Comparison of Effectiveness of Chiropractic Spinal Manipulation and Conservative Therapy for Low Back Pain
Article Information
Emmanuel Wong*, Wai Ting Lee, Cherrie Chau, Hay Yeung Cheng, Ronald Kwok
Mctimoney College of Chiropractic, Ulster University, York St, Belfast BT15 1ED, United Kingdom
*Corresponding Author: Emmanuel Wong, Mctimoney College of Chiropractic, Ulster University, York St, Belfast BT15 1ED, United Kingdom.
Received: 21 December 2022; Accepted: 28 December 2022; Published: 03 January 2023
Citation:
Emmanuel Wong, Wai Ting Lee, Cherrie Chau, Hay Yeung Cheng, Ronald Kwok. Comparison of Effectiveness of Chiropractic Spinal Manipulation and Conservative Therapy for Low Back Pain. Journal of Orthopedics and Sports Medicine 5 (2023): 01-08.
View / Download Pdf Share at FacebookAbstract
The study is to describe the current evidence for the effectiveness of chiropractic spinal manipulation in comparison to the conservative intervention on Low Back Pain (LBP). The PubMed database was searched for randomised clinical trials of spinal manipulation and low back pain. Criteria for inclusion was subjects with low back pain treated with chiropractic spinal manipulation. Studies were excluded when participants were under the age of 18; conditions that were considered to be outside the discipline of manual therapy including systemic disease or malignancy, osteoporosis, pathological causes of LBP, LBP with radiculopathy; and contraindications to spinal manipulation. Data extraction included study design, number of participants, gestational age, spinal region, number of manipulations, manipulation technique details, profession of manipulator, active exercise reporting (Yes vs. No), type, and number of active exercises. Chiropractic care seems to be more effective than conservative intervention for LBP in reducing pain, increasing range of motion in lumbar spine, improving disability status, and enhancing general health. Furthermore, integrative care for LBP could be considered to improvise in the future treatment plan. The review of comparing different treatment approaches for LBP is still lacking and future research is needed to consider including a control group in order to provide accurate and persuasive outcomes.
Keywords
Low Back Pain; Chiropractic; Spinal manipulation
Active exercise articles Active exercise Research articles Active exercise review articles Active exercise PubMed articles Active exercise PubMed Central articles Active exercise 2023 articles Active exercise 2024 articles Active exercise Scopus articles Active exercise impact factor journals Active exercise Scopus journals Active exercise PubMed journals Active exercise medical journals Active exercise free journals Active exercise best journals Active exercise top journals Active exercise free medical journals Active exercise famous journals Active exercise Google Scholar indexed journals Intervertebral discs articles Intervertebral discs Research articles Intervertebral discs review articles Intervertebral discs PubMed articles Intervertebral discs PubMed Central articles Intervertebral discs 2023 articles Intervertebral discs 2024 articles Intervertebral discs Scopus articles Intervertebral discs impact factor journals Intervertebral discs Scopus journals Intervertebral discs PubMed journals Intervertebral discs medical journals Intervertebral discs free journals Intervertebral discs best journals Intervertebral discs top journals Intervertebral discs free medical journals Intervertebral discs famous journals Intervertebral discs Google Scholar indexed journals Lower back pain articles Lower back pain Research articles Lower back pain review articles Lower back pain PubMed articles Lower back pain PubMed Central articles Lower back pain 2023 articles Lower back pain 2024 articles Lower back pain Scopus articles Lower back pain impact factor journals Lower back pain Scopus journals Lower back pain PubMed journals Lower back pain medical journals Lower back pain free journals Lower back pain best journals Lower back pain top journals Lower back pain free medical journals Lower back pain famous journals Lower back pain Google Scholar indexed journals Chiropractic care articles Chiropractic care Research articles Chiropractic care review articles Chiropractic care PubMed articles Chiropractic care PubMed Central articles Chiropractic care 2023 articles Chiropractic care 2024 articles Chiropractic care Scopus articles Chiropractic care impact factor journals Chiropractic care Scopus journals Chiropractic care PubMed journals Chiropractic care medical journals Chiropractic care free journals Chiropractic care best journals Chiropractic care top journals Chiropractic care free medical journals Chiropractic care famous journals Chiropractic care Google Scholar indexed journals Spinal Manipulation Technique articles Spinal Manipulation Technique Research articles Spinal Manipulation Technique review articles Spinal Manipulation Technique PubMed articles Spinal Manipulation Technique PubMed Central articles Spinal Manipulation Technique 2023 articles Spinal Manipulation Technique 2024 articles Spinal Manipulation Technique Scopus articles Spinal Manipulation Technique impact factor journals Spinal Manipulation Technique Scopus journals Spinal Manipulation Technique PubMed journals Spinal Manipulation Technique medical journals Spinal Manipulation Technique free journals Spinal Manipulation Technique best journals Spinal Manipulation Technique top journals Spinal Manipulation Technique free medical journals Spinal Manipulation Technique famous journals Spinal Manipulation Technique Google Scholar indexed journals Musculoskeletal articles Musculoskeletal Research articles Musculoskeletal review articles Musculoskeletal PubMed articles Musculoskeletal PubMed Central articles Musculoskeletal 2023 articles Musculoskeletal 2024 articles Musculoskeletal Scopus articles