pateints less than 30 years of age. A prospective study following removal of 1220 mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol 116 (2013): 411-417.
- Engelke W, Beltran V, Cantin M, et al. Removal of impacted mandibular third molars using an inward fragmentation technique (IFT) – Method and first results. Journal of cranio-maxillo-facial surgery 42 (2014): 213-219.
- Sortino F, Cicciu M. Strategies used to inhibit post-operative swelling following removal of impacted lower third molar. Dent res J 8 (2011): 162-171.
- Hill CM, Mostafa P, Thomas DW, et al. Nerve morbidity following wisdom tooth removal under local and general anaesthesia. Br J Oral Maxillofac Surg 39 (2001): 419-422.
- Renton T, McGurk M. Evaluation of factors predictive of lingual nerve injury in third molar surgery. Br J Oral Maxillofac Surg 39 (2001): 423-428.
- Sekhar CH, Narayanan V, Baig MF. Role of antimicrobials in third molar surgery: Prospective, double blind, randomized, placebo–controlled clinical study. Br J Oral Maxillofac Surg 39 (2001): 134-137.