Musculoskeletal impact factor journals Musculoskeletal Scopus journals Musculoskeletal PubMed journals Musculoskeletal medical journals Musculoskeletal free journals Musculoskeletal best journals Musculoskeletal top journals Musculoskeletal free medical journals Musculoskeletal famous journals Musculoskeletal Google Scholar indexed journals Temporomandibular joint pain articles Temporomandibular joint pain Research articles Temporomandibular joint pain review articles Temporomandibular joint pain PubMed articles Temporomandibular joint pain PubMed Central articles Temporomandibular joint pain 2023 articles Temporomandibular joint pain 2024 articles Temporomandibular joint pain Scopus articles Temporomandibular joint pain impact factor journals Temporomandibular joint pain Scopus journals Temporomandibular joint pain PubMed journals Temporomandibular joint pain medical journals Temporomandibular joint pain free journals Temporomandibular joint pain best journals Temporomandibular joint pain top journals Temporomandibular joint pain free medical journals Temporomandibular joint pain famous journals Temporomandibular joint pain Google Scholar indexed journals Shoulder pain articles Shoulder pain Research articles Shoulder pain review articles Shoulder pain PubMed articles Shoulder pain PubMed Central articles Shoulder pain 2023 articles Shoulder pain 2024 articles Shoulder pain Scopus articles Shoulder pain impact factor journals Shoulder pain Scopus journals Shoulder pain PubMed journals Shoulder pain medical journals Shoulder pain free journals Shoulder pain best journals Shoulder pain top journals Shoulder pain free medical journals Shoulder pain famous journals Shoulder pain Google Scholar indexed journals Back pain articles Back pain Research articles Back pain review articles Back pain PubMed articles Back pain PubMed Central articles Back pain 2023 articles Back pain 2024 articles Back pain Scopus articles Back pain impact factor journals Back pain Scopus journals Back pain PubMed journals Back pain medical journals Back pain free journals Back pain best journals Back pain top journals Back pain free medical journals Back pain famous journals Back pain Google Scholar indexed journals Knee pain articles Knee pain Research articles Knee pain review articles Knee pain PubMed articles Knee pain PubMed Central articles Knee pain 2023 articles Knee pain 2024 articles Knee pain Scopus articles Knee pain impact factor journals Knee pain Scopus journals Knee pain PubMed journals Knee pain medical journals Knee pain free journals Knee pain best journals Knee pain top journals Knee pain free medical journals Knee pain famous journals Knee pain Google Scholar indexed journals Inflammatory arthritis articles Inflammatory arthritis Research articles Inflammatory arthritis review articles Inflammatory arthritis PubMed articles Inflammatory arthritis PubMed Central articles Inflammatory arthritis 2023 articles Inflammatory arthritis 2024 articles Inflammatory arthritis Scopus articles Inflammatory arthritis impact factor journals Inflammatory arthritis Scopus journals Inflammatory arthritis PubMed journals Inflammatory arthritis medical journals Inflammatory arthritis free journals Inflammatory arthritis best journals Inflammatory arthritis top journals Inflammatory arthritis free medical journals Inflammatory arthritis famous journals Inflammatory arthritis Google Scholar indexed journals Rheumatoid arthritis articles Rheumatoid arthritis Research articles Rheumatoid arthritis review articles Rheumatoid arthritis PubMed articles Rheumatoid arthritis PubMed Central articles Rheumatoid arthritis 2023 articles Rheumatoid arthritis 2024 articles Rheumatoid arthritis Scopus articles Rheumatoid arthritis impact factor journals Rheumatoid arthritis Scopus journals Rheumatoid arthritis PubMed journals Rheumatoid arthritis medical journals Rheumatoid arthritis free journals Rheumatoid arthritis best journals Rheumatoid arthritis top journals Rheumatoid arthritis free medical journals Rheumatoid arthritis famous journals Rheumatoid arthritis Google Scholar indexed journals Neuromusculoskeletal articles Neuromusculoskeletal Research articles Neuromusculoskeletal review articles Neuromusculoskeletal PubMed articles Neuromusculoskeletal PubMed Central articles Neuromusculoskeletal 2023 articles Neuromusculoskeletal 2024 articles Neuromusculoskeletal Scopus articles Neuromusculoskeletal impact factor journals Neuromusculoskeletal Scopus journals Neuromusculoskeletal PubMed journals Neuromusculoskeletal medical journals Neuromusculoskeletal free journals Neuromusculoskeletal best journals Neuromusculoskeletal top journals Neuromusculoskeletal free medical journals Neuromusculoskeletal famous journals Neuromusculoskeletal Google Scholar indexed journals Pain management articles Pain management Research articles Pain management review articles Pain management PubMed articles Pain management PubMed Central articles Pain management 2023 articles Pain management 2024 articles Pain management Scopus articles Pain management impact factor journals Pain management Scopus journals Pain management PubMed journals Pain management medical journals Pain management free journals Pain management best journals Pain management top journals Pain management free medical journals Pain management famous journals Pain management Google Scholar indexed journals Radiating leg pain articles Radiating leg pain Research articles Radiating leg pain review articles Radiating leg pain PubMed articles Radiating leg pain PubMed Central articles Radiating leg pain 2023 articles Radiating leg pain 2024 articles Radiating leg pain Scopus articles Radiating leg pain impact factor journals Radiating leg pain Scopus journals Radiating leg pain PubMed journals Radiating leg pain medical journals Radiating leg pain free journals Radiating leg pain best journals Radiating leg pain top journals Radiating leg pain free medical journals Radiating leg pain famous journals Radiating leg pain Google Scholar indexed journals
Article Details
Abbreviations:
AE: Active Exercise; CAM: Complementary and Alternative Medicine; CASP: Critical Appraisal Skills Programme; HVLA: High-Velocity Low-Amplitude; IVDs: Intervertebral Discs; LBP: Lower Back Pain; NICE: National Institute for Health and Care Excellence; NRS: Numeric Rating Scale; ODI: The Oswestry Disability Index; PRODISQ: Productivity and Disease Questionnaire; PROMIS: Patient Reported Outcomes Measurement; RCT: Randomised Controlled Trial; SF-39: 39 item Health Status Questionnaire; SMT: Spinal Manipulative Technique; UMC: Usual Medical Care; VAS: Visual Analog Pain Scales; WHO: World Health Organisation
1. Introduction
Chiropractic care is a healthcare profession which focuses on hands-on treatment. It is known for the use of Spinal Manipulation Technique (SMT) or manual manipulation, as it refers to high velocity and low amplitude adjustment to restore and sustain general health and well-being by treating the spine. Also chiropractors have long been visited for musculoskeletal condition such as headache [1], dizziness [2-5], facial pain [6], neck pain [7,8], temporomandibular joint pain [9], shoulder pain [10], back pain [11,12], knee pain [13], and scoliosis [14-17]; inflammatory arthritis such as rheumatoid arthritis [18-21]; and other neurodegenerative disorders [22-29]. Chiropractors often encountered life-threatening condition such as infection [30], tumour [31], and cancer [30-36]. Some chiropractors believe that chiropractic care can help to avoid health issues as well as maintain health and fitness [37]. In fact, research discovered that 40% of patients pursue chiropractic therapy expressly for illness prevention [38] and posture improvement [39-40]. The World Health Organisation (WHO) defines chiropractic as “a health care profession focused with the diagnosis, treatment, and prevention of problems of the neuromusculoskeletal system, as well as the implications of such illnesses on overall health. Manual procedures, such as joint adjustment and/or manipulation, are utilised, with a special emphasis on subluxation [41].
Chiropractic is also marketed as a treatment that is both effective and holistic [42]. Chiropractors believe that the body as a whole is connected, and that the body can sustain its health if the body’s integrity is preserved. There are also suggestions that chiropractic could help with a variety of non-musculoskeletal symptoms such as visual disturbance [43,44], angina and cardiovascular symptoms [45-48], dysphagia and gastrointestinal disorders [49-52], and testicular pain and reproductive dysfunctions [53-55].
In view of conservative treatment for LBP, it generally comprises prevention [56], rest, cold pads, medications, muscle relaxants, post-surgical rehabilitation [57-58] and physiotherapy. People can take an active role in prevention as it is an important self-management skill. Except for the above pain management, there is also some intensive pain management. It includes the nerve blocks and injections, intraspinal implants, spinal cord stimulation, intraspinal infusion systems and surgery.
The purpose of this narrative is to review the current evidence for the effectiveness of chiropractic spinal manipulation in comparison to the conservative intervention on low back pain. Chiropractic manipulative adjustment has become popular and it's essential to understand the optimal method in conservative treatment.
2. Methodology
A review of the literature was performed using the PubMed database. Search terms included subjects with low back pain treated with chiropractic spinal manipulation. The study includes the most relevant data related to LBP regarding the treatment methods and excluded when participants were under the age of 18; conditions that were considered to be outside the discipline of manual therapy including systemic disease or malignancy, osteoporosis, pathological causes of LBP, LBP with radiculopathy; and contraindications to spinal manipulation. Data extraction included study design, number of participants, gestational age, spinal region, number of manipulations, manipulation technique details, profession of manipulator, active exercise reporting (Yes vs. No), type, and number of active exercises. The bibliographies of articles discerned to be relevant were also reviewed. Database was searched from 1st July 2002 to 1st December 2022.
3. Results
The majority of people believe that manual and physical treatments, such as chiropractic, are safe, accessible, and helpful in treating the conditions. According to a study, spinal manipulation or mobilisation is beneficial for acute, subacute, and chronic LBP in adults [59]. Spinal manipulation or mobilisation is recommended as an effective therapy for acute, subacute, and chronic LBP by four guidelines in total which include National Institute for Health and Care Excellence (NICE), The American College of Physicians Pain Society, European guidelines for chronic LBP, and European guidelines for acute LBP. There is strong evidence that spinal manipulation or mobilisation is a viable therapy choice for people suffering with subacute and chronic LBP [60]. Evidence of moderate quality shows spinal manipulation or mobilisation is a viable therapy choice for individuals with acute LBP and older adults with subacute and chronic LBP [61]. On the other hand, evidence is inconclusive when it comes to using SMT for sciatica and radiating leg pain.
There are 8 papers in total that met the inclusion criteria. The following Table 1 has included the title, author and year, study design, methodology, patient group, intervention, and outcome measures (Figure 1).
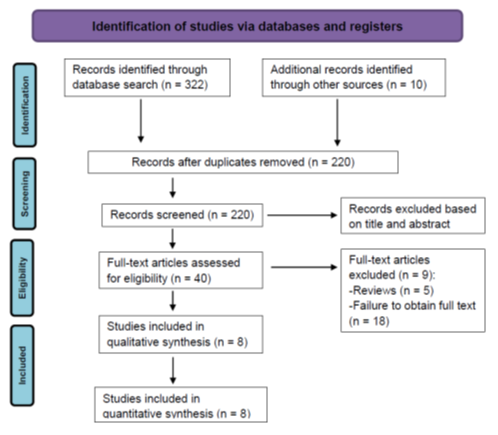
Figure 1: Flow Diagram of Randomised Trial Control of Chiropractic SMT and conservative intervention for LBP.
Goertz et al. [62] conducted an RCT with the primary aim of comparing pain and disability of military personnel with LBP who are treated with chiropractic care and UMC compared with those treated with UMC alone. They hypothesize that those allocated to receive both chiropractic care plus UMC will have greater reduction in pain and disability than those receiving UMC alone. The secondary aim is to explore the effects of adding chiropractic care to UMC on healthcare utilisation, medication use, and quality of life. RCTs have demonstrated that chiropractic care and its signature treatment, spinal manipulation, is an effective conservative care option for patients with LBP. They have concluded that improvements in pain and disability were significantly greater in the chiropractic care group.
Hoskins conducted a RCT with the objective to investigate whether a sports chiropractic intervention consisting of pragmatically and individually determined High-Velocity Low-Amplitude (HVLA) manipulation, mobilisation and/or supporting soft tissue therapies to the spine, pelvis and extremity could decrease LBP [63]. The results showed that a sports chiropractic manual therapy intervention was the best practice multi-disciplinary medical, paramedical and sports science management. Also, reduction in LBP was observed along with improvements measured by the SF-39.
Westrom [64] conducted an RCT with the primary aim to determine the relative clinical efficacy of chiropractic care and integrative care for LBP in both short-term and long-term period. As a secondary aim, they have determined the short- and long-term relative efficacy of the two interventions using the secondary patient-rated outcome measures. Combining modalities has been considered as having a synergistic impact that might lead to higher gains, also this study promotes the use of Complementary and Alternative Medicine (CAM) in conjunction with conventional therapy. Individualising therapy has the potential to improve results in non-specific low back pain when many effective therapies have only small impact when administered to the group as a whole.
Schneder et al. [65] conducted an RCT with the objective of comparing the effectiveness of Manual-Thrust Manipulation (MTM) versus Mechanical-Assisted Manipulation (MAM) and manipulation versus Usual Medical Care (UMC). They have concluded that MTM provides greater short-term reductions in self-reported disability and pain scores compared to UMC or MAM. Furthermore, statistics have shown there was a significant advantage of MTM at 4 weeks compared to MAM and UMC. Yet, no statistically significant group differences were found between MAM and UAC. Both groups appear similar in effect which leads to decreased pain and disability.
Aure et al. [66] conducted an RCT with the aim to compare the effect of manual therapy, consisting of specific exercises and segmental techniques, to general exercise therapy in chronic LBP patients. The results showed that significant improvements were observed in both groups, however, the Manual Therapy (MT) group showed significantly large improvements than the Exercise Therapy (ET) group on all outcome variables throughout the entire experimental period. The authors also mentioned that the study's sample size was small, and the rigorous inclusion criteria may limit the results' applicability to other chronic LBP groups.
Dougherty conducted an RCT with two hypotheses. The first hypothesis is that patients in both Spinal Manipulative Therapy (SMT) and Active Exercise Therapy (AET) groups would demonstrate statistically and clinically significant improvements in disability and pain from baseline [67]. The second hypothesis predicts that the Modification Clinical Predication Rule (mCPR) moderates the comparative effectiveness of treatment in the SMT group but not the AET treatment group. Furthermore, the authors concluded that no evidence that a mCPR can be used to discriminate chronic LBP patients that would benefit more from SMT.
A random control trial evaluated the effectiveness of twelve weeks of monodisciplinary Chiropractic Care (CC), versus multidisciplinary Integrative Care (IC) for adults with sub-acute and chronic LBP [68]. The primary outcome was measuring the pain intensity. In the primary analysis, the authors concluded that participants in IC group to be significantly superior to CC group over the 1-year period. As a result, participants in IC group tended to have better outcomes than the CC group. Furthermore, the authors also mentioned that the magnitude of the group differences was relatively small.
An assessor-blinded RCT was studied with the aim to address the relative effectiveness of joint manipulation, myofascial therapy, combined joint manipulation and myofascial therapy, and back school for the management of subacute LBP [69]. The authors concluded that joint manipulation, myofascial therapy, and back school appeared to be as effective as combined joint manipulation and myofascial therapy for reducing pain and functional disability for subacute LBP. The improvement gained after 3 weeks of treatment was well maintained for 6 months. This study did not reach the recruitment goal of having 300 participants; however, the authors believe that this study should have abilities to detect clinically significant differences between groups.
4. Discussion
When it comes to adopting the principle of ‘do no harm’, chiropractic has a significant advantage. Chiropractic, and especially SMT, is typically safe, according to different research literature. Research suggests that the risk of major harm from SMT is incredibly minimal. Almost all of the side effects associated with SMT are temporary and small. Overall, SMT has a high safety rating, particularly in comparison to alternative therapeutic methods. Chiropractic progressed employing a conservative treatment regimen comprising of manual and physiotherapy, along with exercise, based on historic precedence. There is no need to expand chiropractic’s treatment scope. It depends on the conservative techniques sustained clinical success and improved safety profile compared to various more invasive therapies, including medicine and operation. None of these medicines, whether conservative or not, will stay constant in the future, and the relative benefits might alter as well. Chiropractic’s commitment to a conservative treatment approach would be only legitimate as long as it is scientifically and financially viable.
4.1 Chiropractic care
For the time being, no one therapy technique has been identified as the gold standard therapy for low back pain. SMT which is delivered by chiropractors, is a regularly utilised treatment that has consistently excellent effects in terms of pain intensity and functionality in a civil population. Goertz et al. [62] said that low back pain is one of the primary leading factors of disability among U.S. military personnel, it's critical to identify practical and conservative therapies that would not only heal LBP but also maintain low back function, ensuring military preparedness. LBP has now been called "the hidden military danger" because of its associated expenses of human suffering, healthcare, and disabilities, as well as the accompanying reduced ability of personnel to perform military actions [70]. Clinical practice recommendations for patients with acute, subacute, and chronic LBP suggest chiropractic therapy or spinal manipulation as a scientific proof, cost-effective, conservative treatment approach [61].
Chiropractors, physiotherapists, and osteopathic physicians employ SMT to treat LBP. Schnelder et al. [65] stated that Manual-Thrust Manipulation (MTM) has been the topic of systematic review, which are not applicable to Mechanical-assisted Manipulation (MAM) approaches. Chiropractors still adopt MTM as the most prevalent method of manipulation. However, throughout the last decade, studies of the chiropractic profession have revealed a tendency towards greater use of mechanical manipulation tools. Mechanical tools are marketed as safe and efficient replacements to manual manipulation, though there are few high-quality studies to back this up. The considerable benefit of MTM versus MAM in reducing both disability and pain ratings was a key finding from the research. In addition, as comparing to the MAM group, the MTM group had a minimum 25% higher responses for both outcomes and degrees of improvement. These data dispute the hypothesis that these two manipulation strategies are therapeutically equivalent. When educating patients on the various manipulative therapy choices for LBP, it is yet another crucial thing to examine. Furthermore, MTM resulted with larger short-term pain and disability improvements than MAM and usual medical care [65].
A variety of conservative treatment approaches and treatments for LBP have been examined, however the preferred treatment stays a contentious issue. Different national standards for LBP therapy in primary care have been declared to be generally similar, however discrepancies have now been highlighted particularly in relation to exercise and spinal manipulation. Manual therapy used to have a significant beneficial impact on chronic LBP and had been preferable to medical treatment, bed rest, and educational advice in a study of clinical studies involving individuals with chronic LBP [71]. The goal was to look at a manual therapy method that included spinal manipulation and mobilisation approaches, targeted stretches, localised exercises, and information, is conducted in clinical settings. The therapy approaches are targeted at normalising function by using spinal or peripheral joint manipulation and mobilisation strategies, targeted muscle stretches, and exercises to the afflicted spinal segment or peripheral joint region regarding the clinical evaluation. Despite the fact that both participants in the intervention group saw considerable progress, the manual therapy group outperformed the standard exercise therapy group with all outcome measures, such as pain, functional impairment, health in general, range of motion in the spine, and return to work [66]. Most of the outcomes were obtained throughout the 8-week therapy interval.
4.2 Integrative care
Having numerous effective therapies also gives patients more options, which may improve clinical outcome by enabling patients to voice their preferences [72]. There does not seem to be a particular therapy approach for non-specific LBP which is optimal for all individuals, but rather a number of viable treatments. Furthermore, it is anticipated that by integrating the effort and attention of various clinicians, a collaborative approach may achieve more than monodisciplinary treatment, especially for chronic illnesses [73]. Merging modalities has already been considered as having a synergistic impact that could result in significant improvements. Westrom et al. [64] concluded that the study they have done comparing the monodisciplinary chiropractic care and multidisciplinary integrative care where it promotes the use of complementary alternative medicine in conjunction with conventional therapy. When numerous efficacious therapies have limited impact while administered to the group as a whole, individualising care seems to have a potential to enhance results in non-specific LBP.
Previous research from Kizhakkeveettil et al. [74] has indicated that combining alternative modalities with traditional methods can help with LBP. Such techniques incorporate a variety of effective treatment choices to target multiple sources of pain in a synergistic manner, with the objective of outperforming any single treatment independently [75]. Bronfort et al. [59] conducted a study to compare the clinical effectiveness of chiropractic care and integrative care for adults who have subacute and chronic LBP in 12 weeks [68]. Patients with LBP who got integrative care from a multidisciplinary integrative care team performed much better than those who got chiropractic treatment. Notably, both intervention led to any major adverse events, and less major incidents were roughly equal in both groups. Integrating different modalities offer significant benefits to the infrastructure of the industry. Chiropractic will be possible to attain a far larger number of patients and practise in a wider range of patient care settings by operating inside the mainline of healthcare.
4.3 No differences between chiropractic care and integrative care
Chronic LBP is just second to respiratory problems as a cause for seeing a primary care physician. Inappropriate care owing to a lack of awareness of prognostic variables is one important cause. Both SMT and AET are widely used, evidence-base therapies for chronic LBP, although none of these has been demonstrated to be superior. Investigation of certain factors that predict clinical response to these therapies has been proposed as a way to enhance performance via proper management [76]. Dougherty concluded that patients benefited from both SMT and AET treatment, and there were no differences regarding the outcomes [67]. Future research is required to fully appreciate the specific and non-specific character of chronic LBP therapies, as well as to assist general practitioners in deciding which intervention would be more suitable [77]. In order to effectively tackle these underlying anomalies with more effective therapy, further research is needed to examine the fundamental physiological and psychological principle in chronic LBP. Furthermore, a study done by Hsieh with the aim to compare the effectiveness of four approaches (back school, myofascial therapy, joint manipulation, and combined joint manipulation and myofascial therapy) concluded that there were no major differences in terms of pain, lumbar mobility, and functional disability for subacute LBP [69].
5. Limitations
The nature of the narrative review has the limitation of being misleading due to selection bias, subjective weighting of the papers selected for review, undefined inclusion criteria, and failing to analyse the links among study features and research outcomes. Additionally, the RCTs analysed contains lots of variables; the trials all incorporated manual treatments that are generally delivered by chiropractors, but they also had to incorporate several modalities that are not offered by the profession. The absence of a standardised outcome measurement instrument must be demonstrated, however other less well-known techniques were utilised to assess outcomes in the research. There was no control group in some trials, and the investigations were largely short-term. These variables make it impossible to make a genuine comparison.
6. Conclusion
Either chiropractic spinal manipulation alone or integrative care is effective for patients with acute, subacute, and chronic LBP in reducing pain, increasing range of motion, improving disability, enhancing general health and returning to work. The review of comparing different treatment approaches for LBP is still lacking and future research is needed to consider including a control group in order to provide accurate and persuasive outcomes. Based on the updated results, chiropractic spinal manipulation alone could reduce LBP effectively, however, future treatment plans could promote multidisciplinary care to deal with LBP.
Acknowledgments:
None
Author contribution statement:
EW, WTL, CC, HYC contributed the case information. EW, WTL drafted the manuscript and prepared the figures. All authors have read and approved the final manuscript.
References
- Chu ECP, Ng M. Long-term relief from tension-type headache and major depression following chiropractic treatment. J Family Med Prim Care 7 (2018): 629-631.
- Chu ECP, Chin WL, Bhaumik A. Cervicogenic dizziness. Oxf Med Case Reports (2019): 476-478.
- Chu EC, Trager RJ, Tao C, et al. Chiropractic Management of Neck Pain Complicated by Symptomatic Vertebral Artery Stenosis and Dizziness. Am J Case Rep 19 (2022): e937991.
- Chu EC, Zoubi FA, Yang J. Cervicogenic Dizziness Associated With Craniocervical Instability: A Case Report. J Med Cases 12 (2021): 451-454.
- Chu EC, Wong AY. Cervicogenic Dizziness in an 11-Year-Old Girl: A Case Report. Adolesc Health Med Ther 12 (2021): 111-116.
- Chu EC, Trager RJ, Chen AT. Concurrent Bell's Palsy and Facial Pain Improving with Multimodal Chiropractic Therapy: A Case Report and Literature Review. Am J Case Rep 23 (2022) :e937511.
- Chu ECP, Chakkaravarthy DM, Lo FS, et al. Atlantoaxial Rotatory Subluxation in a 10-Year-Old Boy. Clin Med Insights Arthritis Musculoskelet Disord. 13 (2020): 1179544120939069.
- Chu EC. Preventing the progression of text neck in a young man: A case report. Radiol Case Rep 17 (2022): 978-982.
- Chu EC, Chiang R. Giant cell arteritis: a cause of temporomandibular joint claudication. J Med Life 15 (2022): 1322-1326.
- Chu EC. Shoulder Injury Related to Vaccine Administration (SIRVA) in 16 Patients Following COVID-19 Vaccination Who Presented to Chiropractic, Orthopedic, and Physiotherapy Clinics in Hong Kong During 2021. Med Sci Monit 28 (2022): e937430.
- Chu EC, Trager RJ. Prevalence of Serious Pathology among Adults with Low Back Pain Presenting for Chiropractic Care: A Retrospective Chart Review of Integrated Clinics in Hong Kong. Med Sci Monit. 28 (2022): e938042.
- Chu ECP, Wong AYL. Change in Pelvic Incidence Associated With Sacroiliac Joint Dysfunction: A Case Report. J Med Cases. 13 (2022): 31-35.
- Chu EC, Lin AFC. Knee Pain Following Total Knee Arthroplasty Secondary to Cervical Spondylotic Myelopathy. Curr Health Sci J 48 (2022): 226-229.
- Chu EC. Neuromuscular scoliosis in the presence of spina bifida occulta and a transitional lumbosacral vertebra: A case report. Radiol Case Rep 17 (2022): 3260-3265.
- Pu Chu EC, Kai Huang KH. Bridging the gap between observation and brace treatment for adolescent idiopathic scoliosis. J Family Med Prim Care 6 (2017): 447-449.
- Pu Chu EC, Chakkaravarthy DM, Huang KHK, et al. Changes in radiographic parameters following chiropractic treatment in 10 patients with adolescent idiopathic scoliosis: A retrospective chart review. Clin Pract 10 (2020): 1258.
- Chu EC. Improvement of quality of life by conservative management of thoracic scoliosis at 172°: a case report. J Med Life 15 (2022): 144-148.
- Chu EC, Wong AY, Lee LY. Craniocervical instability associated with rheumatoid arthritis: a case report and brief review. AME Case Rep 5 (2021): 12.
- Chu ECP, Lo FS, Bhaumik A. Remission of recalcitrant dermatomyositis following a chiropractic adjustment. J Family Med Prim Care 8 (2019): 3742-3744.
- Chu ECP, Bellin D. Remission of myasthenia gravis following cervical adjustment. AME Case Rep 3 (2019): 9.
- Chu EC, Yip AS. A rare presentation of benign acute childhood myositis. Clin Case Rep 7 (2019): 461-464.
- Chu EC, Lee LY. Cervical Spondylosis as a Hidden Contributing Factor to Fibromyalgia: A Case Report. Int Med Case Rep J 15 (2022): 639-646.
- Chu EC, Chen AT, Chiang R. Chiropractic care of Parkinson's disease and deformity. J Med Life 15 (2022): 717-722.
- Chu EC, Wong AY. Mitigating Gait Decline in a Woman with Parkinson's Disease: A Case Report. J Med Cases. 13 (2022): 140-144.
- Chu ECP, Wong AYL, Lee LYK. Chiropractic care for low back pain, gait and posture in a patient with Parkinson's disease: a case report and brief review. AME Case Rep 5 (2021): 34.
- Chu EC. Remission of Headache and Neck Pain Following Chiropractic Manipulative Treatment in a Patient with Neurofibromatosis. Chiropractic Journal of Australia 49 (2022): 8-18.
- Chu EC, Wong AY, Lin AF. Isolated Neck Extensor Myopathy Associated With Cervical Spondylosis: A Case Report and Brief Review. Clin Med Insights Arthritis Musculoskelet Disord 13 (2020): 1179544120977844.
- Chu ECP, Lam KKW. Post-poliomyelitis syndrome. Int Med Case Rep J 12 (2019): 261-264.
- Chu ECP, Chan AKC, Lin AFC. Pitting oedema in a polio survivor with lumbar radiculopathy complicated disc herniation. J Family Med Prim Care 8 (2019): 1765-1768.
- Chu EC, Trager RJ, Chen ATC, et al. A 60-Year-Old Man with Gingivitis and Poorly Controlled Diabetes Developing Low Back Pain 1 Week Following Recovery from COVID-19 Diagnosed with Spinal Abscess Due to Streptococcus oralis. Am J Case Rep 23 (2022): e937517.
- Chu EC, Trager RJ, Chen ATC. Conservative Management of Low Back Pain Related to an Unresectable Aggressive Sacral Hemangioma: A Case Report. Am J Case Rep 23 (2022): e936984.
- Chu EC, Trager RJ, Lai CR, Shum JSF. Metastatic Recurrent Breast Cancer Identified in the Chiropractic Office: Case Report and Literature Review. Am J Case Rep. 2022 Sep 4;23:e937609.
- Chu EC, Trager RJ, Chen ATC, et al. A 68-Year-Old Woman with a Remote History of Breast Cancer Presenting with Low Back Pain to a Chiropractic Clinic in Hong Kong with Imaging Findings Consistent with a Vertebral Hemangioma and Vertebral Metastatic Lesions. Am J Case Rep 23 (2022): e938034.
- Chu EC, Trager RJ, Lai CR, Leung BK. Presumptive Prostate Cancer Presenting as Low Back Pain in the Chiropractic Office: Two Cases and Literature Review. Cureus 14 (2022): e30575.
- Chu EC, Trager RJ, Shum JSF, Lai CR. Pancoast Tumor Presenting as Neck Pain in the Chiropractic Office: A Case Report and Literature Review. Am J Case Rep 23 (2022): e937052.
- Chu C, Wong RS. Chiropractic pain control in myelofibrosis: A case report. New Horizons in Clinical Case Reports 2 (2017): 7-9.
- Chu EC. Reducing Cervical Retrolisthesis With Long-Term Monthly Chiropractic Maintenance Care: A Case Report. J Med Cases 13 (2022): 359-364.
- Blum C, Globe G, Terre L, et al. Multinational survey of chiropractic patients: reasons for seeking care. J Can Chiropr Assoc 52 (2008): 175-184.
- Chu ECP. Alleviating cervical radiculopathy by manipulative correction of reversed cervical lordosis: 4 years follow-up. J Family Med Prim Care 10 (2021): 4303-4306.
- Chu ECP, Lo FS, Bhaumik A. Plausible impact of forward head posture on upper cervical spine stability. J Family Med Prim Care. 9 (2020): 2517-2520.
- Vallone SA, Miller J, Larsdotter A, et al. Chiropractic approach to the management of children. Chiropr Osteopat. 18 (2010): 16.
- Keating J. Philosophy in chiropractic. Principles and practice of chiropractic 89 (2005): 91.
- Chu EC, Pong JC. Spontaneous resolution of myopic retinoschisis. AME Case Rep 3 (2019): 3.
- Leung KY, Chu EC, Chin, WL. Cervicogenic visual dysfunction: an understanding of its pathomechanism. Med and Pharm Rep 95 (2022): 2.
- Chu EC. Cervical Radiculopathy as a Hidden Cause of Angina: Cervicogenic Angina. J Med Cases 13 (2022): 545-550.
- Chu ECP, Lin AFC. Relief of postural orthostatic tachycardia syndrome with chiropractic rehabilitation. J Family Med Prim Care 11 (2022): 4006-4009.
- Chu EC. Large abdominal aortic aneurysm presented with concomitant acute lumbar disc herniation - a case report. J Med Life 15 (2022): 871-875.
- Chu EC, Leung K, Ng LL, et al. Vascular Thoracic Outlet Syndrome: A Case Report. J Contemp Chiropr 4 (2021): 142-145.
- Chu EC, Butler KR. Resolution of Gastroesophageal Reflux Disease Following Correction for Upper Cross Syndrome-A Case Study and Brief Review. Clin Pract 11 (2021): 322-326.
- Chu ECP, Shum JSF, Lin AFC. Unusual Cause of Dysphagia in a Patient With Cervical Spondylosis. Clin Med Insights Case Rep 12 (2019): 1179547619882707.
- Chu ECP, Lee LYK. Cervicogenic dysphagia associated with cervical spondylosis: A case report and brief review. J Family Med Prim Care 10 (2021): 3490-3493.
- Chu ECP, Lin AFC. Neck-tongue syndrome. BMJ Case Rep 11 (2018).
- Chu ECP. Taming of the Testicular Pain Complicating Lumbar Disc Herniation With Spinal Manipulation. Am J Mens Health. 14 (2020): 1557988320949358.
- Chu E. Thoracolumbar disc herniation: a hidden cause of monosymptomatic nocturnal enuresis. European Journal of Molecular and Clinical Medicine 8 (2021): 2834-2840.
- Chu ECP, Wong AYL. Chronic Orchialgia Stemming From Lumbar Disc Herniation: A Case Report and Brief Review. Am J Mens Health. 15 (2021): 15579883211018431.
- Chin WL, Chu EC, Chiang R. Screening and Diagnosing Osteoporosis Among Postmenopausal Women in Primary Care Settings in Malaysia: A Systematic Review. Maedica (Bucur) 17 (2022): 492-504.
- Chu ECP, Lee LYK. Adjacent segment pathology of the cervical spine: A case report. J Family Med Prim Care 11 (2022): 787-789.
- Chu EC, Trager RJ. Effectiveness of Multimodal Chiropractic Care Featuring Spinal Manipulation for Persistent Spinal Pain Syndrome Following Lumbar Spine Surgery: Retrospective Chart Review of 31 Adults in Hong Kong. Med Sci Monit 28 (2022): e937640.
- Bronfort G, Haas M, Evans R, et al. Effectiveness of manual therapies: the UK evidence report. Chiropr Osteopat 18 (2010): 3.
- Chou R, Huffman LH; American Pain Society; American College of Physicians. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med 147 (2007): 492-504.
- Koes BW, van Tulder MW, Ostelo R, et al. Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine (Phila Pa 1976) 26 (2001): 2504-2513.
- Goertz CM, Long CR, Vining RD, et al. Assessment of chiropractic treatment for active duty, U.S. military personnel with low back pain: study protocol for a randomized controlled trial. Trials 17 (2016): 70.
- Hoskins W, Pollard H. The effect of a sports chiropractic manual therapy intervention on the prevention of back pain, hamstring and lower limb injuries in semi-elite Australian Rules footballers: a randomized controlled trial. BMC Musculoskelet Disord 11 (2010): 64.
- Westrom KK, Maiers MJ, Evans RL, et al. Individualized chiropractic and integrative care for low back pain: the design of a randomized clinical trial using a mixed-methods approach. Trials 11 (2010): 24.
- Schneider M, Haas M, Glick R, et al. Comparison of spinal manipulation methods and usual medical care for acute and subacute low back pain: a randomized clinical trial. Spine (Phila Pa 1976) 40 (2015): 209-217.
- Aure OF, Nilsen JH, Vasseljen O. Manual therapy and exercise therapy in patients with chronic low back pain: a randomized, controlled trial with 1-year follow-up. Spine (Phila Pa 1976) 28 (2003): 525-531.
- Dougherty PE, Karuza J, Savino D, et al. Evaluation of a modified clinical prediction rule for use with spinal manipulative therapy in patients with chronic low back pain: a randomized clinical trial. Chiropr Man Therapy 22 (2014): 41.
- Bronfort G, Maiers M, Schulz C, et al. Multidisciplinary integrative care versus chiropractic care for low back pain: a randomized clinical trial. Chiropr Man Therap 30 (2022): 10.
- Hsieh CY, Adams AH, Tobis J, et al. Effectiveness of four conservative treatments for subacute low back pain: a randomized clinical trial. Spine (Phila Pa 1976) 27 (2002): 1142-1148.
- Aldington DJ. Back pain: the silent military threat: comment on "back pain during war". Arch Intern Med 169 (2009): 1923-1924.
- van Tulder MW, Koes BW, Bouter LM. Conservative treatment of acute and chronic nonspecific low back pain. A systematic review of randomized controlled trials of the most common interventions. Spine (Phila Pa 1976) 22 (1997): 2128-2156.
- Preference Collaborative Review Group. Patients' preferences within randomised trials: systematic review and patient level meta-analysis. BMJ 337 (2008): a1864.
- Boon H, Verhoef M, O'Hara D, et al. From parallel practice to integrative health care: a conceptual framework. BMC Health Serv Res 4 (2004): 15.
- Kizhakkeveettil A, Rose K, Kadar GE. Integrative therapies for low back pain that include complementary and alternative medicine care: a systematic review. Glob Adv Health Med 3 (2014): 49-64.
- Wayne PM, Eisenberg DM, Osypiuk K, et al. A Multidisciplinary Integrative Medicine Team in the Treatment of Chronic Low-Back Pain: An Observational Comparative Effectiveness Study. J Altern Complement Med 24 (2018): 781-791.
- Hebert J, Koppenhaver S, Fritz J, et al. Clinical prediction for success of interventions for managing low back pain. Clin Sports Med 27 (2008): 463-479.
- Machado LA, Kamper SJ, Herbert RD, et al. Analgesic effects of treatments for non-specific low back pain: a meta-analysis of placebo-controlled randomized trials. Rheumatology (Oxford) 48 (2009): 520-527.
